
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
By: Dr. Sajeda Al-Chalabi
Assist.Proff / Dept .of Physiology
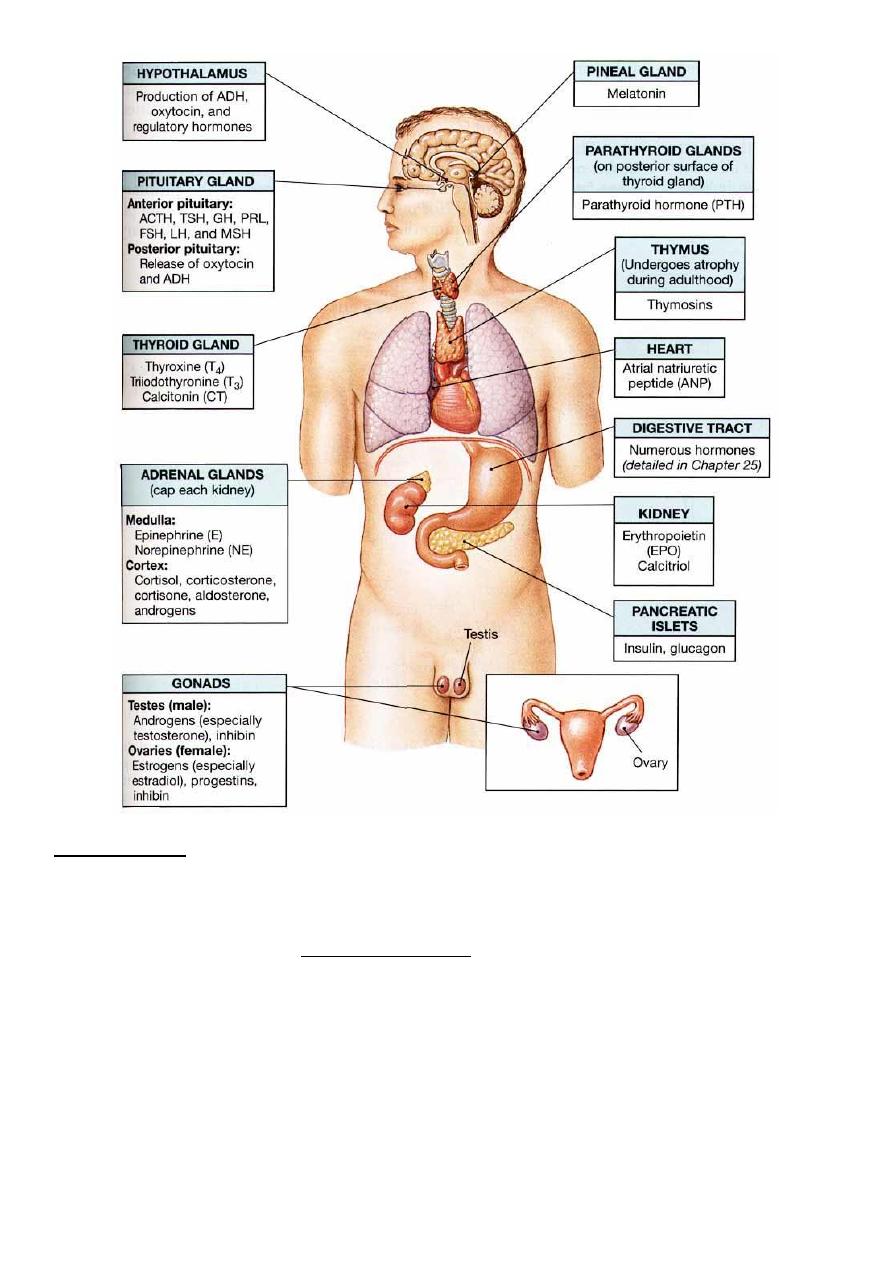
You should now be familiar with:
The major chemical classes and general mechanisms of hormones.
-
-The location and structure of the pituitary gland, and its structural and functional relationships with the
hypothalamus.
-The location and structure of each of the endocrine glands.
-The hormones produced by each of the endocrine glands, and the functions of those hormones.
-The functions of the hormones produced by the kidneys, heart, thymus, testes, ovaries and adipose
tissue.
How hormones interact to produce coordinated physiological responses.
-
What is endocrinology?
Endocrinology = Intercellular Chemical Communication
Endocrinology is about communication systems & information transfer.
What are endocrine systems for?
Endocrine Functions
Maintain Internal Homeostasis
-
-Support Cell Growth
-Coordinate Development
-Coordinate Reproduction
-Facilitate Responses to External Stimuli
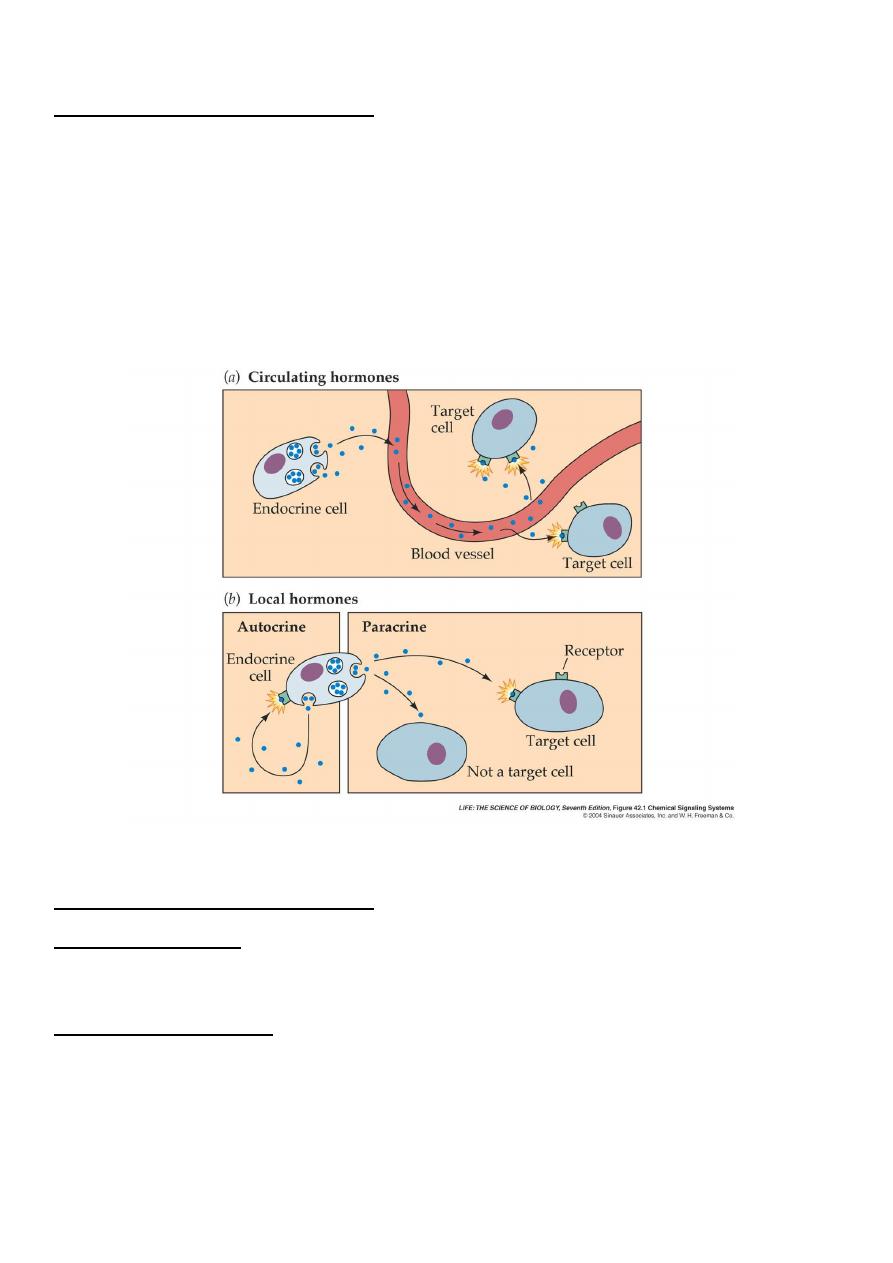
Endocrine: glands or specialized cells release into the circulating blood hormones that influence the
function of cells at another location in the body.
Paracrine: in which cells secrete substances that diffuse into the extra cellular fluid & affect neighboring
cells.
in which a cell secrets substances that affect the function of the same cell by binding to the
:
Autocrine
same surface receptor.
There are three classes of hormones:
Proteins& polypeptides including hormones secreted by the anterior & posterior pituitary gland, insulin
& glucagon ,the parathyroid hormone.
Steroids as cortisol & aldosterone , estrogen, progesterone and testosterone.
Derivatives of the amino acid tyrosine as thyroxine& triiodothyronine, epinephrine &norepinephrine.
Transport of hormones in the blood
) are dissolved in the plasma & transported from
catechol amines
( peptides &
soluble hormones
-
ter
Wa
their sites of synthesis to target tissues where they diffuse out of the capillaries into the interstitial fluid
& then to target cells.
sma proteins. Usually
, circulate in the blood bound to pla
Steroids & thyroid hormones
less than 10 per cent of steroid or thyroid hormones in the plasma exist free in solution. For example,
more than 99 per cent of the thyroxin in the blood is bound to plasma proteins. These can not diffuse
easily across the capillaries ,so they are inactive until they dissociate from plasma proteins .The
relatively large amounts of hormones bound to proteinsb serve as reservoirs, replenishing the

concentration of free hormones when they are bound to target receptors or lost from the circulation.,
binding of hormones to plasma proteins greatly slows their clearance from the plasma.
learance of hormones from blood
C
Two factors can increase or decrease the concentration of a hormone in blood. One of these is the rate of
hormone secretion in blood. The second is the rate of removal of the hormone in blood. which is called
the (metabolic clearance rate= rate of disappearance of hormone from the plasma/ concentration of
hormone in each milliliter of plasma.
Hormones are cleared from the plasma in several ways, including:
-Metabolic destruction by the tissues.
-Binding with the tissues.
-Excretion by the liver .
Excretion by the kidneys..
-
Mechanism of action of hormones
The first step of hormone action is to bind to specific receptors at the target cells.
:
Receptor located
In or on the surface of cell membrane as for protein ,peptide &catecholamine hormones.
-
In the cell cytoplasm as for steroid hormones.
-
In the cell nucleus as for thyroid hormones.
-
After binding with the receptor some change the membrane permeability for ions , some activate
intracellular enzymes ,some activate gens.
-What is hormone receptors?
Hormone Receptors are cellular proteins that bind with high affinity to hormones & are altered in shape
& function by binding; they exist in limited numbers.( Binding to hormone is reversible.)
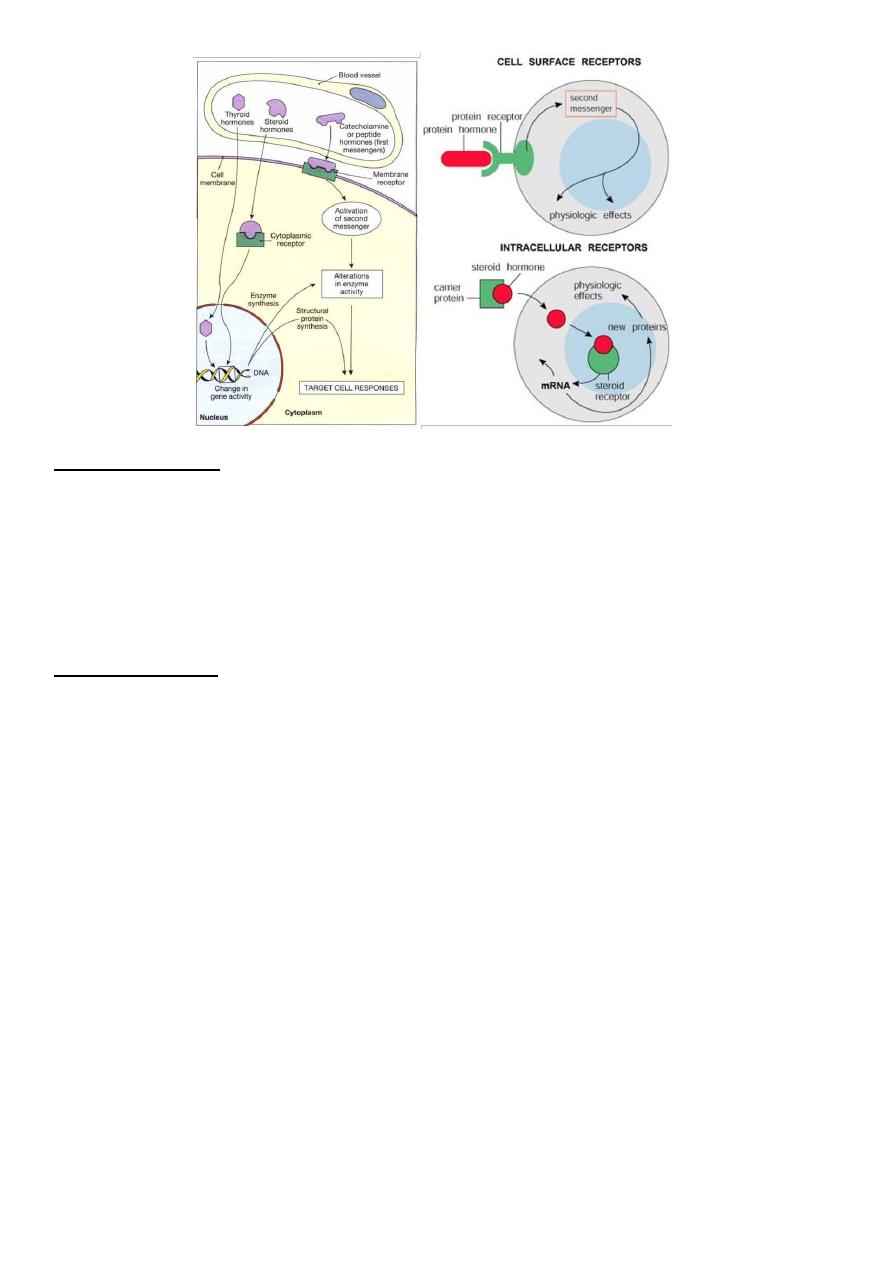
Peptide Hormones
Peptide hormones do not enter the cell directly. These hormones bind to receptor proteins in the cell
membrane.
When the hormone binds with the receptor protein, a secondary messenger molecule initiates the cell
response.
Because peptide hormones are water soluble, they often produce fast responses.
Steroid Hormones
Steroid hormones enter through the cell membrane and bind to receptors inside of the target cell.
These hormones may directly stimulate transcription of genes to make certain proteins.
Because steroids work by triggering gene activity, the response is slower than peptide hormones.
Hypothalamus
It is the portion of the anterior end of the diencephalon, it is divided into a variety of nuclei & nuclear areas
the principal afferent & efferent neural pathways to & from the hypothalamus are mostly unmyelinated .
. An intrahypothalamic system of dopamine
oxytocin& vasopressin
secrete
neurons
Para ventricular
secreting neurons have cell bodies in the accurate nucleus & end on or near the capillaries that form the
portal vessels in the median eminence .
There are neural connections between the hypothalamus & the posterior lobe of the pituitary gland &
vascular connections between the hypothalamus & the anterior lobe .
The major hypothalamic releasing &inhibitory hormones are:
1
.
) which causes release of TSH.
TRH
(
releasing hormone
-
Thyrotropin
2
.
) which causes release of adrenocorticotropin.
CRH
(
releasing hormone
-
Corticotropin
3
.
one inhibitory
growth horm
) causes release of GH &
GHRH
(
Growth hormone releasing hormone
ostatin which inhibits release of GH.
also called somat
GHIH)
(
hormone
4
.
) causes release of FSH &LH
GNRH
(
releasing hormone
–
Gonadotropin
5
.
) inhibits PRL secretion.
PIH
(
Prolactin inhibitory hormone
All or most of hypothalamic hormones are secreted at nerve endings in the median eminence before being
transported to the anterior pituitary gland
.
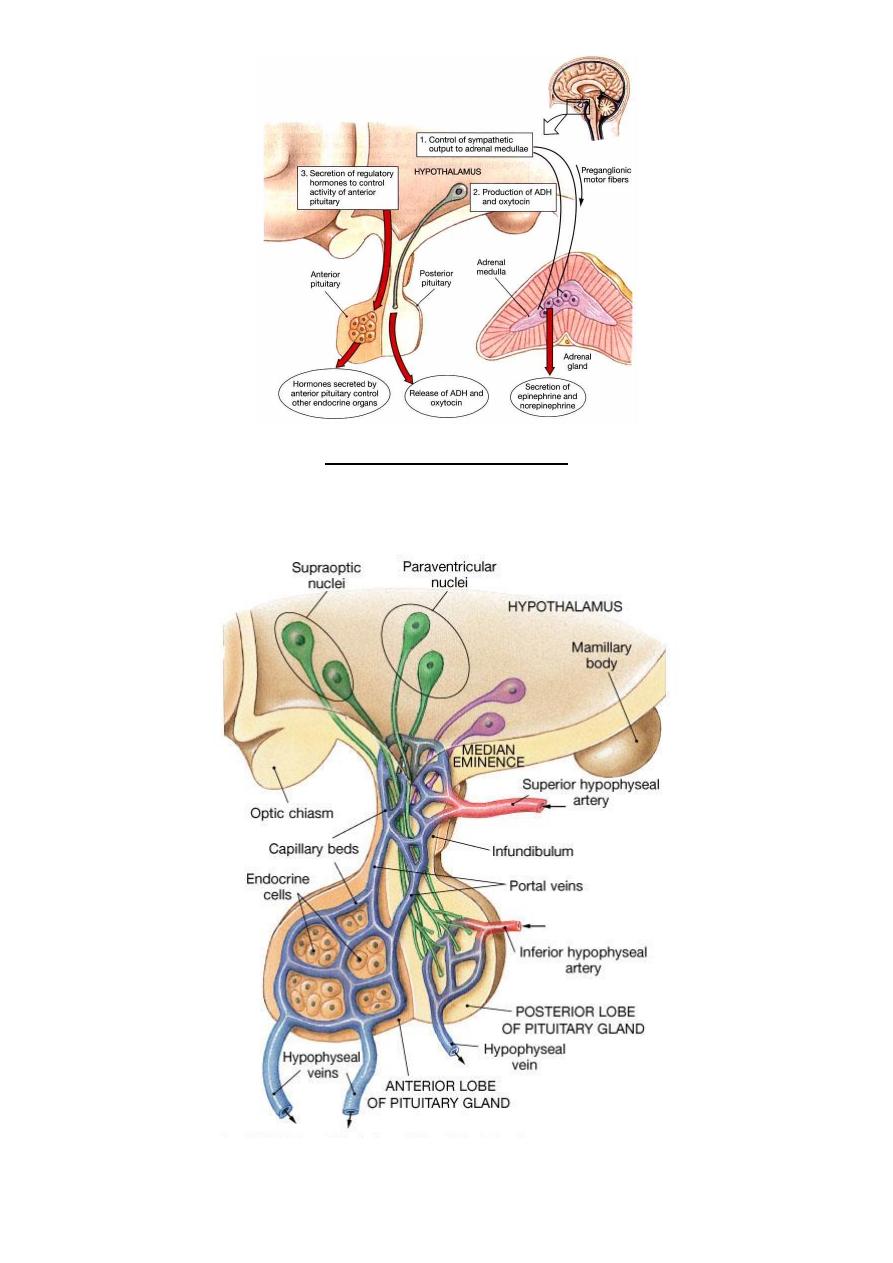
Hypophyseal portal system
All blood entering the portal system will reach the intended target cells before returning
to the general circulation
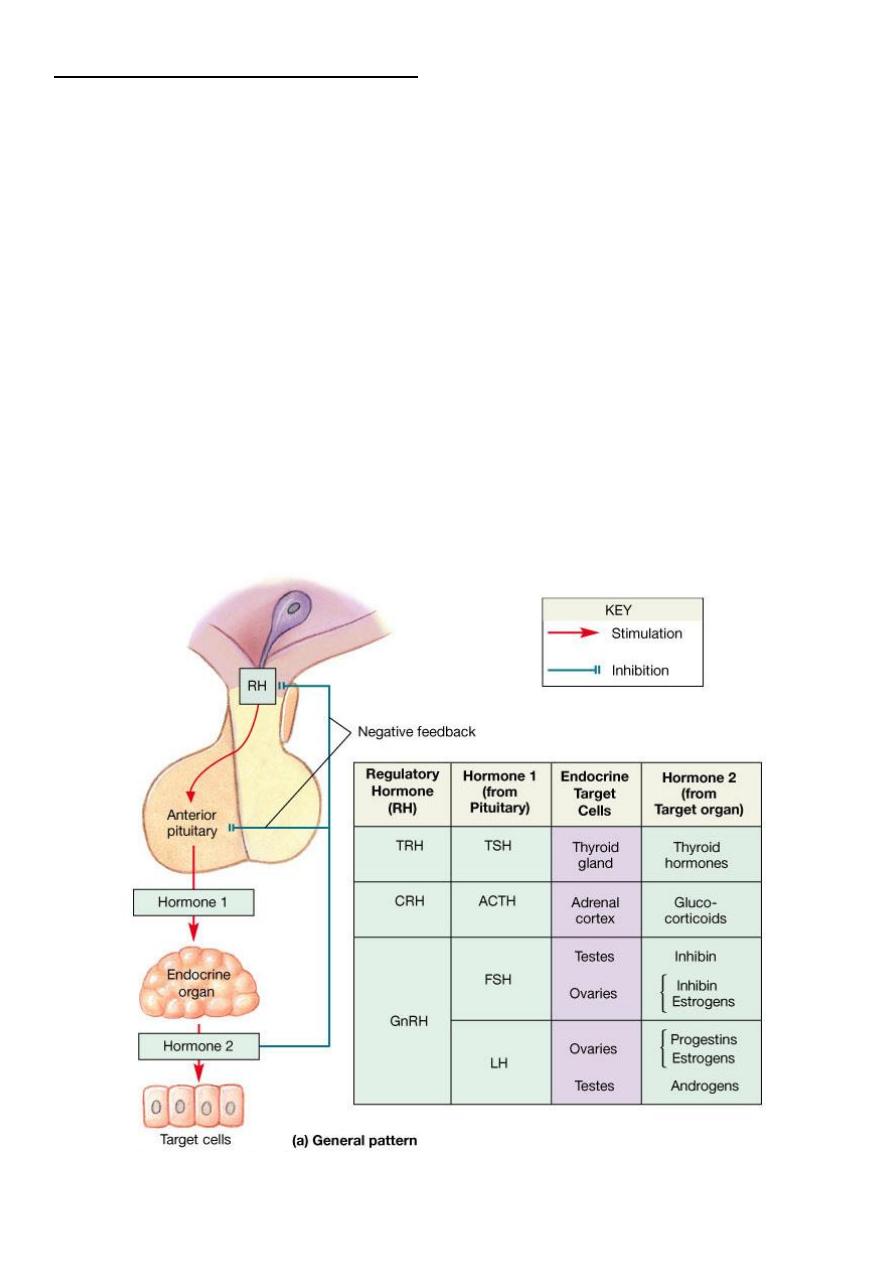
Hormone Secretion
Feedback Control of
Negative Feedback Prevents Over activity of Hormone Systems.
Although the plasma concentrations of many hormones fluctuate in response to various stimuli that occur
throughout the day, all hormones studied thus far appear to be closely controlled. In most instances, this
control is exerted through negative feedback mechanisms that ensure a proper level of hormone activity at
the target tissue. After a stimulus causes release of the hormone, conditions or products resulting from the
action of the hormone tend to suppress its further release. In other words, the hormone (or one of its
products) has a negative feedback effect to prevent over secretion of the hormone or over activity at the
target tissue.
Surges of Hormones Can Occur with Positive Feedback
. In a few instances, positive feedback occurs when the biological
action of the hormone causes additional secretion of the hormone. One example of this is the surge of
luteinizing hormone (LH) that occurs as a result of the stimulatory effect of estrogen on the anterior
pituitary before ovulation. The secreted LH then acts on the ovaries to stimulate additional secretion of
estrogen, which in turn causes more secretion of LH. Eventually, LH reaches an appropriate concentration,
and typical negative feedback control of hormone secretion is then exerted
.
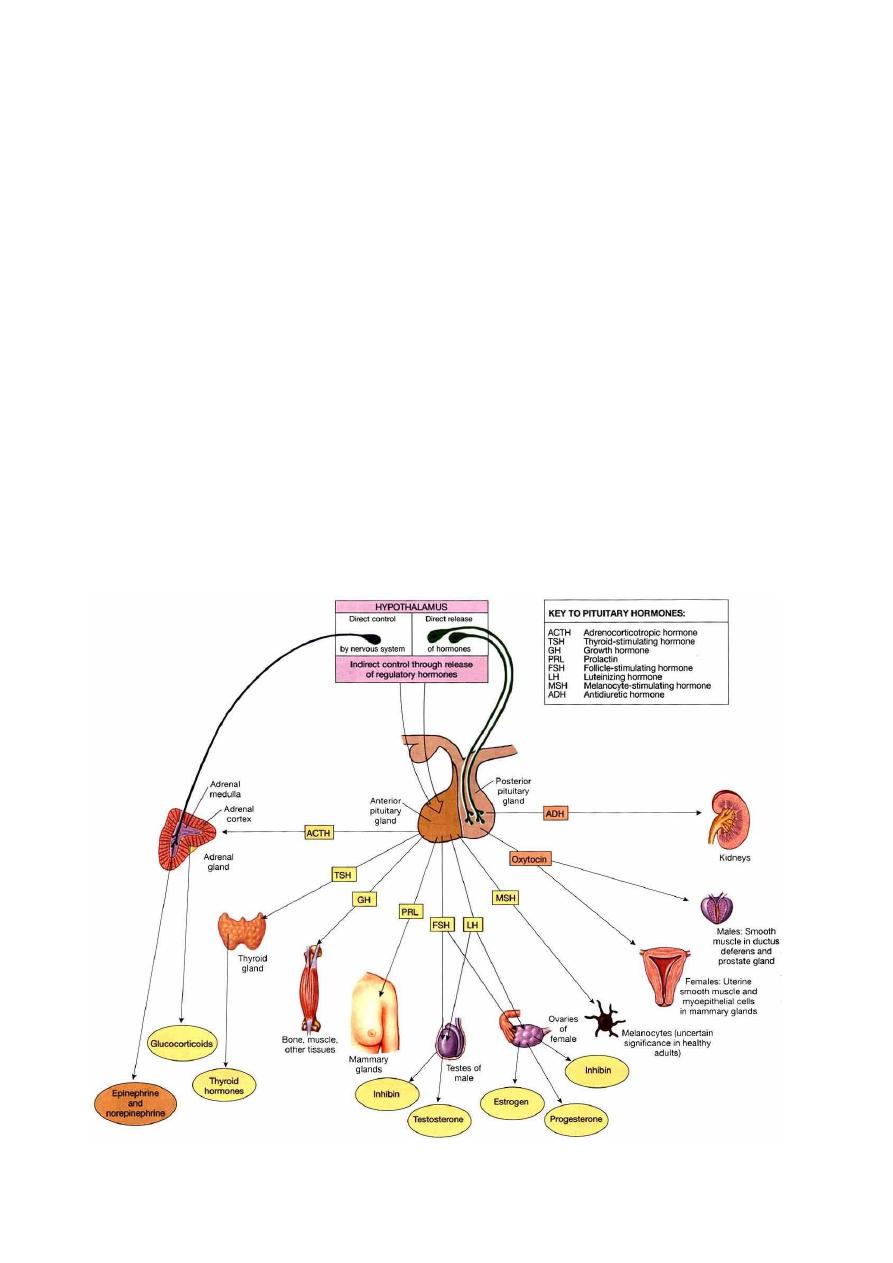
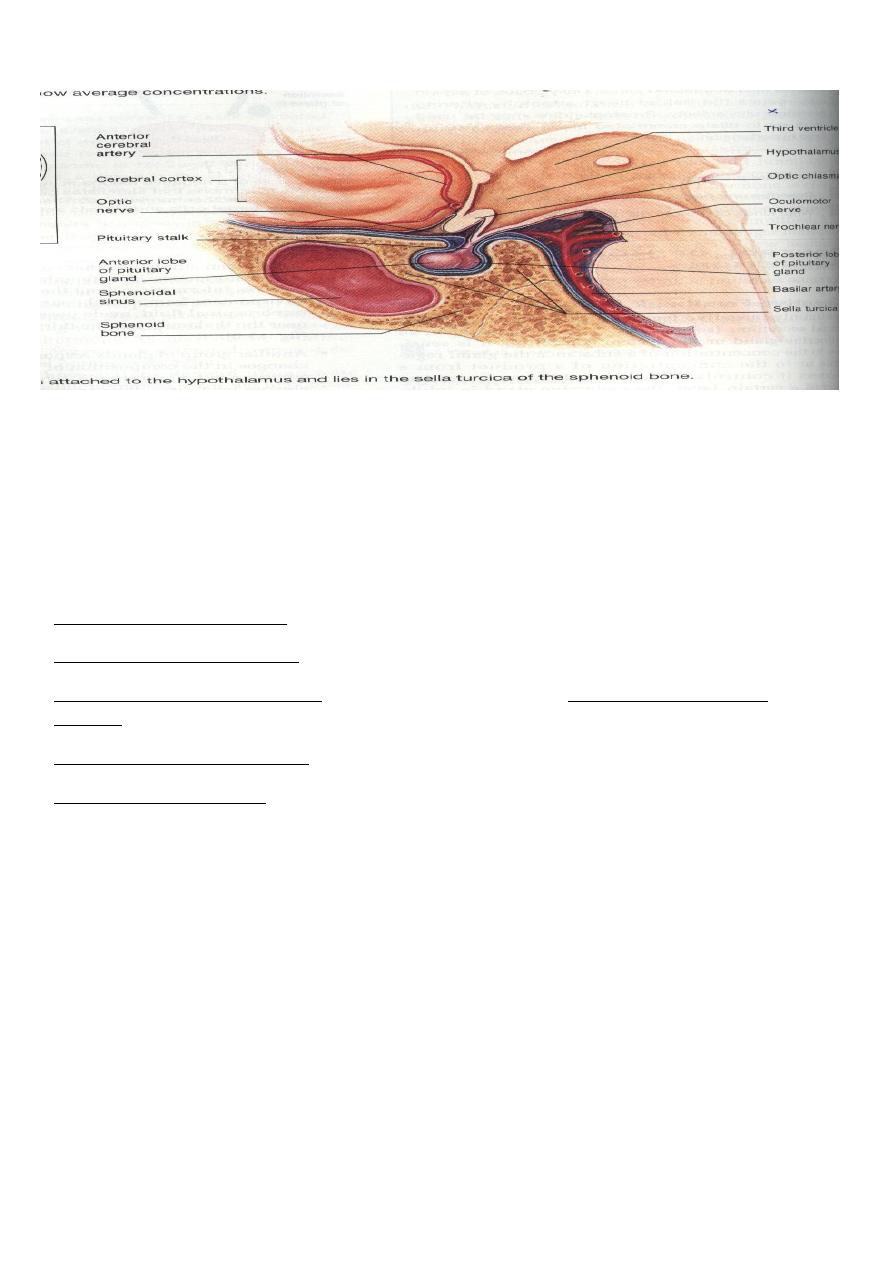
The pituitary gland
called the hypophysis, is a small gland—about 1 centimeter in diameter and 0.5 to 1 gram in weight—
that lies in the sella turcica, a bony cavity at the base of the brain, and is connected to the hypothalamus
by the pituitary (or hypophysial) stalk. Physiologically, the pituitary gland is divisible into two distinct
portions: the anterior pituitary, also known as the adenohypophysis, and the posterior pituitary, also
known as the neurohypophysis
The anterior pituitary secrets six hormones : growth hormone (GH), adrenocorticotropin (ACTH) ,
thyroid stimulating hormone (TSH) , luteinizing hormone (LH) , follicle stimulating hormone (FSH) ,
prolactin (PRL) .
There are five cell types in the anterior pituitary:
-
Somatotropes---human growth hormone.
-Corticotropes----ACTH.
-Gonadotropes—FSH&LH.
-Thyrotropes------TSH.
-Lactotropes------PRL
.
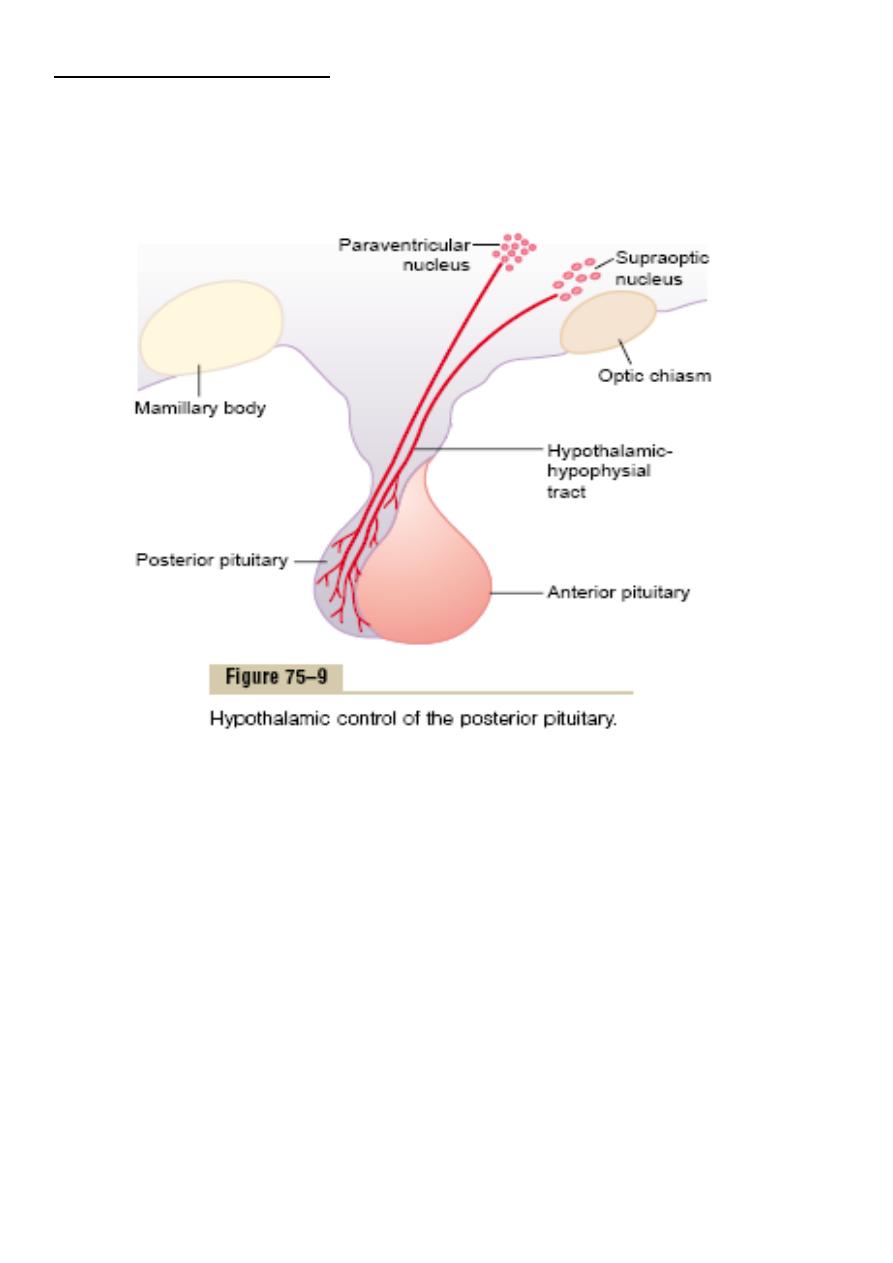
Its also called the neurohypophysis or pars nervosa, contains the
The Posterior Pituitary Gland
axones of some hypothalamic neurons. Neurons within the supraoptic & paraventricular nuclei
manufacture :
-
Antidiuretic hormone (ADH) also called vasopressin
- Oxytocin
The posterior pituitary is made up of the endings of the axons that arise from the cell bodies in the
supraoptic & the paraventricular nuclei & pass to the posterior pituitary via the hypothalamo-hypophysial
tract , the portal hypophysial vessels form a direct vascular link between the hypothalamus & the anterior
pituitary.
The hormones of the posterior pituitary gland , oxytocin & vasopressin are nonapeptides synthesized in the
cell bodies of the magnocellular neurons in the supraoptic & paraventricular nuclei & transported down the
axons of these neurons to their endings in the posterior lobe, where they are secreted in response to the
electrical activity in the endings.
Vasopressin secreting neurons are found in the suprachiasmatic nuclei , & vasopressin & oxytocin are also
found in the endings of neurons that project from the paraventricular nuclei to the brain stem & the spinal
cord . These neurons appears to be involved in the cardiovascular control
Chemical structures ADH and oxytocin
Both oxytocin and ADH are polypeptides , each containing nine amino acids. These two hormones are
almost identical except that in vasopressin, phenylalanine and arginine replace isolucine and leucine of the
oxytocin molecule .
Ejection of milk (function of oxytocin)
When baby suckles the breast , nerve signals transmitted to the spinal cord & then to the hypothalamus
cause oxytocin secretion which result in contraction of myoepithelial cells surrounding the alveoli &
ejection of milk . Generalized sympathetic stimulation inhibit oxytocin secretion & milk ejection .
oxytocin causes contraction of smooth muscle of the uterus. The sensitivity of uterine
:
r actions
Othe
musculature to oxytocin is enhanced by estrogen & inhibited by progesterone , the inhibitory effect of
progesterone is through direct effect on oxytocin receptors in the uterus . Oxytocin may also act on non-
pregnant uterus to facilitate sperm transport .
Circulating oxytocin is increased at time of ejaculation in males & it is possible that this increase causes
increased contraction of smooth muscle of the vas deferens , propelling the sperm toward the urethra.
Physiologic functions of ADH
ADH decrease the excretion of water by the kidneys.
1.In the absence of ADH , the collecting tubules and ducts become almost impermeable to water , which
prevents significant reabsorption of water and therefore allows extreme loss of water into the urine and
causes dilution of urine .
2.In the presence of ADH , the permeability of collecting ducts and tubules to water increases greatly and
allows most of the water to be re absorbed as the tubular fluid passes through these ducts , thereby
conserving water in the body and producing very concentrated urine. .
Regulation of ADH Production
1. Osmotic regulation
Somewhere in or near the hypothalamus are modified neuron receptors called osmoreceptors . When the
extracellular fluid becomes too concentrated , fluid is pulled by osmosis out of the osmoreceptor cell ,
decreasing its size and initiating nerve signals in the hypothalamus to cause ADH secretion . Conversely ,
when the extra cellular fluid becomes too dilute , water moves by osmosis in the opposite direction into the
cell & this decreases signal for ADH secretion.
So concentrated body fluid stimulate the supraoptic nuclei , whereas dilute body fluids inhibit them .
Higher concentrations of ADH have a potent effect of vasoconstricting the arterioles throughout the body ,
therefore increasing the arterial pressure . For this reason it is also called vasopressin .
2. One of the stimuli for causing ADH secretion is decreased blood volume , this occurs especially when
the blood volume decreases 15-25 % , the secretory rate then sometimes rises to as high as 50 times normal .
3. The atria especially the right atrium have stretch receptors that are excited by overfilling , they signals to
the brain to inhibit ADH secretion .
4. Decreased stretch of baroreceptors of the carotid , aortic & pulmonary regions , increases ADH
secretion
Growth Hormone (Somatotropin)
Most abundant pituitary hormone
Growth hormone is a 191-
, single-chain
that is synthesized, stored, and secreted
Structurally similar to prolactin. and chorionic somatomammotropin
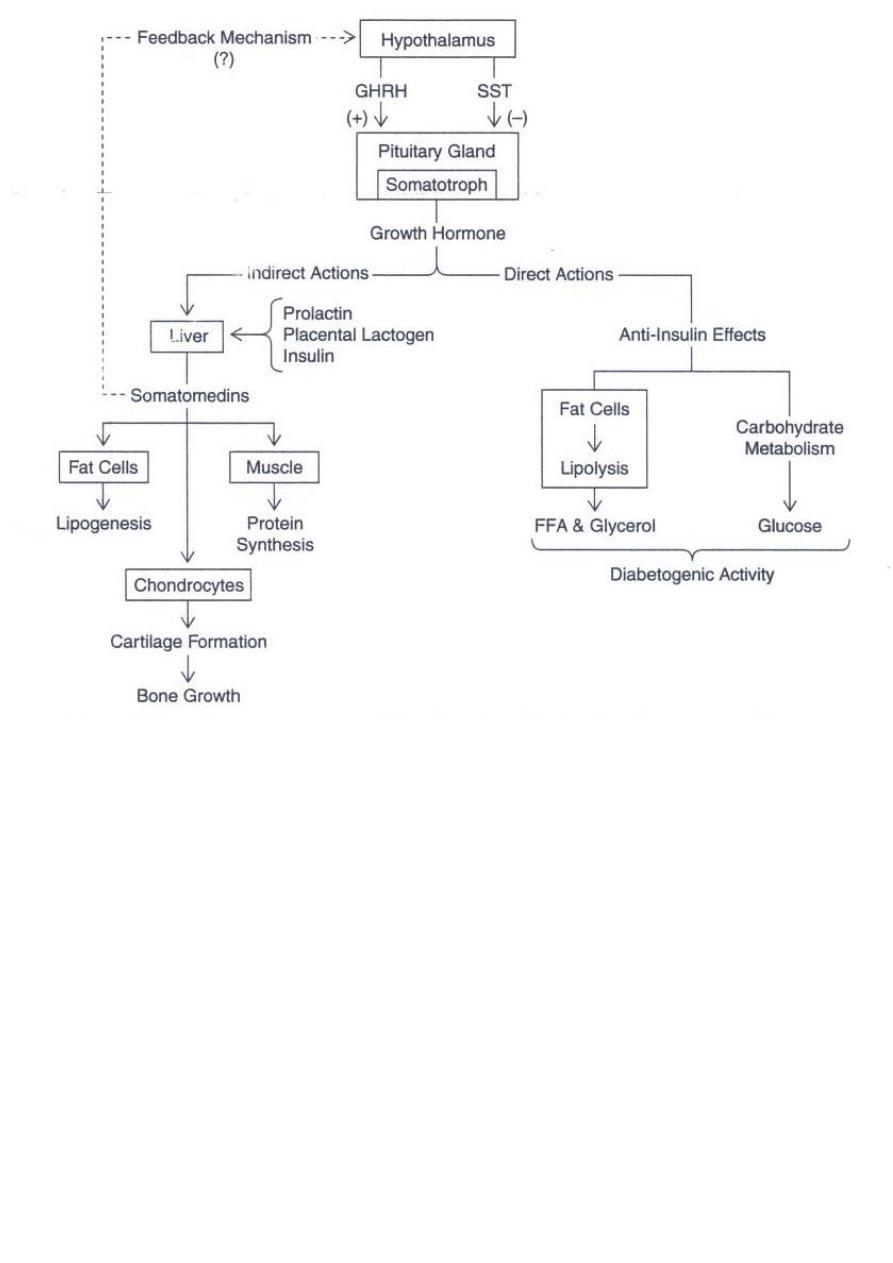
Metabolic effects
: (1) increased rate of protein synthesis in most cells of the body
(2) increased mobilization of fatty acids from adipose tissue,
increased free fatty acids in blood, & increased use of fatty acids for energy.
(3) decreased rate of glucose utilization throughout the body.
Thus, in effect, growth hormone enhances body protein, uses up fat stores, and conserves carbohydrates.
Growth Hormone: Physiologic Effects
Promotes Growth
Increases cell number in organs
Skeletal growth
Cartilage formation
Collagen biosynthesis (epiphysal plates)
Muscle cell growth
Growth Hormone Action Most functions via somatomedins
that have the potent effect of increasing all aspects of bone growth. Many of thesomatomedin effects on
growth are similar to the effects of insulin on growth. Therefore, the somatomedins
are also called insulin-like growth factors(IGFs)
.
Regulation of Growth Hormone Secretion
The secretion of GH is not stable over time .
Adolescents have the highest level of circulating GH , followed by children,& finally adults .levels decline
in old age.
Growth hormone is secreted in a pulsatile pattern, increasing & decreasing.
several factors related to a person’s
state of nutrition or stress are known to stimulate
secretion: (1) starvation, especially with severe protein
deficiency; (2) hypoglycemia or low concentration of
fatty acids in the blood; (3) exercise; (4) excitement; and
(5) trauma.
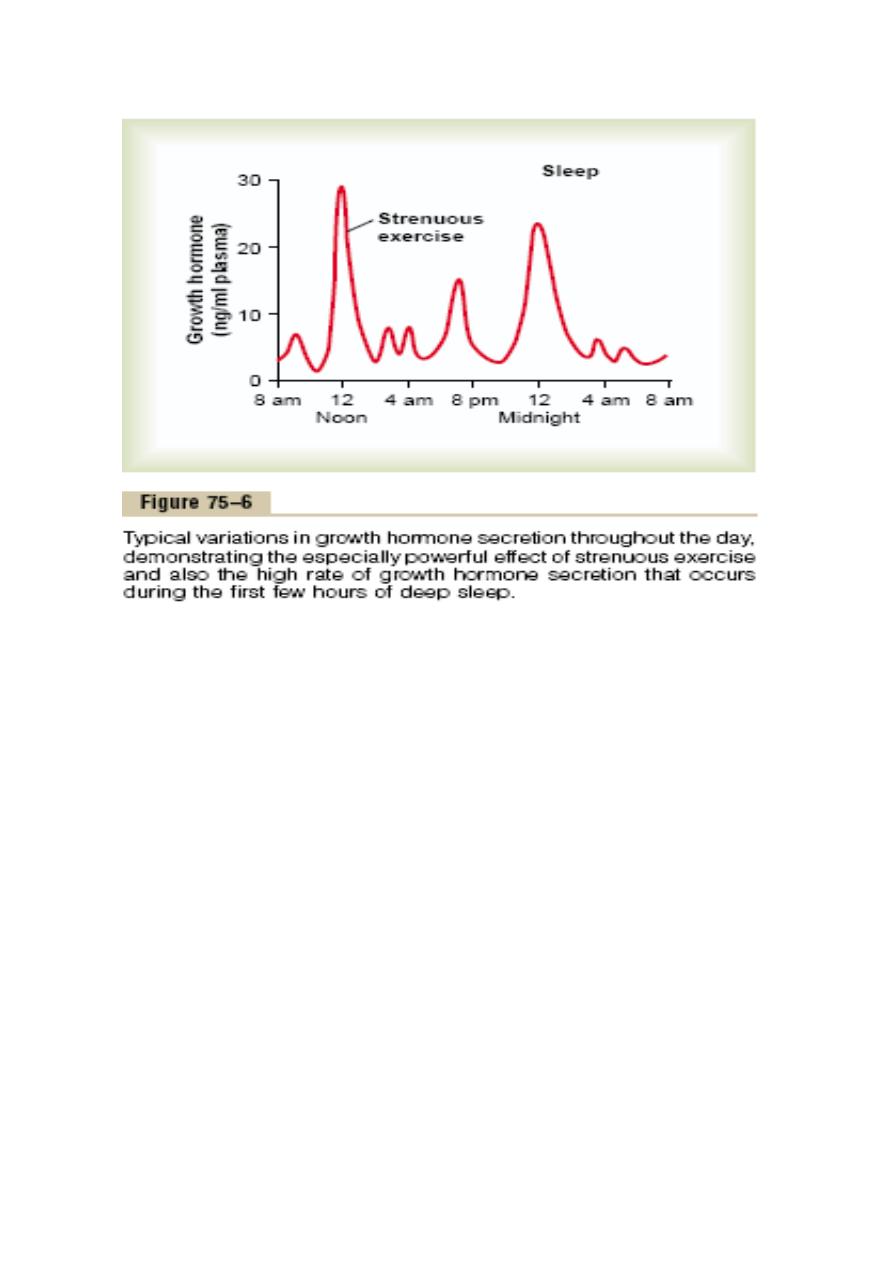
Growth hormone also characteristically increases during the first 2 hours of deep sleep, as shown in the
figure.
Control of Growth Hormone Secretion
Growth hormone secretion is controlled by two factors secreted in the hypothalamus and
then transported tothe anterior pituitary gland through the hypothalamic hypophysial
portal vessels
1.growthhormone–releasing hormone (GHRH)
2.growth hormone inhibitory hormone (also called somatostatin)
Most of the control of growth hormone secretion is probably mediated through GHRH
rather thanthrough the inhibitory hormone somatostatin.
Abnormalities of Growth Hormone Secretion
Gigantism Over-secretion of growth hormone prior to puberty.
-Excessive growth of long bones
-Treatment: drug therapy to inhibit GH release

Acromegaly
-Over-secretion of growth hormone during adulthood
usually from tumor
-
-Enlargement of the extremities and/or face
Treatment: drug therapy to inhibit GH release
-
Dwarfism
Most instances of dwarfism result from generalized deficiency of anterior
pituitarysecretion(panhypopituitarism)during childhood.
A person with panhypopituitary dwarfism does notpass through puberty and never secretes sufficient
quantities of gonadotropic hormones to develop adult sexual functions.
In one third of such dwarfs, however,
Only growth hormone is deficient; these persons do mature sexually and occasionally reproduce.
Prolactin
-Structure similar to GH
-Glycoprotein hormone
-Synthesized and stored in lactotrophs
-Principally responsible for lactation
-Effects on gonads- species specific
-Concentration increases 20 –40x during pregnancy
-Mechanism of action- binds to cell surface receptors
Physiological Effects of Prolactin
-Growth and development of breasts during pregnancy
-Maintains lactation (in presence of estrogens, progesterone, insulin and corticosteroids)
-Blocks effects of FSH and LH; initially prevents lactation
Edited by Mohammed Awchi
