Trichomonas vaginalis
1
1
Trichomonas vaginalis:
Trichomoniasis is the most prevalent non-viral sexually transmitted infection in
the world, affecting an estimated 3.7 million persons in USA. It is an anaerobic,
flagellated motile protozoan parasite. Alfred Francois Donné (1801-1878) was
the first to describe a procedure to diagnose trichomoniasis through "the
microscopic observation of motile protozoa in vaginal or cervical secretions in
1836.
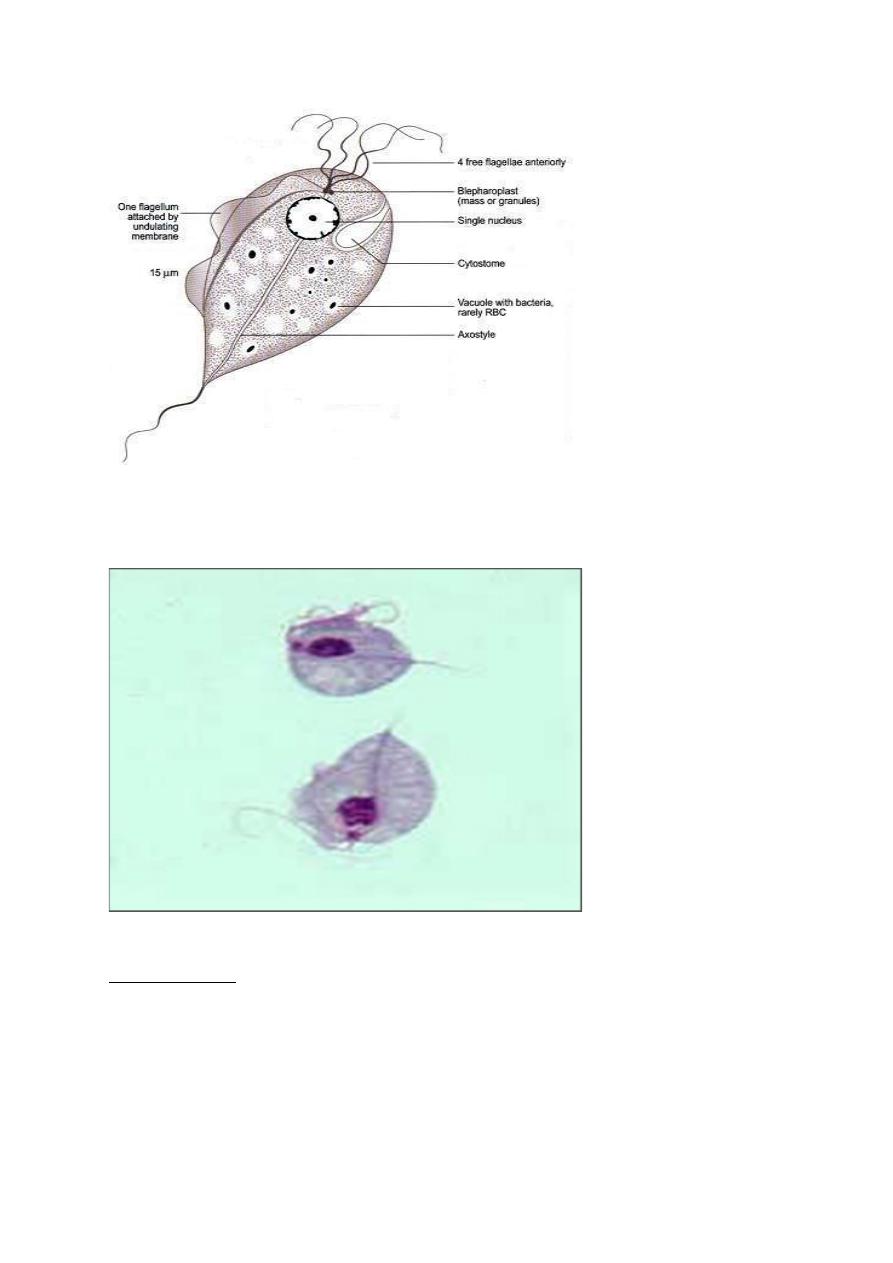
Morphology:
Trichomonas vaginalis exists in only one morphological stage, a trophozoite,
and cannot encyst. The T. vaginalis trophozoite is oval as well as flagellated, or
"pear" shaped as seen on a wet-mount. It is slightly larger than a white blood
cell, measuring 9 × 7 µm. Five flagella arise near the cytostome; four of these
immediately extend outside the cell together, while the fifth flagellum wraps
backwards along the surface of the organism. In addition, a conspicuous barb-
like axostyle projects opposite the four-flagella bundle. The axostyle may be
used for attachment to surfaces and may also cause the tissue damage seen in
trichomoniasis infections. While T. vaginalis does not have a cyst form,
organisms can survive for up to 24 hours in urine, semen, or even water
samples.
Trichomonas vaginalis
2
2
Morphology of T.vaginalis trophozoite
Trichomonas vaginalis trophozoitestain stained with Geimsa under microscope.
Transmission:
The infection is usually transmitted by Sexual intercourse (sexually transmitted
disease). The WHO has estimated that 160 million cases of infection are
acquired annually worldwide.
Trichomonas vaginalis
3
3
Virulence factors
One of the hallmark features of Trichomonas vaginalis is the adherence factor
that allows cervico vaginal epithelium colonization in women. The adherence
that this organism illustrates is specific to vaginal epithelial cells and is pH,
time and temperature dependent. A variety of virulence factors mediate this
process some of which are the microtubules, microfilaments, adhesins, and
cysteine proteinases. Cysteine proteinases also may degrade extracellular matrix
proteins like hemoglobin, fibronectin or collagen IV.
Clinical picture:
Some infected men have symptoms of urethritis, epididymitis, or prostatitis, and
some infected women have vaginal discharge that might be diffuse,
malodorous, or yellow-green with or without vulvar irritation. Only 2% of
women with the infection will have an erythematous "strawberry" cervix or
vagina on examination. This is due to capillary dilation as a result of the
inflammatory response. Untreated infections might last for months to years.
T. vaginalis infection is associated with two to threefold increased risk for HIV
transmission, preterm birth, and other adverse pregnancy outcomes among
pregnant women. Among women with HIV infection, T. vaginalis infection is
associated with increased risk for pelvic inflammatory diseases and developing
cervical cancer. Trichomonas vaginalis infection in males has been found to
cause asymptomatic urethritis and prostatitis.
Routine screening of asymptomatic women with HIV infection for T. vaginalis
is recommended because of the adverse events associated with asymptomatic
trichomoniasis and HIV infection.
Diagnosis:
Diagnostic testing for T. vaginalis should be performed in women seeking care
for vaginal discharge. Screening might be considered for persons receiving care
in high-prevalence settings (e.g., sexual transmitted disease clinics) and for

Trichomonas vaginalis
4
4
asymptomatic persons at high risk for infection (e.g., persons with multiple sex
partners, drug addicts, or a history of STD).
The use of highly sensitive and specific tests is recommended for detecting T.
vaginalis.
Tests commonly used are:
1. NAAT (nucleic acid amplification test): It is highly sensitive (96.5%) and
highly specific (97.5%), often detecting three to five times more T.
vaginalis infections than wet-mount microscopy, which has poor
sensitivity (51%–65%).
2. Microscopic wet mount examination: The most common method for T.
vaginalis diagnosis might be microscopic evaluation of wet preparations
of genital secretions because of convenience and relatively low cost.
Unfortunately, the sensitivity of wet mount is low (51%–65%) in vaginal
specimens. and lower in specimens from men (e.g., urethral specimens,
urine sediment, and semen). Clinicians using wet mounts should attempt
to evaluate slides immediately because sensitivity declines as evaluation
is delayed, decreasing by up to 20% within 1 hour after collection.
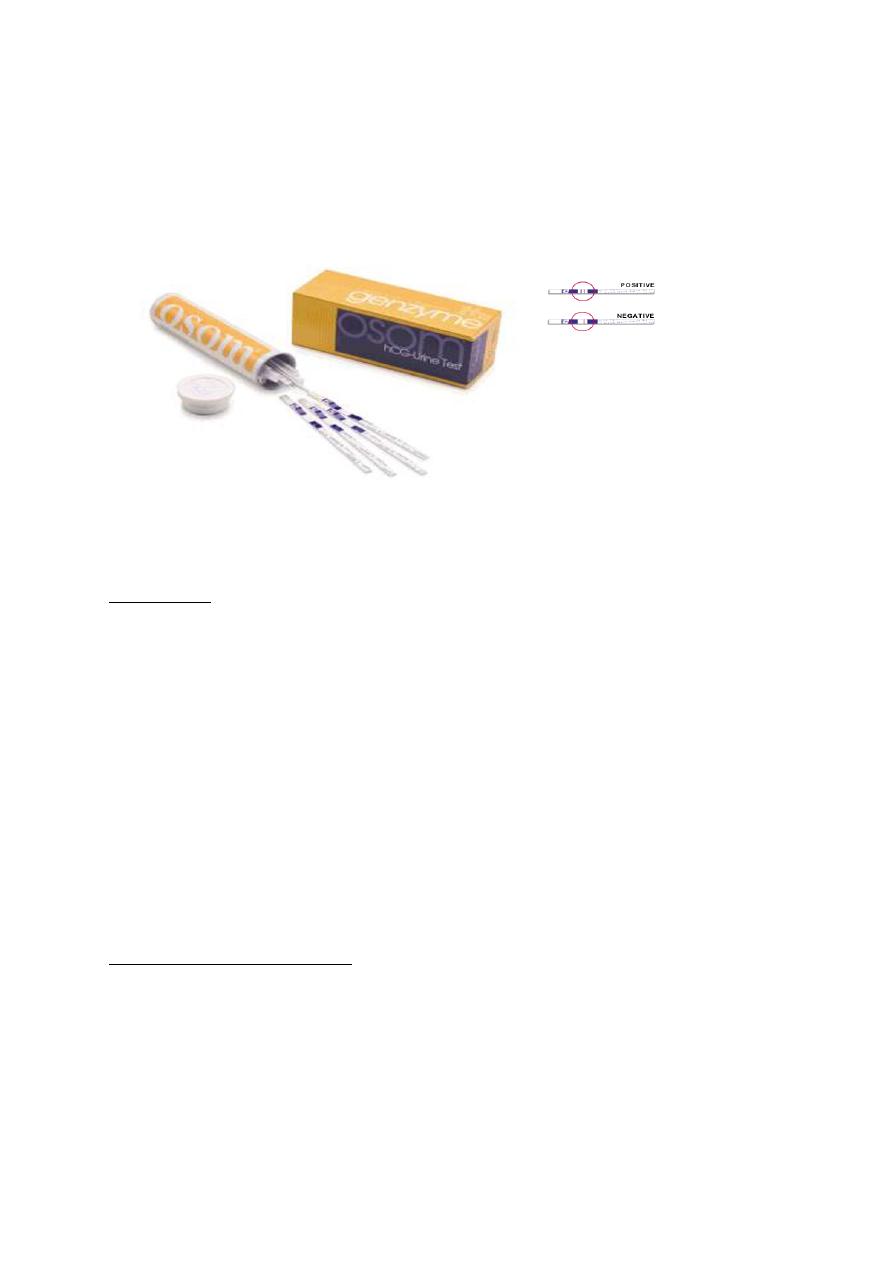
3. OSOM Trichomonas Rapid Test: It is used to detect T. vaginalis in
vaginal secretions. It is an antigen-detection test uses immune
chromatographic capillary flow dipstick technology that can be
performed at the point of care. The results of the OSOM Trichomonas
Rapid Test are available in approximately 10 minutes, with sensitivity
82%–95% and specificity 97%–100%. Self-testing might become an
option.
4. Culture was considered as the gold standard method for diagnosing T.
vaginalis infection before molecular detection methods became available.
Culture has a sensitivity of 75%–96% and a specificity of up to 100% .In
women, vaginal secretions are the preferred specimen type for culture. In
Trichomonas vaginalis
5
5
men, culture specimens require a urethral swab, urine sediment, and/or
semen. To improve yield, multiple specimens from men can be used to
inoculate a single culture.
Trichomonas vaginalis OSOM test
Treatment:
Treatment reduces symptoms and signs of T. vaginalis infection and might
reduce transmission. Likelihood of adverse outcomes in women with HIV also
is reduced with T. vaginalis therapy.
Recommended Regimen
Metronidazole 2 g orally in a single dose
OR Tinidazole 2 g orally in a single dose
Alternative Regimen
Metronidazole 500 mg orally twice a day for 7 days
Management of Sex Partners
Concurrent treatment of all sex partners is critical for symptomatic relief,
microbiologic cure, and prevention of transmission and reinfections. Partners
should be advised to avoid intercourse until they and their sex partners have
been adequately treated and any symptoms have resolved.

Trichomonas vaginalis
6
6
Prevention:
• Among persons who are sexually active, the best way to prevent
trichomoniasis is through consistent and correct use of condoms during
all sexual relation.
• Partners of men who have been circumcised might have a somewhat
reduced risk of T. vaginalis infection.
• Effective treatment of both partners
