Baghdad College of Medicine / 5
th
grade
Student’s Name :
Dr. Yasser Naif Qassim
Lec. 1
Basic Principles in
Plastic Surgery
Sun. 25 / 9 / 2016
DONE BY : Ali Kareem
مكتب
اشور لالستنساخ
2016 – 2017
Basic Principles Dr. Yasser N. Qassim
25-9-2016
2
©Ali Kareem 2016-2017
BASIC PRINCIPLES IN PLASTIC SURGERY
Dr.YASSER NAIF QASSIM , F.I.B.M.S(plastic & reconstructive)
Definitions:
Plastic as a word came from a Greek word plastikos which means remold or reform.
Plastic as an adjective = capable of being shaped or formed.
Is a branch of surgery that deals with remold,repair & restore body parts. Unlike other surgical
specialties, plastic surgery is not organized around a specific organ system so it is based on
principles rather than specific surgical procedures.It is divided into 2 main parts:
1.Cosmetic(aesthetic)plastic surgery:That deals with reshaping the normal structures of the
body to improve the patients appearance e.g. rhinoplasty,abdominoplasty,facelift,…etc.
2.Reconstructive plastic surgery:That deals with repairing or reshaping(reconstructing) the
acquired or congenital abnormalities e.g.reconstructing cleft lip,cleft palate,traumatic
wounds,burn deformities,…etc.
WOUNDS
A wound can be defined as a disruption of the normal anatomical relationships of tissues as a
result of an injury. The injury may be intentional such as a surgical incision or accidental
following trauma. Immediately following wounding, the healing process begins.
PHASES OF WOUND HEALING:
1-The inflammatory phase: begins immediately following tissue injury and lasts 2-3 days.
Begins at the time of injury; lasts 2 to 3 days.Initially there will be vasoconstriction to achieve
hemostasis,then platelet plug forms and clotting cascade is activated, resulting in fibrin
deposition.Platelets release platelet-derived growth factor (PDGF) and transforming growth
factor β (TGF-β) from their alpha granules, attracting inflammatory cells, particularly
macrophages ,then vasodilation occurs and vascular permeability increases (due to histamine,
platelet-activating factor, bradykinin, prostaglandins), aiding the infiltration of inflammatory
cells into the wound.Neutrophils peak at 24 hours and help with débridement.Monocytes enter
the wound, becoming macrophages, and peak within 2 to 3 days.Limited numbers of
lymphocytes arrive later.
Basic Principles Dr. Yasser N. Qassim
25-9-2016
3
©Ali Kareem 2016-2017
2-Proliferative phase:begins around day 3, as fibroblasts arrive,and lasts through week
three.Fibroblasts attracted and activated by (PDGF and TGF-β released by platelets and
macrophages) reaching peak numbers by day 7.Collagen synthesis (mainly type III),
angiogenesis, and epithelialization occur.
3-Remodeling phase:
The remodeling phase is the longest part of wound healing and is
believed to last from 21 days to 1-2 year.
collagen accumulation reaches a steady-state, where
there is no change in total collagen content. During this time,there is replacement of the random
collagen fibrils with organized, cross-linked fibrils. Type I collagen replaces type III until it
reaches a 4:1 ratio of type I to type III (that is of normal skin and mature scar tissue).Scars
continue to gain strength over this phase ; however, the tensile strength of scars never reaches
that found in unwounded skin, approaching approximately 70-80% of normal strength.
TYPES OF WOUND HEALING:
1.Primary healing (primary intention):wound closure by direct approximation, pedicle flap or
skin graft within hours of an injury.
2-Secondary Spontaneous healing (secondary intention):wound left open to heal
spontaneously by contraction and epithelialization.Contraction results from centripetal force in
wound margin probably provided by myofibroblasts and epithelialization proceeds from wound
margins to wards center at 1 mm/day.
3-Tertiary healing ( tertiary intention):delayed wound closure after several days and can occur
any time after granulation tissue has formed in wound.Delayed closure should be performed
when the wound is not infected.
Forms of abnormal wound healing:
1-Impaired healing:that occurs due to local and systemic factors.
Local factors
Systemic factors
local ischemia.
edema.
infection.
radiation.
foreign body.
pressure.
D.M.
malnutrition.
chemotherapy.
steroids.
smoking.
immunocompromized state.
aging process.
Basic Principles Dr. Yasser N. Qassim
25-9-2016
4
©Ali Kareem 2016-2017
2-Excessive wound healing: in a form of keloids or hypertrophic scars.
Keloids:
scar tissue that extends beyond the boundaries of the incision or wound, may develop months
to a year after injury, and do not resolve spontaneously. Common in ear lobes,presternal area,shoulders
and areas of tension.
Hypertrophic scars:
scar tissue that does not extend beyond the boundaries of the incision or
wound,develop within weeks of wounding (during the inflammatory phase), and there is usually some
degree of improvement with time.
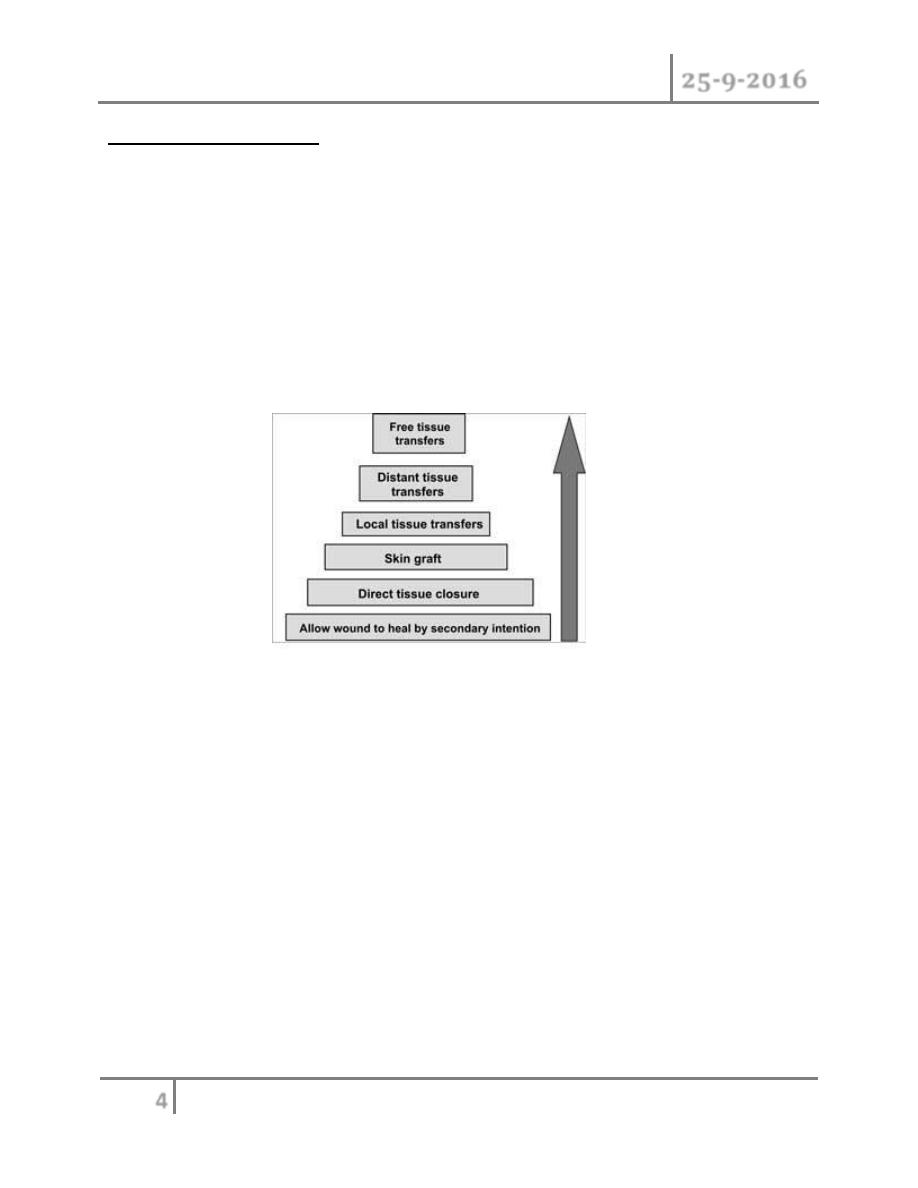
When analyzing a wound, the options for closure are evaluated beginning with the simplest and
progressing up to the more complex option according to the “reconstructive ladder” .
Healing by secondary intention: mostly adopted for small wound,by leaving the wound to heal
by itself without surgical intervention apart from local wound care.It depends upon
epithelialization and wound contraction provided by myofibroblast.
Direct closure: most preferable method because it use the same skin and tissue of the area with
the same coloure and quality but this depends on the availability of the surrounding tissues.When
the wound is clean,direct closure is achieved by approximating the wound edges without
tension.When the wound is contaminated with irregular margins direct closure should not be
done unless the wound is copiously irrigated with normal saline and all the devitalized tissues are
debrided.There are many methods of wound debridment:
1. Mechanical:by sharp or blunt excision of the dead tissues.
2. Gauze:wet to dry dressing.
3. Chemicals:like topical enzymes that digest the dead tissues.
On closing the wounds aseptic measures(hand scrubbing,using sterile istruments,hair shaving
and clean operative site)should be followed and haemostasis should be secured by(digital
pressure,electrocautery,clamping or ligating the bleeding vessel or even by using fibrin glue).
Basic Principles Dr. Yasser N. Qassim
25-9-2016
5
©Ali Kareem 2016-2017
Antibiotics are indicated in:
o Presence of gross contamination or surrounding cellulitis.
o Human or animal bites.
o Immunocompromized and diabetic patients.
o Patients with vulvular heart disease to prevent endocarditis.
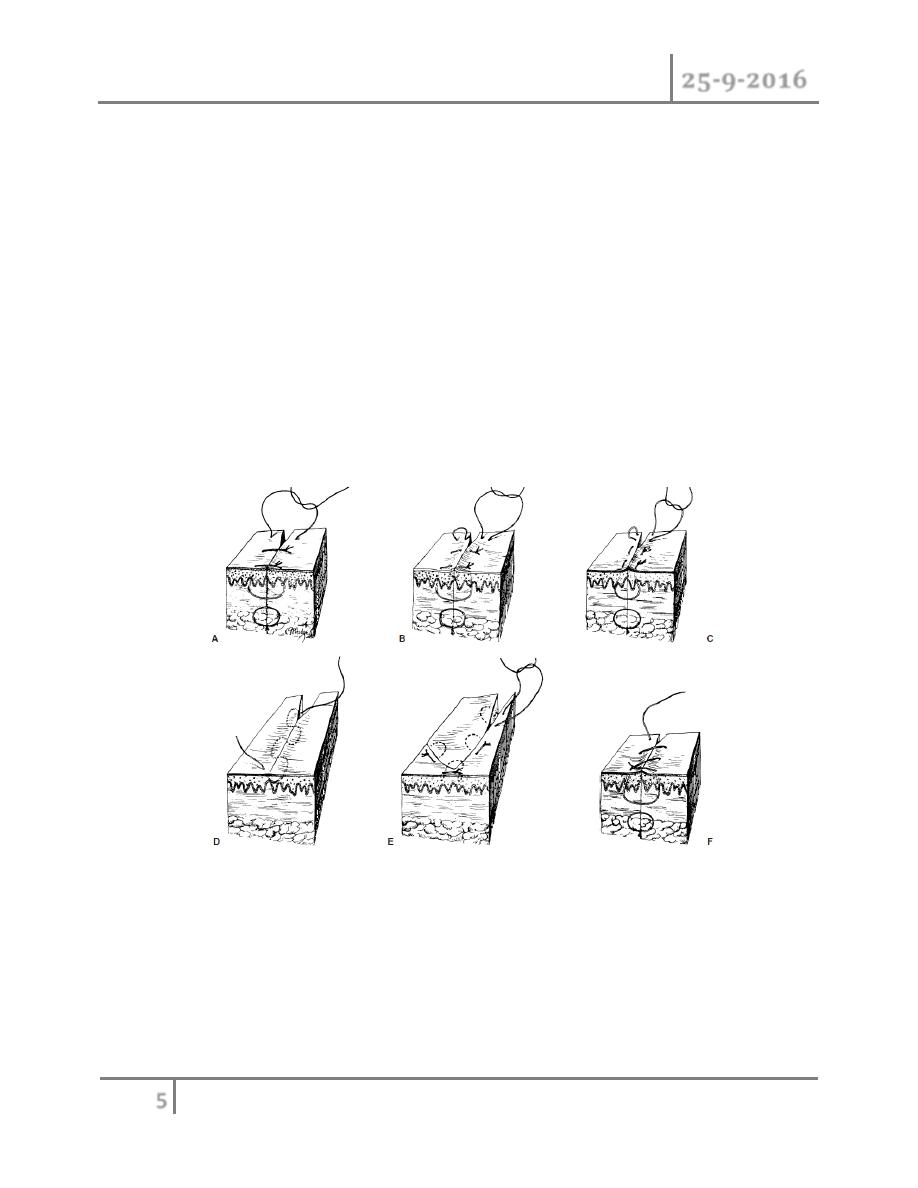
Methods of wound closure:
o Simple interrupted.
o Vertical mattress.
o Horizontal mattress.
o Subcuticular.
o Half buried horizontal mattress.
o Continuous over and over.
In addition to sutures;staples,surgical tapes e.g. steri-strips,and biological or synthetic materials
e.g.cyanoacrylate are used as wound closure materials.
Surgical flaps :
A flap is a segment or unit of tissue that has its own blood supply indicated for:
1. Covering recipient beds that have poor vascularity(e.g. denuded bone,denuded
cartilage,denuded tendon,…etc).
Basic Principles Dr. Yasser N. Qassim
25-9-2016
6
©Ali Kareem 2016-2017
2. Covering vital structures(exposed nerves,exposed major vessels…etc).
3. Reconstructing the full thickness defects of eyelids, lips, ears, nose, and cheeks.
4. Padding body prominences.
5. When it may be necessary to operate through the wound at a later date to repair
underlying structures.
6. Providing a functional motor unit using muscle flaps.
7. Providing sensation using sensate flap.
8. Controlling infection in the recipient area(e.g.in chronic O.M.).
CLASSIFICATION
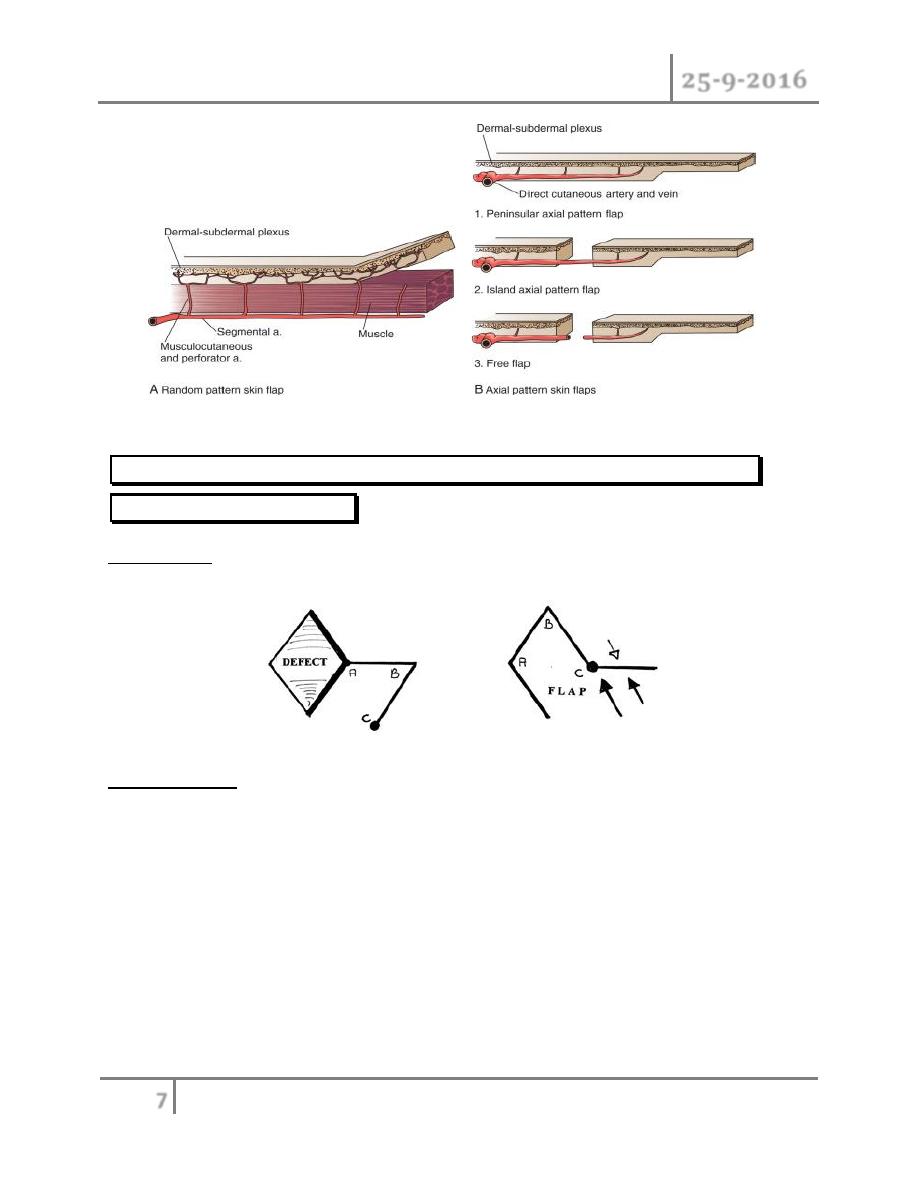
I-ACCORDING TO BLOOD SUPPLY:
A.Random flaps:
have no specific or named blood vessel incorporated in the base of the
flap.They derive their blood supply from the dermal and subdermal plexus.
B.Axial flaps: have specific named vascular system that enters the base and runs along its
axis.They can be sub classified into:
1. Peninsular axial flaps:that keep both the skin and vessel intact at their base.
2. Island axial flaps:that keep only the vessels intact at their base.
3. Free flaps:both the skin and the vessels are transected at flap base and transferred from
the donor site to the recipient site. They require re-anastamosis of the artery and vein with
the recipient vessels at the recipient site.
Basic Principles Dr. Yasser N. Qassim
25-9-2016
7
©Ali Kareem 2016-2017
II.ACCORDING TO LOCATION (proximity to the primary defect that
needs to be reconstructed):
1.Local flaps: are raised from tissues directly adjacent to the primary defect
(in direct contact with the defect).
2.Regional flaps: are raised from tissue in the vicinity but not directly adjacent to the primary
defect(no direct contact with the defect).
Basic Principles Dr. Yasser N. Qassim
25-9-2016
8
©Ali Kareem 2016-2017
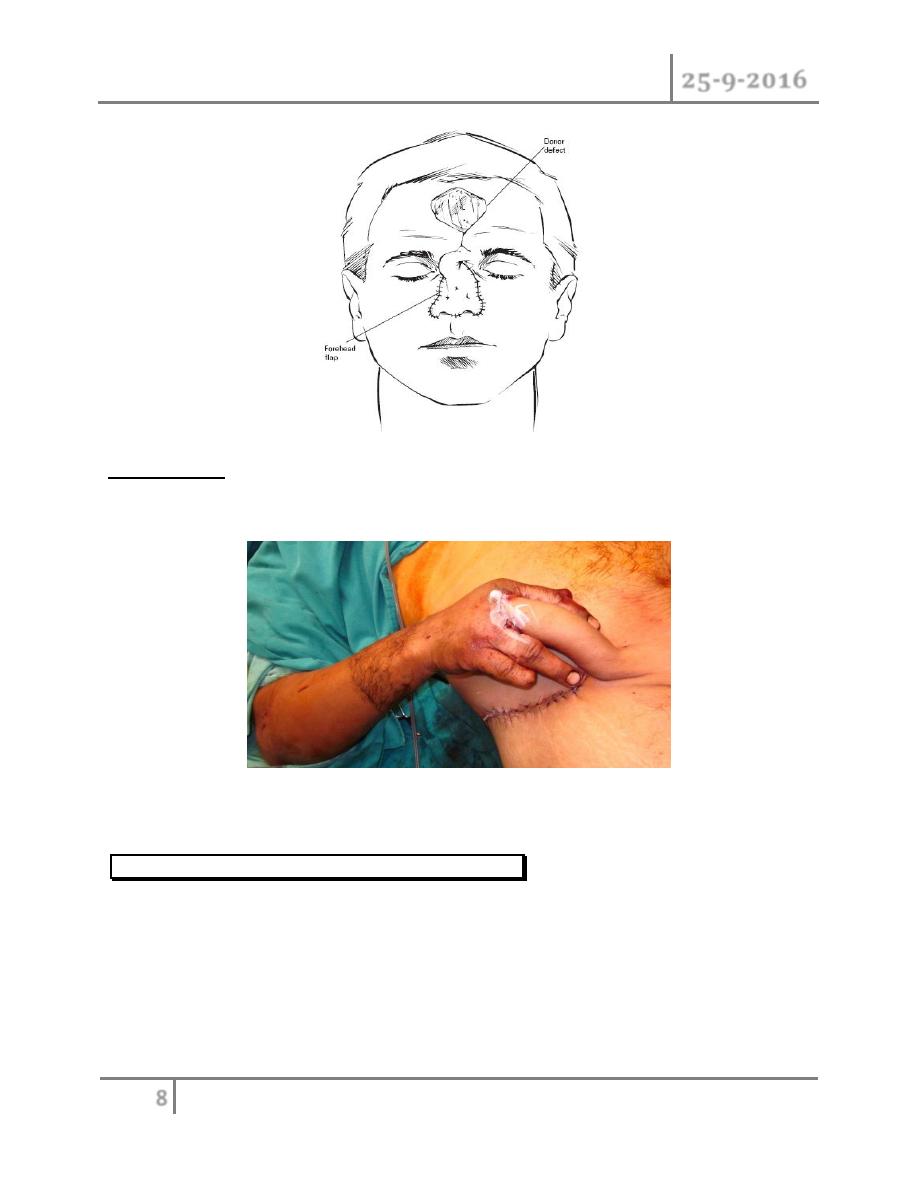
3.Distant flaps: are raised from tissue at a distance from the primary defect.The free flaps
considered distant flaps.
III.ACCORDING TO THE WAY OF MOVEMENT:
A.Pivotal flaps:
flaps that rotate about a pivot point and subdivided into:
1. Rotational flaps:designed and moved in an arc( curvilinear)manner
.

Basic Principles Dr. Yasser N. Qassim
25-9-2016
9
©Ali Kareem 2016-2017
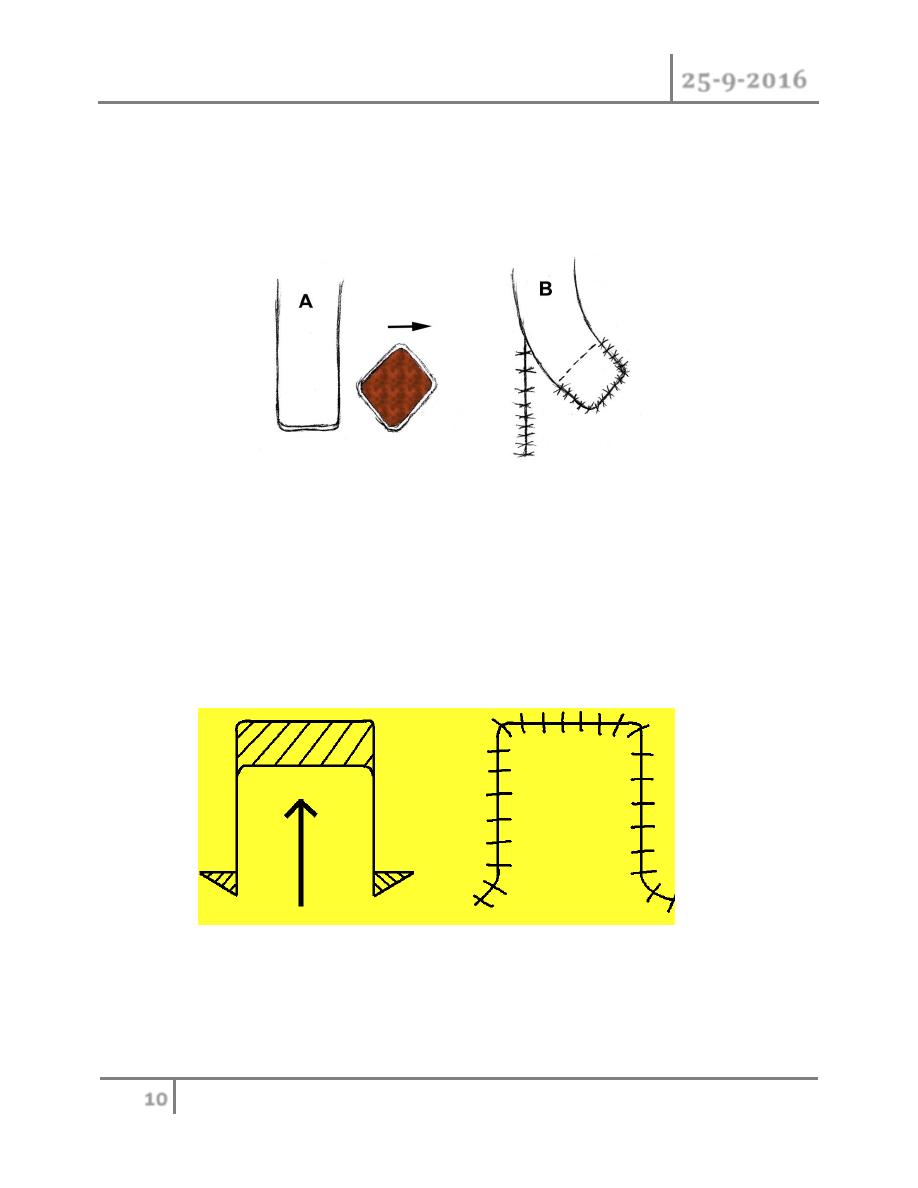
2. Traspositional flaps:triangular or rectangular flaps that move laterally to cover the
directly adjacent defect (its movement is not in an arc manner).
3. Interpolational flaps:as the transpositional flaps but there is a bridge of tissue between
the flap and the defect(i.e. the flap is not in a direct contact with the defect),so
Basic Principles Dr. Yasser N. Qassim
25-9-2016
10
©Ali Kareem 2016-2017
iterpolational flaps are either tunneled under or passed over intervening tissue to close a
defect
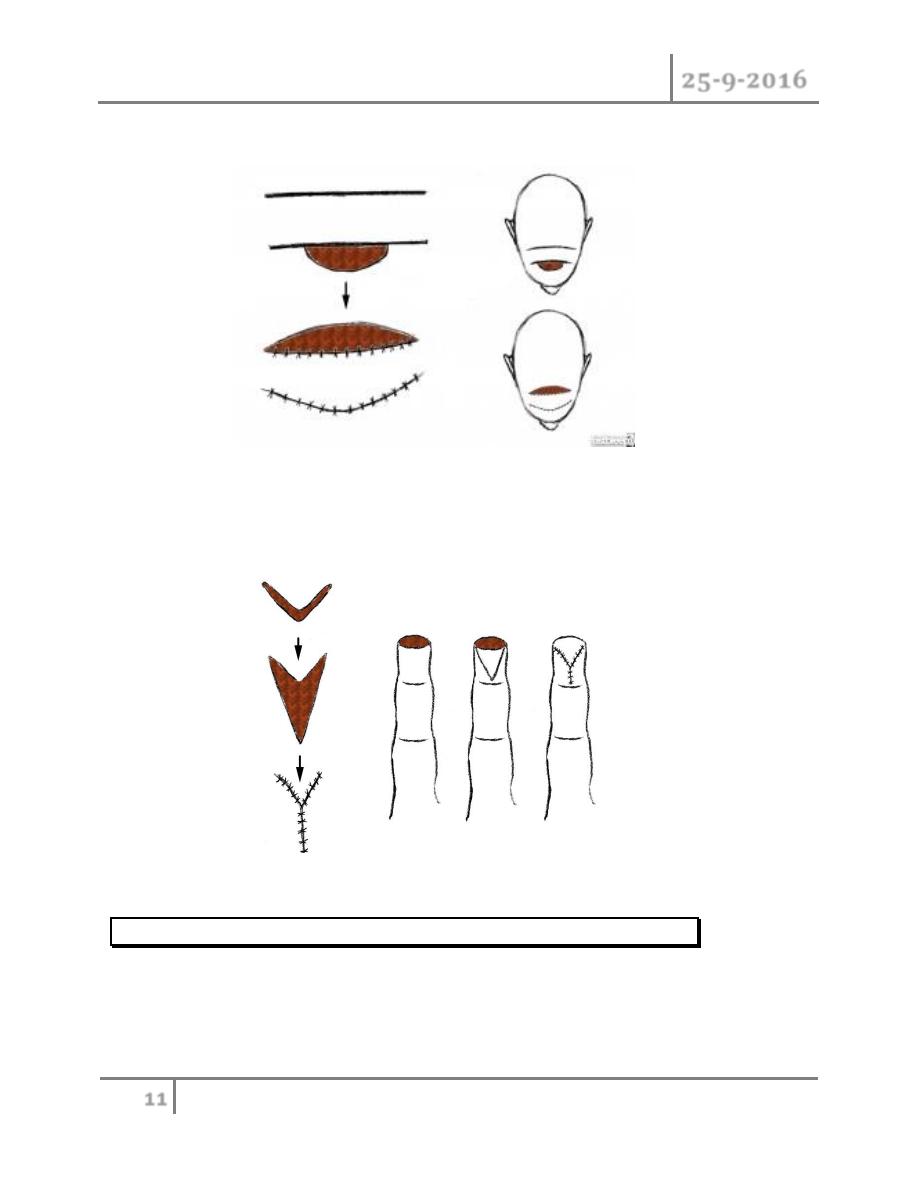
B.Advancement flaps: All advancement flaps are moved directly forward or to one side into a
defect without any rotation or lateral movement about a pivot point like the single-pedicle
advancement, bipedicle advancement, and the V-Y advancement flaps.
single-pedicle advancement flap
Basic Principles Dr. Yasser N. Qassim
25-9-2016
11
©Ali Kareem 2016-2017
bipedicle advancement flap
V-Y advancement flap
IV.ACCORDING TO TISSUE CONTAINED(COMPOSITION):
o Skin flap (skin+superficial fascia).
o Fascia flap e.g. Serratus fascia flap
o Fasciocutaneous (skin +superficial fascia+deep investing fascia)
o Muscle flap e.g.temporalis muscle flap.
o Bone flap e.g. Fibula flap
o Myocutaneous flap(skin+fascia+muscle).

Basic Principles Dr. Yasser N. Qassim
25-9-2016
12
©Ali Kareem 2016-2017
o Osseomyocutaneous(skin+fascia+muscle+bone).
Monitoring of flaps
1. Clinical evaluation is the best method of flap assessment.
o
Temperature: Should be body temperature.
o
Color: Should be pink, neither white nor blue/purple.
o
Capillary refill: Should be approximately 2 seconds.
o
Point bleeding: Upon introduction of a fine-gauge needle, bleeding should be present. Blood
should be red, not purple/blue.
o
Firmness: Should be soft, but with some appreciable turgor.
Signs of insufficient arterial supply: Cold , Paleapillary refill slower than 2 seconds ,slow or absent
point bleeding and softer.
Signs of insufficient venous return (venous congestion):Warmer than expected , blue to purple hue ,
capillary refill faster than 2 seconds (blood pooled in venous system returns rapidly) , brisk point
bleeding,with dark blood , tense and swollen.
2. Doppler studies.
3. Fluorescein dye.
4. Sensors for O
2
, pH, temperature.
Factors leading to flap necrosis:
1. Haematoma collection beneath the flap.
2. Tight suturing.
3. Tight dressing.
4. Kiking of flap pedicle.
5. Cool ambient.
6. Nicotine,caffeine & other vasoconstrictive agents.
7. Technical errors.
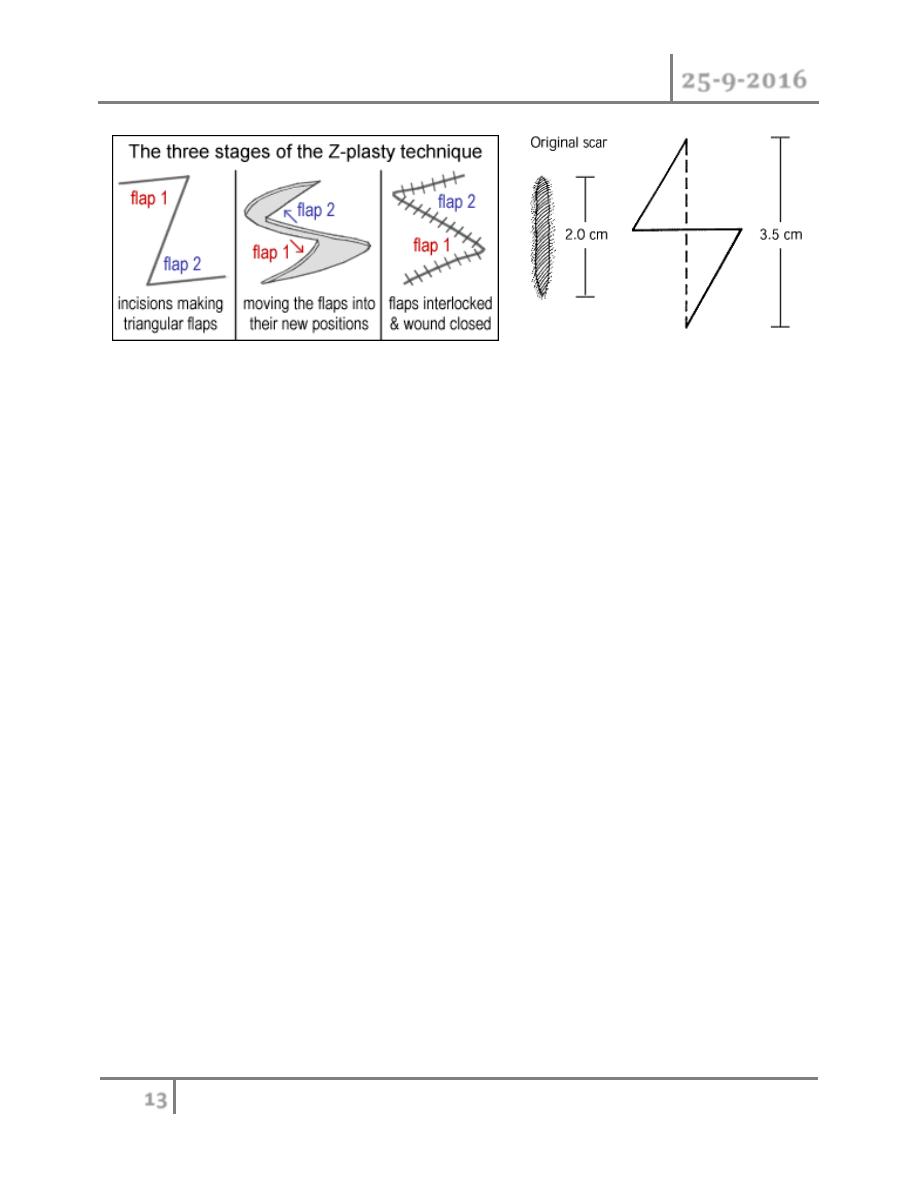
Z-PLASTY:
Is a technique in which two triangular flaps are transposed and interdigitated with each other to
revise and redirect existing scars or to provide additional length in the setting of scar contracture.
Basic Principles Dr. Yasser N. Qassim
25-9-2016
13
©Ali Kareem 2016-2017
#END of this Lecture …
