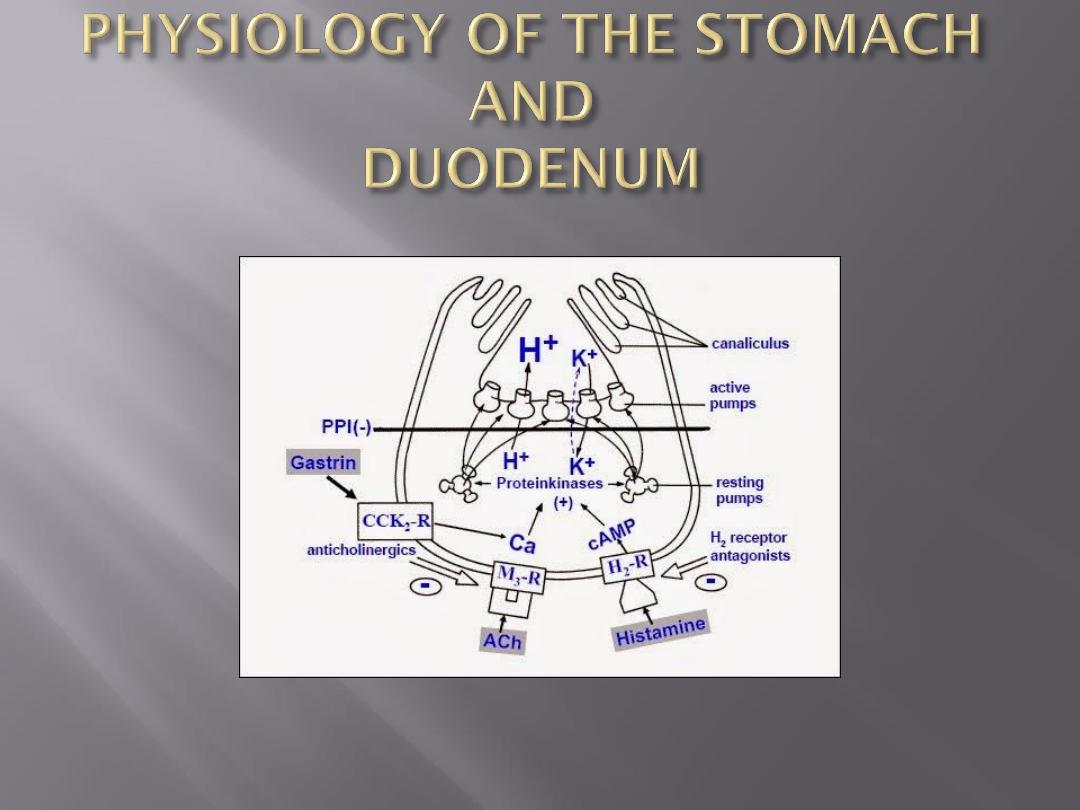
Parietal cells
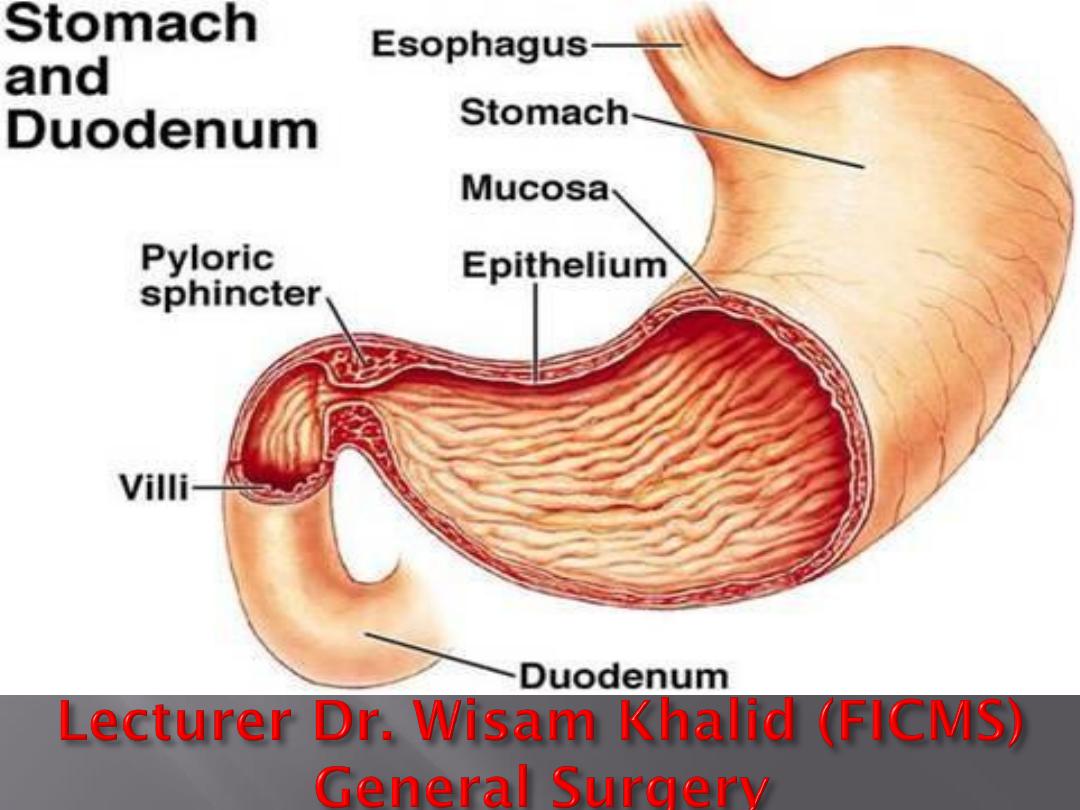
These are in the bodacid-secreting portion) of the stomach
and line the gastric crypts,They
are responsible for the production of hydrogen ions to form
hydrochloric acid.
Chief cells
proximally in the gastric crypts and produce
pepsinogen. Two forms of pepsinogen are described: pepsinogen
I and pepsinogen II.
Endocrine cells
In the gastric antrum, the mucosa contains
G cells
,
which produce
gastrin
. Throughout the body of the stomach,
enterochromaffin-like (ECL) cells
are abundant and produce
Histamine
,
somatostatin-producing D
cells
throughout the stomach, and
somatostatin
has a negative
regulatory role
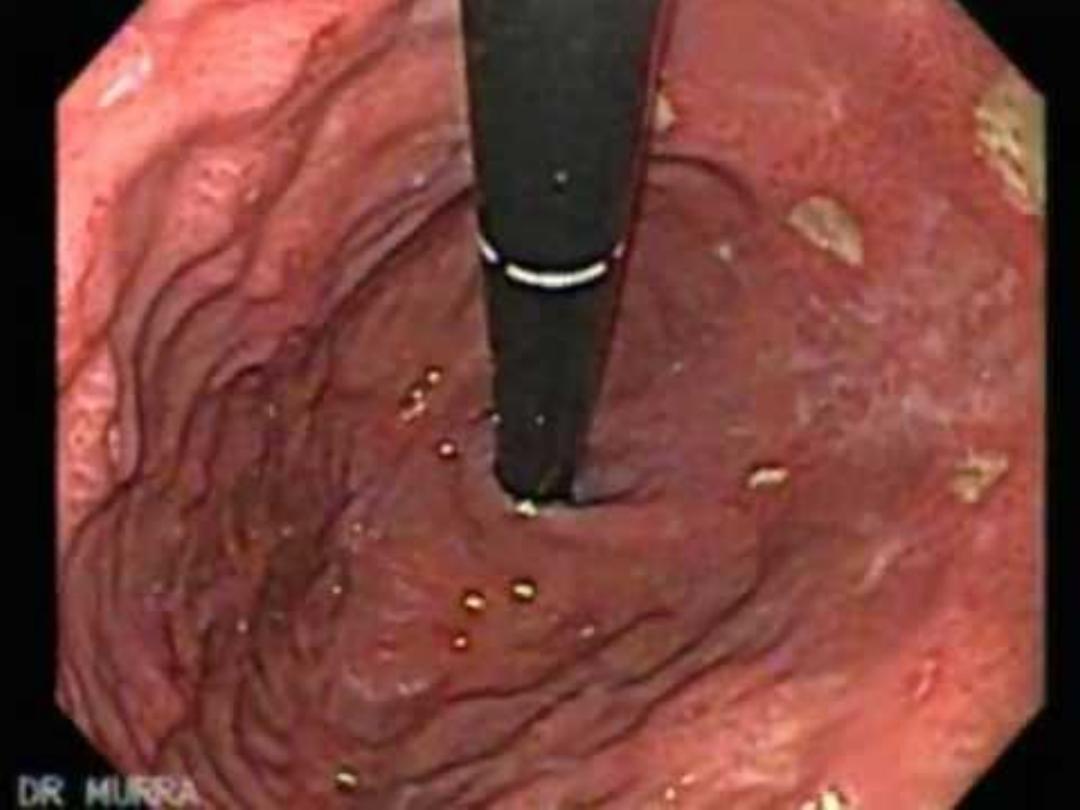
Flexible endoscopy
Contrast radiology
Ultrasonography
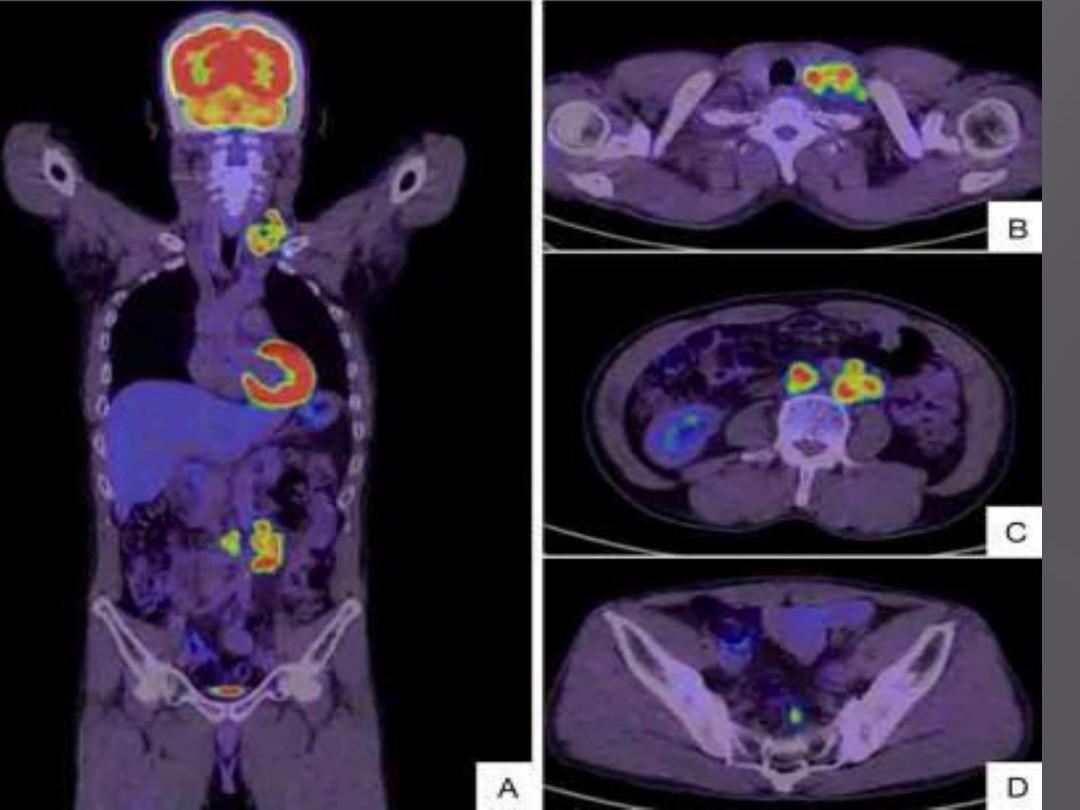
CT scanning and magnetic resonance imaging
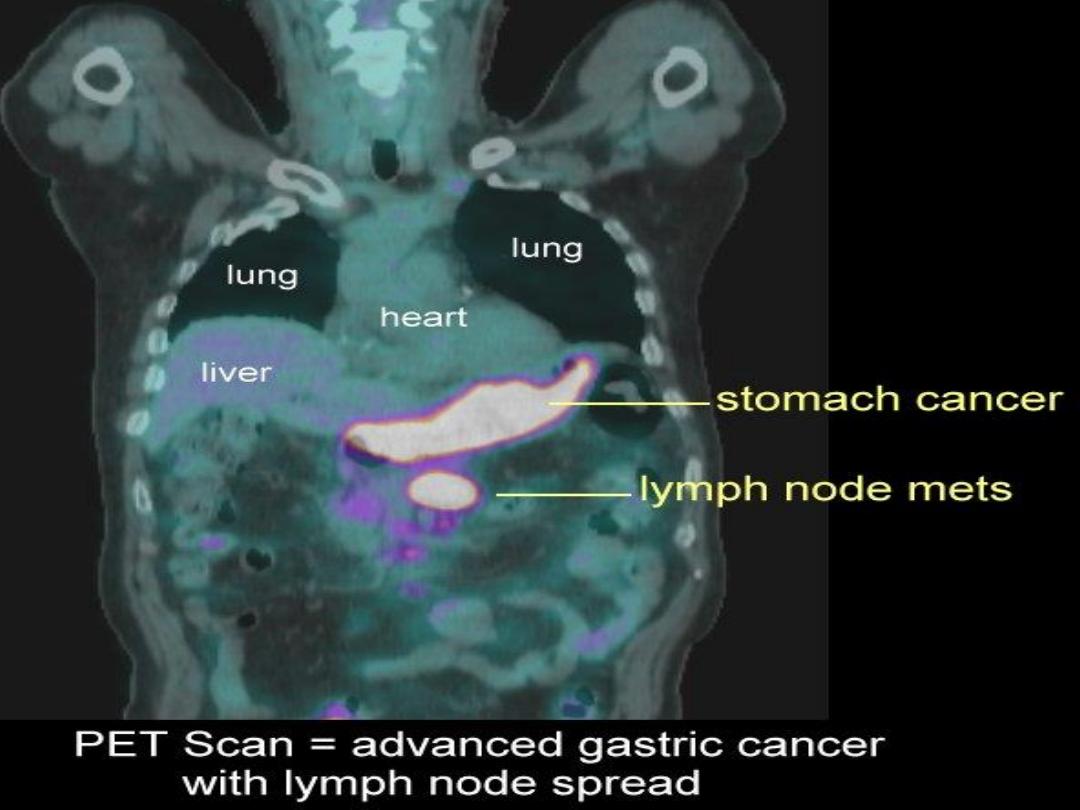
CT/positron emission tomography
Laparoscopy
Gastric emptying studies
Angiography
13C and 14C Urea breath test
HISTOLOGICALLY Giemsa or the Ethin–Starey silver
stains,
Serological test
Breath tests or faecal antigen tests are recommended for the
pretreatment diagnosis of H. pylori infection in the
community
It causes chronic gastritis,peptic ulcer and gastric cancer
eradication therapy is recommended for patients with duodenal
ulcer disease, but not for patients with nonulcer
dyspepsia or in asymptomatic patients who are infected
H. pylori is now classed by the World Health Organisation as a
class 1 carcinogen
The spiral bacterium
H. pylori
is critical in the development of type
B gastritis, peptic ulceration and gastric cancer
Infection appears to be acquired mainly in childhood and the
infection rate is inversely associated with socioeconomic
status
Eradication,
recommended specifically in patients with peptic
ulcer disease, can be achieved in up to 90 per cent of patients
with a combination of a proton pump inhibitor and
antibiotics, and reinfection is uncommon (<0.5 percent)
Erosive gastritis
is usually related to the use of NSAIDs
Type A gastritis
is an autoimmune process and is associated
with the development of pernicious anaemia and gastric
cancer
Autoimmune
Circulating antibodies to the parietal cell
hypochlorhydria and ultimately achlorhydria
pernicious anaemia
Production of high levels of gastrin from the antral G
cells
Patients with type A gastritis are predisposed to the
development of gastric cancer
Affect antrum
Association of this type of gastritis with H. pylori
Patients with
pangastritis seem to be most prone to the development
of gastric cancer.
This is caused by enterogastric reflux and is
particularly common after gastric surgery
have had a cholecystectomy. Bile chelating or
prokinetic agents may be useful in treatment
Operation for the condition should be reserved
for the most severe cases..
The NSAID-induced gastric lesion is associated with
inhibition of the cyclo-oxygenase type 1 (COX-1)
receptor enzyme, hence reducing the production of
cytoprotective prostaglandins in the stomach.
The use of specific COX-2 inhibitors reduces the
incidence of these side effects.
common sequel of serious illness(follows
cardiopulmonary bypass) or injury and is
characterised by a reduction in the blood supply
to superficial mucosa of the stomach.
the routine use of H2-antagonists with or without
barrier agents, such as sucralfate, in patients
who are on intensive care unit.
Unusual condition
gross hypertrophy of the gastric mucosal folds, mucus
production and hypochlorhydria.
Hypoproteinemia & anemia
Premalignant condition
Over expression of TGF-ᾳ
Treatment : gastrecomy
Rare type
infiltration of the gastric mucosa by T cells and is
probably associated with H. pylori infection.
resembles pattern seen in coeliac disease or
lymphocytic colitis..
Eosinophilic gastritis: allergy
Granulomatous gastritis: Crohns disease and TB
Acquired immunodeficiency syndrome (AIDS) gastritis
Phlegmonous gastritis: bacterial
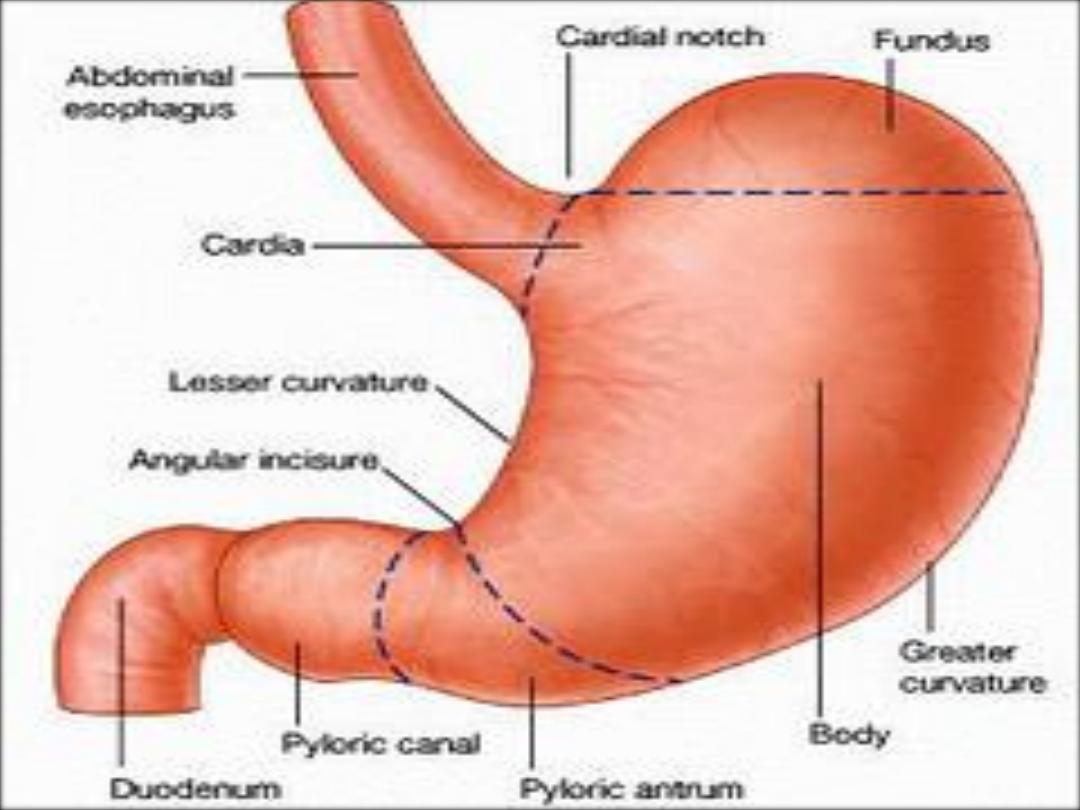
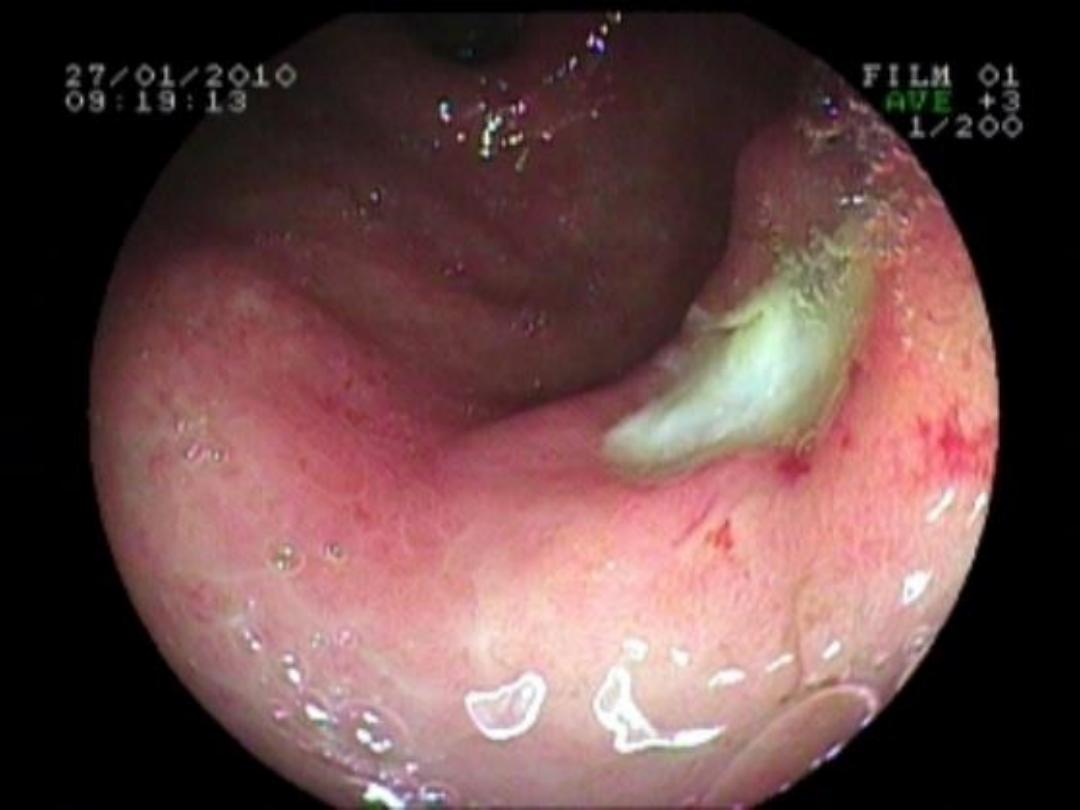
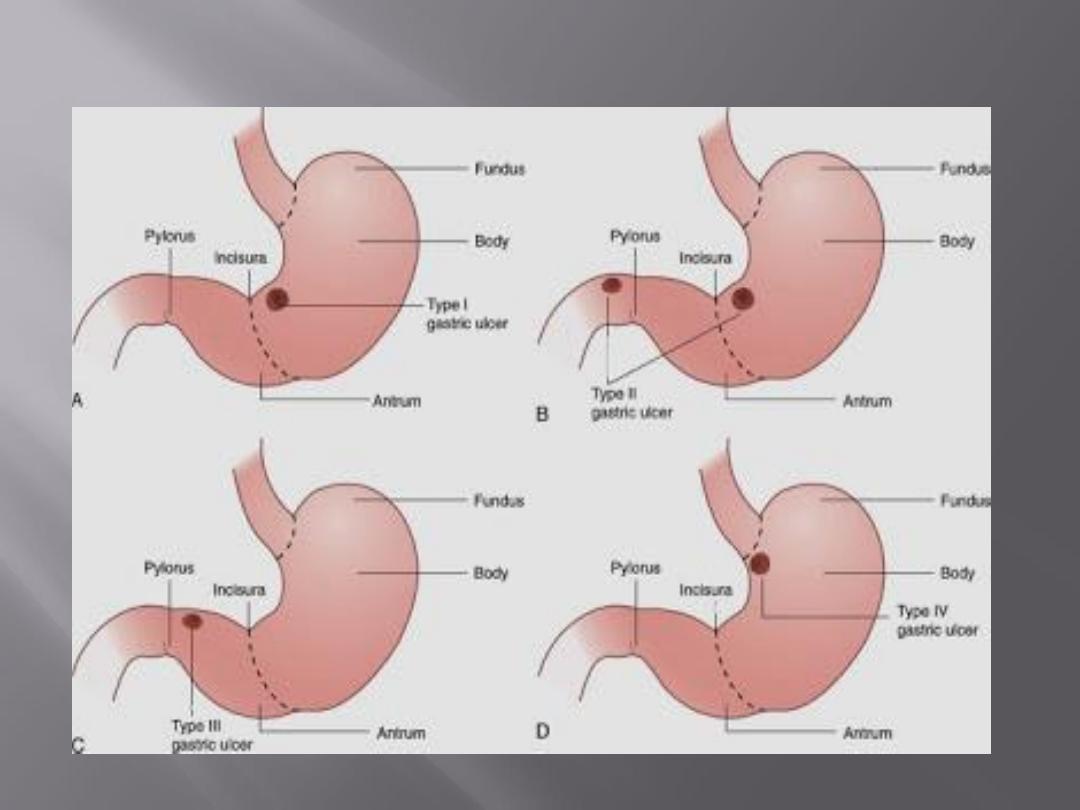
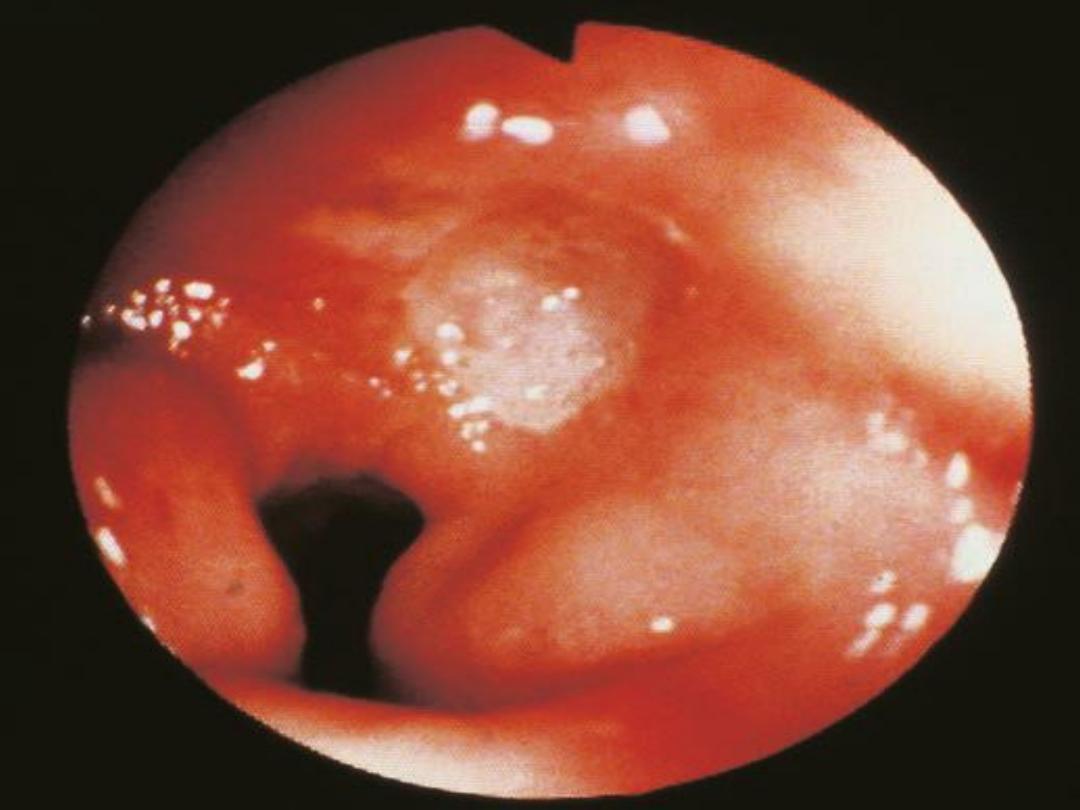
Common
sites for peptic ulcers are the first part of the
duodenum and the lesser curve of the stomach.
They
also occur on the stoma following gastric surgery,
the oesophagus and even in a Meckel’s diverticulum
infection
with H. pylori and the consumption of NSAIDs
are the most important factors in the development of
peptic ulceration
Cigarette
smoking predisposes to peptic ulceration and
increases the relapse rate after treatment, with either
gastric antisecretory agents or, in the past, elective
Surgery
the peak incidence is now in a much older age
group
More common in men,
Most
occur in the first part of the duodenum
chronic
ulcer penetrates the mucosa and into the muscle coat,
leading to fibrosis.
The fibrosis
causes deformities such as pyloric stenosis
‘kissing ulcers’.
Anterior ulcer
tend to perforate ,
Posterior ulcer
tend to
bleed
malignancy
in this region is so uncommon that under
normal circumstances surgeons can be confident that
they are dealing with benign disease
Destruction
of the muscular coat is observed and the
base of the ulcer is covered with granulation tissue,
THE
arteries in this region showing the typical changes
of endarteritis Obliterans

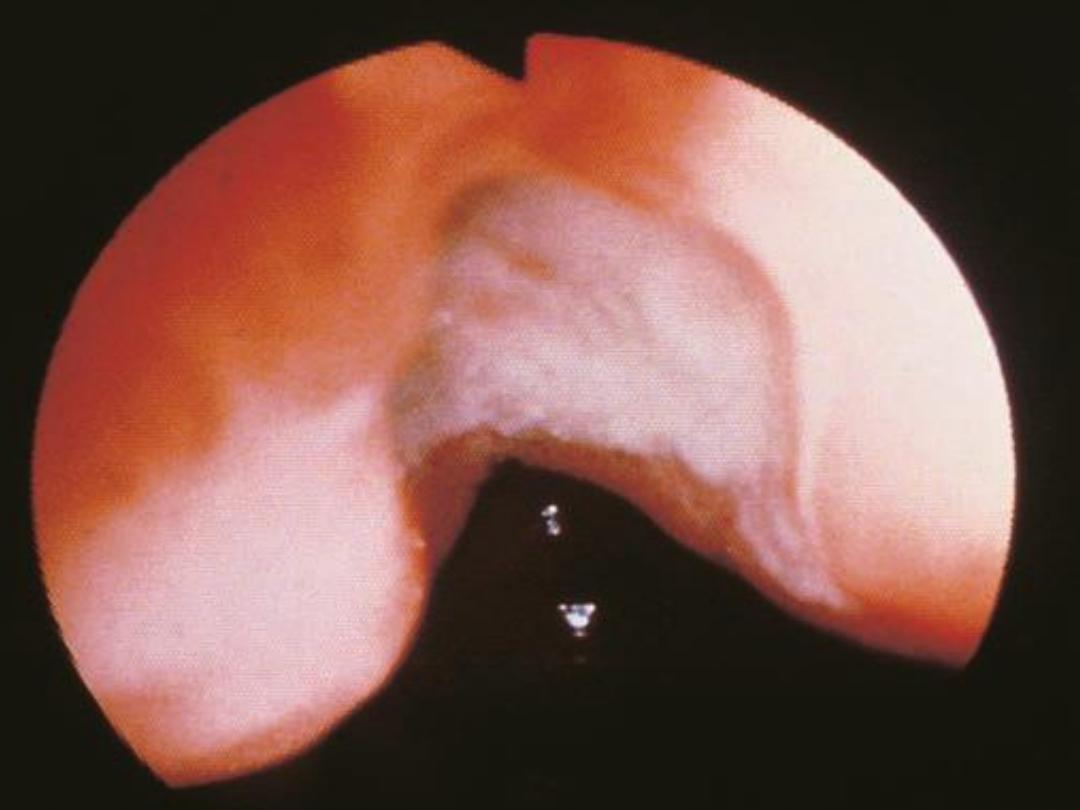
As with duodenal ulceration, H. pylori and NSAIDs are
the important aetiological factors.
Gastric ulceration is also associated with smoking
gastric ulceration is substantially less common than
duodenal ulceration
The sex incidence is equal and the population with
gastric ulcers tends to be older.
It is more prevalent in low socioeconomic groups
Gastric ulcers tend to be larger
Fibrosis rarely seen hourglass contraction of the
stomach.
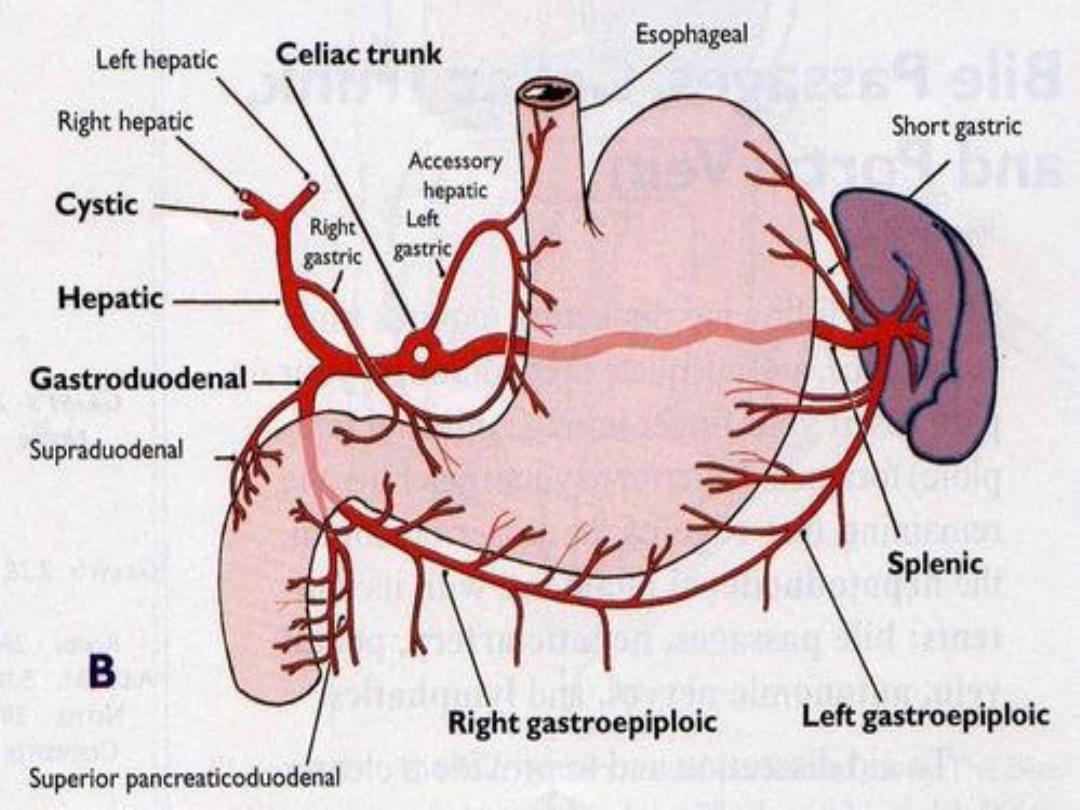
Large chronic ulcers may erode posteriorly into the
pancreas and, on other occasions, into major vessels
such as the splenic artery
. Chronic gastric ulcers are much more common on the
lesser curve (especially at the incisura angularis)

Giant ulcers are those that are more than 3 cm in
diameter.
These ulcers have an increased association with cancer:
30% of those larger than 3 cm harbor malignant
disease.
Earlier surgical intervention is generally warranted
given this association.
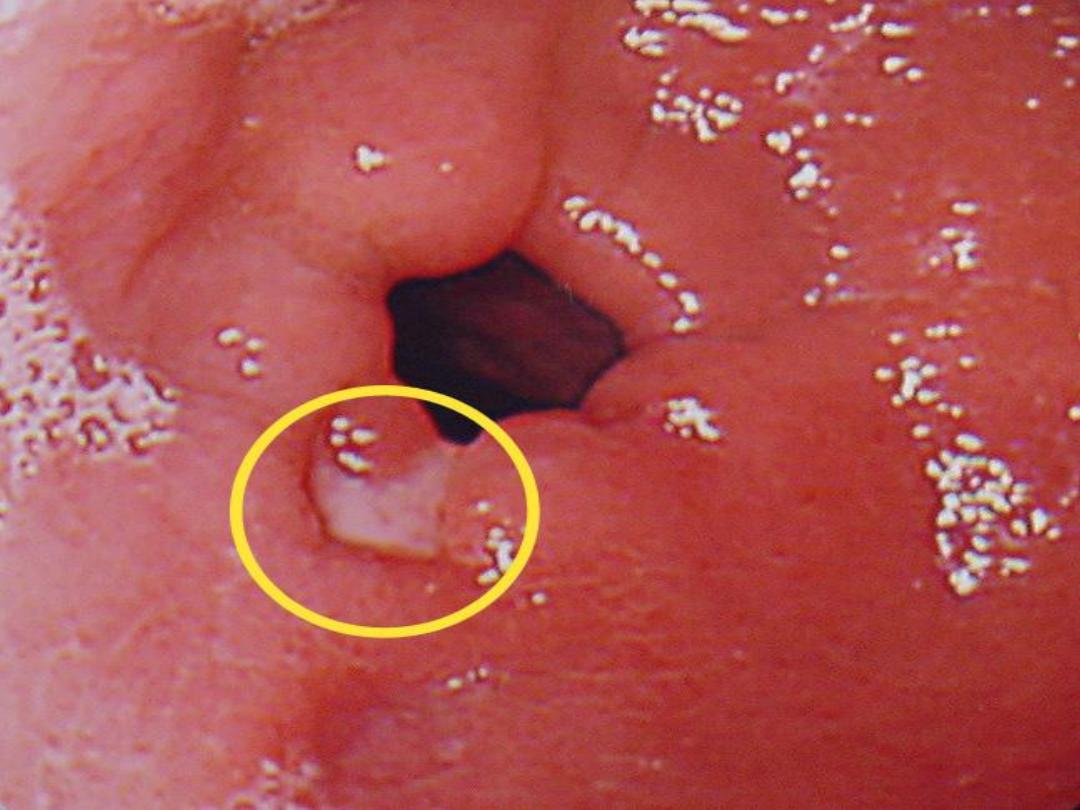
Endoscopy with multiple biopsies (at least four with
jumbo forceps and eight with regular) to include
both the ulcer base and edge usually provide
sufficient tissue for diagnosis to guide therapy, with
treatment of nonmalignant ulcers adhering to
guidelines as outlined previously, depending on the
location.
It is fundamental that any gastric ulcer should be
regarded as being malignant,
Multiple biopsies should always be taken, perhaps as
many as ten well-targeted biopsies
It is important
that further biopsies are taken while the
ulcer is healing and when healed.
At operation
, even experienced surgeons may have
difficulty distinguishing between the gastric cancer
and a benign ulcer
Pain
Periodicity
Vomiting : fibrosis
Alteration in weight
Bleeding: microcytic anaemia
is not uncommon


Peptic ulcer and H. pylori
then eradication Rx
NSAIDS and stomal ulcer
Patients with
Zollinger–Ellison syndrome
should be
treated in the long term with proton pump inhibitors
unless the tumour can be adequately managed by
surgery.
Agent
Length of treatment
PPI (omeprazole 20 mg OR lansoprazole
30 mg)
+ Amoxicillin 1000 mg
+ Clarithromycin 500 mg
Orally, twice daily for 14 days
PPI (omeprazole 20 mg OR lansoprazole
30 mg)
+ Metronidazole 500 mg
+ Clarithromycin 500 mg
Orally, twice daily for 14 days
Alternative regimen:
Bismuth subsalicylate 525 mg qid
+ Metronidazole 500 mg tid
+ Tetracycline 500 mg qid
+ PPI (omeprazole 20 mg OR lansoprazole
30 mg daily)
Orally, given as indicated for 14 days
persistent H. pylori
Infection
poor compliance
ingestion of NSAIDs
Zollinger–Ellison syndrome
Billroth II gastrectomy:Two-thirds
of the stomach
removed, the duodenal stump is closed and the stomach
.
anastomosed to the jejunum
Gastrojujenostomy
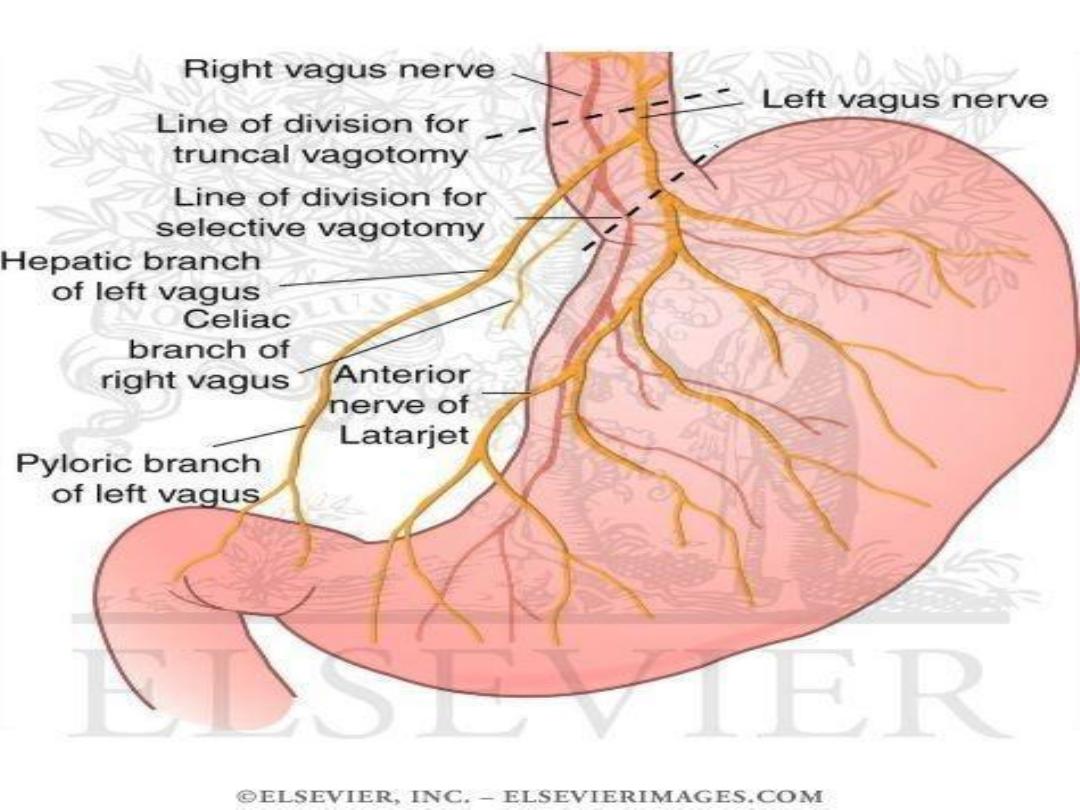
Truncal vagotomy with drainage(HM)
Highly Selective vagotomy with drainage
Truncal vagotomy with antrectomy
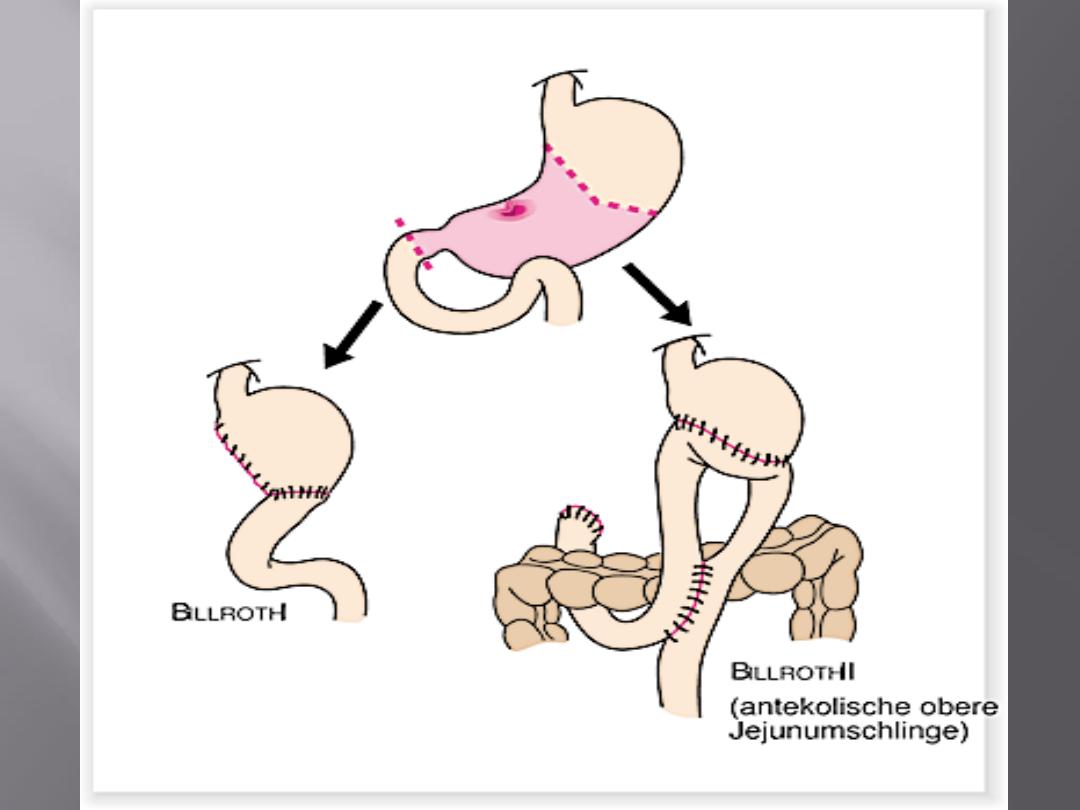

Billroth I
gastrectomy
Most
peptic ulcers are caused by H. pylori or NSAIDs
Duodenal ulcers
are more common than gastric ulcers, but
the symptoms are indistinguishable
Gastric ulcers
may become malignant and an ulcerated
gastric cancer may mimic a benign ulcer
Gastric
antisecretory agents and H. pylori eradication
therapy are the mainstay of treatment, and elective
surgery is very rarely performed
The
long-term complications of peptic ulcer surgery may
be difficult to treat
The
common complications of peptic ulcers are perforation,
bleeding and stenosis
The
treatment of the perforated peptic ulcer is primarily
surgical, although some patients may be managed
conservatively
1.
Recurrent ulceration
2.
Small stomach syndrome
3.
Bile vomitting
4.
Early and late dumping
5.
Postvagotomy diarrhea
6.
Malignant transformation
7.
Nutritional consequences(B12,iron,bone)
8.
Gall stones
The small bowel is filled with foodstuffs from the
stomach, which have a high osmotic load, and this
leads to the sequestration of fluid from circulation
into the gastrointestinal tract..
The principal treatment is
dietary manipulation
. Small,
dry meals are best, and avoiding fluids with a high
carbohydrate content..
Surgery:
Roux en Y reconstruction
This is reactive
hypoglycaemia
. The carbohydrate load
in the small bowel causes a rise in the plasma
glucose, which, in turn causes insulin levels to rise,
causing a secondary hypoglycaemia
The treatment is essentially the same as for early
dumping.
Octreotide
is very effective in dealing with this problem
late
Early
5%
5-10%
incidence
Second hour after
meal
immediately
Relation to meal
same
30-40 min
Duration of attack
food
Lying down
relief
exercise
More food
Aggrevated by
CHO
CHO
Precipitating factor
Tremor faintness
and prostration
Fullness,sweating,
tacchycardia and
sometimes diarrhea
Major symptom
Epidemiology
Previously
, most patients were middle aged, with a
ratio of 2:1 of male:female.
With time, there has been a steady increase in the age
of the patients suffering this complication and an
increase in the numbers of females, such that
perforations now occur most commonly in
elderly
female
patients.
NSAIDs appear to be responsible for most of these
perforations.
sudden onset
severe generalised abdominal pain
Initially, the patient may be
shocked
with a tachycardia
but a pyrexia is not usually observed until some
hours after the event.
Boardlike rigidity
and the patient is disinclined to move
because of the pain. The abdomen does not move
with respiration.
The perforation may be
self-limiting
??how
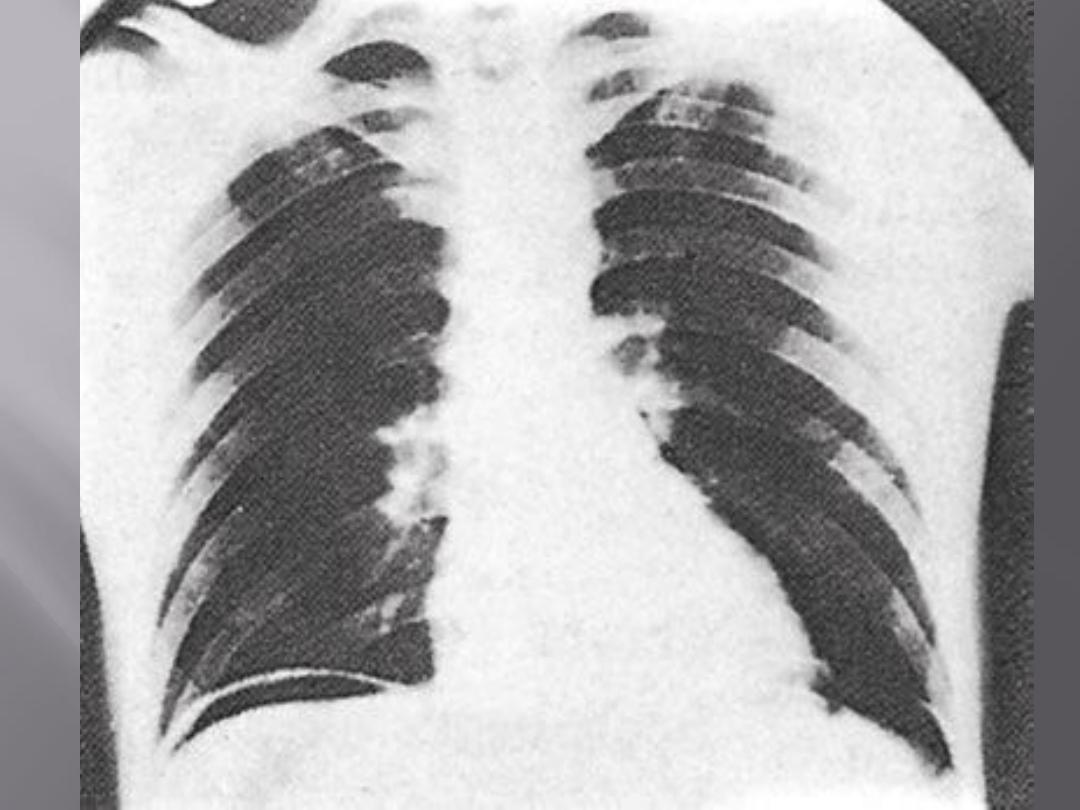
Erect plain
chest radiograph
will reveal free gas under
the diaphragm in an excess of 50 per cent of cases..
CT
imaging is more accurate
serum amylase: WHY?
The treatment is principally surgical
.
systemic antibiotics resuscitation and analgesia
Laparotomy
is performed, usually through an upper midline incision
,thorough peritoneal toilet to
remove all of the fluid and food debris
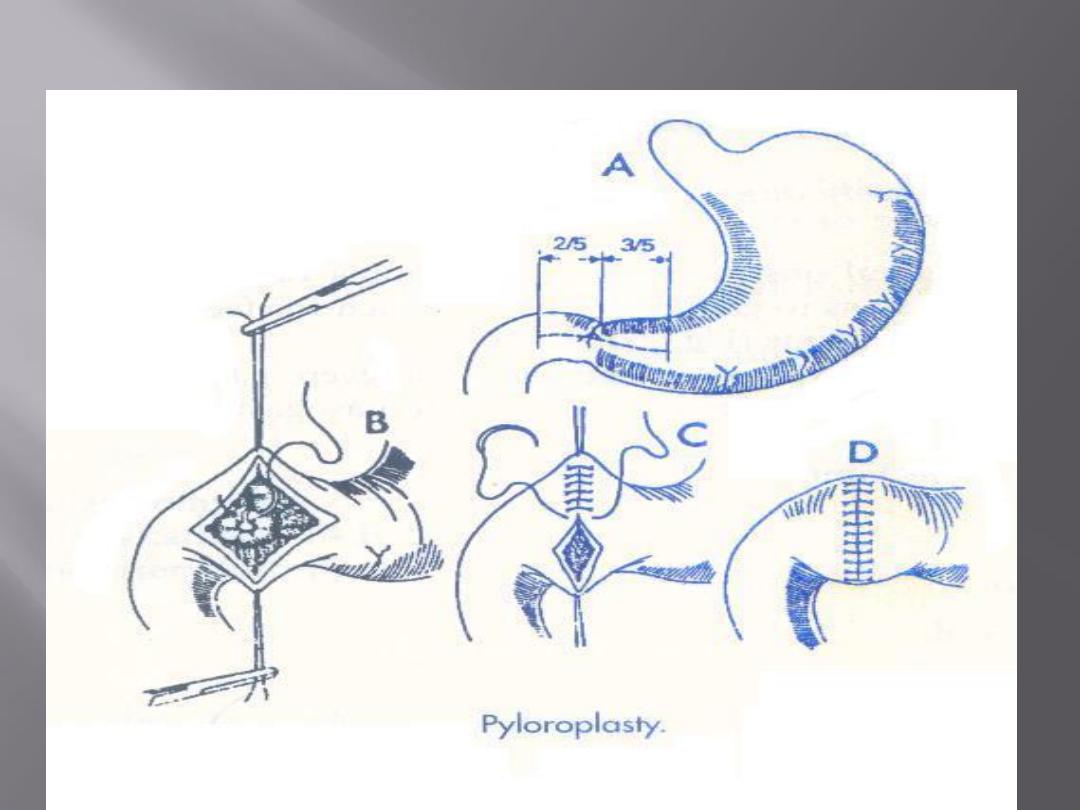
If the perforation is in the duodenum it can usually be closed by
several well-placed
sutures, closing the ulcer in a transverse direction as with a
pyloroplasty.
It is common to place an omental patch over the perforation .
Gastric ulcers shouldbe excised and closed, so that malignancy can be
Excluded
Massive duodenal
or gastric perforation such that simple closure is
impossible; in these patients a Billroth II gastrectomy or subtotal
gastrectomy with Roux-en-Y reconstruction
s
tomach
is kept empty postoperatively by nasogastric suction,
and that gastric antisecretory agents are commenced to promote
healing of the residual ulcer.
• delay in diagnosis (>24 hours)
• medical comorbidities
• shock
• increasing age (>75).
Patients who have suffered one perforation may suffer
another one
The
two
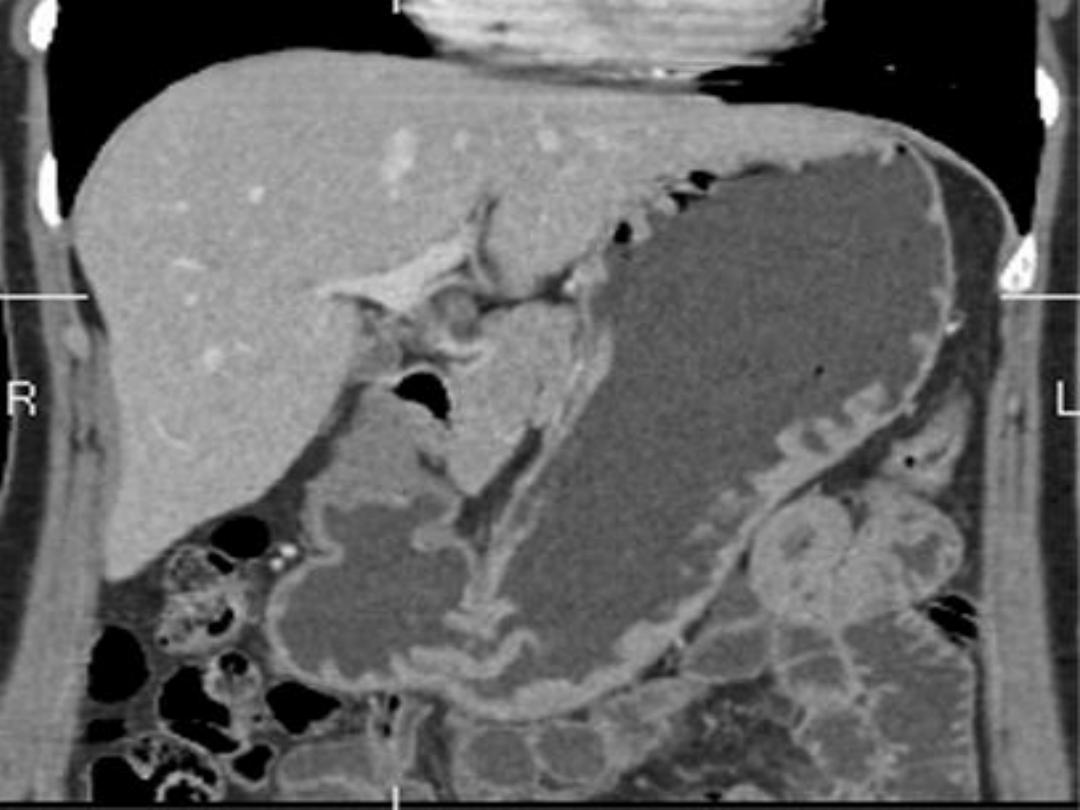
common causes of gastric outlet obstruction
are:
1-
gastric cancer
2-pyloric stenosis secondary to peptic
ulceration.
pain
may become unremitting and in other cases it may
largely disappear
The
vomitus
is characteristically unpleasant in nature
and is totally lacking in bile.
It is possible to recognise foodstuff taken several days
previously
losing weight
, and appears unwell and
dehydrated
.
succussion splash
may be audible on shaking the
patient’s abdomen.
vomiting
of hydrochloric acid results in
hypochloraemic
alkalosis
Initially, the
sodium
and
potassium
may be relatively normal
Dehydration Progresses lead to renal dysfunction
Initially, the
urine
has
a low chloride
and
high bicarbonate
content
This
bicarbonate
is excreted along with
sodium
, and so with time
the patient becomes progressively
hyponatraemic
and more
profoundly dehydrated
Because of the
dehydration
, a phase
of sodium retention
follows
and potassium and hydrogen are excreted
The urine becoming paradoxically acidic and
hypokalaemia
Alkalosis leads to a lowering in the circulating ionised calcium,
and tetany can occur
The patien should be rehydrated with intravenous isotonic
saline with potassium supplementation
Replacing the sodium chloride and water allows the kidney to
correct the acid–base abnormality
gastric antisecretory agent given intravenously
a wide-bore gastric Tube
endoscopy and contrast radiology
Biopsy of the area around the pylorus is essential to exclude
malignancy
Dilatation, stent ,drainage procedure and surgery for CA
Adult pyloric stenosis
Pyloric mucosal diaphragm
Risak of CA
Biopsy is essential
Types:
Metaplastic
: most common associated with H.P and
regress after eradication therapy
Inflammatory
polyps: common
Fundic gland polyps
: associated with PPI use and FAP
Adenomatous
polyp: pre malignant,10% of polyps
Gastric carcinoids arising from the ECL cells are seen in
patients with pernicious anaemia and usually appear
as small polyps
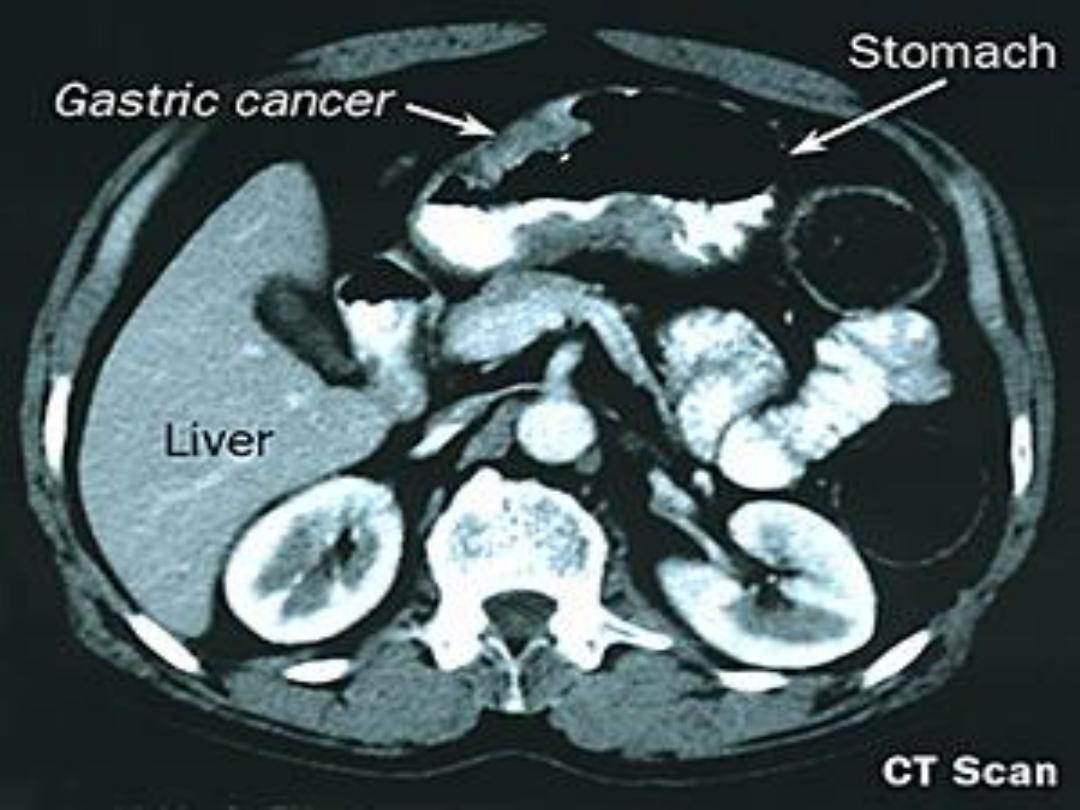
major cause of cancer mortality Worldwide
prognosis tends to be poor, with cure rates little better
than 5–10 per cent
Early diagnosis is the key to success
The only treatment modality able to cure the disease is
resectional surgery
In the UK, it is approximately 15/100 000 per Year
USA 10/100 000 per year
70/100 000 per Year in Japan
men are more affected by the disease than women
Increase the proximal stomach, particularly the
oesophagogastric junction
Proximal gastric cancer does not seem to be associated with
H. pylori infection,
Proximal CA : high SE
Distal CA : Low SE
H. pylori
gastric atrophy ,intestinal metaplasia ,Pernicious Anaemia
gastric polyps
Billroth II, gastroenterostomy or pyloroplasty, duodenogastric reflux
and reflux gastritis
Cigarette smoking and dust ingestion
DIETS: spirit , salt intake,
Obesity: proximal CA
Genetic factors:
Mutation APC gene(Tumor supressor gene) or b-catenin, E cadherin
hereditary non-polyposis colorectal(HNPCC) (Lynch syndrome)
Inactivation of p53
Dyspepsia
In advanced cancer, early satiety, bloating, distension
Vomiting
iron deficiency anaemia
Obstruction leads to dysphagia, epigastric Fullness
Gastric outlet obstruction
Thrombophlebitis (Trousseau’s sign) and deep venous
thrombosis.
Upper oesophagus:2%
Mid oesophagus:6%
Lower oesophagus:22%
GE:18%
Cardia :17%
Body:15%
Antrum :13%
Pylorus:7%
60%
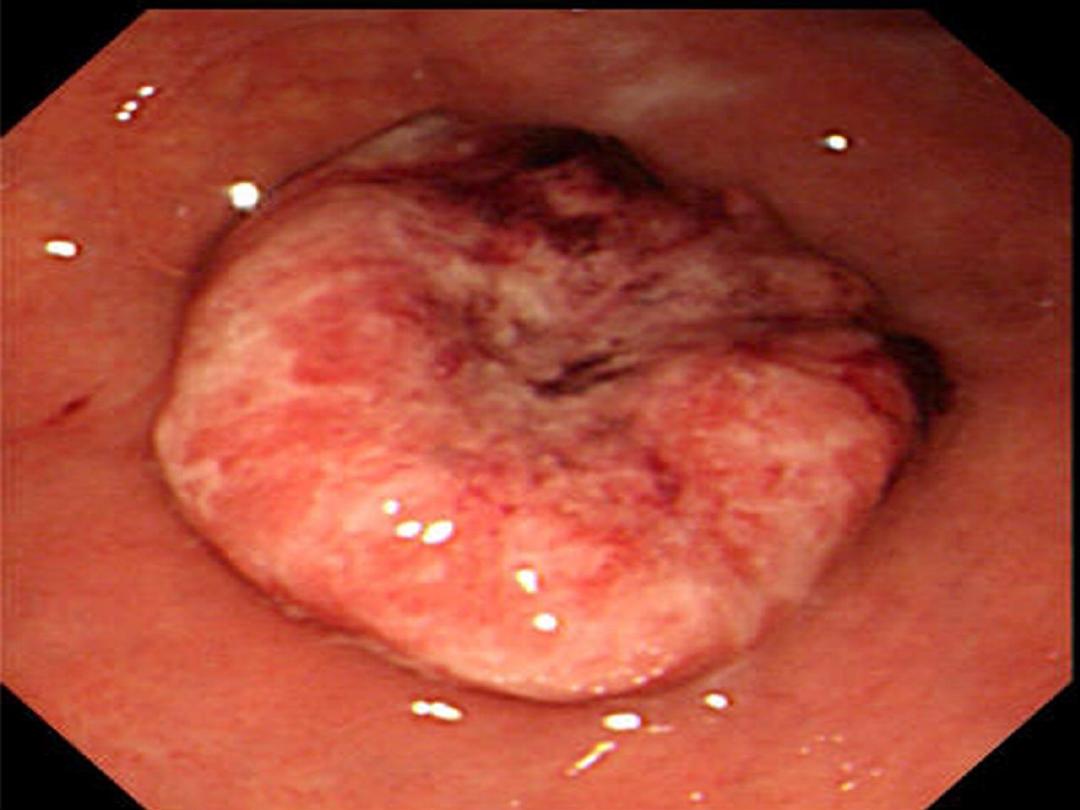
Intestinal : polyp or ulcer
Diffuse : without mass but more
involvement(worse Px)
early gasric CA:
Mucosa and submucosa with or without LN
involvement
T1 & any N
CURABLE
5yrs survival rate 90%
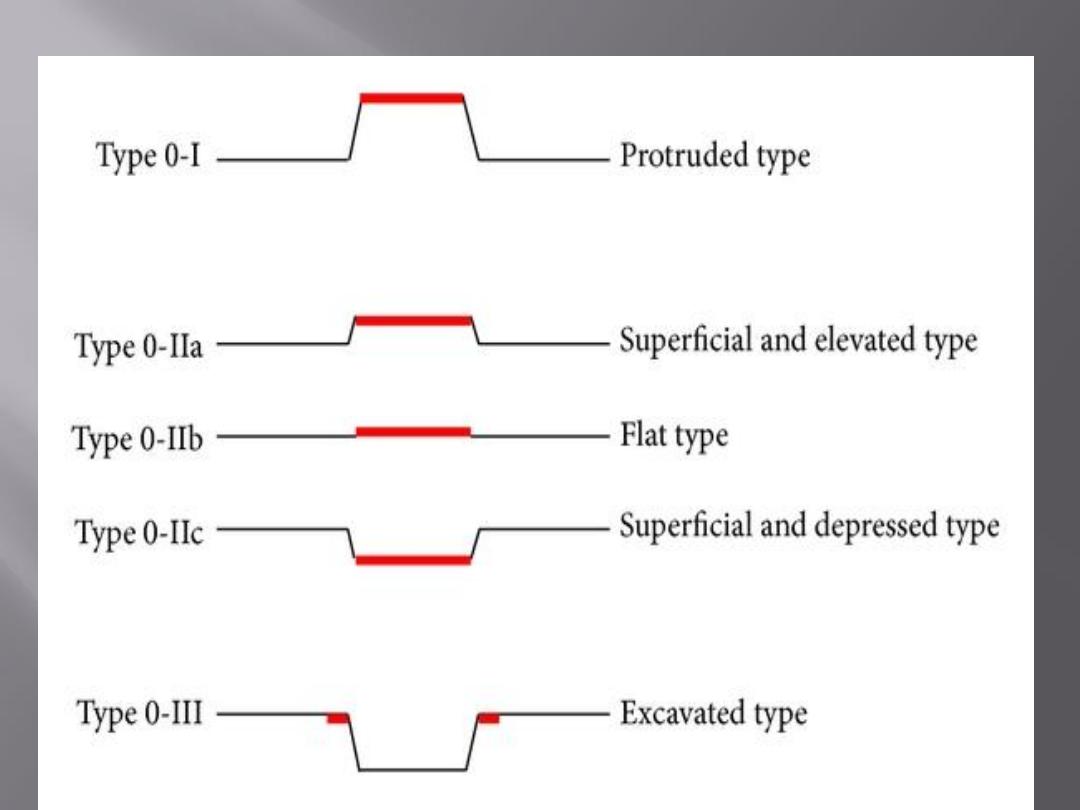
involves the muscularis
Bormann classification from I to IV
III & IV are incurable

T1 :Tumour involves lamina propria, submucosa
T2 :Tumour invades muscularis propria
T3 :Tumour involves subserosa
T4a: Tumour perforates serosa
T4b :Tumour invades adjacent organs
N0: No lymph nodes
N1 :Metastasis in 1–2 regional nodes
N2 :Metastasis in 3–6 regional nodes
N3a: Metastasis in 7–15 regional nodes
N3b :Metastasis in more than 15 regional nodes
M0 :No distant metastasis
M1 : Distant metastasis (this includes peritoneum and distant
lymph nodes)
Lymph node involvement can occur in stage I
No distant metastasis before stage IV disease
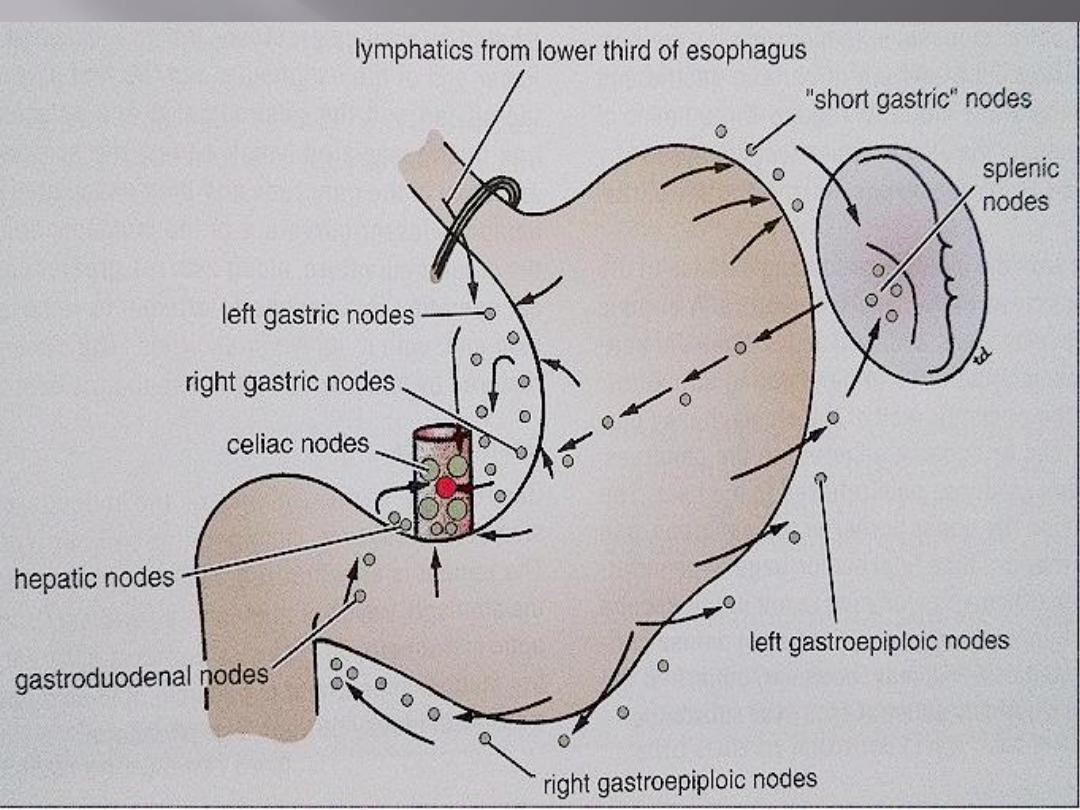
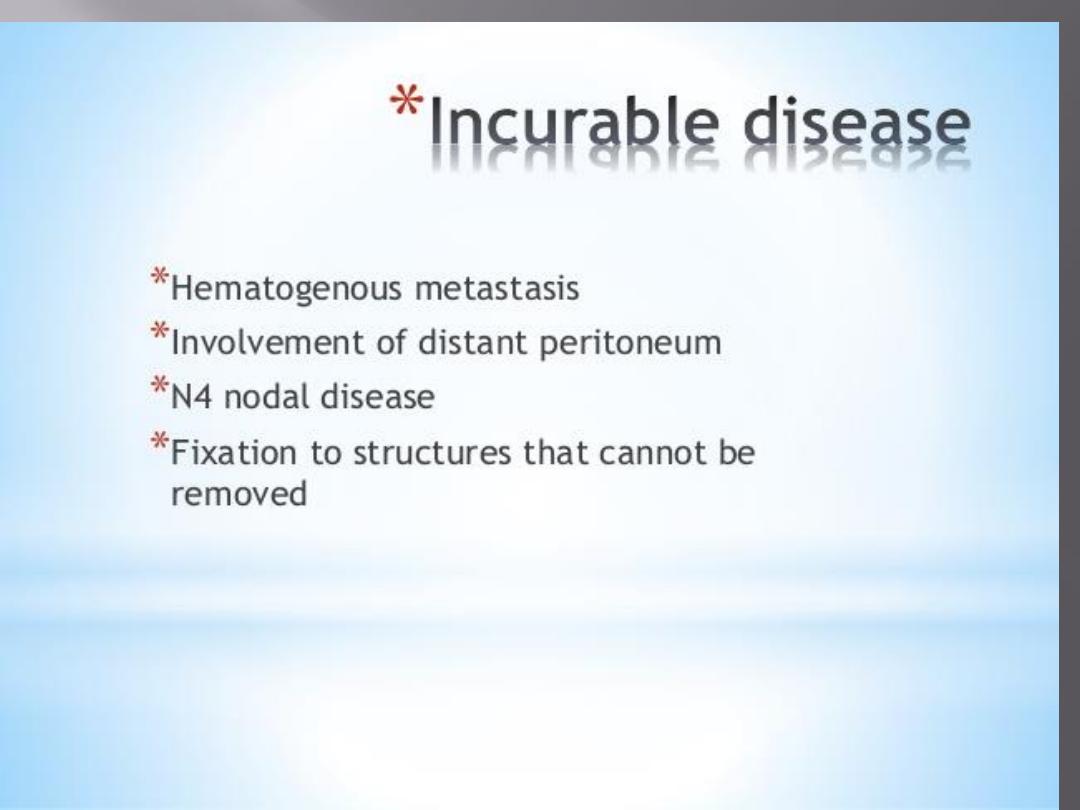
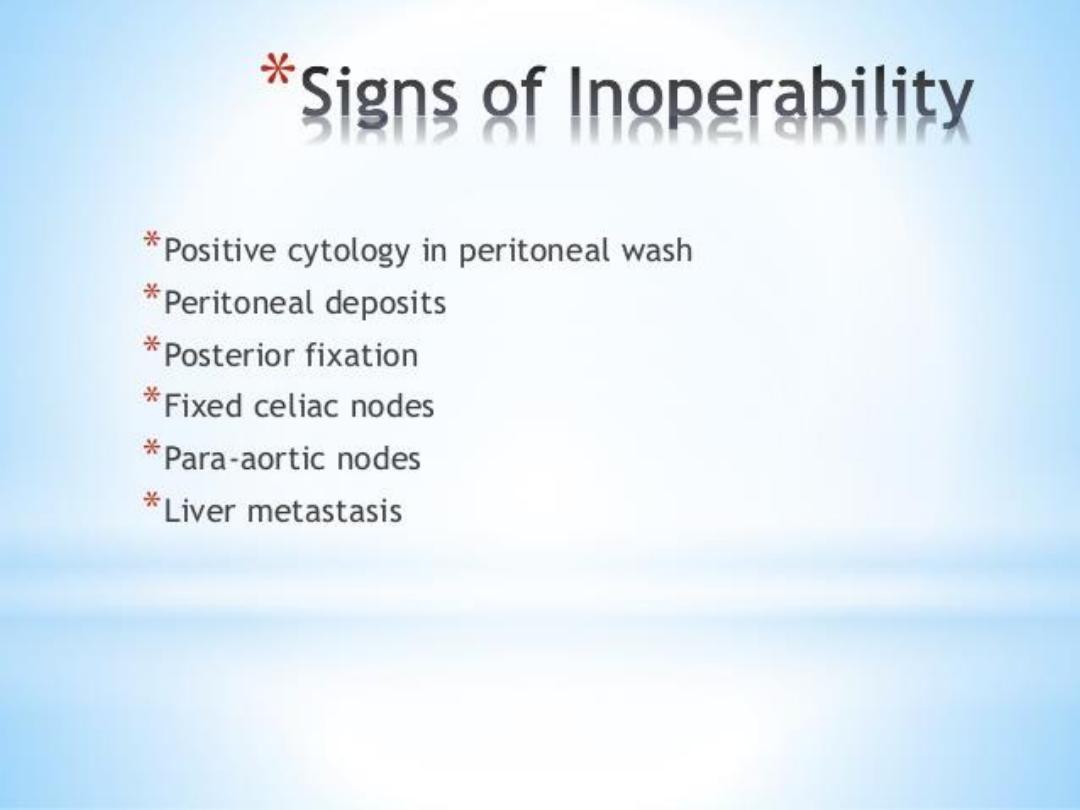
Direct spread pancreas, colon and liver
Lymphatic spread (Troisier’s sign).
Blood-borne metastases liver,lung and bone
Transperitoneal spread:Krukenberg’s tumours and
Sister Joseph’s nodule
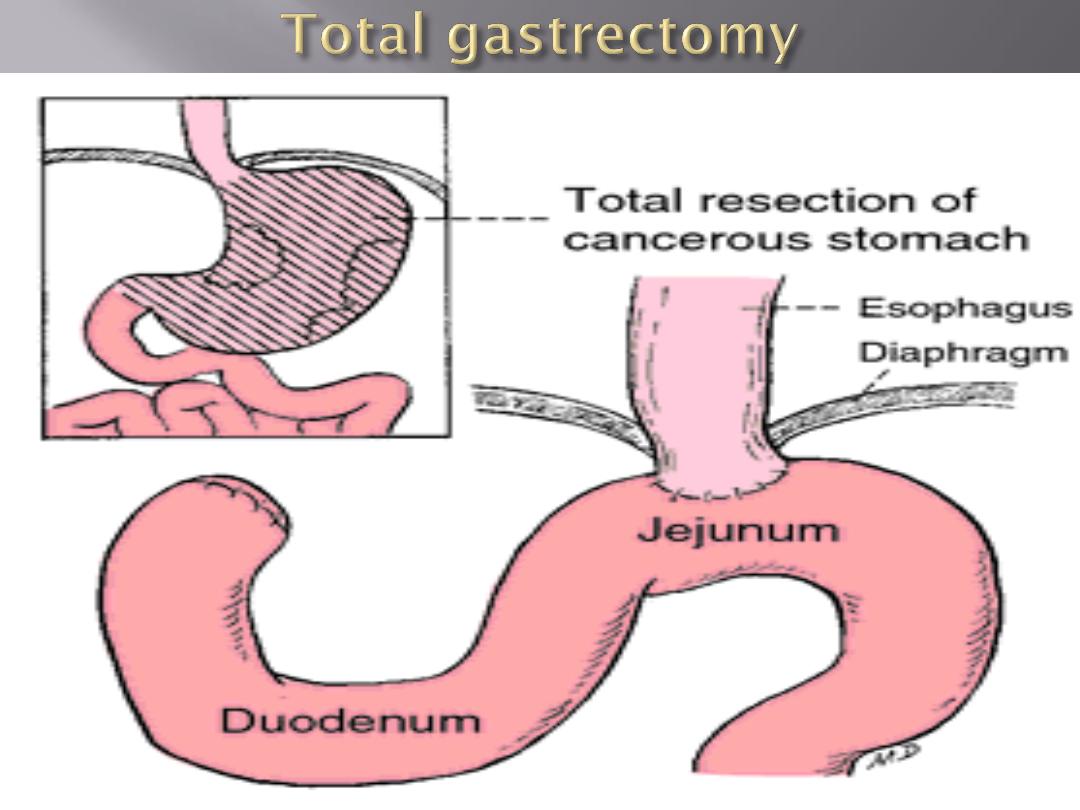
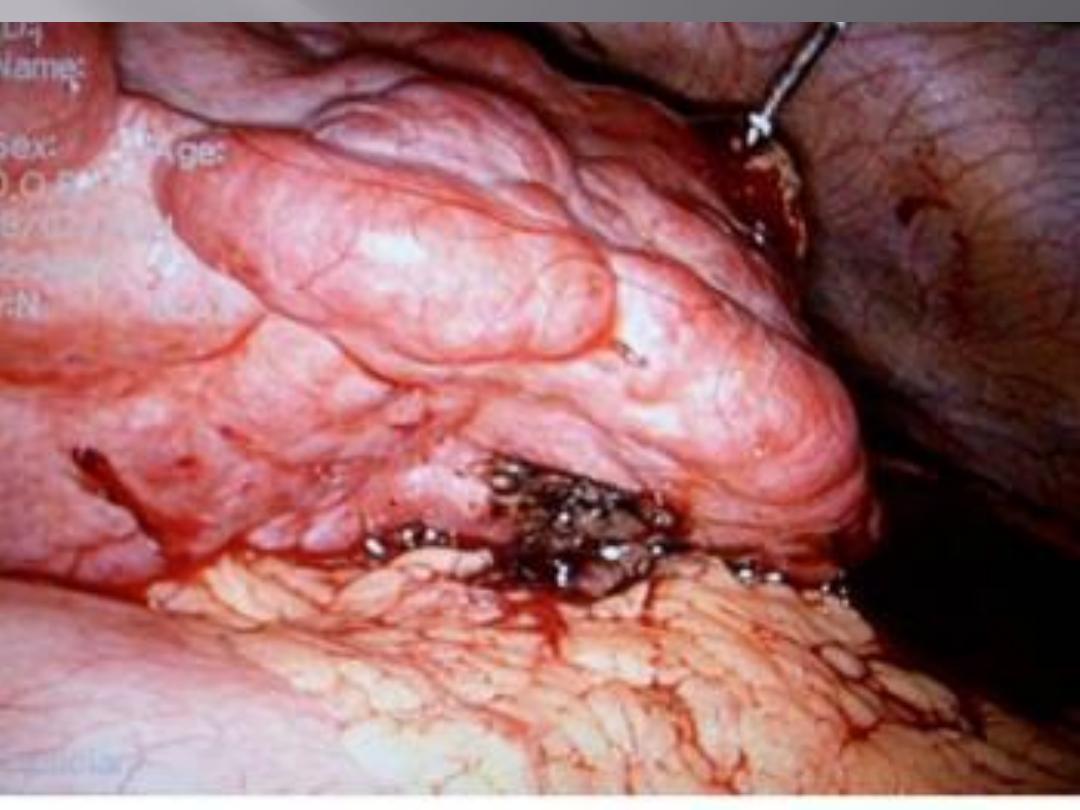
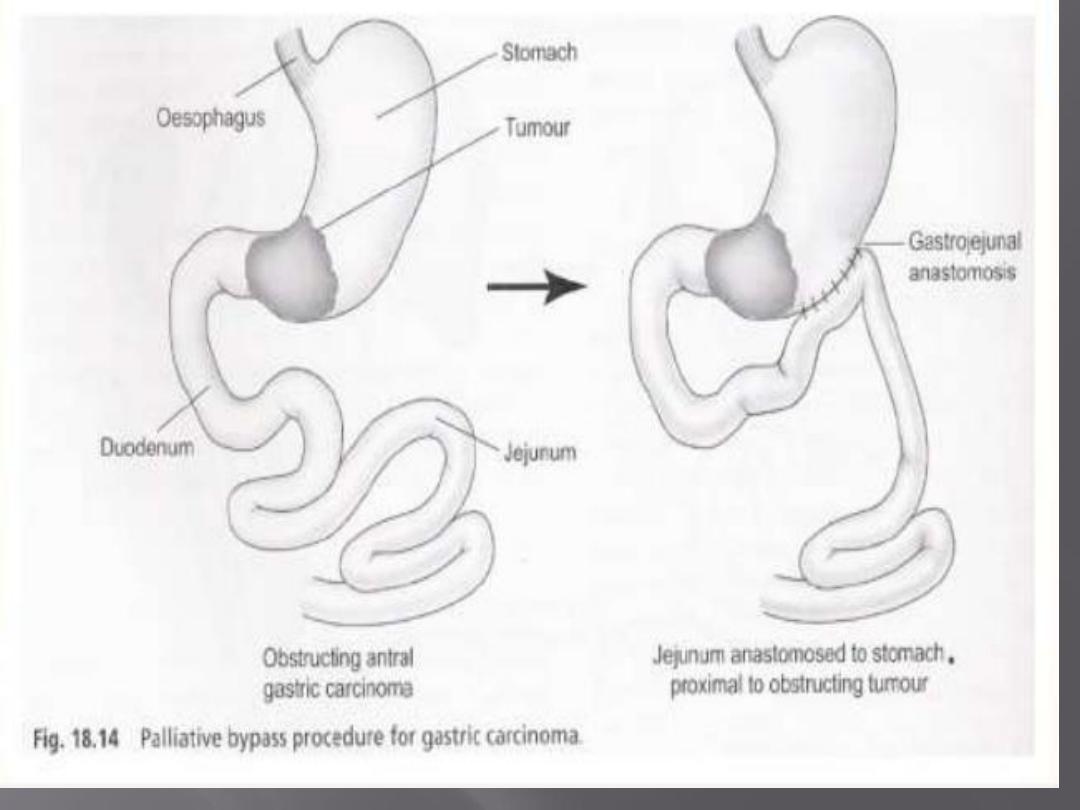
For tumours distally placed in the stomach
This will lead to enterogastric reflux So Roux loop
will solve the problem
Leakage
of the oesophagojejunostomy
fistula
from the wound or drain site
perform
a water-soluble contrast swallow at 5–7 days
after the operation to determine whether the
anastomosis is intact
leakage
from the duodenal stump
Paraduodenal
collections can be drained radiologically
Biliary
peritonitis requires a laparotomy and peritoneal
toilet
secondary
haemorrhage from the exposed or divided
blood vessels
obstruction
bleeding
,

Radiotherapy is contraversal
Chemotherapy by :epirubacin, cis-platinum and
infusional 5-FU or an oral analogue such as
capecitabine
Gastric cancer is one of the most common causes of cancer death
in the world
The outlook is generally poor, owing to the advanced stage of
the tumour at presentation
Better results are obtained in Japan, which has a high population
incidence, screening programmes and a high quality surgical
treatment
The aetiology of gastric cancer is multifactorial, but H. pylori is
an important factor for distal but not proximal gastric cancer
Early gastric cancer is associated with very high cure rates
Gastric cancer can be classified into intestinal and diffuse types,
the latter having a worse prognosis

In the West, proximal gastric cancer is now more
common than distal cancer and is usually of the
diffuse type
Spread may be by lymphatics, blood, transcoelomic or
direct, but distant metastases are uncommon in the
absence of lymph node involvement
The treatment of curable cases is by radical surgery
and removal of the second tier of nodes (around the
principal arterial trunks) may be advantageous
Gastric cancer is chemosensitive and chemotherapy
improves survival in patients having surgery for the
condition and in advanced disease

50 per cent will be found in the Stomach
tumours of mesenchymal origin and are observed equally
in males and females
mutation in the tyrosine kinase c-kit oncogene.
sensitive to the tyrosine kinase antagonist imatinib, an 80
per cent objective response rate
size and mitotic figures index are the best predictors of
metastasis.
GIST comprise 1–3 per cent of all gastrointestinal neoplasia.
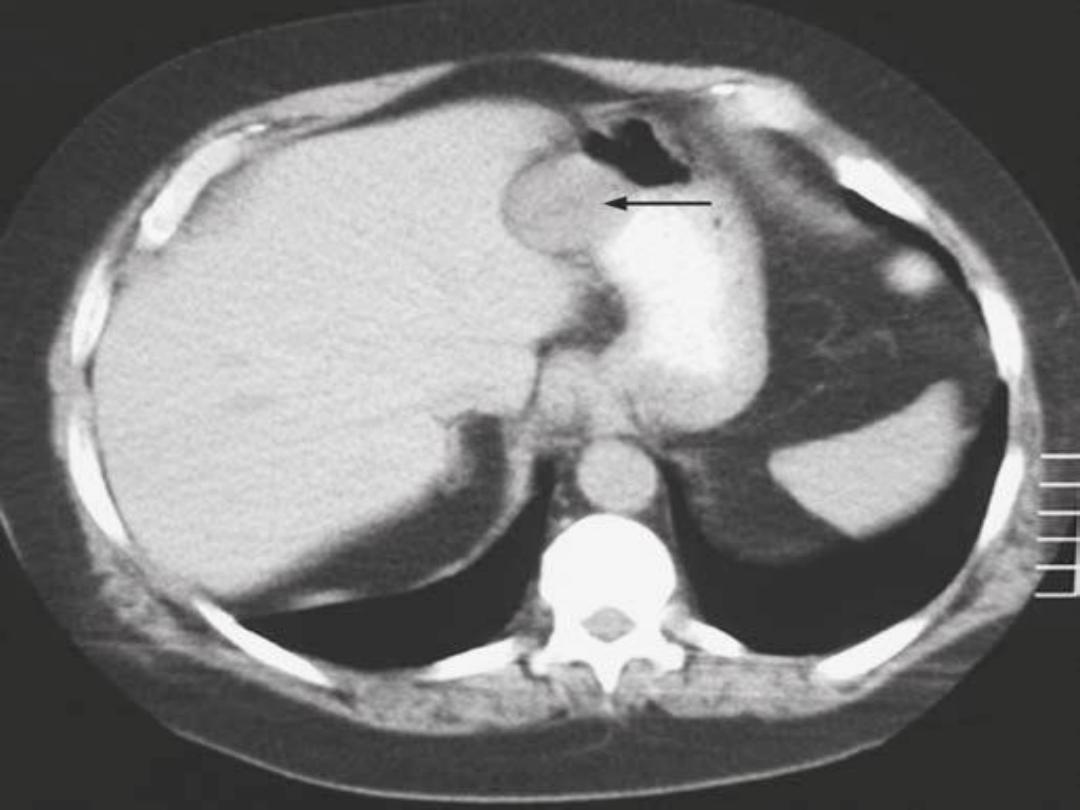
The only ways that many stromal tumours are recognised
are either that the mucosa overlying the tumour ulcerates leading to bleeding,
or that they are noticed incidentally
at endoscopy.
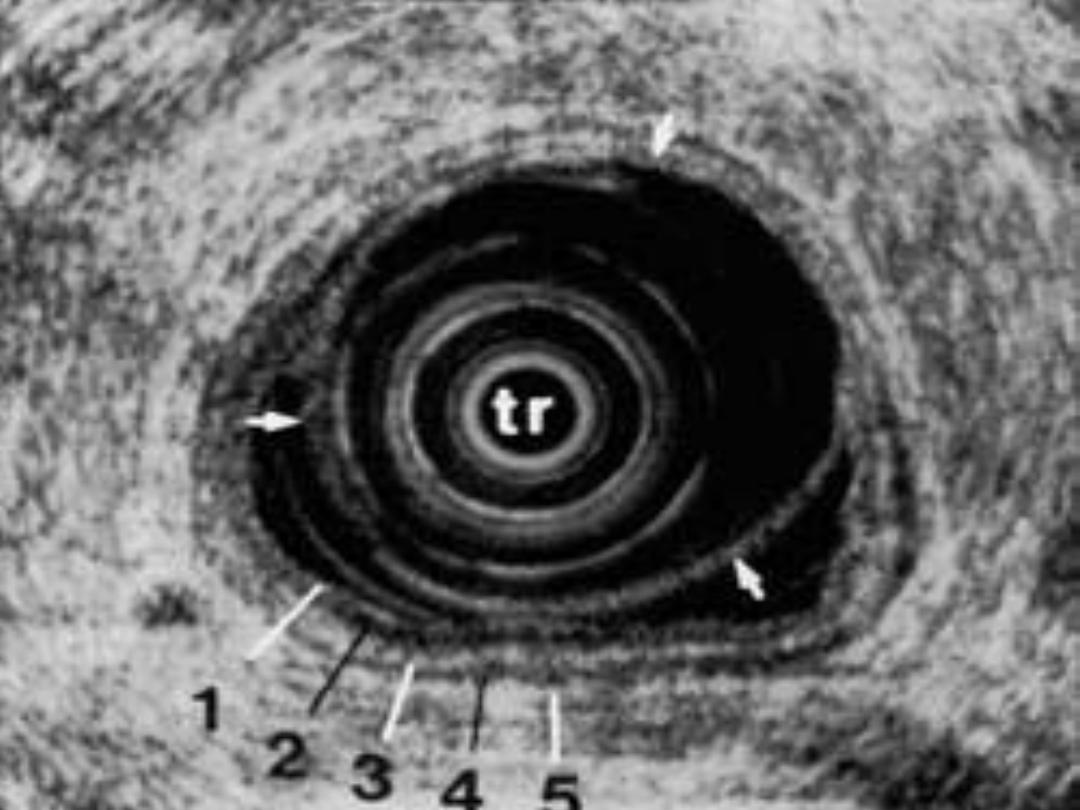
Targeted biopsy by endoscopic ultrasound is more helpful
Tumours over 5 cm in diameter should be considered to have metastatic
potential.
surgery is the primary mode of treatment
lymphadenectomy is not required
The prognosis of advanced metastatic GIST has been dramatically improved
with imatinib chemotherapy but resection of metastases, especially from
the liver, still has an important role


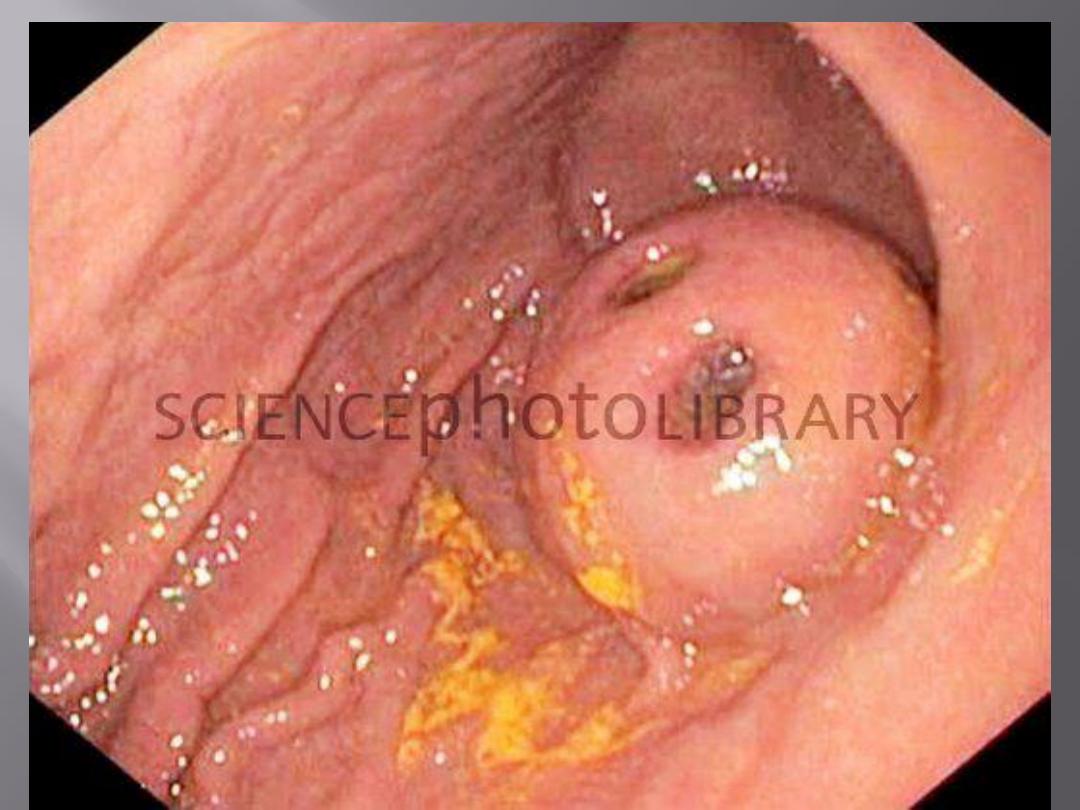
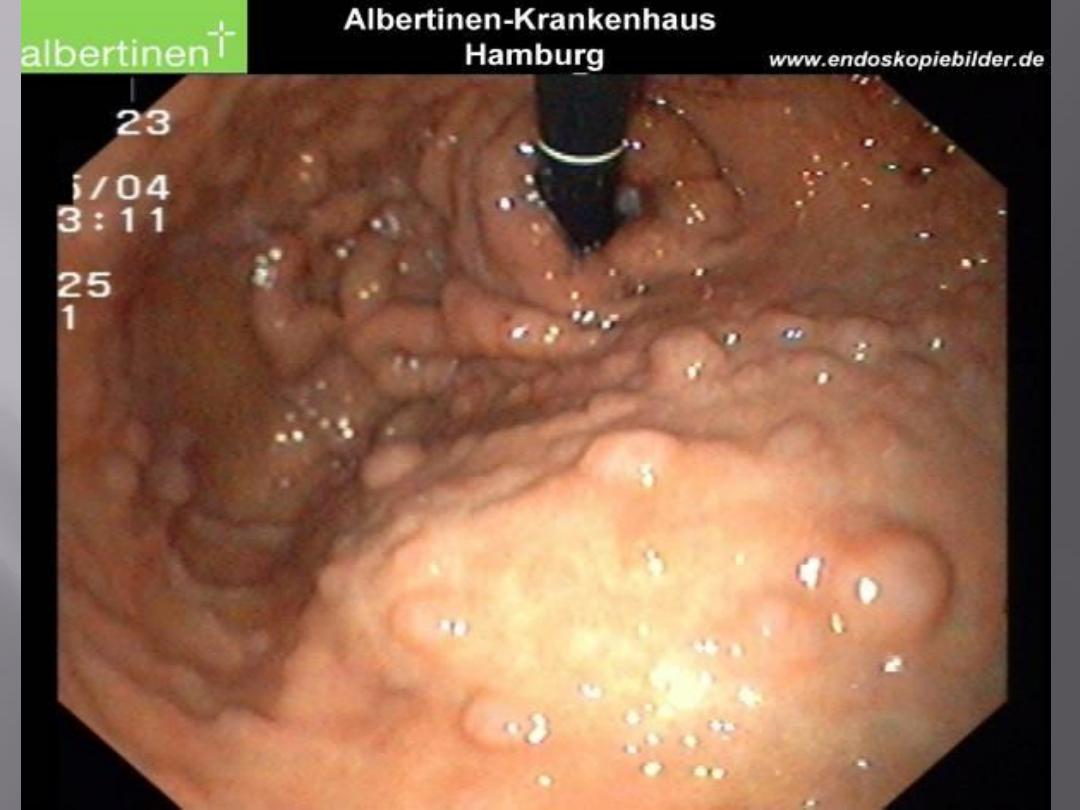
It is first important to distinguish primary gastric
lymphoma from involvement of the stomach in a
generalised lymphomatous process
incidence of lymphoma increasing
accounts for approximately 5 per cent of all gastric
Neoplasms
Common in 6
th
decade
pain, weight loss and bleeding
Acute presentations(
POUB
)
obstruction, are not common

B cell derived
the tumour arising from the mucosa-associated lymphoid
tissue (MALT)
Diffuse mucosal thickening, which may ulcerate
Diagnosis is made as a result of the endoscopic biopsy
CT scans of the chest
abdomen and bone marrow aspirate are required, full
blood count
early gastric lymphomas may regress and disappear when
the Helicobacter infection is treated.
Treatment: surgery although some prefer chemoRx??
Benign : villous adenoma(FAP), periampullary area and
premalignant
Doudenal adenocarcinoma: uncommon, ass. With FAP
most common site for adenocarcinoma arising in the
small bowel.
anaemia due to ulceration of the tumour or obstruction
as the polypoid neoplasm begins to obstruct the
duodenum.
obstructive jaundice
70 per cent of the patients have resectable disease
The five-year survival rate is in the region of 20 per
cent
Curative surgical treatment(Whiplle procedure)


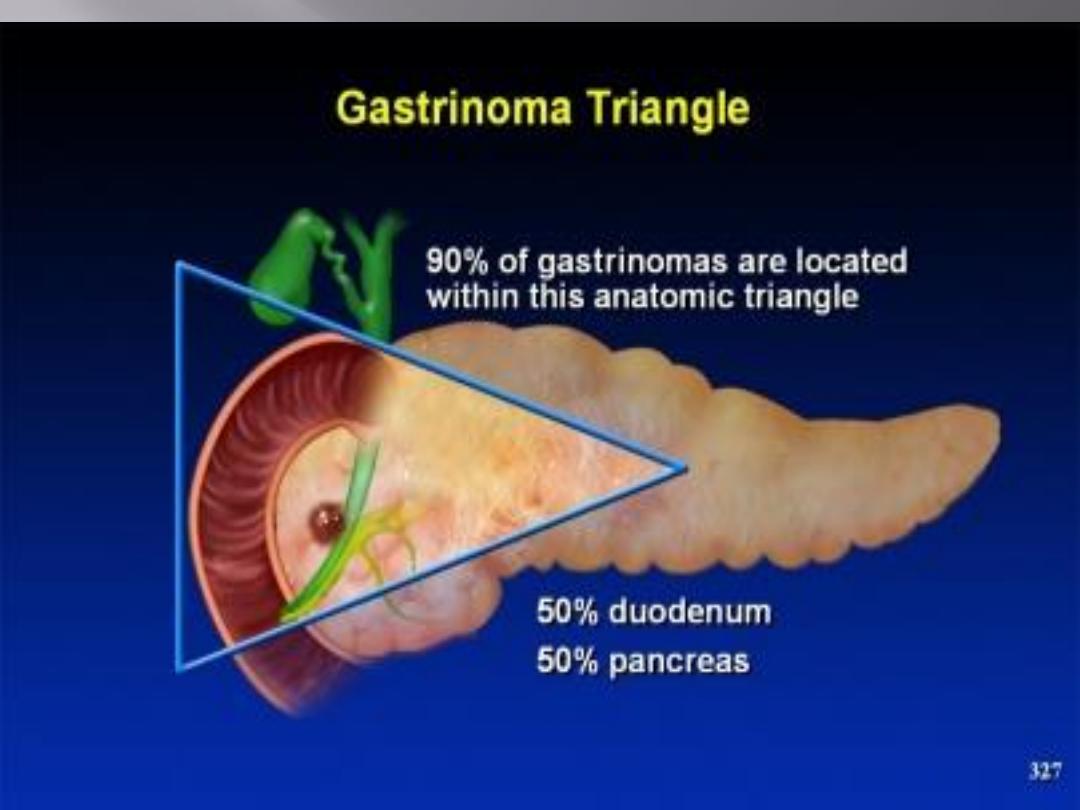
Found in doudenum and head of pancreas
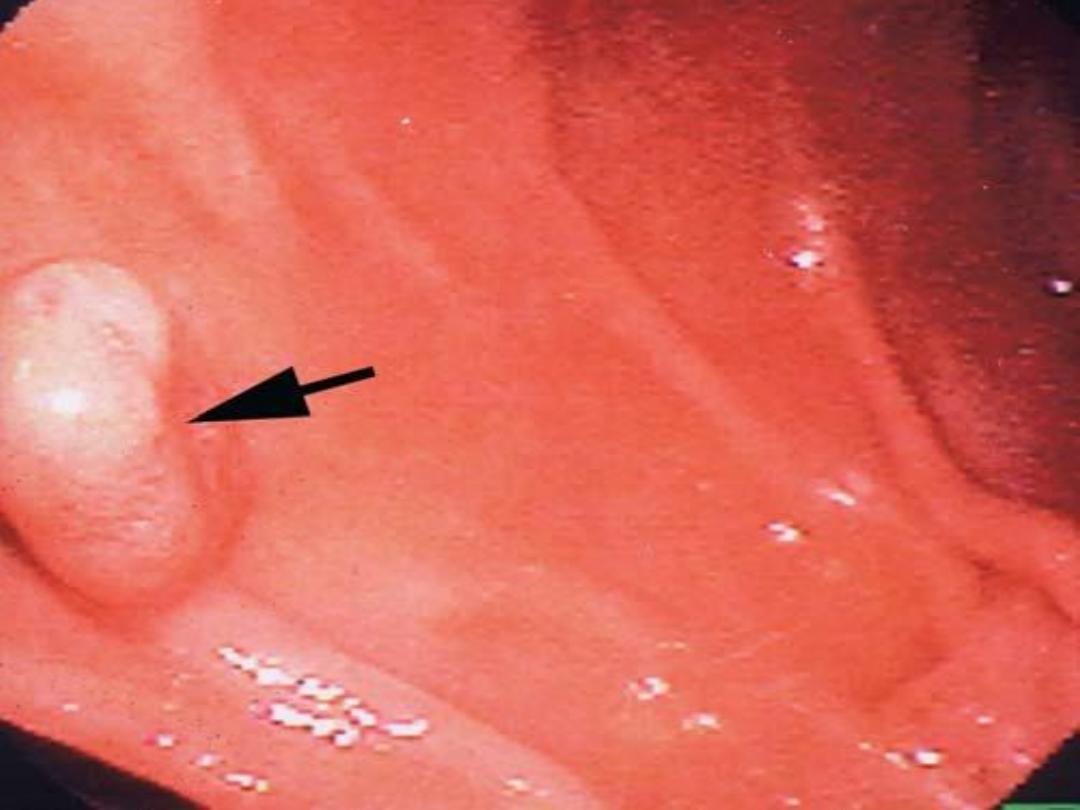
It is a cause of persistent peptic ulceration
sporadic or associated with the autosomal dominantly
inherited multiple endocrine neoplasia (MEN) type I
PASSARO triangle
Dx:
Fasting serum gastrin
In case of moderate hypergastrinemia, a secretin
stimulation test can help in the diagnosis
Localization by somatostatin scintigraphy(octeriotide
scan)
Rx : PPI and surgery
Doudenal causes
Pancreatic causes
Superior mesentric artery syndrome
Metastasis from colorectal and gastric CA
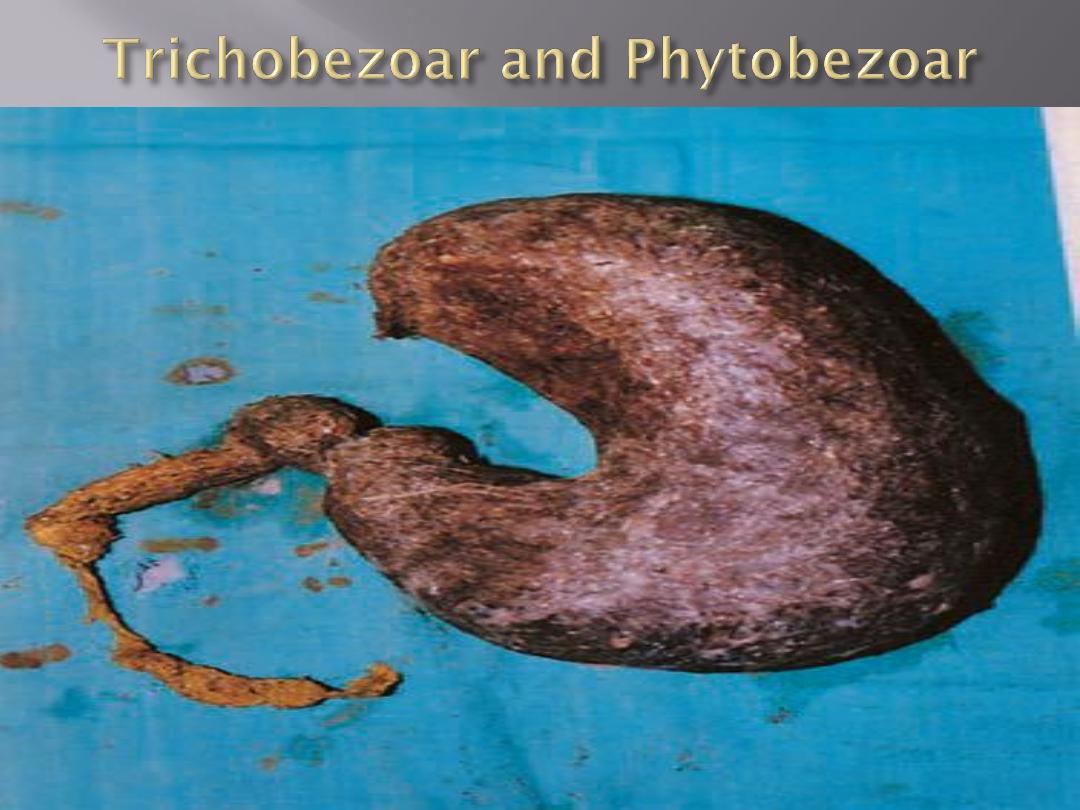
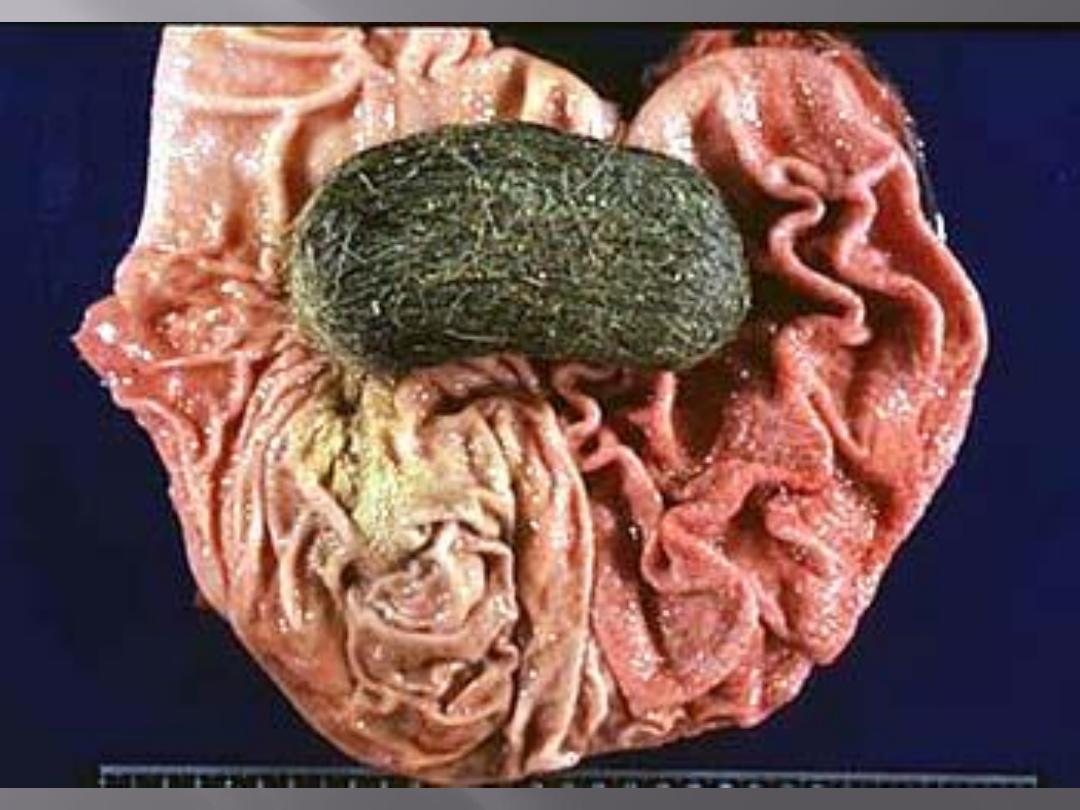

Rotation of the stomach usually occurs around the axis
and between its two fixed points: cardia& pylorus
horizontal (organoaxial)common
vertical (mesenteroaxial) direction
Associated with a large diaphragmatic defect
(paraoesophageal herniation)
The condition is commonly chronic,
the patient presenting with difficulty in eating
Ischemia when acutely presented
contrast radiograph is superior to endoscopy in Dx
Diphragmatic defect repair with mesh
Seperation of stomach from tansverse colon
Anterior gastopexy
