
Adrenergic Agonists
Department of Pharmacology
College of Medicine- University of
Kirkuk
2016-2017
Adrenergic Agonists
The adrenergic drugs affect receptors that are
stimulated by norepinephrine or epinephrine.
Some adrenergic drugs act directly on the
adrenergic receptor (adrenoceptor) by activating
it and are said to be sympathomimetic.
block the action of the neurotransmitters at the
receptors (sympatholytics),
THE ADRENERGIC NEURON
Adrenergic neurons release norepinephrine
as the primary neurotransmitter.
These neurons are found in the central
nervous system (CNS) and also in the
sympathetic nervous system where they
serve as links between ganglia and the
neuroeffector tissues.
The adrenergic neurons and receptors,
located either presynaptically on the neuron
or postsynaptically on the effector organ, are
the sites of action of the adrenergic drugs.
Neurotransmission at adrenergic
neurons
Neurotransmission in adrenergic neurons
closely resembles that already described for the
cholinergic neurons. except that
norepinephrine is the neurotransmitter instead of
acetylcholine.
The process involves five steps:
Synthesis
Storage
Release
Receptor binding of Norepinephrine
Removal of the neurotransmitter from the synaptic gap.
Synthesis of norepinephrine:
Tyrosine is transported by a Na+- linked carrier into
the axoplasm of the adrenergic neuron, where
it is hydroxylated to dihydroxyphenylalanine (DOPA)
by tyrosine hydroxylase
This is the rate-limiting step in the formation of
norepinephrine.
DOPA is then decarboxylated by the enzyme dopa
decarboxylase (aromatic l-amino acid decarboxylase)
to form dopamine in the cytoplasm of the presynaptic
neuron.
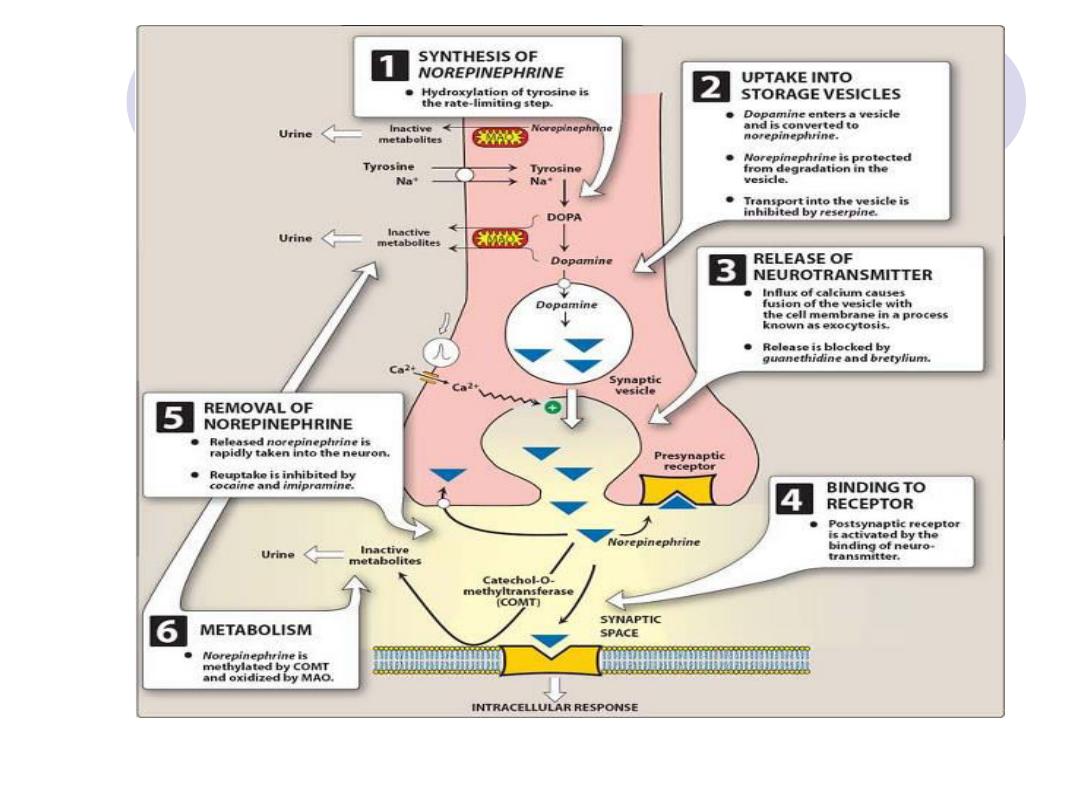
Storage of norepinephrine in vesicles:
Dopamine is then transported into synaptic vesicles
by an amine transporter system that is also involved
in the reuptake of preformed norepinephrine.
This carrier system is blocked by reserpine
Dopamine is hydroxylated to form norepinephrine by
the enzyme, dopamine
β-hydroxylase.
Synaptic
vesicles
contain
dopamine
or
norepinephrine plus adenosine triphosphate (ATP)
and b-hydroxylase as well as other co transmitters
In the adrenal medulla, norepinephrine is methylated
to yield epinephrine, which is stored in chromaffin
cells along with norepinephrine.

Release of norepinephrine
An action potential arriving at the nerve
junction triggers an influx of calcium ions from
the extracellular fluid into the cytoplasm of the
neuron.
The increase in calcium causes vesicles
inside the neuron to fuse with the cell
membrane and expel (exocytose) their
contents into the synapse
.
Drugs such as guanethidine block this
release.

Binding to receptors
Norepinephrine released from the synaptic vesicles diffuses
across the synaptic space and binds to either postsynaptic
receptors on the effector organ or to presynaptic receptors
on the nerve ending.
The recognition of norepinephrine by the membrane
receptors triggers a cascade of events within the cell,
resulting in
the formation of intracellular second messengers that act as
links (transducers) in the communication between the
neurotransmitter and the action generated within the effector
cell.
Adrenergic
receptors
use
both
(cAMP)
and
phosphatidylinositol cycle to transduce the signal into an
effect.
Norepinephrine also binds to presynaptic receptors that
modulate the release of the neurotransmitter.
Removal of norepinephrine
Norepinephrine may:
diffuse out of the synaptic space and enter the general
circulation
be metabolized to O-methylated derivatives by
postsynaptic cell membrane
–associated catechol O-
methyltransferase (COMT) in the synaptic space and
oxidized by MAO
be recaptured by an uptake system that pumps the
norepinephrine back into the neuron.
The uptake by the neuronal membrane involves a
sodium- or potassium-activated ATPase that can be
inhibited by tricyclic antidepressants, such as
imipramine, or by cocaine
Uptake of norepinephrine into the presynaptic neuron is
the primary mechanism for termination of
norepinephrine’s effects.
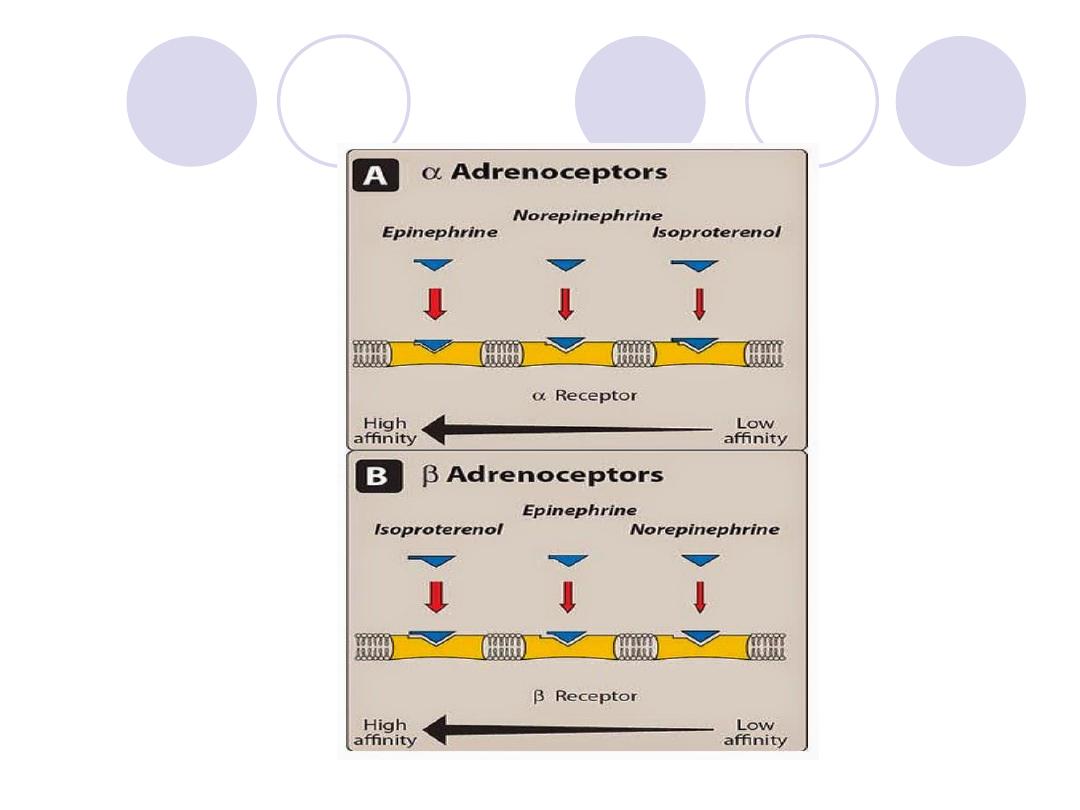
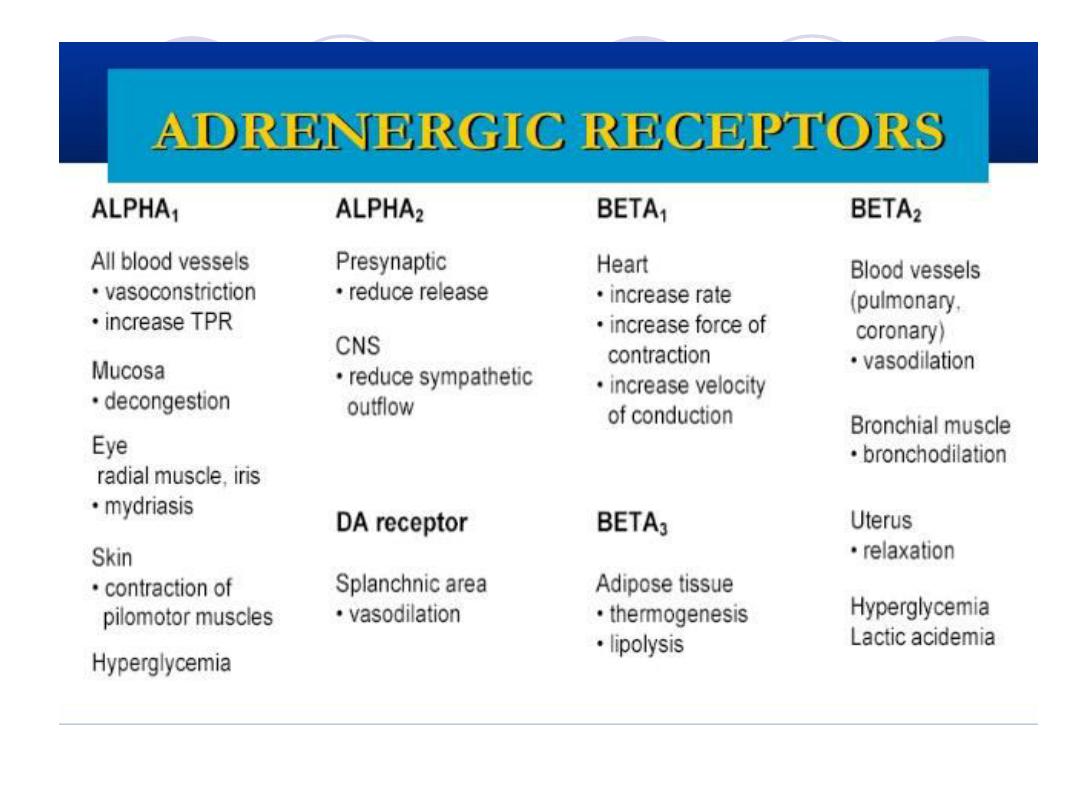
Adrenergic receptors (adrenoceptors)
several classes of adrenoceptors can be
distinguished pharmacologically.
Two families of receptors:
α and β, were initially identified on the basis of their
responses to the adrenergic agonists epinephrine,
norepinephrine, and isoproterenol.
A number of receptor subtypes
:
α1 and α2 Receptors: The α-adrenoceptors show a
weak response to the synthetic agonist isoproterenol, but
they are responsive to the naturally occurring
catecholamines epinephrine and norepinephrine

For α receptors, the rank order of potency is
epinephrine
≥ norepinephrine >>
isoproterenol.
The α-adrenoceptors are subdivided into two
subgroups, α1 and α2, based on their
affinities for α agonists and blocking drugs.
For example, the α1 receptors have a higher
affinity for phenylephrine
than do the α2
receptors.
Conversely, the drug clonidine selectively
binds to α2 receptors and has less effect on
α1 receptors.
Type of adrenergic Receptors

α1 Receptors
1-These receptors are present on the
postsynaptic membrane of the effector organs
and mediate many of the classic effects,
originally designated as α adrenergic, involving
constriction of smooth muscle.
Activation of α1 receptors initiates a series of
reactions through the G protein activation,
resulting in the generation of (IP3) &(DAG)
from phosphatidylinositol
α2 Receptors
located primarily on:
presynaptic nerve endings
on other cells, such as the b cell of the pancreas
on certain vascular smooth muscle cells
*Control adrenergic neuromediator and insulin output, respectively.
These are Further subdivided into:
Alpha 1 A, B,C, and D
Alpha 2 A, B and C
Alpha 1 Adrenoceptors:
They're present on postsynaptic membrane of effecter organ.
This extended classification is necessary for understanding the selectivity of
some drugs.
For example, tamsulosin
is a selective α1A antagonist that is used to treat
benign prostate hyperplasia.
drug is clinically useful because it targets α1A receptors found primarily in
the urinary tract and prostate gland.
Their function:
On
Vessels:
cause
smooth
muscle
contraction
so
there
will
be
Vasoconstriction of blood vessels found in
skin, splanchnic vessels and skeletal
muscles, this will cause pallor and increase
peripheral vascular resistance.
On Eyes: contraction of radial muscles of
the iris this will lead to dilation of the pupil
Mydriasis.
contraction of smooth muscles of Vas
Deferens and seminal vesicle ejaculation
Pregnant uterus contraction low
placental blood flow.
Skin: contraction of Pilo erector muscle
goose flesh skin erection of hair.
Sweat glands: are of two types:
Apocrine gland: stimulation of this gland
leads to increased secretion
Acrine gland or thermoregulatory gland has
muscarinic receptor even though
they’re
innervated by adrenergic nerves.
Metabolic functions: the effect on the liver
stimulation of lipolysis
Gluconeogenesis
Glycogenolysis
K+ release
• Heart: increase force of contraction ( not so
important).
1
Mechanism of Activation of alpha
receptors:
Stimulation of alpha 1 receptor
Activation of a G-coupling protein
Activation of phospholipase C
It acts on phosphotidyl inositol biphosphate
The release of :
*Diacylglycerol (DAG)
*Inositol triphosphate (IP3)
Major effects mediated by α1adrenoceptors
Vasoconstriction
Increased peripheral resistance
Increased blood pressure
Mydriasis
Increased closure of internal sphincter
of the bladder
Alpha 2 Adrenoceptors:
Location
1-Presynaptic receptor on adrenergic nerve
terminal (auto receptor)
Function
1-They inhibit the release of noradrenaline
2-Presynaptic receptor are present on cholinergic
nerve
terminal,
they
are
called
“Hetero
receptors
On GIT
The relaxation of GIT smooth muscles is probably
due
to
Presynaptic
inhibition
of
parasympathetic activity (because of the
presence on alpha 2 receptors on cholinergic
terminal on GIT)
3
- Postsynaptic CNS adrenoceptors are present in
the brain, e.g.: brain stem vasomotor center
Decrease sympathetic stimulation.
Some drugs used as Antihypertensive act on
these receptors for example “Clonidine”
4-On the beta cells of pancreas
Alpha 2 receptors are inhibitory, they decrease
the insulin release.
5-On platelets
They produce aggregation
6-On vascular smooth muscles
Contraction
7-On fat cells
Inhibition of lipolysis
Mechanism of Activation of alpha 2
receptors:
Alpha 2 receptors (with the help of inhibitory
regulatory G protein) inhibit adenyl cyclase
enzyme activity causing decrease in
intracellular cAMP.
In addition there are other mechanisms
include:
Activation of Potassium channels.
Closing of Calcium channel
Major effects mediated by α2
adrenoceptors
Inhibition of norepinephrine release
Inhibition of acetylcholine release
Inhibition of insulin release
β Receptors
β Receptors: exhibit a set of responses different from those of the α
receptors. These are characterized by a strong response to Isoproternol,
with less sensitivity to epinephrine and norepinephrine.
β1 receptors have approximately equal affinities for epinephrine and
norepinephrine
whereas β2 receptors have a higher affinity for epinephrine than for
norepinephrine.
Thus, tissues with a predominance of β2 receptors (such as the
vasculature of skeletal muscle) are particularly responsive to the
hormonal effects of circulating epinephrine released by the adrenal
medulla
Binding of a neurotransmitter at any of the three β receptors results in
activation of adenylyl cyclase and, therefore, increased concentrations of
cAMP within the cell.
For β receptors, the rank order of potency is isoproterenol > epinephrine
> norepinephrine.
Major effects mediated by β1
adrenoceptors.
Tachycardia
Increased lipolysis
Increased myocardial contractility
Increased release of renin
receptors:
1
Beta
Location
Heart
: increased Automaticity of SA node with
increased heart rate (i.e. positive chronotropic
effect).
Increased conductivity (velocity) in conducting
tissues including AV node (i.e. positive
dromotropic effect).
Increased excitability of AV node and muscles.
predisposing to arythmias.
and increased Oxygen consumption.
Decreased Refractory Period.

Kidney:Stimulation of Beta1 receptors on
juxtaglomerular cells will increase Renin
release (Renin converts Angiotensinogen
into Angiotensin I )
Nerves: Presynaptic adrenergic and
cholinergic terminals.
Receptors:
2
Beta
Distribution of receptors: Adrenergically
innervated organs and tissues tend to have a
predominance of one type of receptor. For
example, tissues such as the vasculature to
skeletal muscle have both α1 and β2
receptors, but the β2 receptors predominate.
Other tissues may have one type of receptor
exclusively, with practically no significant
numbers of other types of adrenergic
receptors. For example, the heart contains
predominantly β1 receptors.
Major effects mediated by β2
adrenoceptors
Vasodilatation
Decreased peripheral resistance
Bronchodilation
Increased muscle and liver
Glycogenolysis
Relaxed uterine smooth muscle
Increased release of glucagons
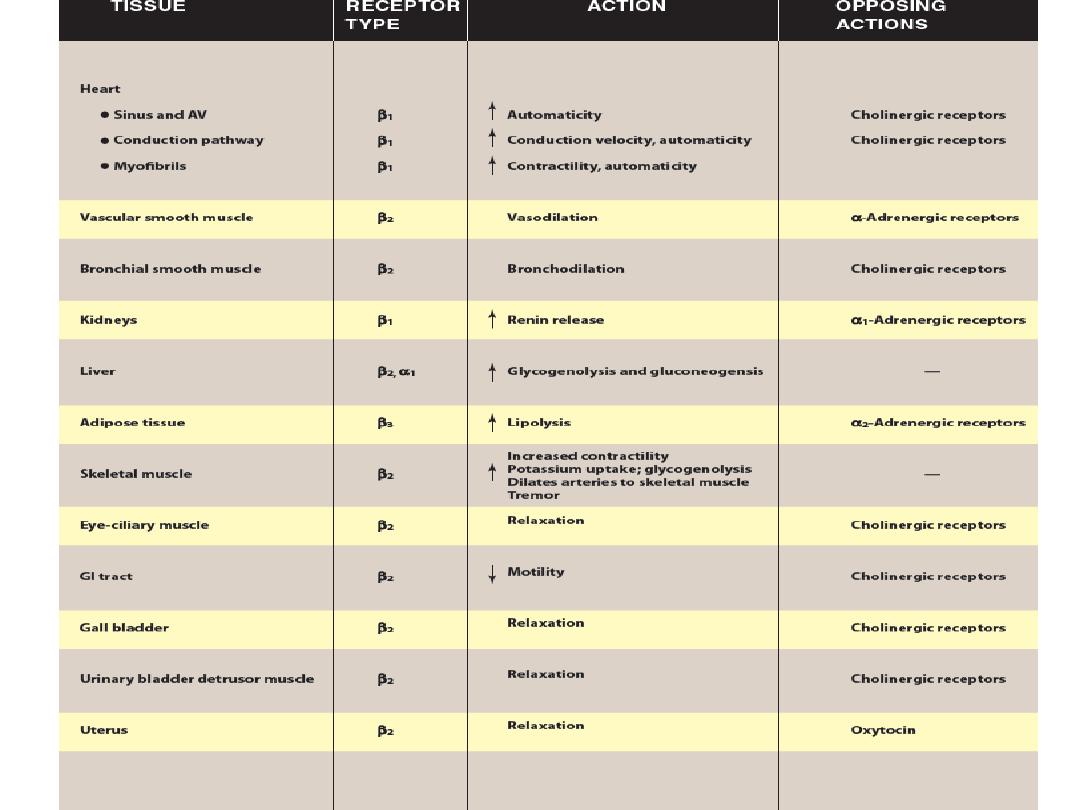
Location&Action
Blood Vessels
: Vasodilation of skeletal muscles, renal
and visceral vessels. Decreased total peripheral
resistance (TPR).
Lung:Bronchodilation
GIT: Smooth muscles in the intestinal wall are relaxed
Genitourinary system: Relaxation of Bladder wall.
Pregnant uterus relaxation delay of premature labour
Skeletal muscles:Activation of Beta2 receptors
Tremor and increased K+ by skeletal muscles
Hypokalemia
Mast Cells: Decreased Histamine release.
Liver: Increased Gluconeogenesis and
GlycogenolysisThis will lead to Hyperglycemia.
Pancreas: Increase release of Glucagon lead to
Hyperglycemia
Heart: has beta2 but much lesser than other organs.
Mechanism of Activation of Beta
Receptors:
Activation of all subtypes of Beta receptors activation of
adenyl cyclase increased conversion of ATP to cAMP,
both are mediated by protein Gs (stimulatory).
cAMP is the major 2nd messenger of beta receptor activation
In the heart, the activation of beta receptors increased influx of
calcium across cell membrane and its sequestration from
sarcoplasmic reticulum inside the cell.
Relaxation of smooth muscle may involve the Phosphorylation
(inactivation) of myosin light chain kinase.
Beta activation increase cAMP Phosphorylation of myosin
light chain kinase inactive form vasodilation and relaxation
Nitrate increase cGMP dephosphorylation of myosin light
chain kinase inactive form relaxation.

Dopamine Receptors:
They're of 5 subtypes arranged in two
families:
Family (1) :D1 and D5
Family (2) :D2, D3 and D4
•
Stimulation of D1 family stimulation of adenyl
cyclase smooth muscle relaxation renal
vessels dilation
•
Stimulation of D2 family inhibit adenylyl
cyclaes and open potassium channels
modulate transmitter release
Desensitization of receptors:
rolonged exposure to the catecholamines
reduces the responsiveness of these receptors,
a phenomenon known as desensitization.
Three mechanisms have been suggested:
1-sequestration of the receptors
2-down-regulation
3-inability to couple to G protein, because the
receptor has been phosphorylated on the
cytoplasmic side by eitherof protein kinase A or
beta adrenergic receptor kinase (BARK).
Supersensitivity:occure when there is:
Depletion of Noradrenaline in synaptic cleft
by receptors
Cut off adrenergic nerve supply (de
innervation)
Up-regulation: increase the no. of receptors
to that drug then when suddenly he stops
using that drug the effect will be much greater
than before even before he began to use the
drug.
Note:To avoid such cases we're "Tapering"
the drug. I.e. gradually decrease the doses
till stopping the drug.
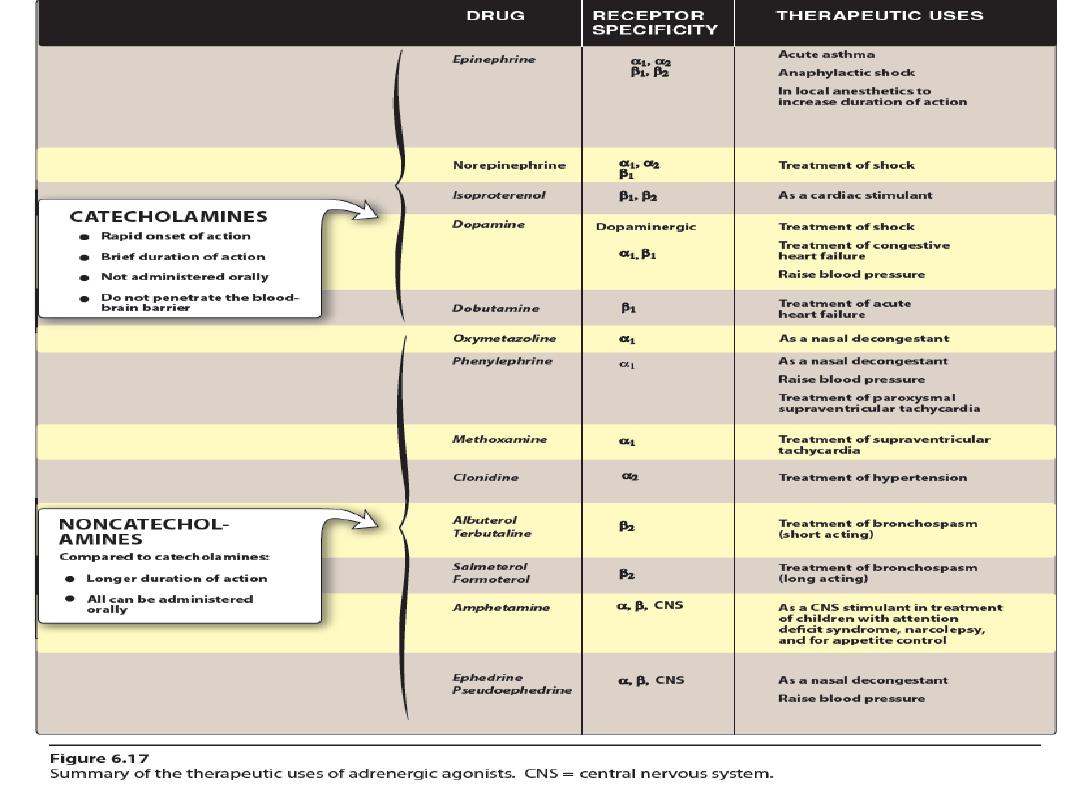
Adrenergic Agonists
Adrenergic Agonists:
According to chemical structure.
According to receptor sensitivity.
According to their mode of action.
According to chemical structure:
Catecholamine:
They're sympathomimitic amine that contains
3,4-dihydroxybenzene group like adrenaline,
Noradrenaline, dopamine, Dobutamine and
Isoprenaline.
Both Dobutamine and Isoprenaline are
synthetic
Characteristics:
*Show the highest potency
*Shortest half-life in pharmacology (2 min)
*Do not readily penetrate into CNS
*Metabolized by COMT (postsynaptically and
in the gut wall), MAO (intraneuronally and
in the mitochondria of liver cells and gut
wall cells).
They're ineffective if given orally except
Isoprenaline.
Catecholamine:
-
Non
They're phenylisopropylamines compounds lack the
catechol hydroxyl groups, They include:
phenylphrine,
ephedrine and
amphetamine group.
Characteristics:
Not metabolized by COMT and they're poor substrates for MAO
so they are given ORALLY.
Have prolonged duration of action.
Have increased lipid solubility
Have greater access to CNS due to lipid solubility and they may
act indirectly producing unwanted side effects.
According to receptor sensitivity:
Alpha-agonist
Beta-agonist
According to their mode of action:
•
1- Direct acting agonists. Ex: (catecholamine and
phenylephrine).
2- Indirectly acting agonists. Ex: (Amphetamine,
Tyramine). It interacts with MAO inhibitors causing
hypertensive crisis.
These drugs are taken up into Presynaptic neurons and
cause the release of NA
3-Mixed action some agonist have both modes of action,
they can directly stimulate Adrenoceptors and release NA
from adrenergic neurons (indirect action). Ex: Ephedrine
(mainly direct) Metaraminol (mainly indirect)
Effect of Adrenergic Agonists:
depends on:
Selectivity of drug or Affinity of the
receptor
Dose of the drug.
Homeostatic reflexes: The most important
one is the baroreceptors reflex which is
mediated by the stretch receptors located
in the carotid sinus, aortic arch and atrium.
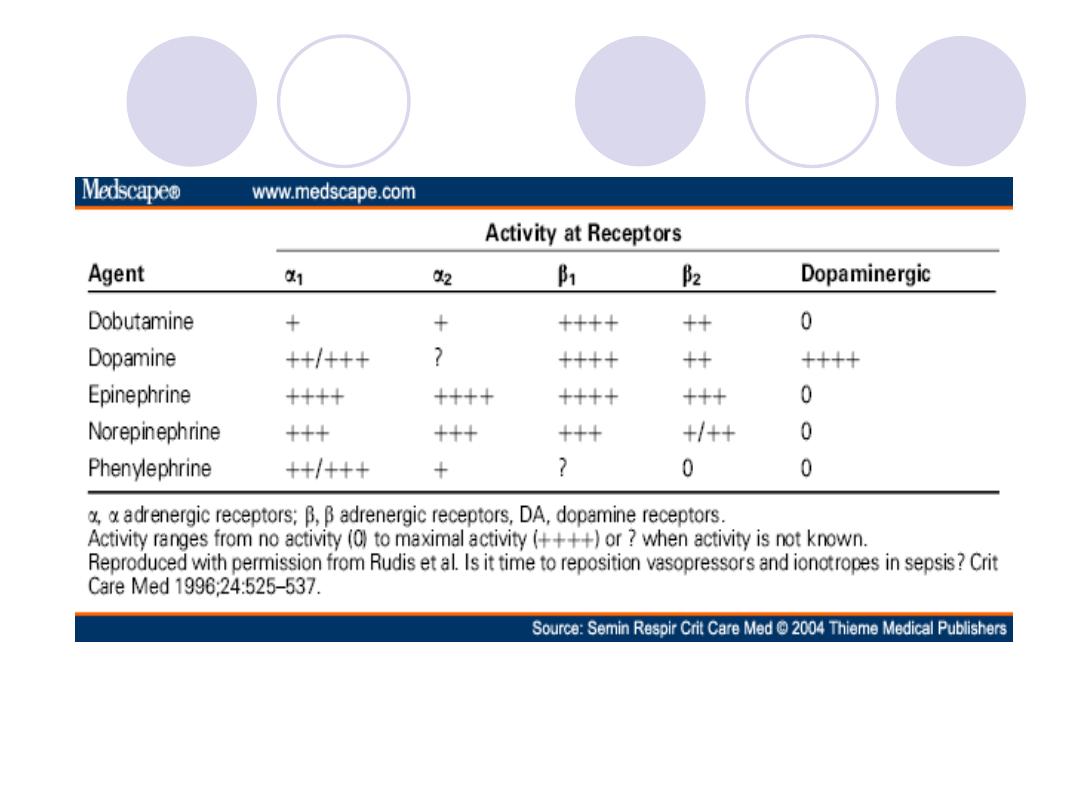
Catecholamine:
Noradrenaline:
Mainly affects alpha receptors.
Has weak effect on Beta1 receptors
Has no effect on Beta2 receptors.
So action on alpha1 = alpha2 and beta1 >> beta2
Adrenaline:Interacts with both alpha and beta
receptors
At low doses: Beta effect (vasodilation) on the vascular
system predominates.
At Higher doses:Alpha effect (vasoconstriction) is
strongest.
So action on alpha1 = alpha2 and beta1 = beta2
Isoprenaline:
Predominantly stimulated beta adrenergic receptors, it's
action on alpha receptors is insignificant.
So; beta1 = beta2 >>>>>>>> alpha
Comparison of effect of Noradrenaline, adrenaline and
Isoprenaline:
Heart rate :
*Adrenaline & Isoprenaline increase heart rate
*Noradrenaline decreases heart rate due to increased
blood pressure by stimulating the baroreceptors and
due to intense vasoconsitriction.
*If atropine is given before Noradrenaline, or the vagas is
cut ,or the patient is in shock then there will be
tachycardia.
Note: the Baroreceptors reflex predominates over
noradrenaline effects.
Force of contraction:
( contractility
S↑ )
Noradrenaline, Adrenaline and Isoprenaline
increase contractility and stroke volume.
The reflex compensation doesn't affect the
positive entropic effect of Noradrenaline
Cardiac output :
Adrenaline and Isoprenaline increase
cardiac output .
Noradrenaline has little or no effect on
cardiac output (due to weak beta1 effect)

Myocardial oxygen consumption :
Increase with all (least with Noradrenaline).
Conductivity :
Increased by all and may cause arrhythmias.
Blood vessels of skeletal muscles :
Noradrenaline causes constriction (i.e. increase
total peripheral resistance TPR) through αlpha
action .
Adrenaline & Isoprenaline dilate vessels going to
the skeletal muscles & liver also . the effect,
therefore, is a decreasing in total peripheral
resistance more evident with Iso. (β
action).
Skin blood vessels:
Noradrenaline & Adrenaline constrict skin and mucus
membrane arterioles (αlpha action).
Isoprenaline has no effect because ??
Renal blood vessels :The same of the skin.
Veins :
Adrenaline & Noradrenaline produce venoconstriction
which leads to increased venous return .
Isoprenaline produces dilation of veins which leads to
decreased venous return.
↑eins contain α and β
receptors (alpha are more than
beta).
Blood pressure :
Noradrenaline increases systolic and diastolic blood
pressure (alpha action).
Adrenaline increases systolic blood pressure
(Beta1) with slight decrease in diastolic blood
pressure (Beta2 vasodilation).
The mean blood pressure (MBP) =
(2 x diastolic +
systolic blood pressure ⁄3 )
may be slightly
increased because the increase in systolic pressure
is much more than the decrease in diastolic
pressure. So Adrenaline increases the mean blood
pressure but the increase is less with Noradrenaline.
Isoprenaline may increase systolic pressure slightly
but it greatly reduces the diastolic pressure & the
mean arterial pressure.
Capillaries:
Adrenaline reduces capillary permeability due
to widening of the endothelial cells that
decreases the pores.
Noradrenaline and Isoprenaline have no effect.
•
Bronchiolar smooth muscle :
Adrenaline and Isoprenaline cause powerful
bronchiodilation (β
effect).
Noradrenaline has no effect, because??
Gastrointestinal Tract:
Noradrenaline (αlpha
action) , Adrenaline (alpha
and beta
action) and Isoprenaline (βeta
action)
cause relaxation .
Pregnancy uterus :
Noradrenaline (alpha action ) causes
contraction.
Adrenaline and Isoprenaline (beta
action)
causes relaxation.
Radial muscles of the iris :
Adrenaline (alpha
Ό
action) causes contraction
of radial muscles (mydriasis).
Noradrenaline has little effect because it is not
absorbed (causes severe vasoconstriction).
Isoprenaline has no effect.
Blood glucose: (increased by all)
Adrenaline has significant hyperglycemic effect
because it :
increases glycogenolysis in the liver (beta
effect)
increases the release of glucagon (beta
effect)
Decreases the insulin (alpha
effect on Beta cells of
Pancreas).
Iso. cause increase in blood sugar (β
effect).
Nor. may increase blood sugar.
Lipolysis:
Adrenaline initiates Lipolysis (through its agonist
activity on B
Ύ
receptors).
The increased Lipolysis induced by Isoprenaline is not
clinically significant.
Lipolysis is least increased by Noradrenaline.
Serum pottasium k:
Adrenaline & Isoprenaline lead to hypokalemia because
the biochemical pump that shifts k
+
into the cells is
activated by beta
agonists.
However Noradreanline may cause hyperkalemia
through alpha
Ό effect.
Release of mediators from mast cells :
The release is inhibited by Adrenaline & Isoprenaline
(beta
effect)
Noradrenaline has no effect.
Muscle tremor :
Adrenaline & Isoprenaline cause muscle tremor (beta
effect) while it less with Noradrenaline.
Note: Adrenaline constricts skin blood vessels and dilates
skeletal muscle blood vessels.
:
Therapeutic uses of Noradrenaline
To treat shocks:
To treat Hypovolemic shock because it increases
vascular resistance which leads to increased
blood pressure ,but it cause decrease blood flow
to the kidney. *dopamine is better
* Nor. is given by I.V. infusion 2- 4
mg⁄min .
As a local vasoconstrictor:
Mixed with local anesthetic to prolong its action
because it delays its absorption into the blood
stream. However Adrenaline is preferred.
•
Noradrenaline is not used as nasal decongestant
because it is not absorbed (it causes severe
vasoconstriction).
:
Therapeutic uses of Adrenaline
Anaphylactic shock :
(Type І) hypersensitivity reaction in response to
allergens that cross-link IgE fixed to mast cells and
basophiles leading to degeneration and release of
histamine and other mediators.
Adrenaline is the drug of choice in anaphylactic attacks.
500 micrograms of adrenaline (epinephrine) injection (0.5 ml of the 1 in 1000
solution) should be given i.m. to raise the blood pressure and to dilate the
bronchi (vasoconstriction renders the s.c. route less effective).
Up to 10% of patients may need a second injection 10-20 min later and
subsequent injections may be given until the patient improves
.
Adrenaline is given intramuscularly or intravenously .
It acts as physiological antagonist to histamine.
Note:Drugs of Anaphylactic Shock: (Adrenaline,
Corticosteroids and anti-histamines).
Acute asthma :
In the presence of bronchoconstriction, the
respiratory exchange is greatly improved within
few minutes after subcutaneous administration
of Adrenaline (beta
action).
Glaucoma :
Adrenaline solution may be used topically to
reduce(IOP) in open angle glaucoma.
It reduces the production of aqueous humor by
vasoconstriction of the ciliary body blood
vessels and by enhanced outflow of aqueous
humor.
In closed angle glaucoma mydriasis (including
Adrenaline)are contraindicated .

acute angle glaucoma
with Local anesthetics :
Local anesthetic solution usually contains
1:100,000 adrenaline.
The effect is to greatly increase the duration of
local anesthesia by producing vasoconstriction
at the site of injection.
Adrenaline controls bleeding during
surgery(Vasoconstriction as in dental
extraction).
Epistaxis: very weak solution of Adrenaline
can also be used topically to vasoconstrict
mucus membranes to control oozing of
capillary blood.
Cardiac arrest: Adrenaline is given by
intracardiac injection.
Therapeutic uses of Isoprenaline:
Complete heart block : (Stokes
–Adams attack)
refers to a sudden, transient episode of syncope
Beta blockers poisoning : Isoprenaline is used
as an antidote.
Acute asthma: Isoprenaline is now rarely used
as bronchodilator because it's not selective and
has side effects.
Pharmacokinetics:
Catecholamines have a t½ of 2 minutes
(very short) because they are rapidly
metabolized by MAO & COMT;
therefore, they are given in continuous
I.V. infusion.
Common adverse effects of
catecholamine :
CNS disturbances: anxiety, insomnia,
headache and tremor.
Cardiovascular disturbances: palpitation,
cardiac arrhythmias, pulmonary edema,
hypertension & sometimes cerebral
hemorrhage.
Isoprenaline causes hypotension ,
Noradrenaline may cause tissue necrosis.
Contra indication of Adrenaline and
Isoprenaline:
Angina pectoris (due to increased O2
consumption).
Cardiac arrhythmias.
Thyrotoxicosis
With halogenated general anesthetics
because they sensitize the heart to
catecholamine.
Patients taking tricyclic antidepressant
TCA.
:
Dopamine
Dopamine activates D
Ό
receptors in peripheral
mesenteric and renal vascular beds, which leads to
Vasodilation.
The activation of Presynaptic D
receptors on adrenergic
neurons , which suppresses Nor. release, contributes to
these effect (renal Vasodilation) .
A continuous I.V. infusion of dopamine 2-5
mg⁄kg⁄min
causes increased renal blood flow, by activation of
dopaminergic receptors (mainly D
Ό
).
As the dose raises 5-15
mg⁄kg⁄min, dopamine activates
beta receptors in the heart with tachycardia and
increased contractility and cardiac output. It causes
slight reduction in total peripheral resistance.
Higher doses more than 15
mg ⁄kg⁄min can cause
vasoconstriction and hypertension by activating alpha
receptors
Therapeutic uses of dopamine:
1- Shocks : dopamine is the drug of
choice for shock (hypovolemic) because:
it raises blood pressure by stimulating the heart
(beta
Ό
action).
it enhances perfusion of the kidney and Splanchnic
areas, enhances GFR and causes Na+ diuresis.
2. Congestive heart failure: is an inability
of the heart to provide sufficient pump
action to distribute blood flow to meet the
needs of the body.
Adverse effects :
tachycardia
Angina worsening
arrhythmia
Vomiting (because of the stimulation of
chemoreceptors triggers
Tissue necrosis (subcutaneous leakage)
(works on heart more
Dobutamine :
than vessels).
It's a synthetic direct acting catecholamine, that
is the beta
Ό
receptors agonist.
It's available as racemic mixture.
It stimulates the heart with few vascular effects
(beta
Ό
action).
side effect: increases cardiac output with little
tachycardia and doesn't significantly elevate O
consumption of myocardium
Therapeutic uses of Dobutamine :
Congestive heart failure.
Shock: in patient with ischemic heart
diseases ??
Ephedrine:
Non catecholamine, mixed action (mainly indirect). It is a
plant alkaloid , now it is made synthetically.
It differs from adrenaline in the following :
It is a mixed action adrenergic agent.
release stored noradrenaline from nerve endings (indirect)
stimulate alpha & beta receptors (direct).
It is about 100 times less potent than adrenaline.
Has along duration of action? (t½ = 4 hours).
Excellent absorption orally
Penetrates to CNS causing mild stimulation ( alertness
, fatigue).
Raises both systolic and diastolic blood pressure. (like Nor.)
→hile adrenaline systolic & diastolic (slightly).
Tachyphylaxis occurs.
Therapeutic uses :
As a presser agent (to raise blood pressure).
As a nasal decongestant.(while Nor. is not)
As a mydriatic agent. (alpha
Ό action)
Chronic treatment of asthma ).(it is used only in
chronic cases
due to its slow action). acute
Subcutaneous admininistration of Adrenaline.
Incontinence by alpha
Ό receptors.
Heart block thus enhances contractility. (beta action)
Myasthenia gravis : ephedrine improves motor
function??

Adverse effects :
Tachycardia
Arrhythmia
Hypertension
Worsening angina
Tremor
Hyperglycemia
Metaraminol
Mixed action (but direct is more) adrenergic
drug with action similar to noradrenaline.
This agent has been used in treatment of
shock and acute hypotension
Amphetamine
(non catecholamine, indirect action)
Action and adverse effects
1- CNS : it has a marked central stimulatory
action leads to ↑ alertness (euphoria), ↓
fatigue , depress appetite and insomnia
it may causes weakness , delirium , tremor ,
dizziness , panic states and suicidal
tendencies
In higher doses it causes convulsions .
Chronic use produces a state of psychosis
resembles an acute schizophrenic attack.
2- Sympathetic nervous system
It acts indirectly through noradrenaline
release causing:
A)
Hypertension (from α effect on
vasculature “↑PR” & β effect on heart
“↑CO” ).
B)
Cardiac arrhythmias
C)
Anginal pains
D)
Headache
E)
Excessive sweating
Therapeutic uses :
Factors that limit the therapeutic usefulness
of amphetamine include:
psychological and physical dependence
and development of tolerance to euphoric and
anorectic effects with chronic use
attention deficit syndrome
Narcolepsy
Anorexiant
Depression
Note: there are three drugs similar to
amphetamine:
Methamphetamine (very similar to Amphetamine).
Methylphenidate : (Amphetamine derivative)used
in children with attention deficit syndrome.
Hydroxyamphetamine : used to differentiate
between preganglionic and postganglionic lesions
(
Horner΄s syndrome : loss of sympathetic
stimulation due to destruction of the superior
cervical sympathetic ganglion).
Anorexigenic drugs:
Amphetamine : has temporary effect , it causes
tolerance and antagonizes antihypertensive drugs.
fenfluramine and dexfenfluramine : it causes
serotonin release and inhibited reuptake and also
stimulated (5-
HT) receptors. serotonin acts on
satiety center .
unfortunately, this drug induces pulmonary
hypertension and valvular lesion were reported.
agonist :
-
β
1.non-selective agonist: e.g.: adrenaline ,
ephedrine, Isoprenaline.
2.slective agonist:
either βΌ or β agonist.
Selective β
Ό
agonist : 2 drugs:
1.dobutamine : mentioned before.
2.xamoterol :it is a partial agonist
at βΌ Adrenoceptor.
Note: Partial agonist : means that it acts as agonist
or antagonist according to certain circumstances
particularly the level of sympathetic autonomic
activity present.
At low level of sympathetic activity, it acts as
agonist heart rate, contractility..it may
benefit:
1-mild chronic heart failure: it is likely to worsen
moderate and sever heart failure.
2- chronic orthostatic hypotension:
suddenly falls when standing up or stretching.
β
agonists
Vasodilators : they are used in peripheral vascular
diseases e.g. Isoxsuprine, nylidrine.
Uterine relaxants : they relax the pregnant uterus
and are used in premature labour to delay it e.g.
Ritodrine, terbutaline.
Bronchodilators (in bronchial asthma ): e.g.
salbutamol & terbutaline (both t½ = 3 hours),
ferometerol (t½ =12 hours) are adminstrated orally
(chronic cases) or may be inhaled (acute cases )or
IV (in status asthmaticus).
Others are albuterol, salmeterol,metaproterenol.
Side effect is minimal by inhalation route :
headache (due to vasodilation), anxiety ,
tremor, tachycardia and hypotension.
agonists :
-
α
αΌ-agonists : mainly used as vasoconstrictors. They include:
1
.phenylephrine (αΌ & slightly βΌ effect )
2
.methoxamine (only αΌ effect )
3
. metaraminol (direct αΌ & some indirect sympathomimetic effect).
Therapeutic uses :
Nasal decongestant
To raise the blood pressure
Open angle glaucoma
Mydriatic agent for ophthalmological examination of the eye.
Supraventricular tachycardia treatment
it causes marked vasoconstriction & lead to raise B.P. a reflex
vagal discharge is evoked that may convert the arrhythmia to sinus
rhythm.
Nasal decongestants :
Common cold.
Allergy
Sinusitis: enhance drainage of sinus.
Prevent otitic barotrauma to open eustachian
tube
Mode of adminstration :
Nasal drops.
Sprays
Tubes
Oral preparations ; there are different types of oral
preparation:
Short acting (2 hrs.) : phenylephrine, phenylpropanolamine.
Intermediate acting : ephedrine , pseudoephedrine.
Long acting (8-12
hrs) “imidazoline group” :
oxymetazolines , imidazolines , xylometazoline.(e.g. of
imidazoline is naphezoline )
Adverse effect :
Local ischemia :if used more than 3-hourly & for above 3
weeks the mucous membrane is likely to be damaged.
Lipoid pneumonia : oily drops or sprays , used frequently &
long term may enter the lungs.
Allergy (with prolonged use).
Interaction with antihypertensive drugs leading to failure of
therapy.
Interaction with MAO inhibitors (so it may cause
hypertension).
Hypotension with imidazolines..especially : naphezoline as
it enters the CNS & acts on α receptors suppressing the
sympathetic outflow.
It should never be used in children (this is general for
imidazolines “ especially naphezolines “ ).
Chronic orthostatic hypotension :It occurs most commonly with age ,
in primary progrssive autonomic failure & secondary to other diseases as
parkinsonism and diabetes.
Treatment :
Using elastic support stocking to reduce venous pooling.
Increasing sodium intake.
Using sodium retaining adrenocortical steroids (fludrocortisones).
βΌ - adrenocepters agonist e.g. ↓amoterol to cardiac output.
Ephedrine to Na release by nerve endings ( indirect sympathomimetic).
Intake of tyramine rich food e.g. cheese. Some of the tyramine escapes
the destruction by MAO in the intestine.
α - receptor blocker.e.g.Yohimbine.
Dopamine (D
) receptor blocker . e.g. Metoclopramide.
Caffeine
α
-agonists :
they have an important ability to decrease blood
pressure through actions in CNS e.g. Clonidine &
Methyldopa
are
useful
in
treatment
of
hypertension.
Apraclonidine: lower intraocular pressure and are
approved for use in glaucoma. Topical: 0.5, 1%
solutions
After intravenous injection, clonidine produces a
brief rise in blood pressure followed by more
prolonged
hypotension.
Clonidine
reduces
sympathetic and increases parasympathetic tone,
resulting
in
blood
pressure
lowering
and
bradycardia.
