Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
1
The Enterobacteriaceae are a large, heterogeneous group of gram-
negative rods whose natural habitat is the intestinal tract of humans
and animals. The family includes many genera (Escherichia, Shigella,
Salmonella, Enterobacter, Klebsiella, Serratia, Proteus, and others).
Some enteric organisms, eg, Escherichia coli, are part of the normal
flora and incidentally cause disease, while others, the salmonellae and
shigellae, are regularly pathogenic for humans.
The Enterobacteriaceae are facultative anaerobes or aerobes, ferment
a wide range of carbohydrates, possess a complex antigenic structure,
and produce a variety of toxins and other virulence factors.
The family Enterobacteriaceae have the following characteristics:
They are gram-negative rods, either motile with peritrichous flagella
(Bacilli with many flagella all over their surface) or nonmotile.
They grow on peptone (water-soluble protein derivatives) or meat
extract media without the addition of sodium chloride or other
supplements; grow well on MacConkey agar (MacConkey agar is
a culture medium designed to grow Gram-negative bacteria and
differentiate them for lactose fermentation); grow aerobically and
anaerobically (are facultative anaerobes); ferment rather than oxidize
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
2
glucose, often with gas production; are catalase-positive, oxidase-
negative, and reduce nitrate to nitrite; and have a 39–59% G + C DNA
content. Examples of biochemical tests used to differentiate the
species of Enterobacteriaceae are presented in Table 15–1.
The major groups of Enterobacteriaceae are described in here, while
specific characteristics of salmonellae, shigellae, are discussed
separately in another lecture.
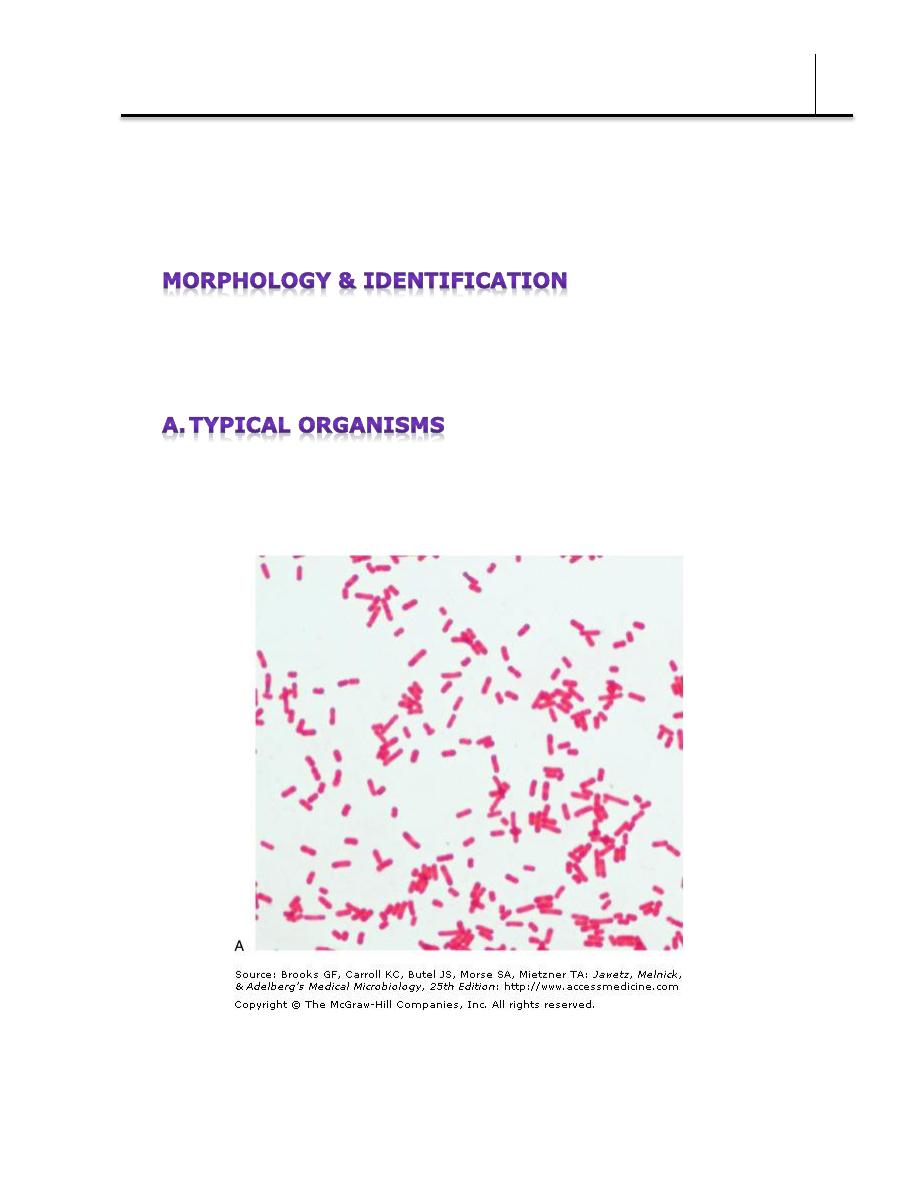
The Enterobacteriaceae are short gram-negative rods. Capsules are
large and regular in Klebsiella, less so in Enterobacter, and uncommon
in the other species.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
3
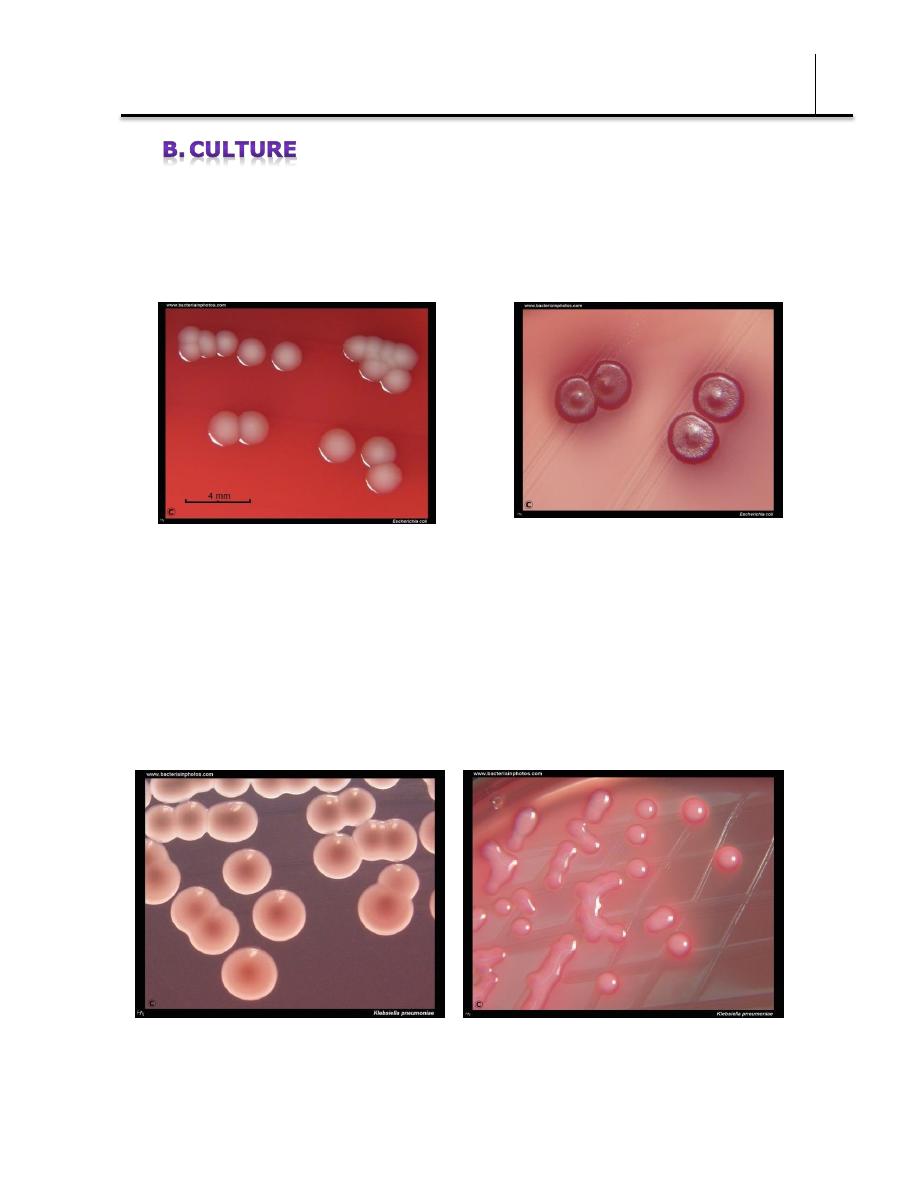
E coli and most of the other enteric bacteria form circular, convex,
smooth colonies with distinct edges. Some strains of E coli produce
hemolysis on blood agar.
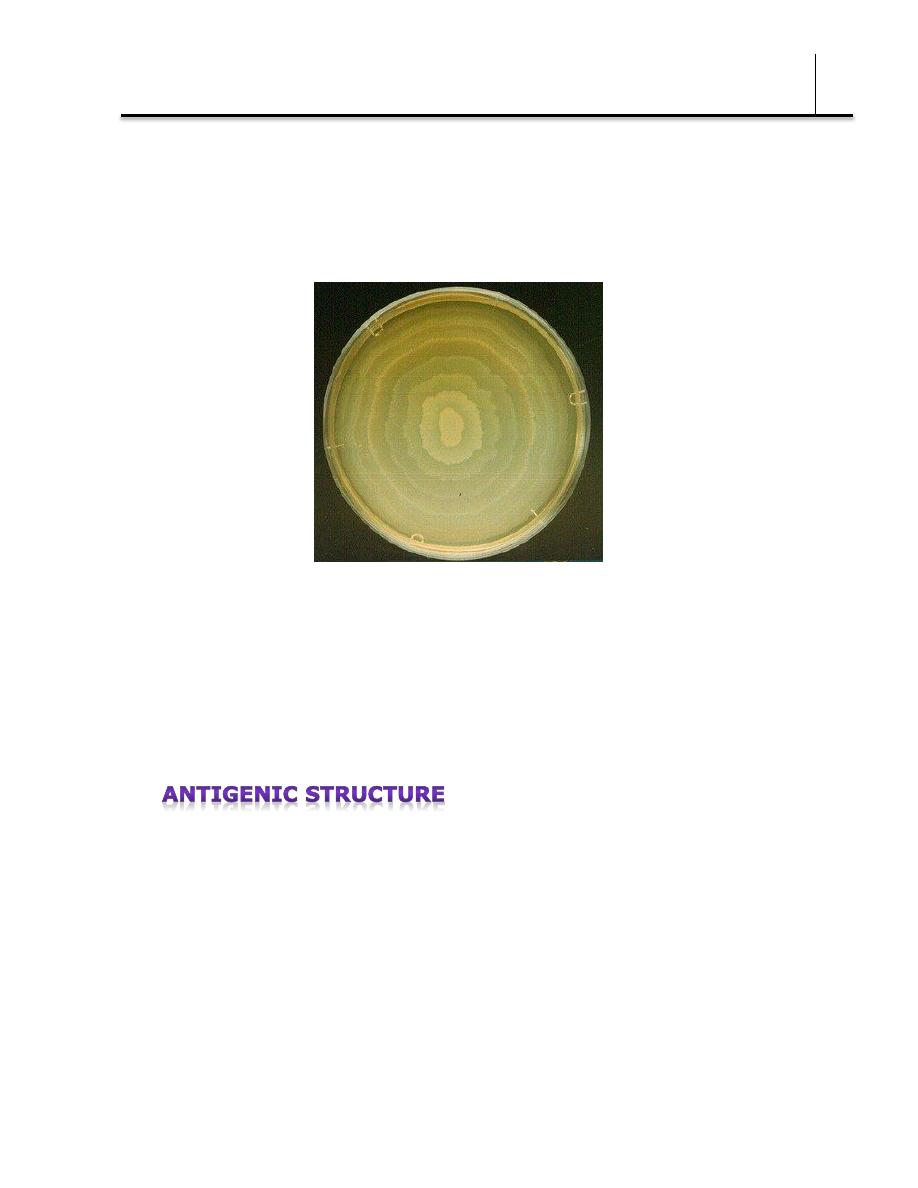
Klebsiella colonies are large and very mucoid and tend to unite with
prolonged incubation.
Klebsiella pneumoniae on Endo agar.
Large, mucous colonies after 24 hours of
cultivation in aerobic atmosphere, 37°C.
Mucous,
lactose
positive
colonies
of Klebsiella pneumoniae on MacConkey
agar. Cultivation 37°C, 24 hours.
Escherichia coli cultivated on blood agar.
Cultivation 24 hours in an aerobic atmosphere,
37°C. Colonies are without hemolysis but many
strains isolated from infections are beta-hemolytic
Escherichia coli cultivated on
MacConkey agar. Lactose positive
colonies. Cultivation 24 hours in an
aerobic atmosphere, 37°C.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
4
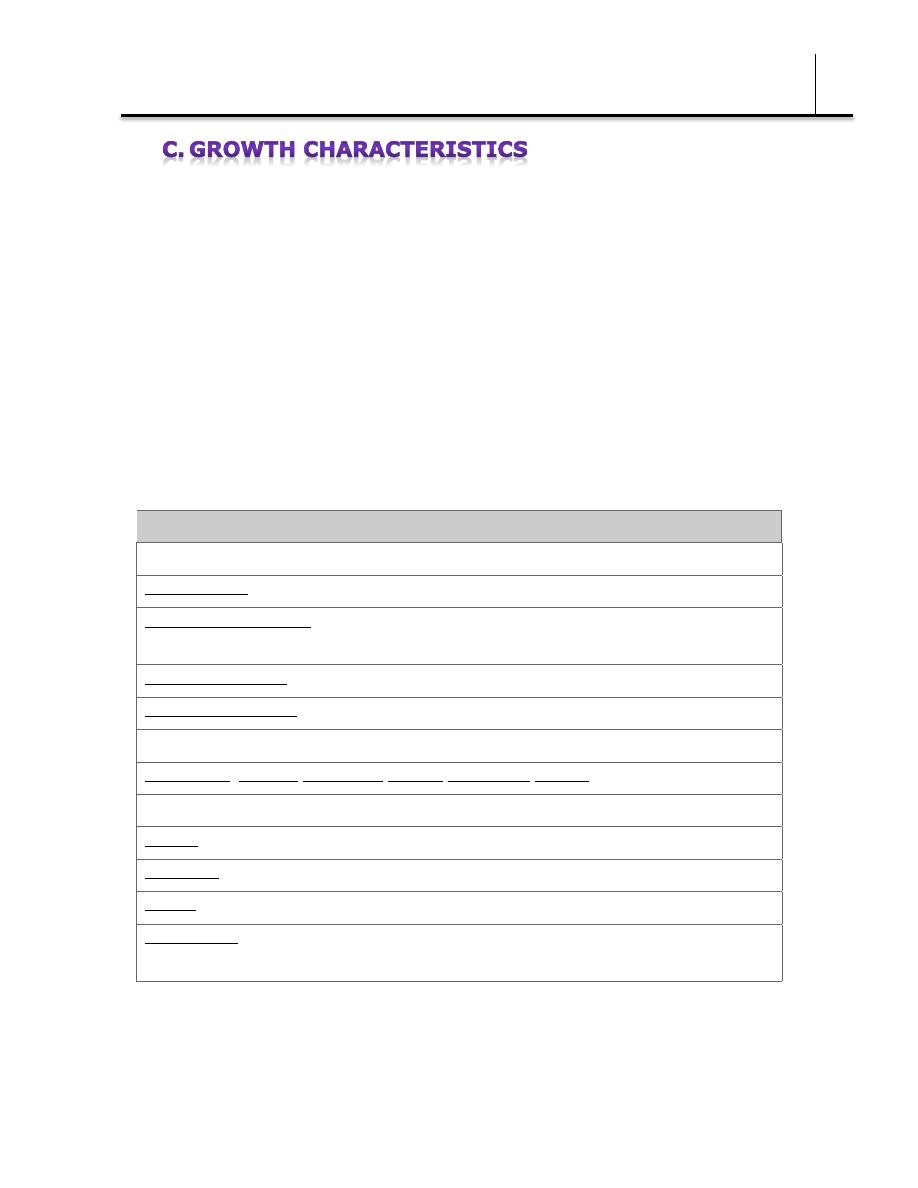
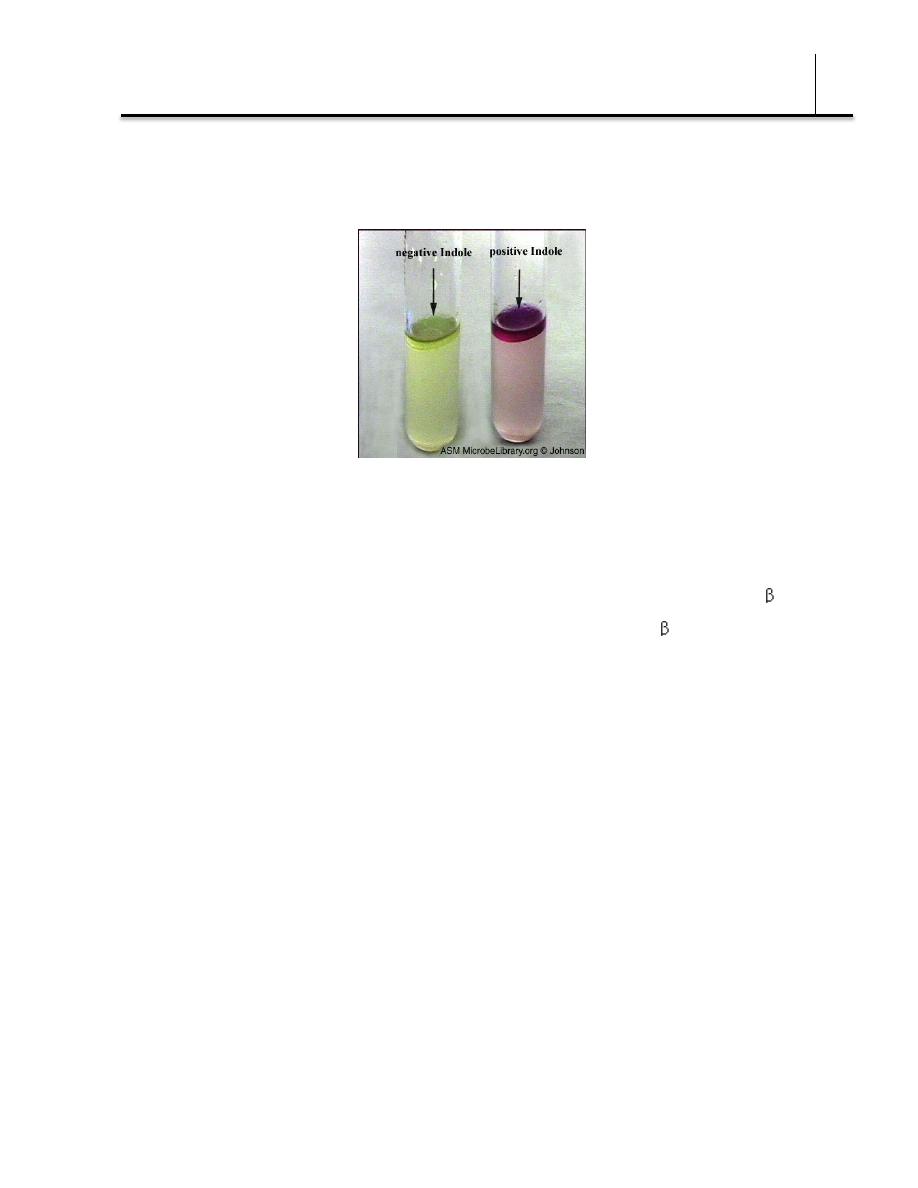
Carbohydrate fermentation patterns and the activity of amino acid
decarboxylases and other enzymes are used in biochemical
differentiation (Table 15–1). Some tests, eg, the production of indole
from tryptophan, are commonly used in rapid identification systems.
Culture on "differential" media that contain special dyes and
carbohydrates (eg, eosin-methylene blue [EMB], MacConkey, or
deoxycholate medium) distinguishes lactose-fermenting (colored) from
nonlactose-fermenting colonies (nonpigmented) and may allow rapid
presumptive identification of enteric bacteria (Table 15–2).
Table 15–2 Rapid, Presumptive Identification of Gram-Negative Enteric Bacteria
Lactose fermented rapidly
Escherichia coli: metallic sheen on differential media; motile; flat, nonviscous colonies
Enterobacter aerogenes: raised colonies, no metallic sheen; often motile; more viscous
growth
Enterobacter cloacae: similar to Enterobacter aerogenes
Klebsiella pneumoniae: very viscous, mucoid growth; nonmotile
Lactose fermented slowly
Edwardsiella, Serratia, Citrobacter, Arizona, Providencia, Erwinia
Lactose not fermented
Shigella species: nonmotile; no gas from dextrose
Salmonella species: motile; acid and usually gas from dextrose
Proteus species: "swarming" on agar; urea rapidly hydrolyzed (smell of ammonia)
Pseudomonas species (see Chapter 16): soluble pigments, blue-green and fluorescing;
sweetish smell
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
5
1. Escherichia—E coli typically produces positive tests for indole,
lysine decarboxylase, and mannitol fermentation and produces gas
from glucose.
The
amino
acid
tryptophan
is
found
in
nearly
all
proteins.
Positive Indole: Bacteria that contain tryptophanase can hydrolyse tryptophan to its metabolic
products (indole, pyruvic acid, ammonia) This will form a layer of red color on the surface
An isolate from urine can be quickly identified as E coli by its
hemolysis on blood agar. Over 90% of E coli isolates are positive for -
glucuronidase using the substrate 4-methylumbelliferyl- -glucuronide
(MUG). Isolates from anatomic sites other than urine, with
characteristic properties (above plus negative oxidase tests) often can
be confirmed as E coli with a positive MUG test.
2. Klebsiella-Enterobacter-Serratia group—
Klebsiella
species
exhibit mucoid growth, large polysaccharide capsules, and lack of
motility, and they usually give positive tests for lysine decarboxylase
and citrate. Serratia produces DNase, lipase, and gelatinase.
Klebsiella, Enterobacter, and Serratia usually give positive Voges-
Proskauer reactions.
3. Proteus-Morganella-Providencia group—The members of this
group deaminate phenylalanine, are motile, grow on potassium
cyanide medium (KCN), and ferment xylose.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
6
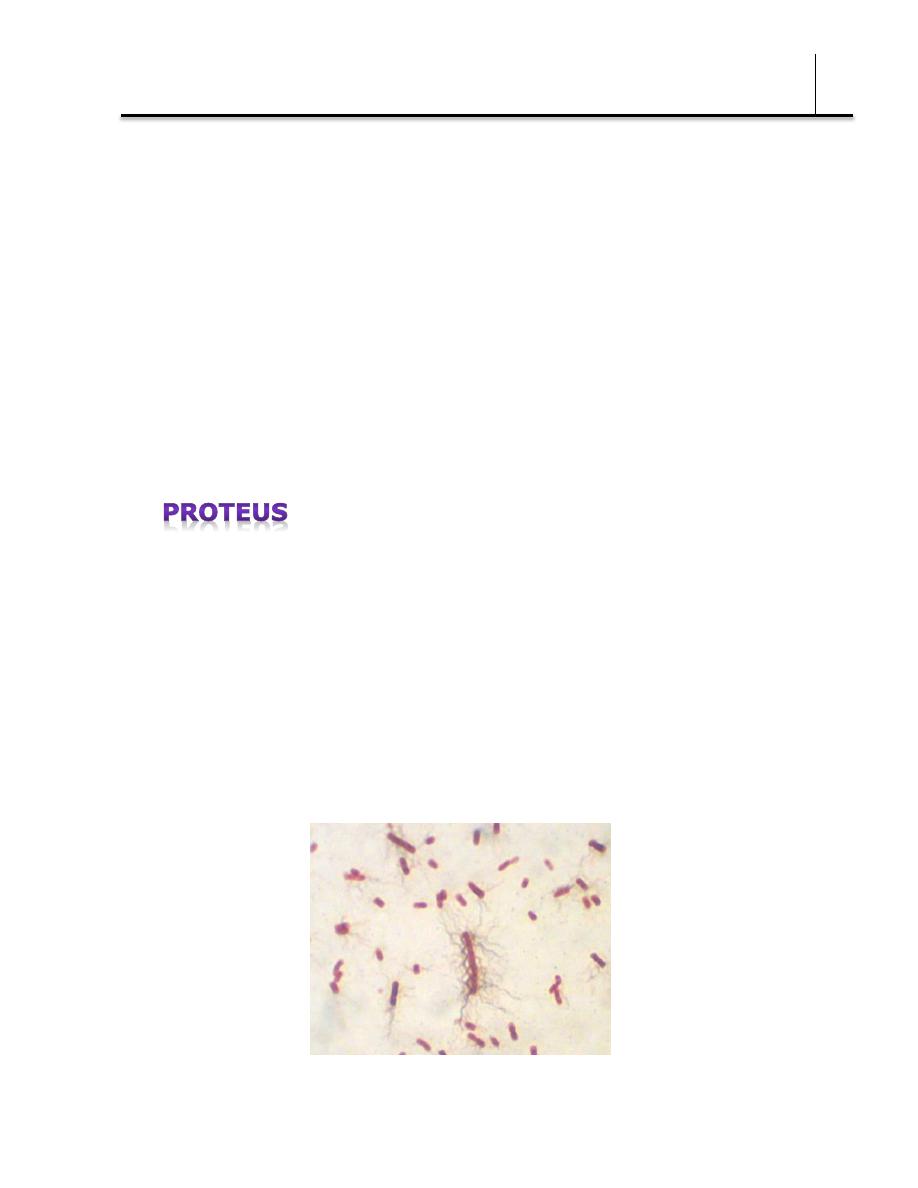
Proteus species move very actively by means of peritrichous flagella,
resulting in "swarming" on solid media unless the swarming is inhibited
by chemicals, eg, phenylethyl alcohol or CLED (cystine-lactose-
electrolyte-deficient) medium.
swarming growth of P. mirabilis inoculated centrally onto a blood agar plate is incubated
overnight @ 37 degrees celcius.
Copyright © 2013, MicrobLog: Microbiology Training Log
Proteus species and Morganella morganii are urease-positive.
The Proteus-Providencia group ferments lactose very slowly or not at
all. Proteus mirabilis is more susceptible to antimicrobial drugs,
including penicillins, than other members of the group.
Enterobacteriaceae have a complex antigenic structure. They are
classified by more than 150 different heat-stable somatic O
(lipopolysaccharide) antigens, more than 100 heat-labile K (capsular)
antigens, and more than 50 H (flagellar) antigens .
O antigens are the most external part of the cell wall
lipopolysaccharide and consist of repeating units of polysaccharide.
Some O-specific polysaccharides contain unique sugars. O antigens are
resistant to heat and alcohol and usually are detected by bacterial
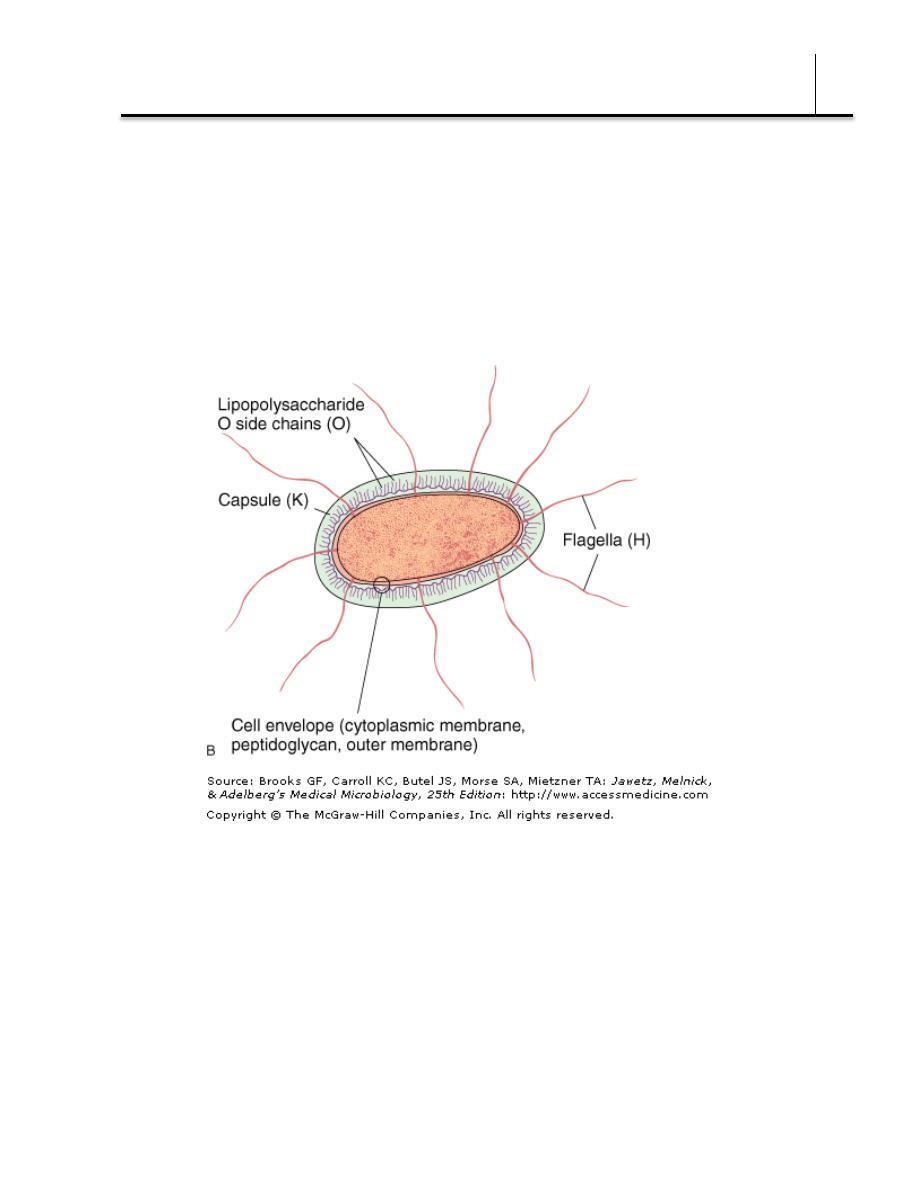
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
7
agglutination. Antibodies to O antigens are predominantly IgM.
While each genus of Enterobacteriaceae is associated with specific O
groups, a single organism may carry several O antigens. E coli may
cross-react with some Providencia, Klebsiella, and Salmonella species.
Occasionally, O antigens may be associated with specific human
diseases, eg, specific O types of E coli are found in diarrhea and in
urinary tract infections.
K antigens are external to O antigens on some but not all
Enterobacteriaceae. Some are polysaccharides, including the K
antigens of E coli; others are proteins. K antigens may interfere with
agglutination by O antisera, and they may be associated with virulence
(eg, E coli strains producing K1 antigen are prominent in neonatal
meningitis, and K antigens of E coli cause attachment of the bacteria
to epithelial cells prior to gastrointestinal or urinary tract invasion).

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
8
Klebsiellae form large capsules consisting of polysaccharides (K
antigens) covering the somatic (O or H) antigens and can be identified
by capsular swelling tests with specific antisera. Human infections of
the respiratory tract are caused particularly by capsular types 1 and 2;
those of the urinary tract, by types 8, 9, 10, and 24.
H antigens are located on flagella and are denatured or removed by
heat or alcohol. They are preserved by treating motile bacterial
variants with formalin. Such H antigens agglutinate with anti-H
antibodies, mainly IgG. The determinants in H antigens are a function
of the amino acid sequence in flagellar protein (flagellin). Within a
single serotype, flagellar antigens may be present in either or both of
two forms, called phase 1 , and phase 2.
The organism tends to change from one phase to the other; this is
called phase variation. H antigens on the bacterial surface may
interfere with agglutination by anti-O antibody.
There are many examples of overlapping antigenic structures between
Enterobacteriaceae and other bacteria. Most Enterobacteriaceae share
the O14 antigen of E coli. The type 2 capsular polysaccharide of
Klebsiella is very similar to the polysaccharide of type 2 pneumococci.
Some K antigens cross-react with capsular polysaccharides of
Haemophilus influenzae or Neisseria meningitidis. Thus, E coli
O75:K100:H5 can induce antibodies that react with H influenzae type
b.
The antigenic classification of Enterobacteriaceae often indicates the
presence of each specific antigen. Thus, the antigenic formula of an E
coli may be O55:K5:H21; that of Salmonella Schottmülleri is
O1,4,5,12:Hb:1,2.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
9
Many gram-negative organisms produce bacteriocins. These high-
molecular-weight bactericidal proteins are produced by certain strains
of bacteria active against some other strains of the same or closely
related species. Their production is controlled by plasmids. Colicins are
produced by E coli, marcescens by Serratia, and pyocins by
Pseudomonas. Bacteriocin-producing strains are resistant to their own
bacteriocin; thus, bacteriocins can be used for "typing" of organisms.
Most gram-negative bacteria possess complex lipopolysaccharides in
their cell walls. These substances, cell envelope (cytoplasmic
membrane, peptidoglycan, outer membrane) endotoxins, have a
variety of pathophysiologic effects that are summarized in Chapter 9.
Many gram-negative enteric bacteria also produce exotoxins of clinical
importance. Some specific toxins are discussed in subsequent sections.
E coli is a member of the normal intestinal flora. Other enteric bacteria
(Proteus, Enterobacter, Klebsiella) are also found as members of the
normal intestinal flora but are considerably less common than E coli.
The enteric bacteria are sometimes found in small numbers as part of
the normal flora of the upper respiratory and genital tracts. The enteric
bacteria generally do not cause disease, and in the intestine they may
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
10
even contribute to normal function and nutrition.
The bacteria become pathogenic only when they reach tissues outside
of their normal intestinal or other less common normal flora sites. The
most frequent sites of clinically important infection are the urinary
tract, biliary tract, and other sites in the abdominal cavity, infections of
the blood stream, prostate gland, lung, bone, meninges can also be
present. When normal host defenses are inadequate—particularly in
infancy or old age, in the terminal stages of other diseases, after
immunosuppression, or with indwelling venous or urethral catheters—
localized clinically important infections can result, and the bacteria
may reach the bloodstream and cause sepsis.
The clinical manifestations of infections with E coli and the other
enteric bacteria depend on the site of the infection and cannot be
differentiated by symptoms or signs from processes caused by other
bacteria.
1. Urinary tract infection—E coli is the most common cause of
urinary tract infection and accounts for approximately 90% of first
urinary tract infections in young women. The symptoms and signs
include urinary frequency, dysuria, hematuria, and pyuria. Flank pain
is associated with upper tract infection. None of these symptoms or
signs is specific for E coli infection. Urinary tract infection can result in
bacteremia with clinical signs of sepsis.
Most of the urinary tract infections that involve the bladder or kidney
in an otherwise healthy host are caused by a small number of O
antigen types that have specifically elaborated virulence factors that

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
11
facilitate colonization and subsequent clinical infections. These
organisms are designated as uropathogenic E coli. Typically these
organisms produce hemolysin, which is cytotoxic and facilitates tissue
invasion. Those strains that cause pyelonephritis (from Greek pyelum,
meaning "renal pelvis", pyelonephritis is an inflammation of the renal
parenchyma, calyces, and pelvis) express K antigen and elaborate a
specific type of pilus, P fimbriae, which binds to the P blood group
antigen (note: P blood group system, classification of human blood
based on the presence of any of three substances known as the P, P1,
and Pk antigens on the surfaces of red blood cells. These antigens are
also expressed on the surfaces of cells lining the urinary tract, where
they have been identified as adhesion sites for Escherichia coli
bacteria, which cause urinary tract infections.).
2. E coli-associated diarrheal diseases—E coli that cause diarrhea
are extremely common worldwide. These E coli are classified by the
characteristics of their virulence properties (see below), and each
group causes disease by a different mechanism. The small or large
bowel epithelial cell adherence properties are encoded by genes on
plasmids.
1) Enteropathogenic E coli (EPEC) is an important cause of
diarrhea in infants, especially in developing countries. EPEC
previously was associated with outbreaks of diarrhea in nurseries
in developed countries. EPEC adhere to the mucosal cells of the
small bowel. There is loss of microvilli (effacement “shortening
or thining of tissue”), formation of filamentous actin pedestals or
cup-like structures, and, occasionally, entry of the EPEC into the
mucosal cells.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
12
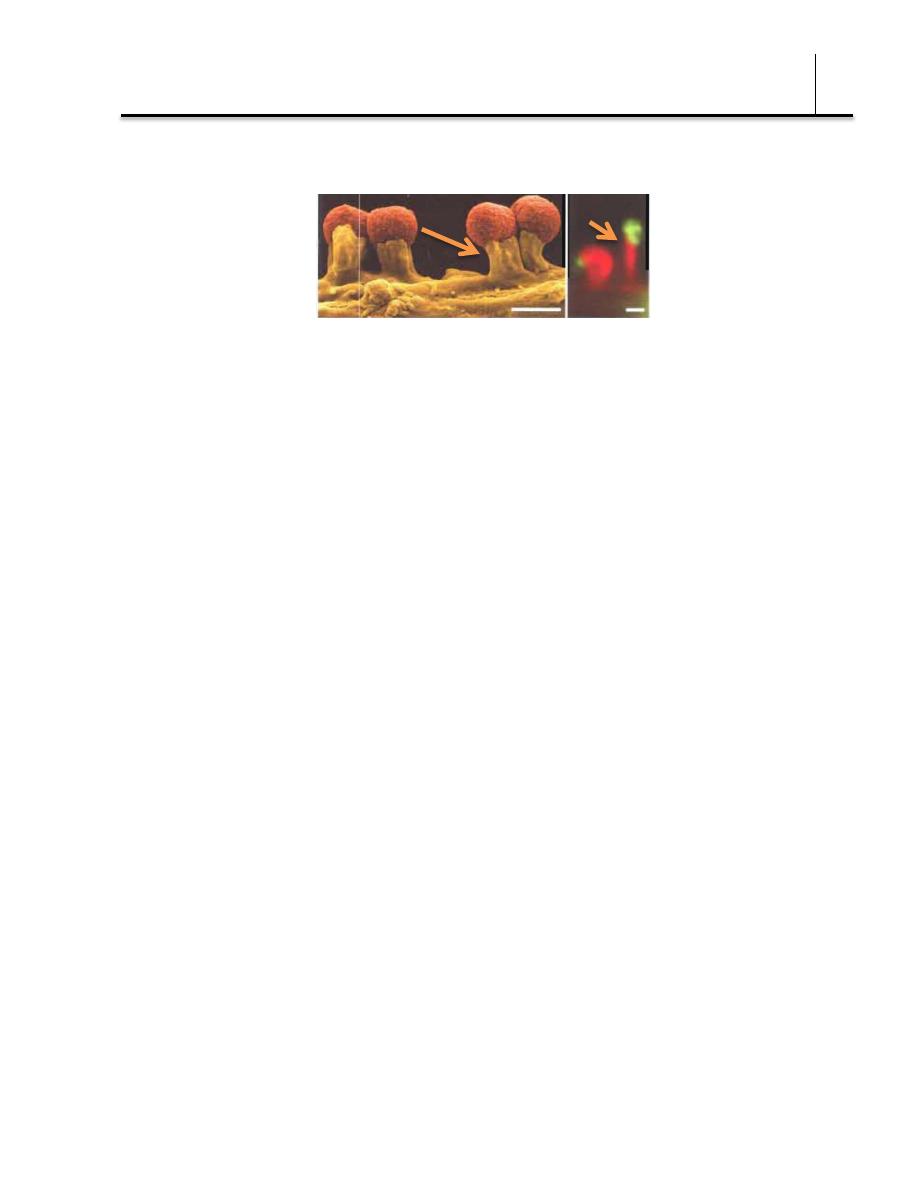
formation of a raised, pedestal-like structure beneath the bacterium that characterizes
this lesion (© Deibel et al., 1998)
Lesions are characterized by a localized loss of microvilli and intimate
adherence of bacteria to the cell surface followed by recruitment of the
cellular actin assembly machinery to sites of bacterial attachment,
resulting in the formation of actin-rich pseudopod-like structures
termed pedestals to which the bacteria intimately adhere.
Characteristic lesions can be seen on electron micrographs of
small bowel biopsy lesions.
The result of EPEC infection is sever, watery diarrhea, vomiting,
and fever, which is usually self-limited but can be chronic. EPEC
diarrhea has been associated with multiple specific serotypes of
E coli; strains are identified by O antigen and occasionally by H
antigen typing. Tests to identify EPEC are performed in reference
laboratories. The duration of the EPEC diarrhea can be shortened
and the chronic diarrhea cured by antibiotic treatment.
2) Enterotoxigenic E coli (ETEC) is a common cause of
"traveler's diarrhea" and a very important cause of diarrhea in
infants in developing countries. ETEC colonization factors specific
for humans promote adherence of ETEC to epithelial cells of the
small bowel. Some ETEC produce heat-labile exotoxin (LT).

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
13
The bacteria subunit B attach to the ganglioside (note: The name
ganglioside came from the first isolation of lipids from ganglion
cells of the brain. Ganglioside is
a component of the cell plasma
signal transduction events) at
the brush border of epithelial
cells of the small intestine and
facilitates the entry of subunit A
into the cell, where the latter
activates adenylyl cyclase. This markedly increases the local
concentration of cyclic adenosine monophosphate (cAMP), which
results in intense and prolonged hypersecretion of water and
chlorides and inhibits the reabsorption of sodium. The gut lumen
is distended with fluid, and hypermotility and diarrhea ensue,
lasting for several days.
LT is antigenic and cross-reacts with the enterotoxin of Vibrio
cholerae. LT stimulates the production of neutralizing antibodies
in the serum (and perhaps on the gut surface) of persons
previously infected with enterotoxigenic E coli. Persons residing
in areas where such organisms are highly prevalent (eg, in some
developing countries) are likely to possess antibodies and are
less prone to develop diarrhea on reexposure to the LT-
producing E coli.
Some strains of ETEC produce the heat-stable enterotoxin (ST), which
is under the genetic control of a heterogeneous group of plasmids. ST
activates guanylyl cyclase in enteric epithelial cells and stimulates fluid
secretion. Many ST-positive strains also produce LT. The strains with

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
14
both toxins produce a more severe diarrhea.
The plasmids carrying the genes for enterotoxins (LT, ST) also may
carry genes for the colonization factors that facilitate the attachment
of E coli strains to intestinal epithelium.
Care in the selection and consumption of foods potentially
contaminated with ETEC is highly recommended to help prevent
traveler's diarrhea. Antimicrobial prophylaxis can be effective but may
result in increased antibiotic resistance in the bacteria and probably
should not be uniformly recommended. Once diarrhea develops,
antibiotic treatment effectively shortens the duration of disease.
3) Shiga toxin producing E coli (STEC) are named for the
cytotoxic toxins they produce. There are at least two antigenic
forms of the toxin referred to as Shiga-like toxin 1 and Shiga-like
toxin 2. STEC has been associated with hemorrhagic colitis, a
severe form of diarrhea, and with hemolytic uremic syndrome, a
disease resulting in acute renal failure, microangiopathic
hemolytic anemia, and thrombocytopenia. The Shiga-like toxins
have many properties that are similar to the Shiga toxin
produced by some strains of Shigella dysenteriae type 1;
however, the two toxins are antigenically and genetically
distinct. Of the E coli serotypes that produce Shiga toxin,
O157:H7 is the most common and is the one that can be
identified in clinical specimens. STEC O157:H7 does not use
sorbitol, unlike most other E coli, and is negative on sorbitol
MacConkey agar (sorbitol is used instead of lactose); O157:H7
strains also are negative on MUG tests (note: MUG is a test used
to determine if there are coliforms in food or water samples. The
detection of E. coli with MUG is based on the ability of beta-
glucuronidase, an enzyme possessed by most E. coli strains, to

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
15
hydrolyze 4-methylumbelliferyl-beta-D-glucuronide (MUG). The
hydrolysis of MUG by E. coli yields a fluorescent end
product. Development of fluorescence allows the detection of E.
coli). Many of the non-O157 serotypes may be sorbitol positive,
when grown in culture. Specific antisera are used to identify the
O157:H7 strains. Assays for Shiga toxin using commercially
available enzyme immunoassays are done in many laboratories.
Other sensitive test methods include cell culture cytotoxin
testing and polymerase chain reaction PCR for the direct
detection of toxin genes from stool samples. Many cases of
hemorrhagic colitis and its associated complications can be
prevented by thoroughly cooking ground beef.
4) Enteroinvasive E coli (EIEC) produces a disease very similar
to shigellosis. The disease occurs most commonly in children in
developing countries and in travelers to these countries. Like
Shigella, EIEC strains are non-lactose or late lactose fermenters
and are nonmotile. EIEC produce disease by invading intestinal
mucosal epithelial cells.
5) Enteroaggregative E coli (EAEC) causes acute and chronic
diarrhea (>14 days in duration) in persons in developing
countries. These organisms also are the cause of food-borne
illnesses in industrialized countries. They are characterized by
their specific patterns of adherence to human cells. EAEC
produce ST-like toxin (see above) and a hemolysin.
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
16
3. Sepsis—When normal host defenses are inadequate, E coli may
reach the bloodstream and cause sepsis. Newborns may be highly
susceptible to E coli sepsis because they lack IgM antibodies. Sepsis
may occur secondary to urinary tract infection.
4. Meningitis—E coli and group B streptococci are the leading causes
of meningitis in infants. Approximately 75% of E coli from meningitis
cases have the K1 antigen.
Klebsiella pneumoniae is present in the respiratory tract and feces
of about 5% of normal individuals.
It causes a small proportion (about 1%) of bacterial pneumonias. K
pneumoniae can produce extensive hemorrhagic necrotizing
consolidation of the lung. It produces urinary tract infection and
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
17
bacteremia with focal lesions in debilitated patients. Other enterics
also may produce pneumonia. Klebsiella sp. rank among the top ten
bacterial pathogens responsible for hospital-acquired infections. Two
other klebsiellae are associated with inflammatory conditions of the
upper respiratory tract: Klebsiella pneumoniae subspecies ozaenae has
been isolated from the nasal mucosa in ozena (Ozena is a disease of
the nose in which the bony ridges and mucous membranes of the nose
waste away.), and Klebsiella pneumoniae subspecies rhinoscleromatis
from rhinoscleroma, a destructive granuloma of the nose and pharynx.
Klebsiella granulomatis causes a chronic genital ulcerative disease.
Proteus species produce infections in humans only when the bacteria
leave the intestinal tract. They are found in urinary tract infections and
produce bacteremia, pneumonia, and focal lesions in debilitated
patients or those receiving intravenous infusions. P mirabilis causes
urinary tract infections and occasionally other infections. Proteus
vulgaris and Morganella morganii are important nosocomial pathogens
(Greek "nosus" meaning "disease" , "komeion" meaning "to take care
of" so nosocomial meaning is hospital acquired infections).
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
18
Proteus species produce urease, resulting in rapid hydrolysis of urea
with liberation of ammonia. Thus, in urinary tract infections with
Proteus, the urine becomes alkaline, promoting stone formation and
making acidification virtually impossible. The rapid motility of Proteus
may contribute to its invasion of the urinary tract.
Strains of Proteus vary greatly in antibiotic sensitivity. P mirabilis is
often inhibited by penicillins; the most active antibiotics for other
members of the group are aminoglycosides and cephalosporins.
Specimens
Specimens include urine, blood, pus, spinal fluid, sputum, or other
material, as indicated by the localization of the disease process.
Smears
The Enterobacteriaceae resemble each other morphologically. The
presence of large capsules is suggestive of Klebsiella.
Culture
Specimens are plated on both blood agar and differential media. With
differential media, rapid preliminary identification of gram-negative
enteric bacteria is often possible.
Immunity
Specific antibodies develop in systemic infections, but it is uncertain
whether significant immunity to the organisms follows.
No single specific therapy is available. The sulfonamides, ampicillin,
cephalosporins, fluoroquinolones, and aminoglycosides have marked
antibacterial effects against the enterics, but variation in susceptibility
Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
19
is great, and laboratory tests for antibiotic susceptibility are essential.
Multiple drug resistance is common and is under the control of
transmissible plasmids.
Certain conditions predisposing to infection by these organisms require
surgical correction, eg, relief of urinary tract obstruction, closure of a
perforation in an abdominal organ, or resection of a bronchiectatic
portion of lung. Treatment of gram-negative bacteremia and
impending septic shock requires rapid institution of antimicrobial
therapy, restoration of fluid and electrolyte balance, and treatment of
disseminated intravascular coagulation.
Various means have been proposed for the prevention of traveler's
diarrhea, including daily ingestion of bismuth subsalicylate suspension
(bismuth subsalicylate can inactivate E coli enterotoxin in vitro) and
regular doses of tetracyclines or other antimicrobial drugs for limited
periods. Because none of these methods are entirely successful or
lacking in adverse effects, it is widely recommended that caution be
observed in regard to food and drink in areas where environmental
sanitation is poor and that early and brief treatment (eg, with
ciprofloxacin or trimethoprim-sulfamethoxazole) be substituted for
prophylaxis.
The enteric bacteria establish themselves in the normal intestinal tract
within a few days after birth and from then on constitute a main
portion of the normal aerobic (facultative anaerobic) microbial flora. E
coli is the example. Enterics found in water or milk are accepted as
proof of fecal contamination from sewage or other sources.
Enteropathogenic E coli serotypes should be controlled. Some of the
enterics constitute a major problem in hospital infection. It is

Bacteriology (Lec 3)
Dr. Donya A Makki Enterobacteriaceae
20
particularly important to recognize that many enteric bacteria are
"opportunists" that cause illness when they are introduced into
debilitated patients. Within hospitals or other institutions, these
bacteria commonly are transmitted by personnel, or instruments. Their
control depends on hand washing, rigorous asepsis, sterilization of
equipment, disinfection, restraint in intravenous therapy, and strict
precautions in keeping the urinary tract sterile (ie, closed drainage).
