PHYSIOLOGY OF MUSCLE
Morphology of Skeletal Muscle FiberAbout 40 % of the body is skeletal muscle, and another 10 % is smooth and cardiac muscle .
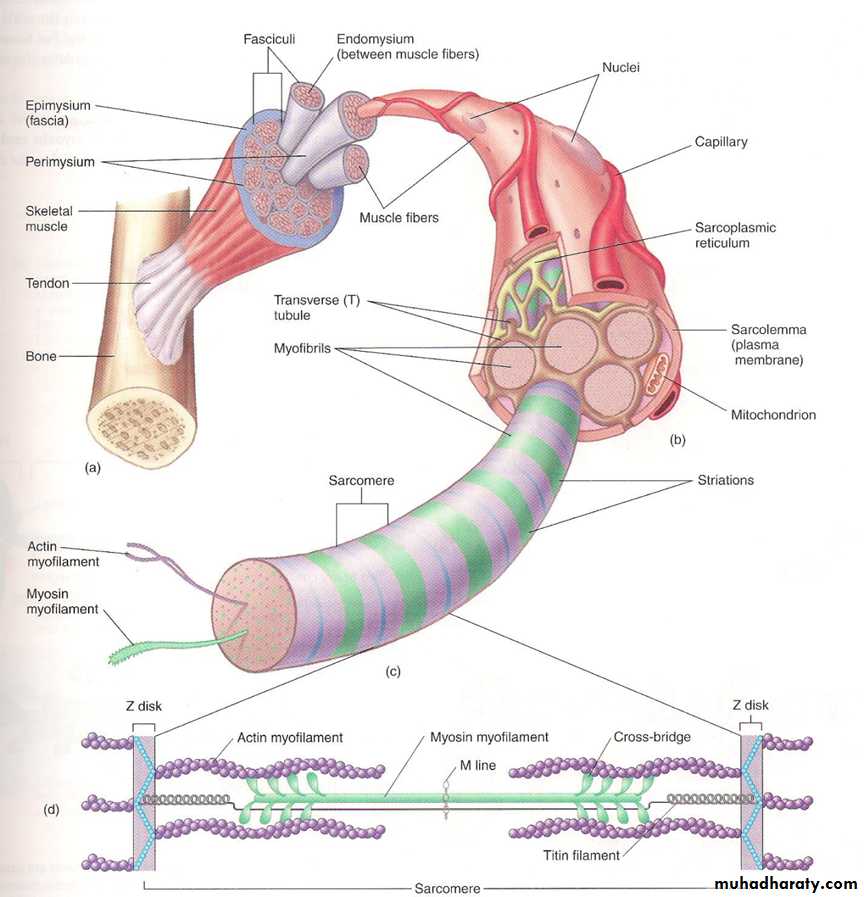
Skeletal muscle is a striated, voluntary (neurogenic) muscle, i.e. needs nerve supply to work. All skeletal muscles are composed of many fibers. Muscle fiber is a single cell, multinucleated cylindrical shape surrounded by cell membrane called sarcolemma and each fiber extends the entire length of the muscle and is usually innervated by only one nerve ending, located near the middle of the fiber. Each of these muscle fibers is made up of successively smaller subunits called (myofibrils). Each myofibrils composed of actin and myosin about 1500 myosin filaments and 3000 actin filaments. (fig 1)
Actin and myosin
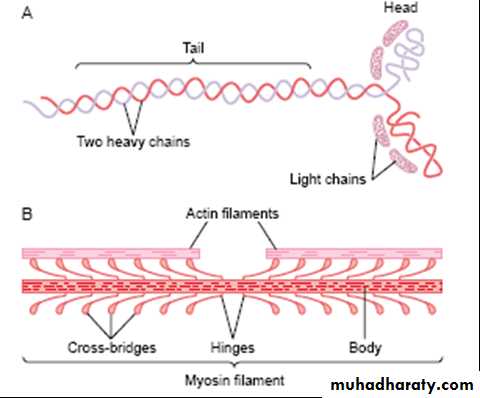
The thick filament (myosin): composed of several hundreds of myosin molecules, each molecule consists of 6 polypeptide chains (4 light and 2 heavy chains). 2 heavy chain wrap spirally form the tail and on the end of the tail folded bilaterally will form the arm and the head. The head of myosin molecule form the cross-bridges which bind with actin. The head of myosin molecule contains actin binding sites and 2 ATPase activity sites (to produce the energy necessary for contraction). (Fig 2)(Fig2)
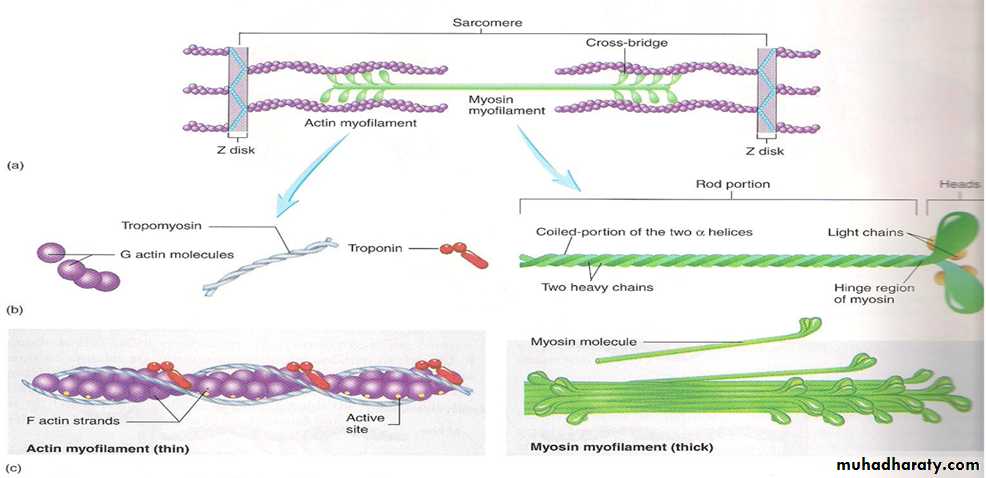
The thin filament (actin): actin filaments composed of three proteins, actin, tropomyosin and troponin(fig 3)Actin contain active sits on its surface in which the cross –bridges of myosin attached
Tropomyosin: lie on the top of the active site of actin strands
Troponin: are 3 loosely bound protein subunits
-Troponin I :has strong affinity to actin .The troponin(I) binds to actin so inhibit interaction between actin and myosin
-Troponin C :has strong affinity to Ca ion, which is necessary to initiate contraction
-Troponin T :has affinity for tropomyosin form troponin tropomyosin complex
(Fig 3)
The myosin and actin filaments partially interdigitate and thus cause the myofibrils to have alternate light and dark bands, as The light bands contain only actin filaments and are called I bands . The dark bands contain myosin filaments, as well as the ends of the actin filaments where they overlap the myosin, and are called A bands, therefore the entire muscle fiber has light and dark bands giving the skeletal and cardiac muscle the striated appearanceThe ends of the actin filaments are attached to the Z disc. From this disc, these filaments extend in both directions .actin held in place by Z disc
myosin held in place by Z disc but its attachment to Z-disc by protein titin
Z -disc: is a filamentous protein passes across the myofibril and from one myofibrils to anther attaching myofibrils to one anther. The ends of the actin filaments attached to Z-disc
Sarcomere: is the portion of myofibrils that lie between two successive Z –disc. It is a smallest functional unit of amyofibril necessary to produce contraction (fig 3)
Sarcolemma :cell membrane of muscle fiber
Sarcoplasm :is the cytoplasm of the muscle fiber contain mitochondria, myofibrils and sarcoplasmic reticulum
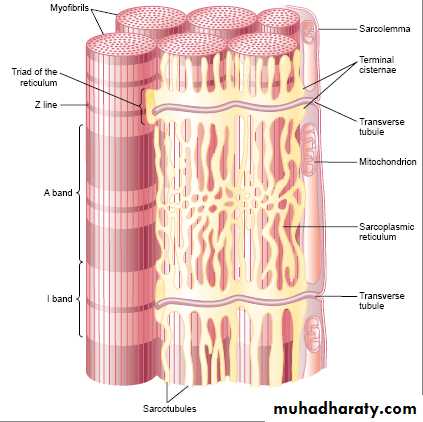
The sarcotubular system: It is composed of:
a)The transverse tubules(T-tubules): originate as invaginations from cell membrane, penetrating the muscle fiber from one side to the opposite side, thus communicating with the ECF. T-tubules help for rapid transmission of action potential from the membrane deep into the muscle.
b) The sarcoplasmic reticulum which composed of:
1-Longitudinal tubules.
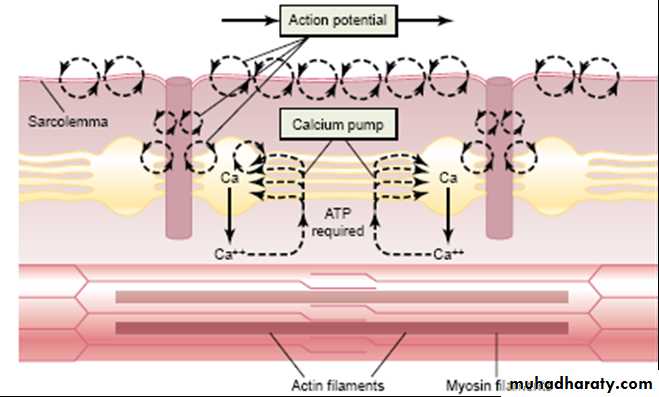
2-Terminal cisterns: large chambers adjacent to T-tubules giving the appearance of triad(1 T-tubule and 2 cisternae). It stores calcium ions with abundant Ca channels and Ca pumps.(fig 4 ).
Fig 4
Molecular mechanism of muscle contraction
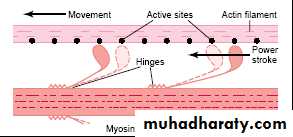
In the relaxed muscle the troponin-I is tightly bound to actin; tropomyosin covers the active sites of actin thus, troponin-tropomyosin complex represent the relaxing proteins which inhibit interaction between actin and myosinWhen the Ca ion bind with troponin C this uncover the active sites of the actin. Then the activated head of myosin cross-bridges attaches to an active sites of actin, here the head automatically tilts towards the arm (called power stroke) so dragging the actin filaments along with it immediately after tilting the head released from the active site then return to its normal perpendicular direction and then it combined with new active site of actin, then the head tilts again, and the actin filament moves another step. Thus, the heads of the cross-bridges step by step walk along the actin filament, pulling the ends of two successive actin filaments toward the center of the myosin this is called “walk-along” theory .(fig 5)
Fig 5
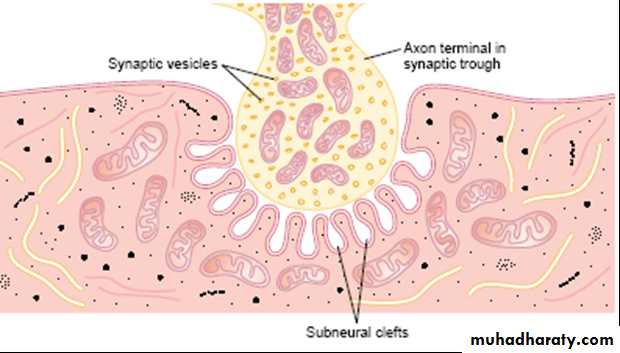
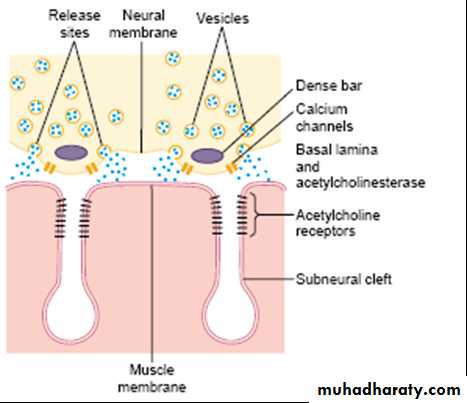
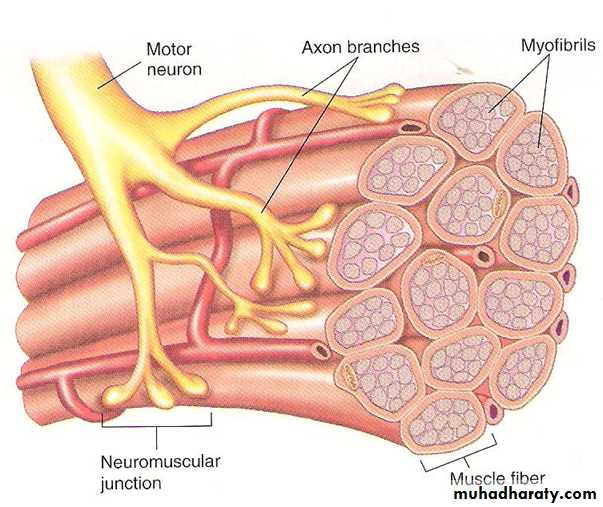
neuromuscular junction: As the motor nerve reaches the muscle fiber, it loses its myelin and divides into a number of terminals. The axon terminal contains many small vesicles of the neurotransmitter acetylcholine. The nerve ending invaginates into a thickened, folded depression in the muscle membrane called the motor end plate (figure 6).Usually there is one junction for each muscle fiber, this invagination is called synaptic gutter and the space between the axon terminal and the muscle fiber is called synaptic cleft(contain acetylcholinesterase that destroy acetylcholine (Ach).Fig 6
Excitation- contraction coupling1-when action potential travel along a motor nerve to its ending ,voltage gated calcium channels(near dense bars ) open and allow calcium ions to diffuse to the interior of the nerve terminal.
2- The calcium ions exert an attractive influence on the acetylcholine vesicles, drawing them to the neural membrane adjacent to the dense bars. The vesicles then fuse with the neural membrane and empty their acetylcholine into the synaptic space by the process of exocytosis
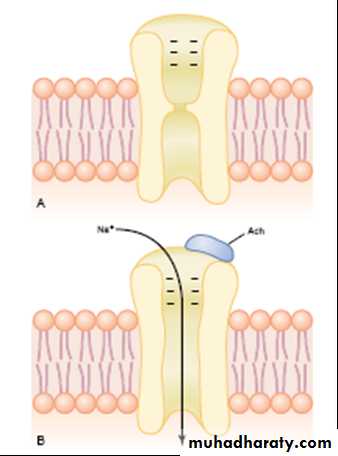
3-The acetylcholine open the acetylcholine- gated channels, which allows sodium ion to flow into muscle fiber, this initiate end plate potential (The sudden entrance of sodium ions into the muscle fiber causes the electrical potential inside the fiber to increase in the positive direction as much as 50 to 75 millivolts), which is necessary to initiate an A.P
4-The action potential travels along the muscle fiber membrane causing the sarcoplasmic reticulum to release calcium ion into myofibrils
5-The Ca ions uncover the active sites of actin and initiates attractive force between the actin and myosin cross-bridges causing the actin filaments to slid inward among the myosin filaments .This is the contractile process which is occur by sliding filament mechanism. The energy for this mechanism is supplied by the ATP cleavage by ATPase enzyme present in the myosin head.
6-After a fraction of a second the Ca ion are pumped back into the sarcoplasmic reticulum where they remain stored until another muscle A.P arrives again .this removal of Ca ion from myofibrils causes muscle contraction to cease.
Note :When active re-pumping of calcium is inhibited, relaxation cannot occur and muscle stays in contraction.
Why sodium ions flow through the acetylcholine gated channels than any other ions?
1-high concentration of sodium ions in the extracellular fluid
2-the very negative potential on the inside of the muscle membrane, –80 to –90 millivolts, pulls the positively charged sodium ions .
The acetylcholine then it is removed rapidly by two means:
(1)Most of the acetylcholine is destroyed by the enzyme acetylcholinesterase
(2) A small amount of acetylcholine diffuses out of the synaptic space or re-uptake by process of pinocytosis. fig (7 ,8)
fig 7
fig 8
Muscle Action Potential
Almost everything regarding initiation and conduction of action potentials in nerve fibers applies equally to skeletal muscle fibers, except for quantitative differences.1-Resting membrane potential: about –80 to –90 millivolts in skeletal fibers—the same as in large myelinated nerve fibers.
2-Duration of action potential: 1 to 5 milliseconds in skeletal muscle—about five times as long as in large myelinated nerves
3-Velocity of conduction: 3 to 5 m/sec—about 1/13the velocity of conduction in the large myelinated nerve fibers .
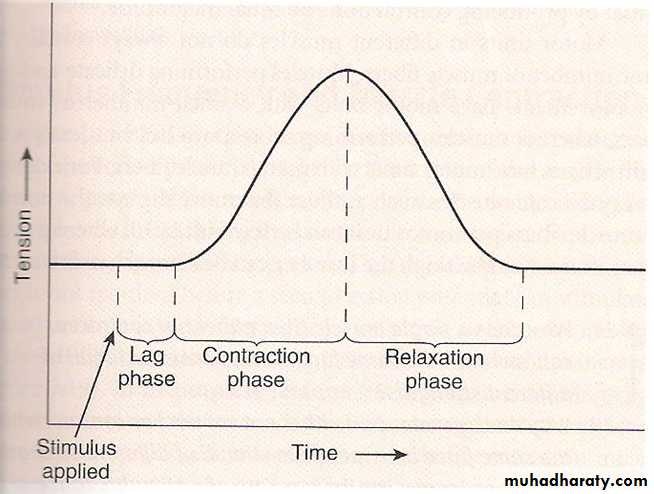
Simple muscle twitch:
The contraction of a muscle in response to a stimulus , its occur in 3 parts: (fig 9)
latent period :The time between application of stimulus to the motor nerve and the beginning of contraction
contraction period : the time during which contraction occurs, muscle shortens & does its work
relaxation period: time during which relaxation occurs ,muscle elongates & returns to original position
refractory period: the refractory period is short which means that skeletal muscle can under go summation and tetanization via repeated stimulation (e.g. Lifting heavy weight)
fig 9
Note :An action potential is an electrochemical event(less than 2 ms)
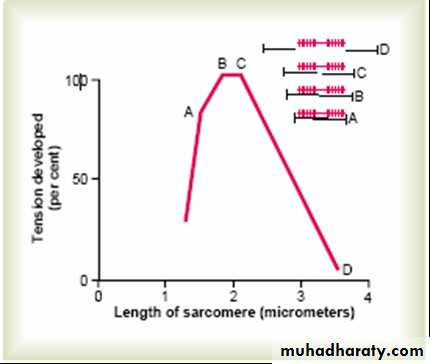
But contraction is a mechanical event which requires up to 1 second to occur.Degree of actin and myosin filaments overlaps on the tension developed by the contracting muscle.
- At a point A- the two actin filaments begin to overlapped causing muscle tension to decrease , the sarcomere length less than 2 micrometer .
At a point B and C- at a sarcomere length 2 micrometer, full tension is maintained because all the cross– bridges of myosin overlapped by the actin at this length it's capable of generating maximum force of contraction
At a point D- at very long sarcomere length a muscle can not develop tension because there is no over lap between actin and myosin filaments
(fig10)
Fig 10
Motor unitAll the muscle fibers which is innervated by a single motor nerve are called motor unit(fig 11)
Muscle that react rapidly for precise function may have only 2-3 muscle fibers in motor unit e.g laryngeal muscle.
While muscle that don’t need precise function may have 100 muscle fiber in motor unit.
fig 11
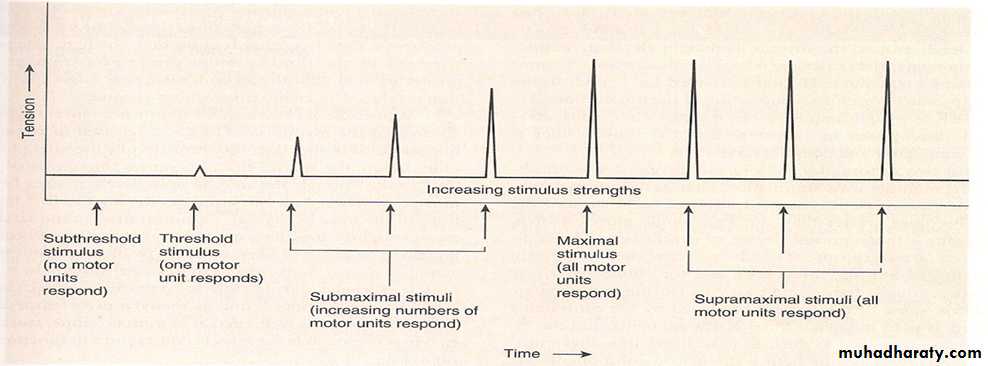
Stimulus strength and muscle contraction
Muscle tension = force exerted by contracting muscle; force is applied to a load
Load = weight of object being acted upon
An isolated skeletal muscle fiber produces contraction of equal force in response to each action potential (all-or-none law of skeletal muscle contraction).
When brief electric stimuli of increasing strength are applied to muscle fiber ,the following events occur:
1-Subthreshold stimulus does not produce an AP, and no muscle contraction occurs.
2-A threshold stimulus produces an AP and results in contraction of the muscle fiber.
3-A stronger than threshold stimulus produces an AP of the same magnitude as the threshold stimulus and therefore produces an identical contraction.
Like individual muscle fiber , motor units respond in all-or-none fashion.
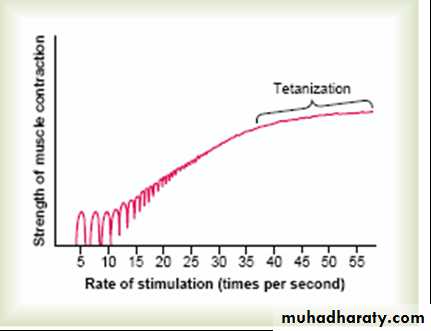
Increasing the force of contraction occurs by summation and in two ways:
1-Multiple motor unit Summation. By increasing the number of motor units contracting at the same time. When the central nervous system sends a weak signal to contract a muscle, smaller number of motor units may be stimulate Then, strength of the signal increases, larger and larger number of motor units begin to be excited as well.
whole muscle responds to stimuli in a graded fashion, (figure 12). which means the strength of the contraction can range from weak to strong depending on the strength of the stimuli.
fig 12
2-Frequency Summation andTetanization by increasing the frequency of contraction. As the frequency increases, here comes a point where each new contraction occurs before the preceding one is over. As a result, the second contraction is added to the first one, so that the total strength of contraction rises progressively.When the frequency reaches a critical level, the successive contractions become so rapid that they fuse together, and the whole muscle contraction appears to be completely smooth and continuous without relaxation This is called tetanization .So that any additional increase in frequency beyond that point has no further effect This occurs because Ca ion is accumulated in sarcoplasm.(fig 13)
fig 13
Types of muscle contraction:
Two types, isometric and isotonicIsometric: tension of muscle increase but do not change in length e.g when person push against the wall
Isotonic contraction: there is change in length but the tension not changed e.g lifts an object
Most contractions are a mixture of the two(e.g: running)
Types of muscle fibers:
Two types according to the twitch duration fast muscle fiber (few) and slow muscle fiber (hundreds). Most of body muscles are a mixture of the two types.
Fast muscle fibers
a-Large fibers and innervated by large nerve
b-Extensive sarcoplasmic reticulum for rapid release of calcium ions to initiate contraction.
c-Large amounts of glycolytic enzymes for rapid release of energy by the glycolytic process.
d-Less blood supply and few mitochondria because oxidative metabolism is of secondary importance.
e-easy fatigability
f-Adapted for very rapid and very strong contraction(short distance running, jumping.)
g-less myoglobin(an iron containing protein similar to hemoglobin in red blood cells) ,deficit of red myoglobin in fast muscle gives it the name white muscle
Slow Fibers
a-Smaller fibers. and innervated by smaller nerve fibers.
b- More extensive blood vessel system and capillaries to supply extra amounts of oxygen.
c-resist fatigue
d-Greatly increased numbers of mitochondria, to support high levels of oxidative metabolism.
d-Contain large amounts of myoglobin red muscle. The myoglobin gives the slow muscle a reddish appearance and the name
e-Adapted for prolonged muscular activity(marathon races, postural muscles which support body against gravity(
Energy expenditure during contraction:
Energy is needed for
-Sliding of actin on myosin filaments1
2-Repumping of calcium ions from sarcoplasm into sarcoplasmic reticulum to start muscle relaxation.
-3-Maintenance of resting membrane potential by Na-K pump
Source of energy for muscle contractions
1-The immediate source of energy is ATP.The concentration of ATP in the muscle fiber is sufficient to maintain full contraction for only 1 to 2 seconds
2-glycolysis of glycogen (previously stored in the muscle cells). The glycolytic reactions can occur even in the absence of oxygen
3-oxidative metabolism. (This means combining oxygen with the glucose and fatty acids) to liberate ATP.
Muscle Fatigue: Prolonged and strong contraction of a muscle leads to the state of muscle fatigue. Muscle fatigue is directly proportion to the rate of depletion of muscle glycogen and ATP.
Skeletal Muscle Tone: Even when muscles are at rest they are in state of continuous small degree of contraction called muscle tone which is probably due to reflex impulses from the spinal cord. Muscle tone decreases during sleep and absent in death
Myasthenia Gravis
Is an autoimmune disease in which the patients have developed antibodies against their own acetylcholine-gated ion channels. The end plate potentials that occur in the muscle fibers are too weak to stimulate the muscle fibers and the patient dies of paralysis.
Drugs That Stimulate the Muscle Fiber by Acetylcholine-LikeAction.
Many compounds, including methacholine, carbachol,and nicotine, have the same effect on the muscle fiber as does acetylcholine. The difference between these drugs and acetylcholine is that the drugs are not destroyed by cholinesterase
Drugs That Stimulate the Neuromuscular Junction by Inactivating Acetylcholinesterase.
Neostigmine, physostigmine, inactivate the acetylcholinesterase in the synapses so that it no longer hydrolyzes acetylcholine. Therefore, acetylcholine accumulates and stimulates the muscle fiber repetitively
Drugs That Block Transmission at the Neuromuscular Junction.
A drugs can prevent passage of impulses from the nerve ending into the muscle. as, D-tubocurarine this drug compete with acetylcholine on its receptor sites.
Poisoning with curare(Ach receptor blocker) cause weak endplate potential, the same effect occurs with the botulinium toxin(bacterial toxin)which decreases the release of Ach by nerve terminals
Muscle Hypertrophy
Forceful muscular activity increases total mass of a muscle. All muscle hypertrophy results from an Increase in the number of actin and myosin filaments in each muscle fiber, causing enlargement the size of the muscle .
Muscle atrophy
Occur when a muscle remains unused for many weeks cause a decreases in muscle mass, the rate of decay of the contractile proteins is more rapid than the rate of replacement.
Rigor
when muscle fibers are completely depleted of ATP, they develop a state of extreme rigidity called rigor, when occur after death it is called rigor mortis, here, all actin filaments bind to myosin filaments permanently in a fixed way no ATP to detach myosin head and SR can not absorb Ca
Physiology of Smooth Muscle
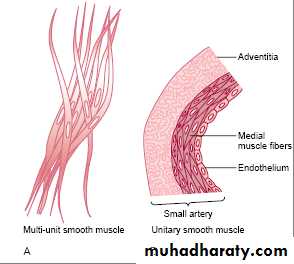
Morphology: smooth muscle is unstriated, involuntary muscle and differ from skeletal and cardiac muscle fiber being much smaller; the sarcoplasmic reticulum is poorly developed. The contractile proteins are actin, myosin, and tropomyosin but no troponin.There are two main types of smooth muscle, the visceral(unitary) and the multiunit (figure 15).
I-Multi-Unit Smooth Muscle.
1-non-syncytial i.e this type of smooth muscle is composed of separate smooth muscle fibers .Each fiber operates independently of the others often is innervated by a single nerve ending2-Neurogenic: controlled by external nerve supply.
3-Contraction not spread widely therefore needed for fine localized contractions (eg: ciliary muscle and iris of the eye)
4-Very sensitive to acetylcholine and noradrenaline
II-Single-unit Smooth Muscle. Also called “unitary” or syncytial or visceral smooth muscle it means a mass of hundreds to thousands of smooth muscle fibers that contract together as a single unit (either the whole muscle contracts or the whole muscle relaxes). The fibers usually are arranged in bundles, and their cell membranes are adherent to one another at multiple points called gap junction through which ions and A.P can flow freely from one muscle cell to the next
e.x gut muscle, bile ducts, ureters, uterus, and many blood vessels.
Fig14
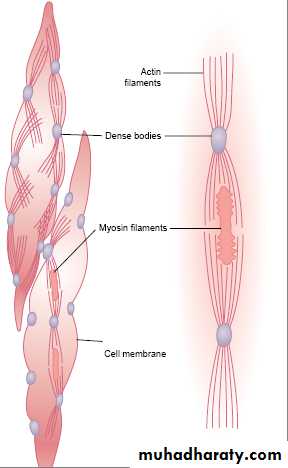
Physical Basis for Smooth Muscle ContractionComparison of contractile unit within a smooth muscle cell with the skeletal muscle
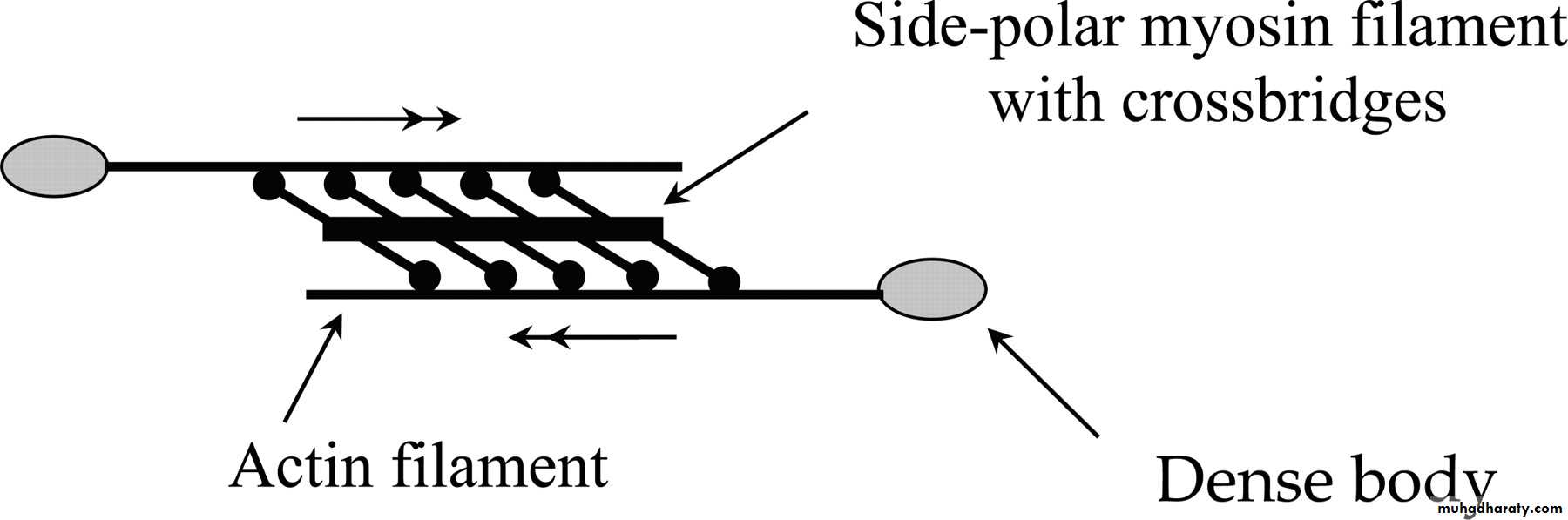
large numbers of actin filaments radiating from two dense bodies; the ends of these filaments overlap a myosin filament. In fact, the dense bodies of smooth muscle serve the same role as the Z discs in skeletal muscle. This contractile unit is similar to the contractile unit of skeletal muscle, but randomly arranged . (Fig 15)
Most of the myosin filaments have “side polar” cross-bridges arranged so that the bridges on one side hinge in one direction and those on the other side hinge in the opposite direction. This allows the myosin to pull an actin filament in one direction on one side while simultaneously pulling another actin filament in the opposite direction on the other side. The value of this organization is that it allows smooth muscle cells to contract as much as 80 per cent of their length.
Fig 15
Comparison of Smooth Muscle contraction with skeletal muscle contractionContraction of smooth muscle also occur by sliding filament mechanism, the difference in contraction are:
I-Although most skeletal muscles contract and relax rapidly, most smooth muscle contraction is prolonged tonic contraction, sometimes lasting hours or even days. This is due to
1-Slow Cycling of the Myosin Cross-Bridges. Their attachment to actin, then release from the actin, and reattachment for the next cycle—is much slower in smooth muscle than in skeletal muscle
2-low Energy Required to Sustain Smooth Muscle Contraction. only1/10 as energy is required to sustain the same contraction in skeletal muscle.
II-Force of Muscle Contraction is often greater than that of skeletal muscle, this is results from the prolonged period of attachment of the myosin cross-bridges to the actin filaments.
III - The role of calcium in excitation-contraction coupling: similar to skeletal muscle with the following differences:
1-The main source of calcium ions is the ECF rather than sarcoplasmic reticulum (which is not well developed) ,therefore, Smooth muscle membrane contains large number of Ca ion channels. .
2-smooth muscle contain tropomyosin but it uncover the active site and does not contain troponin, in state of it the regulatory protein called calmodulin which present in cytoplasm of the cell will activate myosin cross-bridges this occur by:
Calcium ions binds with calmodulin, this binding will cause activation of myosin light chain kinase, a phosphorylating enzyme hydrolyzes ATP and takes the inorganic phosphate (Pi) from the ATP and puts it on the myosin , cause activation of myosin heads this activated head bind with actin and cause muscle contraction. At the end of contraction, Calcium ions are pumped back again to the ECF and to the sarcoplasmic reticulum ,the enzyme myosin phosphatase( located in the fluids of the smooth muscle cell), which splits the phosphate from the myosin head then the cycle stop and contraction ceases and causes relaxation.
Neuromuscular Junctions of Smooth Muscle
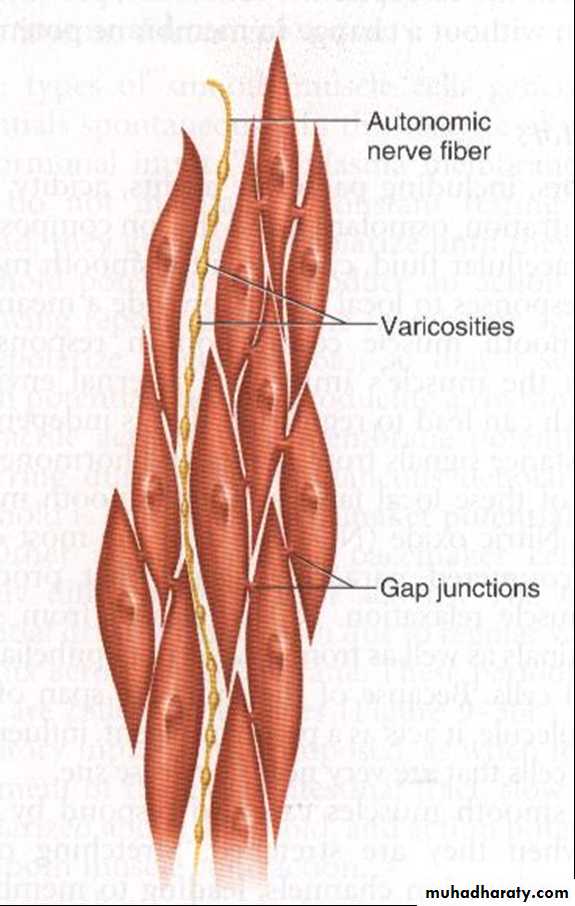
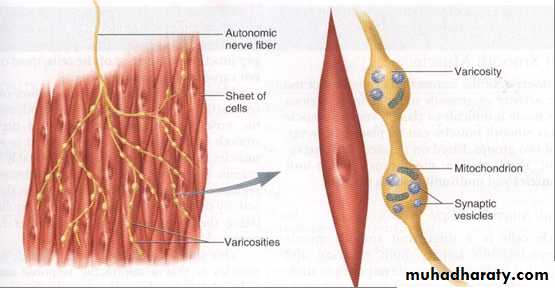
I-Neuromuscular junctions of the highly structured type found on skeletal muscle fibers do not occur in smooth muscle. Instead, the autonomic nerve fibers that innervate smooth muscle branch diffusely on top of a sheet of muscle fibers, these fibers do not make direct contact with the cell membranes but instead they form diffuse junctions that secrete their transmitter substance into the matrix coating of the smooth muscle ;then the transmitter substance diffuse to the cell. (fig16)
II-The axons that innervate smooth muscle fibers divides into many branch, each branch containing series of swollen region called varicosities contain vesicles that contain neurotransmitter substance.
III-the vesicles of the autonomic nerve fiber endings contain acetylcholine in some fibers and norepinephrine in others but they are never secreted by the same nerve fibers. Acetylcholine is excitatory in some organs and inhibitory in others, the same is true for noradrenaline. this is depend on the type of receptor(excitatory or inhibitory receptors). When Ach excite muscle fiber, noradrenaline will inhibit it and vice versa.
Most blood vessels respond to norepinephrine and epinephrine (from sympathetic stimulation) by producing vasoconstriction (this response is mediated through alpha 1-adrenergic receptors). Blood vessels in skeletal muscle and cardiac muscle respond to these catecholamines producing vasodilation because the smooth muscle possess beta-adrenergic receptors
In the multi-unit type of smooth muscle, the varicosities are separated from the muscle cell membrane by as little as 20 to 30 nanometers—the same width as the synaptic cleft that occurs in the skeletal muscle junction. These are called contact junctions (fig 17)
fig 16
Fig 17
Membrane Potentials and Action Potentials in Smooth MuscleThe normal resting membrane potential is usually about -50 to -60 millivolts, which is about 30 millivolts less negative than in skeletal muscle.
The action potentials of visceral smooth muscle occur in one of two forms:
(1)Spike Potentials. rapid depolarization followed by rapid repolarization. Occurs in most types of visceral smooth muscle. The smooth muscle cell membrane has more voltage-gated calcium channels than skeletal muscle but few voltage gated sodium channels .Therefore, flow of calcium ions to the interior of the fiber is mainly responsible for the action potential.
(2)Action Potentials with Plateaus. Rapid depolarization followed by plateau then repolarization .Plateau is responsible for the prolonged contraction of smooth muscle, is due to the opening of slow calcium channels , and they remain open much longer. Occurs in the ureter, uterus, some blood vessels.
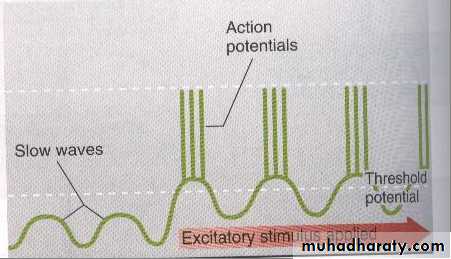
Spontaneous electrical activity and slow wave
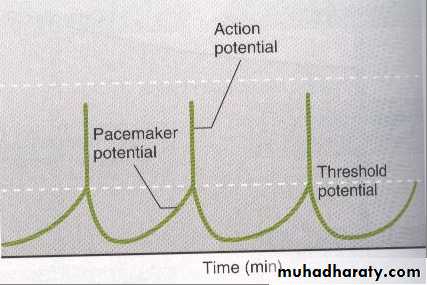
Some type of smooth muscle cell generate action potential spontaneously, plasma membrane of these cell do not maintain constant resting potential instate they gradually depolarized until they reach the threshold potential and produce A.P fallowing repolarization ,membrane begin to depolarized again lead to rhythmical state of contractile activity these cell are pace maker cellother pace maker cell have different pattern of activity, the membrane potential go up and down due to regular variation in Na ion flow across cell membrane this is called slow wave. slow wave rhythm of the membrane potential not an action potential, but when an excitatory in put (as food in intestine ) super imposed, slow wave depolarized above threshold and A.P occur lead to muscle contraction.(fig 18,19(
Fig 18
Fig 19
Excitation of smooth muscles by stretch.When visceral (unitary) smooth muscle is stretched sufficiently, spontaneous action potentials usually are generated. They result from a combination of
(1) the normal slow wave potentials
(2) stretch open mechanosensitive ion channels lead to depolarization and contraction
This response to stretch allows the gut wall, when excessively stretched, to contract automatically and rhythmically.
Smooth Muscle Contraction in Response to Local Tissue Factors.
As occurs in small vessels(arterioles, metarterioles and precapillary sphincters) which have little or no nerve supply but still can undergoes powerful vasoconstriction or vasodilation in response to local interstitial factors and this is called autoregulation of tissue blood flow
1- Lack of oxygen in the local tissues causes smooth muscle relaxation and vasodilatation.
2-Excess carbon dioxide causes vasodilatation.
3- Increased hydrogen ion concentration causes vasodilatation.
4-nitric oxide from endothelial cell cause local vasodilatation
Effects of Hormones on Smooth Muscle Contraction
A hormone will cause contraction of smooth muscle when act on excitatory receptors while cause relaxation of smooth muscle when act on inhibitory receptors. Noradrenaline, vasopressin, and angiotensin hormones are powerful vasoconstrictors lasting for hours.
Some hormone open sodium or calcium channels and cause depolarization of the membrane, other hormone closes the sodium and calcium channels or opening of potassium channels cause hyperpolarization and inhibition of the muscles .
Sympathetic stimulation(noradrenaline) decreases smooth muscle activity
Parasympathetic stimulation(acetylcholine) has opposite effects (increase force and frequancy of contraction)
Stretch and cold produce similar effects of acetylcholine on visceral smooth muscle
Cardiac Muscle
Morphology and physiological characteristics:
The heart actually two separate pumps: a right heart Receive blood from the peripheral organ and pumps blood to the lungs, and a left heart receive blood from lung and pumps blood to the peripheral organs. The heart is composed of three major types of cardiac muscle: atrial muscle, ventricular muscle, and specialized excitatory and conductive muscle fibers.
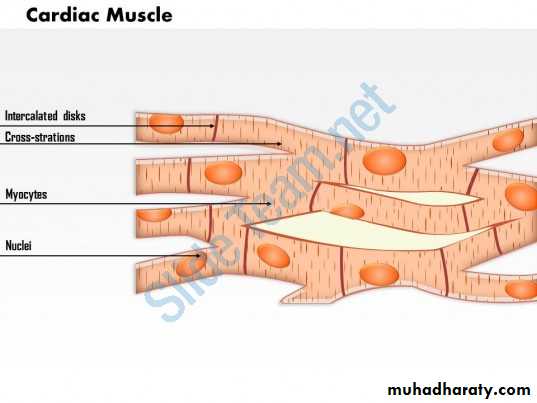
Cardiac muscle is striated, branching, involuntary have single nucleus, and have typical myofibrils that contain actin and myosin filaments (troponin and tropomyosin also present) and their organization give the striated appearance of cardiac muscle fiber ;these filaments lie side by side and slide along one another during contraction in the same manner as occurs in skeletal muscle. Cardiac muscle has a smooth sarcoplasmic reticulum(SR) but less abundant and less organized than in skeletal muscle. Cardiac muscle are connected by intercalated discs (they are actually cell membranes that separate individual cardiac muscle cells from one another). The intercalated disc contains desmosomes(provide strong mechanical union between cardiac muscle fiber) and gap junction (protein- tunnels, allow direct transmission of the depolarizing from cell to cell provide electrical union between cardiac muscle fiber); thus cardiac muscle act as a single unit(syncytium), in which the cardiac cells are so interconnected that when one of these cells becomes excited, the action potential spreads to all of them, Normally, potentials are not conducted from the atrial syncytium into the ventricular syncytium directly. Instead, they are conducted only by a specialized conductive system called the A-V bundle .Cardiac muscle fiber is myogenic (can work without nerve supply). cardiac muscle cell has rich mitochondria and blood supply, thus cardiac muscle resist fatigue. (fig 20)
fig 20
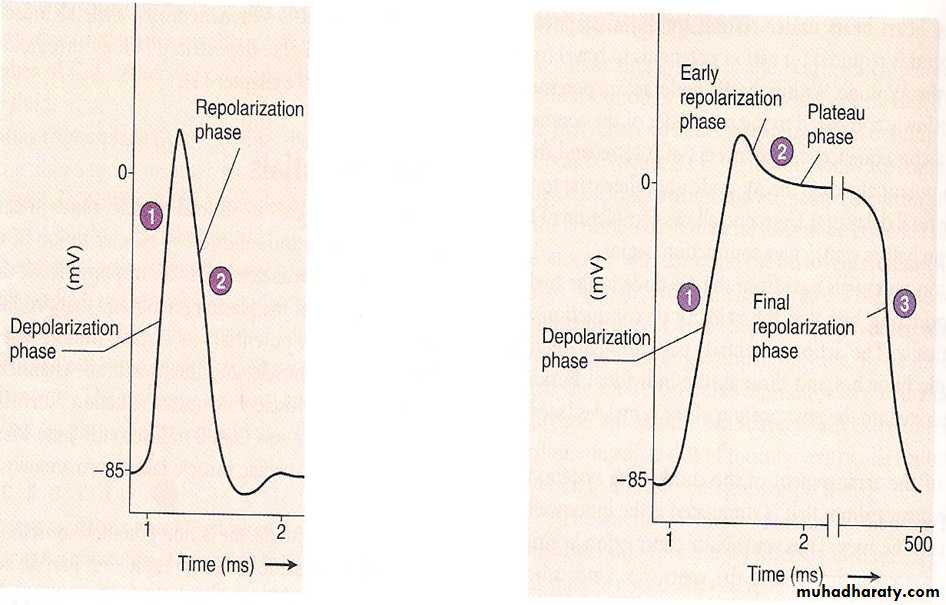
Action Potentials in Cardiac MuscleResting memberane potential in cardiac muscle is about -85 millivolts, Rises to a slightly positive value, during each beat. After the initial spike, the membrane remains depolarized for about 0.2 second ( plateau) , followed at the end of the plateau by abrupt repolarization. The presence of this plateau causes ventricular contraction to last as much as 15 times as longer than in skeletal muscle.
a. Depolarization: increased Na permeability (fast Na channels).
b. Plateau: increased Ca permeability (slow Ca channels)
c. Repolarization: increased K permeability(K efflux).(figure 21).
Skletal M
Skletal M
Cardiac M
Cardiac M
Figure(21) Comparison of action potential in skeletal and cardiac muscle
What Causes the Plateau?1-slow calcium channels, which are also called calcium-sodium channels. they are slower to open and, remain open for longer time.
2- decreases the permeability of the cardiac muscle membrane for potassium ions .
Refractory Period of Cardiac Muscle.is the interval of time, during which a normal cardiac impulse can not re-excite an already excited area of cardiac muscle. The normal refractory period of the ventricle is 0.25 to 0.30 second, which is about the duration of the prolonged plateau, therefore, cardiac muscle cannot be tetanized, a condition which is fatal.
There is an additional relative refractory period about 0.05 second during which the muscle can be excited by a very strong excitatory signal, this may develop ventricular fibrillation, a fatal condition unless immediately treated.
Excitation-Contraction Coupling
As in skeletal muscle, when an action potential passes over the cardiac muscle membrane, the action potential spreads to the interior of the cardiac muscle fiber along the membranes of the transverse tubules and cause sarcoplasmic reticulum to release calcium ions into the muscle sarcoplasm, these calcium ions diffuse into the myofibrils and catalyze the chemical reactions that promote sliding of the actin and myosin filaments along one another; this produces the muscle contraction.
In addition to the calcium ions that are released from the sarcoplasmic reticulum, a large quantity of extra calcium ions also diffuses into the sarcoplasm from the T tubules themselves Indeed, without this extra calcium from the T tubules, the strength of cardiac muscle contraction would be reduced why??
a-the sarcoplasmic reticulum is less developed than skeletal muscle
b-the T tubules of cardiac muscle have a diameter 5 times as great as that of the skeletal muscle tubules, which means a volume 25 times as greater.
Frank-Starling Law: Increase the initial length of cardiac muscle fiber, within physiological limits, will increase the force of contraction
When an extra amount of blood flows into the ventricles, the cardiac muscle itself is stretched .This in turn causes the muscle to contract with increased force because the actin and myosin filaments are brought to a optimal degree of overlap for force generation
Catecholamines (epinephrine and nor epinephrine)increases force of contraction (positive inotropic effect). This effect is mediated via beta adrenergic receptors which increase Ca influx from ECF, Ca bind to troponin-C resulting in forceful contraction.
Spontaneous rhythmicity: cutting the cardiac nerves does not stop heart beating, this is due to the presence of a specialized pace maker tissue that can initiate AP, the pace maker tissue makes up the conductive system of the heart(SA node, AV node, bundle of His, and Purkinji fibers) which normally spread impulses throughout the heart.
The pace maker tissue has unstable membrane potential which decline steadily after each AP until the firing level is reached and another AP is generated(figure22)
The unstable pacemaker potential is due to:
-Decrease K efflux (membrane potential becomes less negative).
-Na or Ca-Na in the resting condition
fig 22
parameters
Skeletal musclesSmooth muscles
Cardiac muscles
Morphology
Striated
cylindrical
Un striated
spindle
Striated
Branching
Voluntary
In voluntaryIn voluntary
Position
Skelton
Viscera
In heart
Nucleus
Multinucleated
Single nucleus
Sing nucleus
Nerve supply
Motor nerve
Autonomic
Autonomic
Autorhythmicity
Not present
Present
Present
Tetaniztion
Possible
Partially possible
Not possible
S R
Well developed
Not well define
Not well define
platue
Not present
Present in some fiber
present
Pace maker
No pace maker
In some fiber
present
Source of Ca
sarcoplasm
ECF
ECF and sarcoplasm
Neuromuscular junction
Synaptic cleft
Contact junction
Diffusion junction
rmp
-90
-50 - -60
-85