Surgical aids to orthodontics
Dr. Wafaa KhalilExtraction of :healthy normal fully erupted teeth
Unerupted, semierupted, misplaced, superneumerary teeth, dilacerated and submerged teethPersistant abnormal labial frenum
Surgical aids to orthodontics
Tooth Impaction
• Third Molars – Most common• Maxillary Cuspids
• Maxillary Central Incisors
• Mandibular/Maxillary second premolar
Impacted Canines
Impacted maxillary canines are quite common, and approximately 12%–15% of the population present with impacted canines. They are localized palatally more often than labially.Even though positions vary, the impacted canine presents five basic localizations (contralateral or ipsilateral and deep in the bone) as follows:
1. Palatal localization
2. Palatal localization of crown and labial localization of root
3. Labial localization of crown and palatal localization of root
4. Labial localization
5. Ectopic positions
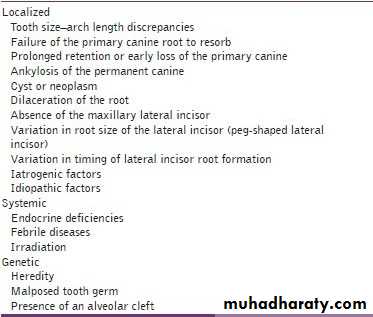
Etiology of impacted canine
Several etiologic factors for canine impactions have been proposed: localized, systemic, or geneticSequelae of Canine Impaction
• Labial or lingual malpositioning of the impacted tooth,• Migration of the neighboring teeth and loss of arch length,
• Internal resorption,
• Dentigerous cyst formation,
• External root resorption of the impacted tooth, as well as the neighboring teeth,
• Periodontal defects,
• Tooth transposition,
• Infection particularly with partial eruption, and
• Referred pain and combinations of the above sequelae.
• Pre-Surgical Preparation
Diagnosis of Canine Impaction
The diagnosis of canine impaction is based on both clinical and radiographic examinations.Clinical Evaluation
• Delayed eruption of the permanent canine or prolonged retention of the deciduous canine beyond 14–15 years of age,
• Absence of a normal labial canine bulge,
• Presence of a palatal bulge in the canine region,
• Delayed eruption, distal tipping, or migration (splaying) of the permanent lateral incisor, and
• Loss of vitality and increased mobility of the permanent incisors
Radiographic Evaluation
Periapical filmsA single periapical film provides the clinician with a two-dimensional representation of the dentition. It would relate the canine to the neighboring teeth both mesiodistally and superoinferiorly. To evaluate the position of the canine buccolingually, a second periapical film should be obtained by one of the following methods.
Tube-shift technique or Clark's rule or (SLOB) rule
Two periapical films are taken of the same area, with the horizontal angulation of the cone changed when the second film is taken. If the object in question moves in the same direction as the cone, it is lingually positioned. If the object moves in the opposite direction, it is situated closer to the source of radiation and is therefore buccally located.
Occlusal films
Also help to determine the buccolingual position of the impacted canine in conjunction with the periapical films, provided that the image of the impacted canine is not superimposed on the other teeth.Extraoral films
Frontal and lateral cephalograms
These can sometimes aid in the determination of the position of the impacted canine, particularly its relationship to other facial structures (e.g., the maxillary sinus and the floor of the nose).
Panoramic films
These are also used to localize impacted teeth in all three planes of space, as much the same as with two periapical films in the tube-shift method, with the understanding that the source of radiation comes from behind the patient; thus, the movements are reversed for position. *(image size distortion; object further away from the image receptor (film) will be depiceted more magnified than objects closer to the film
CT/CBCT
Clinicians can localize canines by using advanced three-dimensional imaging techniques. Cone beam computed tomography (CBCT) can identify and locate the position of impacted canines accurately.
By using this imaging technique, dentists also can assess any damage to the roots of adjacent teeth and the amount of bone surrounding each tooth. However, increased cost, time, radiation exposure, and medicolegal issues associated with using CBCT limit its routine use.
Treatment options
1- Leave insitu2- Surgical extraction
3- Surgical exposure with orthodontic tratment
4- Autotransplantation
When to Extract an Impacted Canine
If it is ankylosed and cannot be transplanted,If it is undergoing external or internal root resorption,
If its root is severely dilacerated,
If the impaction is severe (e.g., the canine is lodged between the roots of the central and lateral incisors and orthodontic movement will jeopardize these teeth),
If the occlusion is acceptable, with the first premolar in the position of the canine and with an otherwise functional occlusion with well-aligned teeth,
If there are pathologic changes (e.g., cystic formation, infection), and
If the patient does not desire orthodontic treatment.
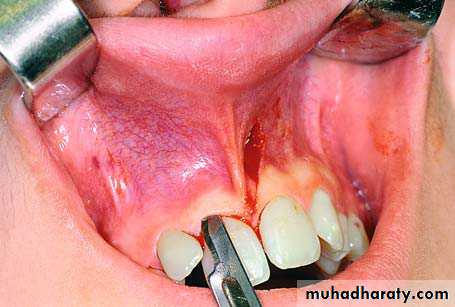
Extraction Using Labial Approach
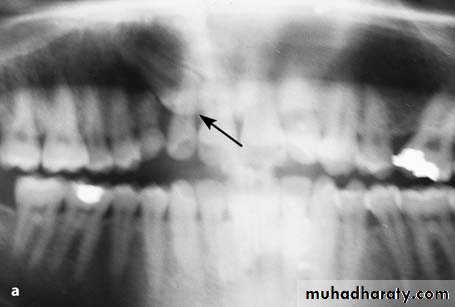
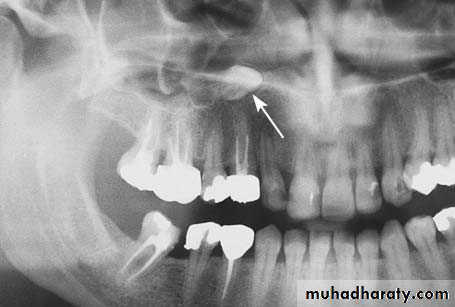
Radiograph showing impacted maxillary canines. Right canine is located labially while left canine is located palatally
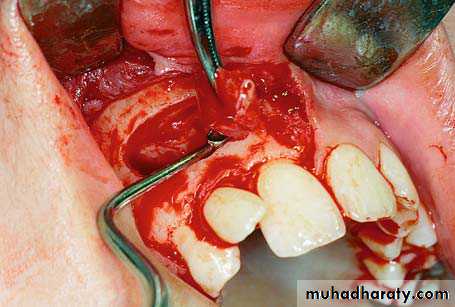
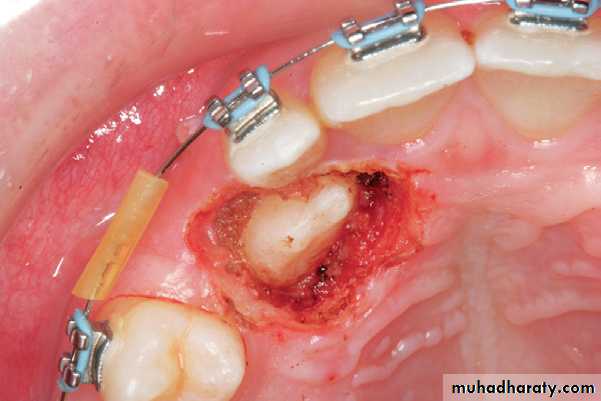
Clinical photograph of the labial area where the right canine is localized labially
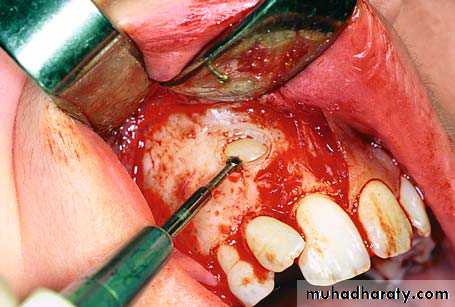
right canineSurgical procedure for removal of right impacted canine. A trapezoidal incision is created buccally. It is desirable to make an intersulcular incision extending to at least one to two teeth in each direction from the area of interest
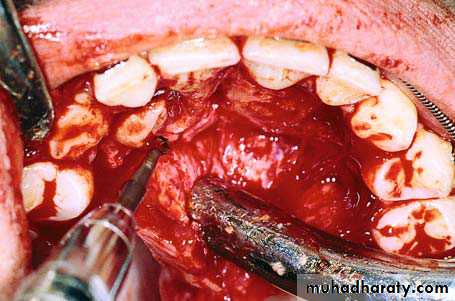
Reflection of the mucoperiosteal flap
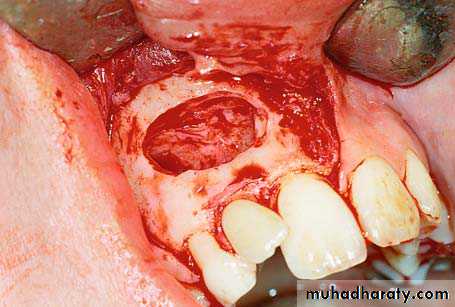
Note: A common error is to develop a small flap and extend it conservatively. This approach, although reasonable in theory, in practice often leads to tearing of the flap and/or inadequate exposure, ultimately resulting in a poor outcome. A well planned and properly retracted large flap generally heals as well, if not better, than a traumatized small flap.A round bur is used to remove the bone covering the crown of the tooth
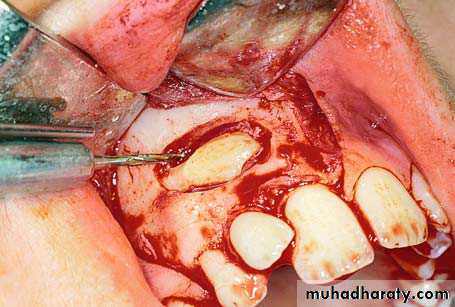
Complete exposure of the crown of the tooth and part of the root
Sectioning of the crown–root at the cervical line of the tooth, using a fissure bur
Removal of the crown of the impacted tooth using a straight elevator
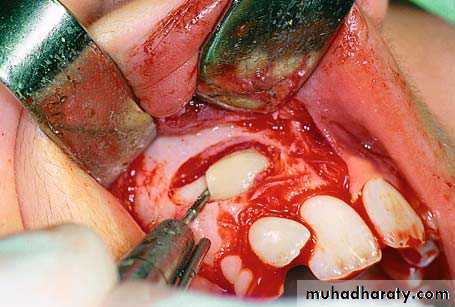
Root of the tooth after removal of the crown
Purchase point created on the root for placement of the elevator blade
Luxation of the root using a curved Chompret elevator
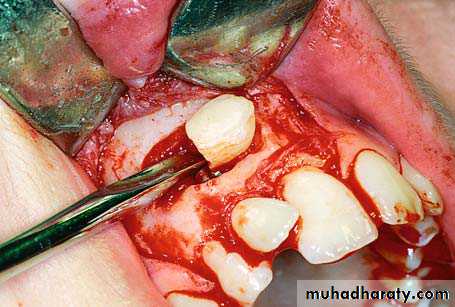
Final step of root extraction
Removal of follicle using a hemostat and periapical curette
Surgical field after removal of the tooth
Smoothing of the bone edges of the wound using a bone file
Surgical field after suturing
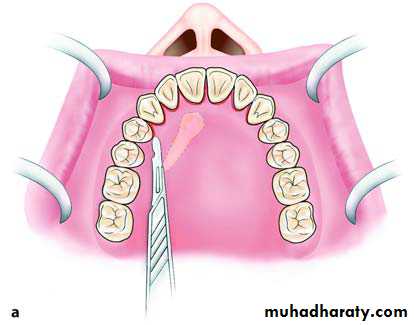
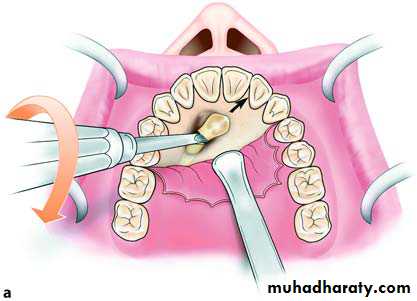
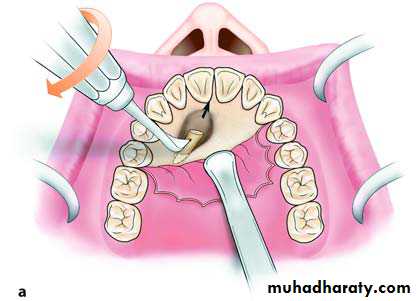
Extraction Using Palatal ApproachWhen the impacted tooth is positioned palatally, the approach is achieved using a bilateral palatal flap. The incision for creation of the flap begins at the first or second ipsilateral premolar and, after continuing along the cervical lines of the teeth, ends at the first premolar on the contralateral side
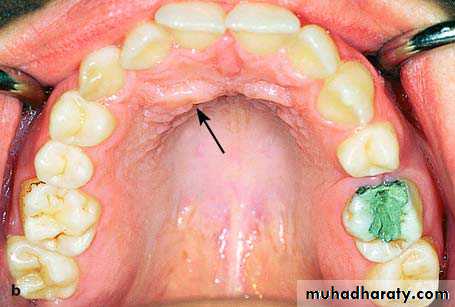
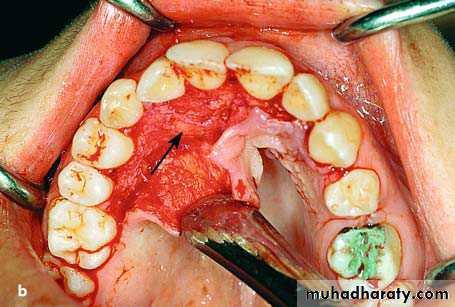
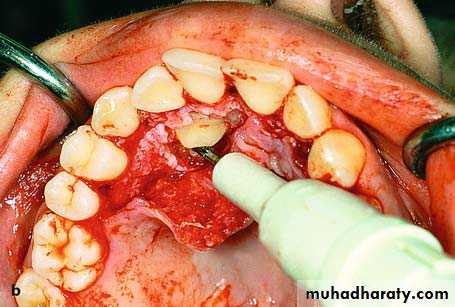
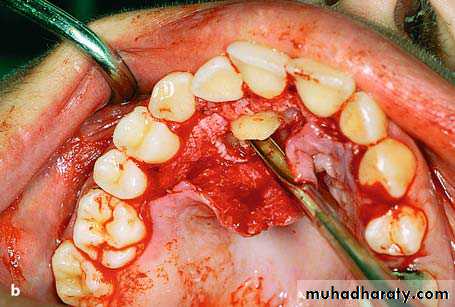
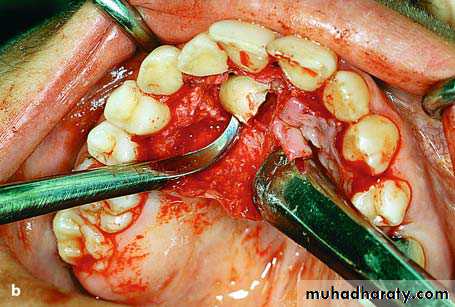
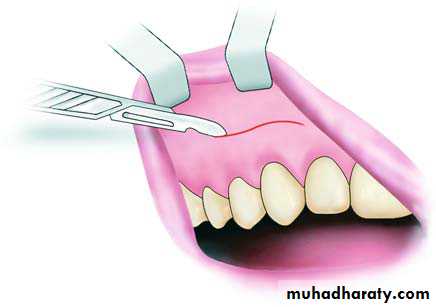
Palatal incision along the cervical lines of the teeth. a Diagrammatic illustration. b Clinical photograph
After careful reflection of the mucoperiosteum, part of the crown of the tooth may be exposed, or the entire crown may be covered by bone, resulting in protuberance at that site
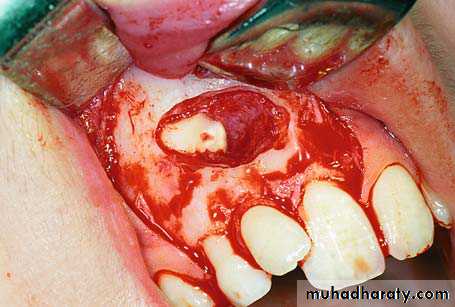
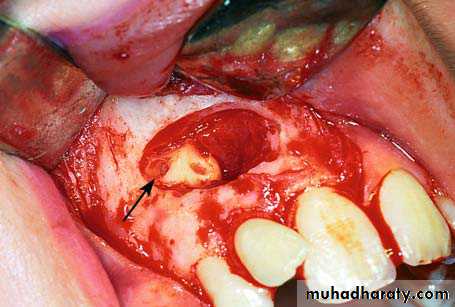
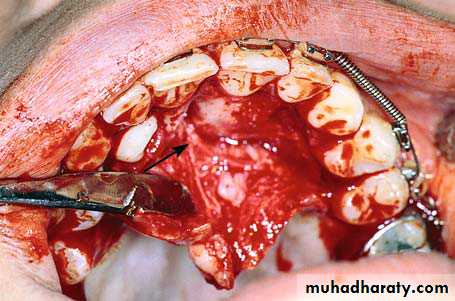
reflection of the flap. Arrow points to the protuberance of bone, which indicates the position of the crown of the impacted tooth
Enough bone must be removed to expose the entire crown, so that the tooth may be extracted using forceps or an elevator. If the tip of the crown is positioned between the roots of the lateral and central incisors, there is a risk of injuring their roots during the exposure attempt. That is why extraction of the canine must be achieved using the technique of separating the crown from the root.
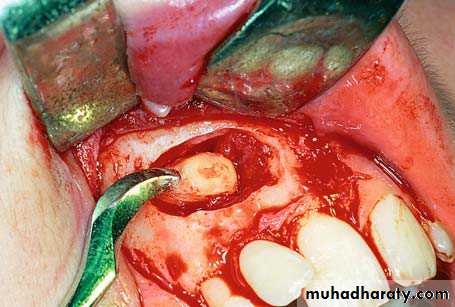
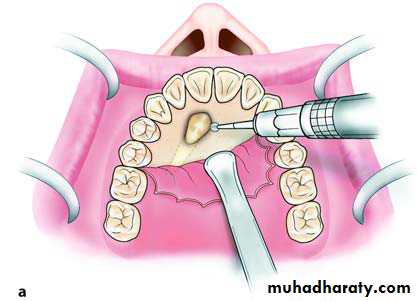
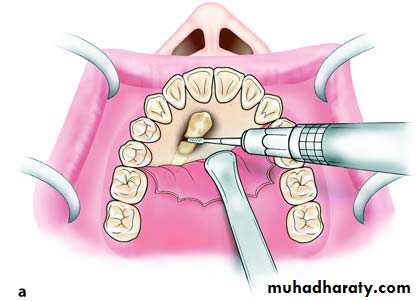
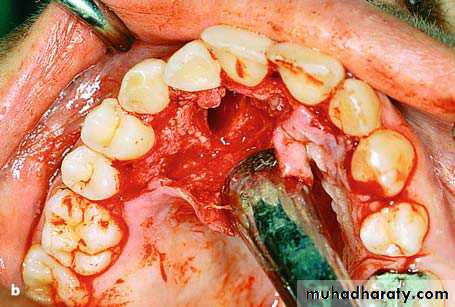
Removal of bone using a round bur, to expose the crown of an impacted tooth
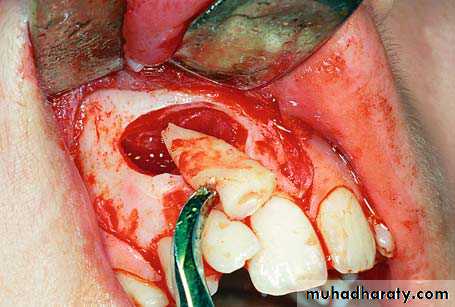
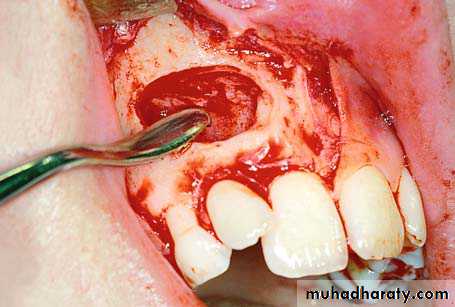
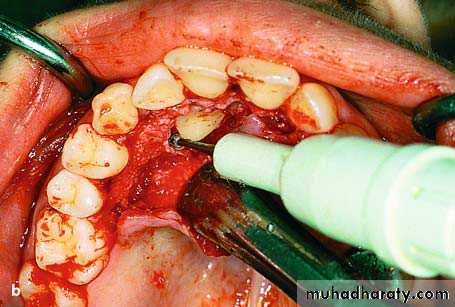
More specifically, a groove is created on the cervical line of the tooth using a fissure bur and, after placing the elevator blade in the groove created, the instrument is rotated until the crown is separated from the root. The crown is then removed, and, after using the round bur to create a purchase point on the root for placement of the angled elevator’s tip, the root is elevated from its bed.Sectioning of an impacted tooth at the cervical line and separation of the crown from the root
Placement of the straight elevator in the groove created to separate the crown from the root and removal of the crown.
Removal of root from its position in the bone using an angled elevator
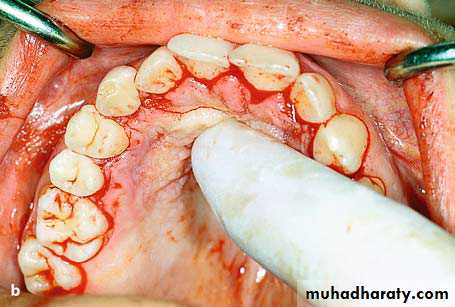
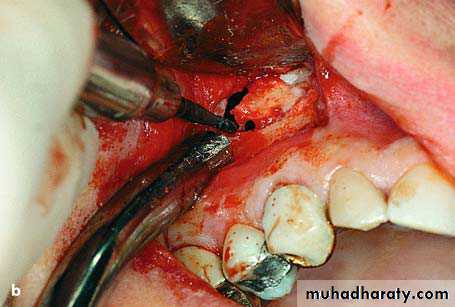
After this procedure, the bone edges are smoothed, and the area is thoroughly irrigated with saline solution, while the flap is repositioned and sutured with interrupted sutures
Surgical field after removal of the impacted tooth
The two segments of tooth after removal
The flap is repositioned in its initial position and pressure is applied to the area with the index finger for a few seconds.
Surgical field after suturing
Ectopic Impacted teethThe presence of ectopic impacted teeth is relatively rare. Ectopic teeth are usually localized in the following places: underneath permanent teeth, near the angle of the mandible, inside the ramus, near the mandibular notch, the coronoid process, the maxillary tuberosity, the wall of the maxillary sinus, the nasal cavity and, rarely, near the orbit.
Radiograph showing impacted canine with a labial localization, which is in contact with the anterior wall of the maxillary sinus
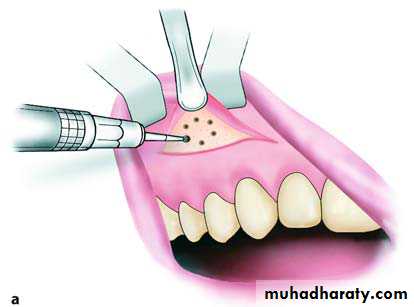
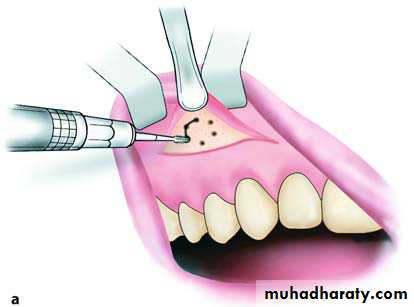
Incision in canine fossa region, for sinus trephination using the Caldwell–Luc approach
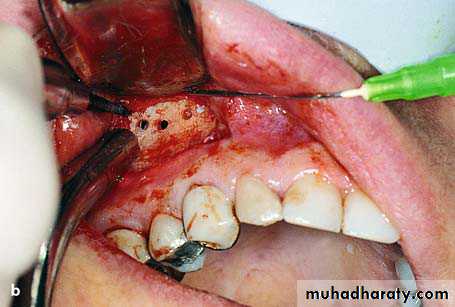
Reflection of the mucoperiosteal flap and exposure of the anterior wall of maxillary sinusFirst a horizontal incision is made in the region of the canine fossa, from the lateral incisor as far as the first molar.
The mucoperiosteum is then reflected and the bone of the anterior wall of the maxillary sinus is exposed.
Holes are drilled through the bone using a small round bur where the impacted tooth is estimated to be, and these holes are then joined together. After removal of the bone surface, the impacted tooth is exposed and carefully luxated outwards.
Holes drilled through the bone surface defining the border of bone to be removed
Connecting holes to remove the bone covering the impacted tooth.
a Exposure and luxation of the impacted tooth using straight elevator. b Removal of tooth using a hemostat
After smoothing the bone edges of the wound, the area is irrigated thoroughly with saline solution and any foreign matter that has entered the maxillary sinus is aspirated with the suction tip.
Finally, the flap is sutured and nasal decongestants are prescribed.
Surgical field after suturing. a Diagrammatic illustration. b Clinical photograph
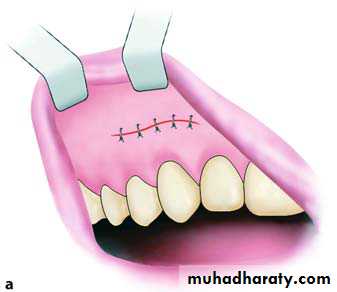
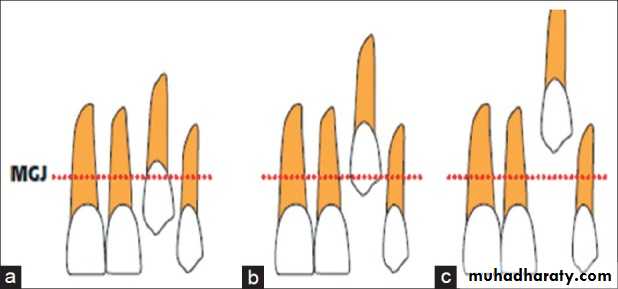
Exposure of Impacted Teeth for Orthodontic TreatmentFour basic surgical techniques have been described by Kokich and Cooke for managing the impacted canines
1.Gingivectomy/soft tissue window
2. Apically positioned flap
3. Open eruption—replaced flap with a soft tissue window or tissue excision without flap
4. Closed eruption—replaced flap without a soft tissue window removed
Recommended surgical techniques relative to the mucogingival junction (MGJ) when the canine cusp is (a) coronal to the MGJ: gingivectomy; (b) apical to the MGJ: creating an apically positioned flap; and (c) significantly apical to the MGJ: using a closed eruption technique
LABIAL/BUCCAL IMPACTIONS
.Labially positioned impacted tooth exposed by gingivectomy
Labially impacted canine tooth managed with an apically positioned flap.
Two basic approaches, either a “closed” or “open” technique, are used to provide access to the impacted canine.
In the “closed eruption” Technique, the crown of the canine is exposed, the orthodontic eruption device is attached to the crown, and the flap is sutured back over the tooth, leaving only the eruption chain exposed for orthodontic manipulation. The eruption chain is usually exited through either the crestal incision or the extraction site of the primary canine and ligated to the archwire or brackets on the adjacent teeth.
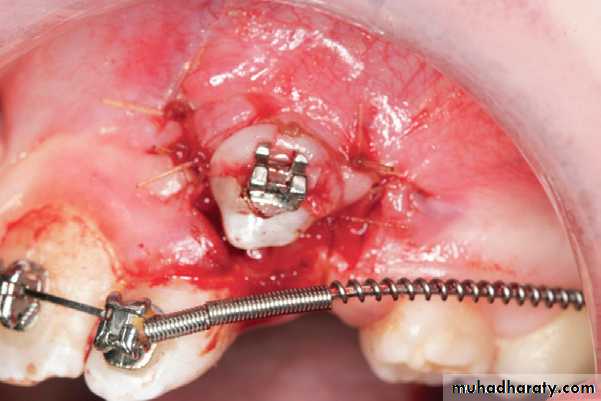
“closed eruption”technique
Surgical exposure of impacted canine
Flap, closed eruption procedure for exposure (A) and bonding (B) of palatally impacted tooth (C), Flap sutured back over
the tooth, leaving only the eruption chain exposed.
C
A
B
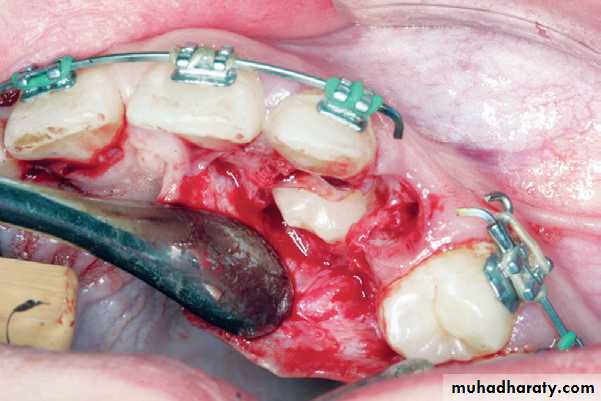
In the “open eruption” technique, the crown of the impacted tooth is exposed with either an opening cut into the overlying tissue without flap reflection, or a flap is reflected, a window cut in it, and then the flap is repositioned.
“open eruption”technique
Flapless open procedure (A) with periodontal dressing applied (B) for palatally impacted tooth
open procedure
Disadvantage of open technique
• Impairment of healing and recovery time• Pain
• Oral function impairment e.g (ability to eat and enjoy food, swallowing, and mouth opening), and
• Food accumulation after an open eruption technique
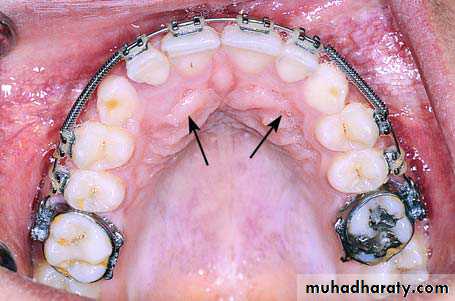
Radiograph showing impacted maxillary canines with a palatal localization
Clinical photograph of the area of impaction
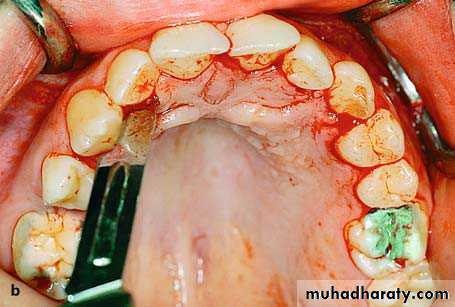
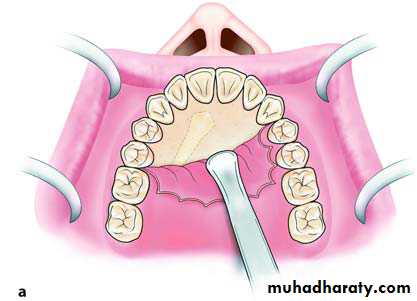
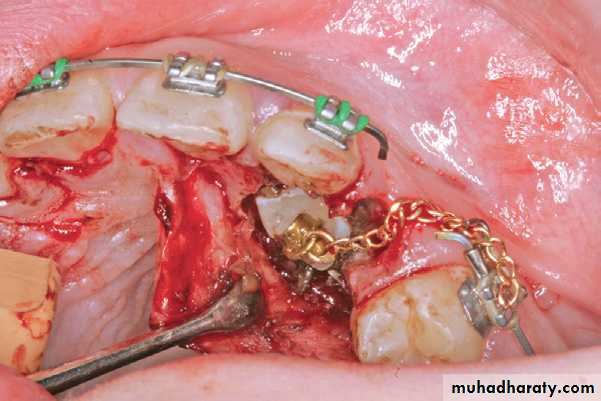
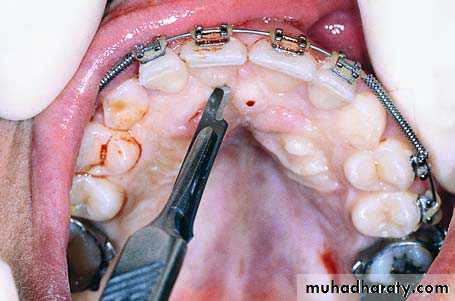
Palatal incision along the cervical lines of teeth using a scalpel with a no. 15 blade
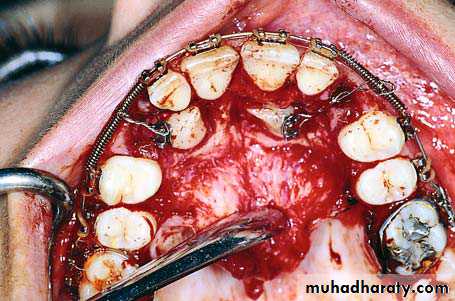
Reflection of the mucoperiosteal flap. Arrow points to the nasopalatine nerve
Removal of the bone covering the crowns of impacted teeth
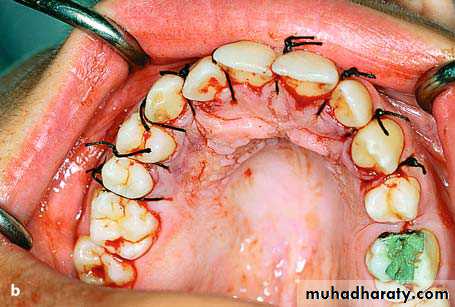
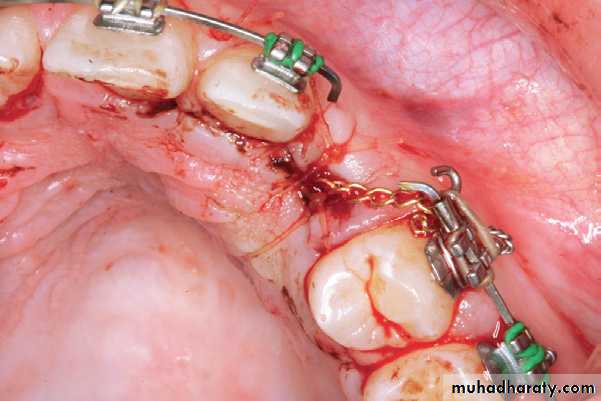
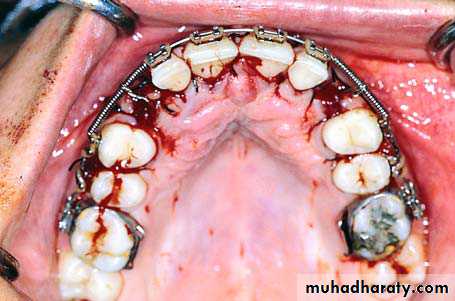
Palatal impaction canineSurgical field immediately after exposure of
impacted teeth. Orthodontic brackets have been placed on exposed parts of the crowns of the teethSurgical field after suturing
Dilaceration
Dilaceration: Is a developmental disturbance in shape of teeth. It refers to an angulation, or a sharp bend or curve, in the root or crown of a formed tooth.Etiology: The condition is thought to be due to trauma or possibly a delay in tooth eruption relative to bone remodeling gradients during the period in which tooth is forming. Developmental disturbances,
Developmental syndromes,
Trauma secondary to neonatal laryngoscopy,
Endotreacheal intubation.
Treatment and prognosis
• Extraction of primary deciduous teeth, if they demonstrate undesired resorption and result in delayed eruption.• Grossly deformed teeth required surgical extraction because of extensive deformation of the affected tooth, repositioning and perforation of buccal alveolar ridge by the mispositioned root.
• In mild dilaceration cases, no treatment is required.
Definition: Is the most common supernumary (extra) tooth. It is located in the maxilla in the midline (hence the special name which means "middle tooth").
They can be well formed or just little clumps of tooth like stuff. A related phenomenon is the odontoma.
Mesiodens tooth
Aetiology
possible causes include
• restricted increase in the activity of the dental lamina (hyperactivity theory)
• splitting of the tooth bud into two equal or unequal sections (dichotomy theory)
Genetics
An X-linked inheritance documented.
Associations
it is often an isolated findingmay be part of a syndrome:
• cleft lip and palate
• cleidocranial dysostosis
• Gardner syndrome
Radiographic features
classified into eumorphic (similar to a normal-sized central incisor) and dysmorphic
three common dysmorphic shapes
• conical or peg shaped (most common ~70%)
• tuberculate (more than one cusp or tubercle)
• supplemental (duplication of a normal tooth)
55% grow in the downward position (35% are inverted and 7% are horizontal)
most remain impacted but 25% will erupt (usually eumorphic or conical shape)
Treatment and prognosis
immediate extraction if there is a complicationearly extraction before root formation of the permanent incisors
late extraction after root formation of the permanent incisors
Infra-eruption or submersion of a tooth is due to a failure in eruption in line with adjacent teeth in the vertical plane of occlusion.
Aetiology
The causes include ankylosis, impaction, absence of a permanent successor, disturbances in local metabolism, gaps in the periodontal membrane, trauma, infection, chemical or thermal irritation, failure in bone growth and abnormal tongue pressure..submerged teeth
Potential complications1. An infraerupted tooth can result in insufficient development of adequate width and height of supporting bone.
2. Insufficient bone may also result in dehiscences, periodontal pocketing and root exposure of the adjacent teeth.
3. The infraerupted tooth and adjacent teeth are also at increased risk of developing a carious lesion due to plaque accumulation surrounding the crown and difficult access for proper oral hygiene.
Diagnosis
• Clinical examination reveals a primary tooth that is below the level of the occlusal plane.
• Tapping on the tooth reveals an abnormal percussive 'cracked tea-cup' sound and is indicative of ankylosis.
• Evaluation with a periapical radiograph is indicated and can illustrate the lack of a well defined periodontal ligament and lamina dura space and fusion of the root with bone.
Treatment
• If the tooth is not ankylosed it has been suggested either to wait for normal exfoliation, or restoration of the occlusal surface, or extraction if there is progressive deep infraocclusion or if a malocclusion is present, the patient should be referred to an orthodontist for evaluation as extraction which may influence future orthodontic treatment.
• If ankylosis is diagnosed, the tooth should be (1) monitored until the time that it interferes with eruption of the succendaneous tooth, tipping of the adjacent teeth occurs or supraeruption of opposing teeth occurs. Restoration as crown buildup should be done to maintain the space. (2) If tipping is occurring and space is lost, the tooth should be extracted and space maintenance should be undertaken.(3) early extraction is recommended followed by orthodontic treatment, if there is no permanent successor.
Illustration of edentulous space following extraction of infraerupted primary molar is replaced with a Maryland bridge .