Psoriasis (cont.)and otherPapulosquamous Diseases
ByDr. Omar Y. Abdullah
MSc in Clinical Dermatology
Treatment of psoriasis
Many topical and systemic agents are available.None of the topical medications is predictably effective.
All topicals require lengthy treatment to give relief that is often temporary.
Compliance is a problem, patients become discouraged with moderately effective and expensive topical treatment that lasts weeks or months.
Limited disease (<20% body surface area) can be managed with topical therapy only.
Determining the degree of inflammation
The most common form of psoriasis is the localized chronic plaque disease involving the skin and scalp.It must be determined whether the plaque is inflamed before instituting therapy.
Red, sore plaques can be irritated by tar, calcipotriol, and anthralin. Irritation can induce further activity.
Inflammation should be suppressed with topical steroids and/or antibiotics before initiating other treatments.
Determining the end of treatment
The plaque is effectively treated when induration has disappeared.
Residual erythema, hypopigmentation, or brown hyperpigmentation is common when the plaque clears.Patients frequently mistake the residual color for disease and continue treatment.
If the plaque cannot be felt by drawing the finger over the skin surface, treatment may be stopped.
Stress control
A study demonstrated a positive correlation between the severity of psoriatic symptoms and psychologic distress.Stress reduction techniques may be appropriate for certain patients.
Topical steroids
Rapid response. Control inflammation and itching. Best for intertriginous areas and face. Convenient, and not messy.Temporary relief. Tolerance occurs. Brief remissions. Expensive.
Best results occur with pulse dosing (e.g., 2 weeks of medication and 1 week of lubrication only).
Plastic occlusion is very effective but not used in intertriginous areas and not with superpotent steroids.
S.E.?
Patients with a few, small, chronic psoriatic plaques of the scalp or body can be effectively treated with a single or few intralesional injection of triamcinolone acetonide. Remissions are long. The face and intertriginous areas are avoided here.
Calcipotriene (Dovonex cream) 0.005%
Is a vitamin D3 analogue
Inhibits epidermal cell proliferation and enhances cell differentiation.
Well tolerated. Long remissions possible.
Burning, skin irritation, expensive.
Valuable for long-term scalp treatment programs (Dovonex scalp solution).
Not more than 100g per week is used
Newer combination product (Dovobet) is more effective (calcipotriene hydrate plus betamethasone dipropionate).
Hypercalcemia can occur.
Ultraviolet light B
Wave length = (290-320nm)The most effective topical programs use UVB in combination with lubricating agents, tar, or tazarotene.
Also, the combination of UVB phototherapy with systemic agents can be very effective.
Combining methotrexate (or acitretin) and UVB results in clearing of extensive psoriasis and reduces the cumulative dose (and thus toxicity) of both.
Treatment with narrow-band UVB (311 nm) is superior to treatment with broadband UVB.
UVB is the treatment of choice in guttate psoriasis.
Photochemotherapy
Also called PUVA because of the use of psoralens (P) (photosensitizers), along with exposure to long-wave ultraviolet light (UVAI 340-400).PUVA can control severe psoriasis with relatively few maintenance sessions, and can be done on an outpatient basis.
PUVA is indicated for the symptomatic control of severe, recalcitrant, and disabling plaque psoriasis that is not responsive to other forms of therapy.
Pustular psoriasis of the palms and soles responds best to PUVA-acitretin.
Psoriatic arthropathy (nonspondylitic) may respond to PUVA.
Because of the concerns about long-term toxicity, PUVA is most appropriate for severe psoriasis in patients older than 50 years of age.
Light does not penetrate hair
PUVA Side effects
Long term side effects (most of which are dose-dependant):
Skin tumors.PUVA promotes skin aging, actinic keratoses, and squamous cell
carcinoma (SCC).
Risk of genital tumors in males with exposure to PUVA and UVB.
Approximately 15 years after the first treatment with PUVA, the risk of
malignant melanoma increases, especially among patients who receive
250 treatments or more.
Lentigines. Small black macules occur in PUVA-exposed sites.
Cataracts. The incidence seems to be very low if eye protection is used during the first two days of PUVA treatment (from the time the drug is ingested until the end of the following day).
Short-term side effects include dark tanning, pruritus, nausea, and severe sunburn.
Treatment of scalp psoriasisScale must be removed first to facilitate penetration of medicine.
Superficial, thin scale can be removed with shampoos that contain tar and salicylic acid (e.g., T/Gel).
Thicker scale is removed by massaging the scalp with 10% liquor carbonis detergens (LCD) in Nivea oil and washing the scalp 6 to 8 hours later with shampoo. Combing during washing helps dislodge scale. Nightly applications are continued until the scalp is acceptably clear.
Treating scalp psoriatic lesions:
Steroid gels (e.g., fluocinonide gel, clobetasol gel).
Betamethasone foam and clobetasol foam are also effective.
Small plaques are treated with intralesional injections of triamcinolone acetonide.
Ketoconazole cream is sometimes useful. Oral ketoconazole (400 mg daily) may be effective.
Dovobet is a topical suspension for the treatment of moderate-to-severe psoriasis of the scalp in adults.
10% LCD in Nivea oil applied to the scalp, covered with a shower cap and washed out each morning, removes scale and suppresses inflammation.
Treatment of psoriatic arthritis
Non-steroidal anti-inflammatory drugs
Intra-articular steroid injections
Methotrexate
Biologics
Cyclosporine
PUVA
Systemic treatment of psoriasis
IndicationsModerate-to-severe psoriasis (20% or more involvement of body surface area).
Patient is unresponsive to topical therapy.
A number of systemic drugs are available, some of which have potentially serious side effects.
Methotrexate is highly effective, relatively safe, and well-tolerated
Photochemotherapy (PUVA) is effective and relatively safe.
Acitretin is used to potentiate the effects of PUVA and as a monotherapy for plaque, pustular, and erythrodermic forms of psoriasis.Cyclosporine is rapidly effective, but long-term use may be associated with loss of kidney function.
Biologic drugs (eg., adalimumab and etanercept) are safe and effective and are rapidly becoming the preferred systemic therapy for psoriasis. Very expensive.
PITYRIASIS ROSEA
Pityriasis rosea (PR) is a common, benign, usually asymptomatic, distinctive, self-limiting skin eruption of unknown etiology.There is some evidence that human herpesvirus 6 (HHV-6) and 7 (HHV-7) may be involved.
More than 75% of cases occur between 10 and 35 years of age with an age range of 4 months to 78 years.
Recurrence rate is about 2%.
The incidence is higher during winter time.
Upper respiratory tract infection occurs before the eruption in about 70% of cases.
CLINICAL MANIFESTATIONS
Typically, the herald patch, a single 2- to 10-cm round-to-oval lesion, abruptly appears in 17% of patients. May occur anywhere, but is most frequently located on the trunk or proximal extremities.
Within a few days to several weeks the disease enters the eruptive phase and reach its maximum in 1 to 2 weeks.
Lesions are typically limited to the trunk (lower trunk) and proximal extremities, but any area could be affected
Individual lesions are salmon pink in whites and hyperpigmented in blacks.
Typically 1- to 2-cm oval plaques appear, a fine, wrinkled, tissue-like scale remains attached within the border of the plaque, giving the characteristic ring of scale, called collarette scale.
The long axis of the oval plaques is oriented along skin lines. Numerous lesions on the back, oriented along skin lines, give the appearance of drooping pine-tree branches, which explains the designation “Christmas-tree distribution.”
The number of lesions varies from a few to hundreds.
Differential diagnosis
Secondary syphilisGuttate psoriasis
Viral exanthems
Tinea corporis
Nummular eczema
Drug eruptions
Management of PR
Whether or not PR is contagious is unknown.The disease is benign and self-limited and can resolve spontaneously.
Oral erythromycin 250 mg 4 times daily for 2 weeks.
Group V topical steroids (eg., fluticasone propionate cream 0.05%) and oral antihistamines may be used as needed for itching.
UVB phototherapy five times per week for 2 weeks.
Oral acyclovir (800 mg five times daily for 1 week).
Lichen Planus
Lichen planus (LP) is a unique inflammatory cutaneous and mucous membrane reaction pattern of unknown etiology.The disease may occur at any age, it is rare in children younger than 5 years. The mean age of onset is 40 years in males and 46 years in females.
The main eruption clears within 1 year in about 70% of patients, but 50% of eruptions recur.
Approximately 10% of patients have a positive family history.
Cutaneous and oral LP may be associated with hepatitis C virus (HCV)-related, chronic, active hepatitis.
Various patterns of lichen planus
Most common site
Actinic
Sun-exposed areas
Annular
Trunk, external genitalia
Atrophic
Any area
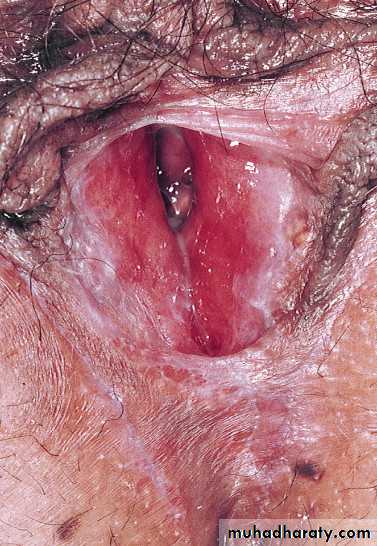
Erosioulcerative
Soles of feet, mouth
Follicular (lichen planopilaris)
Scalp
Guttate (numerous) small papules
Trunk
Hypertrophic
Lower limbs (especially ankles)
Linear
Zosteriform (leg), scratched area
Nail disease
Fingernails
Papular (localized)
Flexor surface (wrists and forearms)
Vesiculobullous
Lower limbs, mouth
Eruptions from drugs (e.g., gold, chloroquine, methyldopa, penicillamine), chemical exposure (film processing), bacterial infections (secondary syphilis), and post–bone marrow transplants (graft-versus-host reaction) that have a similar appearance are referred to as lichenoid.
PRIMARY LESIONS
Th five Ps rule of lichen planus: pruritic, planar (flat-topped), polyangular, purple papules.The primary lesion is a <1cm flat-topped papule with an irregular angulated border (polygonal papules).
Close inspection of the surface shows a lacy, reticular pattern of crisscrossed, whitish lines (Wickham’s striae) that can be accentuated by a drop of immersion oil.
Papules aggregate into different patterns, they may also Koebnerize.
Many patients have persistent brown staining many years after the rash has cleared.
Localized LP
Papules are most commonly located on the flexor surfaces of the wrists and forearms, the legs immediately above the ankles and the lumbar region.Itching is variable; 20% of patients with LP do not itch. Itch does not necessarily correlate with disease severity.
The course is unpredictable. Some patients experience spontaneous remission in a few months, but the most common localized papular form tends to be chronic and endures for an average of approximately 4 years.
Treatment
THERAPY FOR CUTANEOUS LICHEN PLANUSTopical steroids
Intralesional steroids
Systemic steroids
Acitretin
Azathioprine
Cyclosporine
Antihistamines
Light therapy
PUVA (psoralen + UVA light) and broadband and narrow-band UVB therapy.
Tacrolimus ointment: Ulcerative lichen planus of the sole may respond to topical tacrolimus 0.1% ointment.
THERAPY FOR MUCOUS MEMBRANE LICHEN PLANUS
The course of oral and vaginal lichen planus can extend for years.
Consider a biopsy to establish the diagnosis.
Most patients are asymptomatic (non-erosive type) and do not need treatment.
Tacrolimus ointment and pimecrolimus cream.
Corticosteroids (topical, systemic and intralesional)
Dapsone
Hydroxychloroquine
Azathioprine
Mycophenolate mofetil