Cystoisosporiasis
!
!
1!
1!
Cystoisosporiasis
[Cystoisospora belli (synonym: Isospora belli)]
It is intestinal coccidian parasite that infects humans. It is Worldwide, especially
in tropical and subtropical areas.
Transmission:
Humans are the only known hosts for C. belli, which has no known animal
reservoir.
The mode of transmission of isosporiasis is fecal-oral, i.e. through food or water
contaminated with human feces. Oocysts become mature and infective after
their release to the environment by 2-3 days therefore, direct person-to-person
transmission is unlikely.
Morphology:
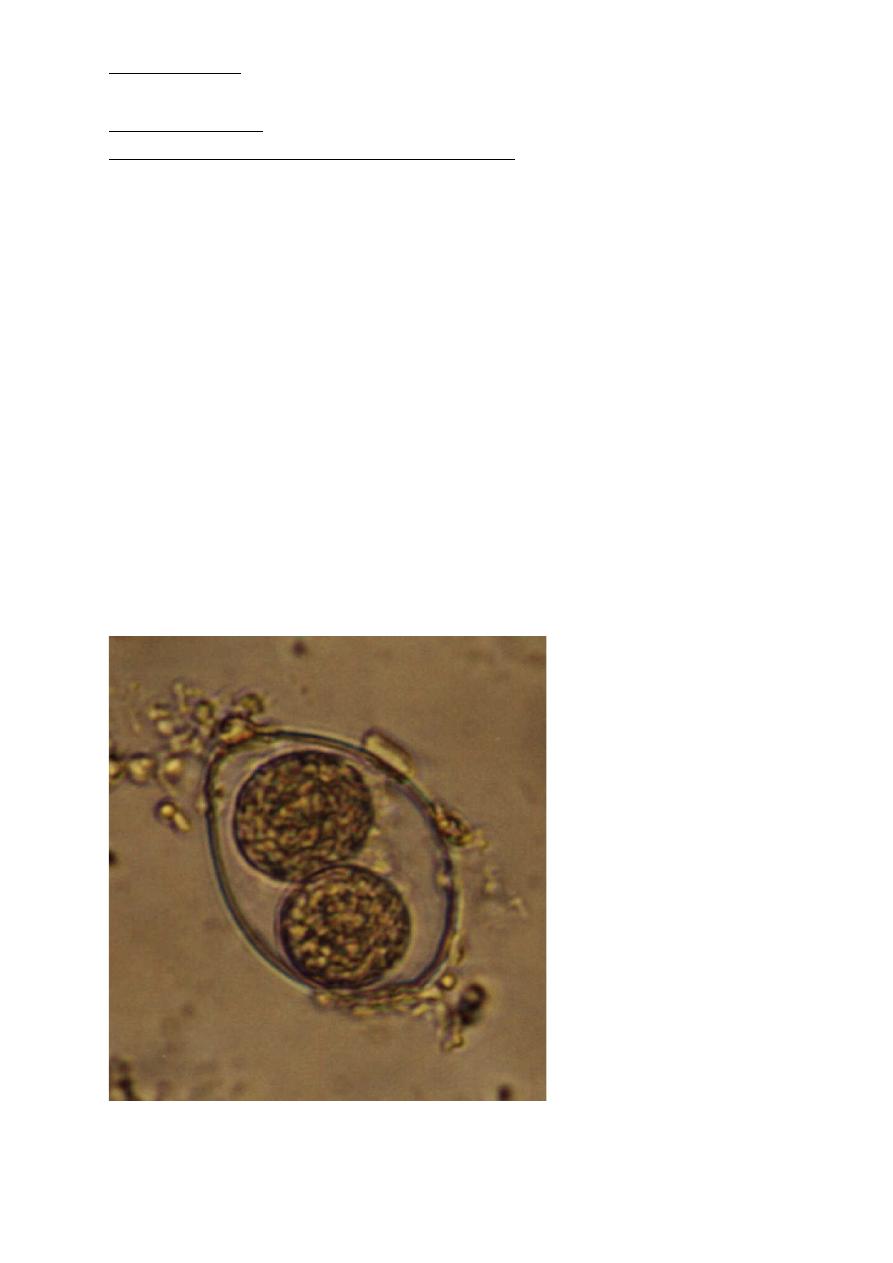
The oocysts of Cystoisospora belli are long and oval shaped. They measure
between 20 and 33 micrometers in length and between 10 and 19 micrometers
wide. A fully mature (sporulated) oocyst of Isospora genus has two sporocysts
and each sporocyst contains four sporozoites.
Oocyst of Cystoisospora belli with 2 sporocysts

!
[Cystoisosporiasis]!
!
!
2!
2!
Life cycle:
C. belli is ingested in contaminated food or water, and its life cycle requires a
stage outside the host (becomes mature oocyst out side the host). After mature
C. belli oocysts are ingested, they liberate sporozoites (possibly in response to
bile in the small intestine), which invade the enterocytes of the proximal small
intestine. Here, they become trophozoites, and asexual multiplication
(schizogony) produces merozoites that invade previously uninfected cells.
Sexual multiplication cycle (sporogony) occurs too, generating oocysts that
pass into the environment. Outside the host, oocysts become mature and
infectious after 2-3 days. The oocysts of C. belli are resistant and remain viable
in the environment for months.
Clinical picture:
C belli infection is most commonly observed in immunocompromised
individuals or in individuals who have recently traveled to tropical areas, in
people who are institutionalized, or in persons who live in poor sanitary
conditions.
The incubation period ranges from 3 to 14 days. Symptoms begin
approximately 1 week after ingestion of the oocysts and last 2-3 weeks, with
gradual improvement. Infection in people who are immunocompromised may
continue indefinitely.
Symptoms of isosporiasis suggest a toxin-mediated mechanism, but no toxin
has been identified. In humans, extraintestinal forms of cystoisosporiasis are
reported in patients with AIDS. Clinical presentation may mimic those of
inflammatory bowel disease and irritable bowel syndrome.
Symptoms and signs may include the following:
• Profuse, watery, non bloody, offensive-smelling diarrhea, which may contain
mucus
• Foul-smelling flatus
• Abdominal colic, vomiting
• Malaise, loss of appetite, weight loss
• Low-grade fever
• Steatorrhea (malabsorption and passage of fatty stool) in chronic cases
Complications:
• Severe dehydration is the most common complication and almost always
occurs in patients who are very young or immunocompromised.
Cystoisosporiasis
!
!
3!
3!
• Acalculous cholecystitis, colitis, reactive arthritis and tissue invasion and
dissemination have been reported in patients with AIDS.
Diagnosis
Microscopic demonstration of the large, typically shaped oocysts, is the basis
for diagnosis. Because the oocysts may be passed in small amounts and
intermittently, repeated stool examinations and concentration procedures are
recommended as Zinc sulfate or sugar flotation which is the most sensitive stool
concentration technique.
Fluorescent stains, modified acid-fast, hematoxylin/eosin, and Giemsa staining
are helpful in identifying the translucent oocysts. Duodenal specimens biopsy
may be needed if stool examinations are negative.
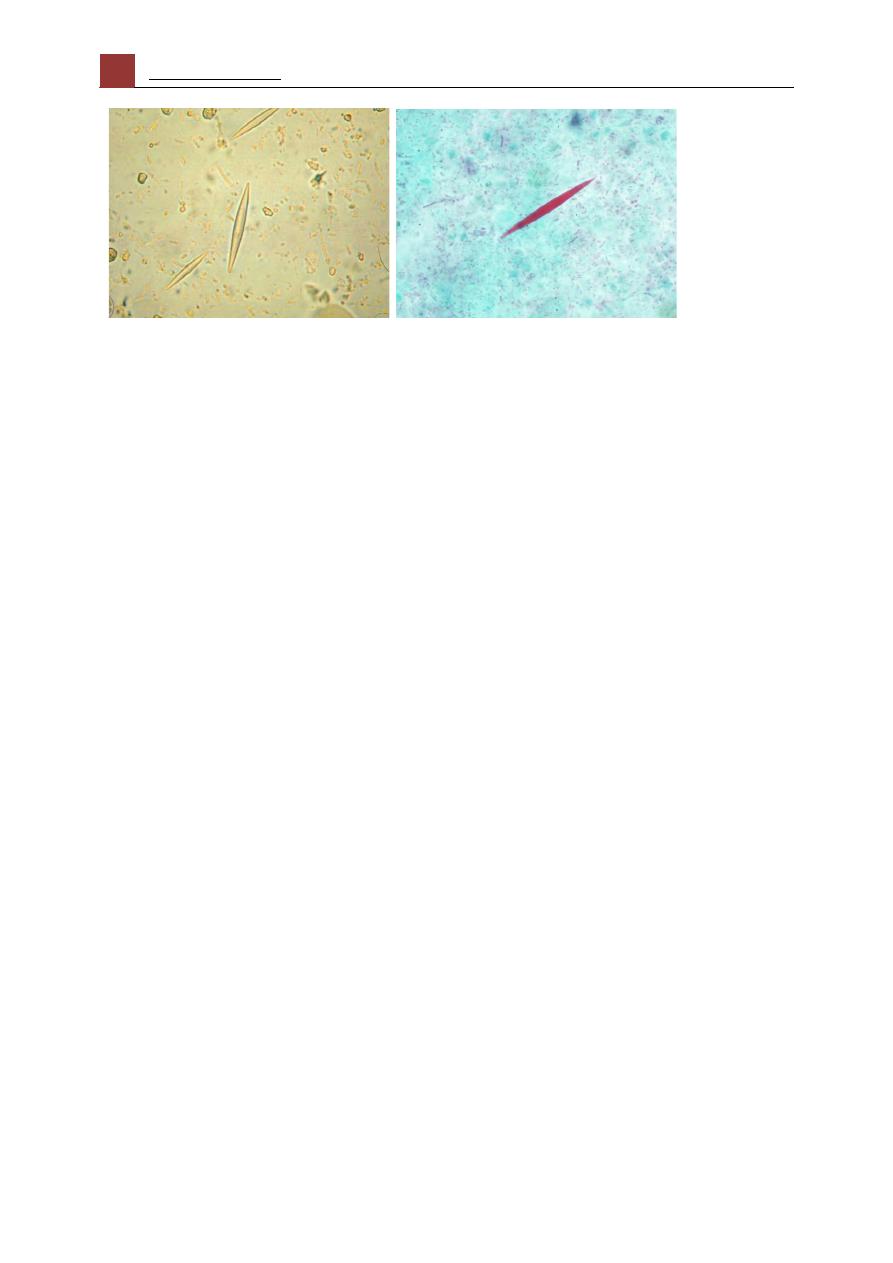
In the stool examination we can find microscopic crystals called charcot-
Leyden crystals. It is found in people who have allergic diseases such as asthma
or parasitic infections such as parasitic pneumonia or ascariasis. These crystals
are formed by the reaction between Charcot-Leyden crystal protein and
eosinophil lysophospholipases. They vary in size and may be as large as 50 µm
in length. Charcot–Leyden crystals are slender and pointed at both ends,
consisting of a pair of hexagonal pyramids joined at their bases. Normally
colorless, they are stained purplish-red by trichrome stain to differentiate them
from fruits and other crystals. Blood picture revealed Peripheral eosinophilia.
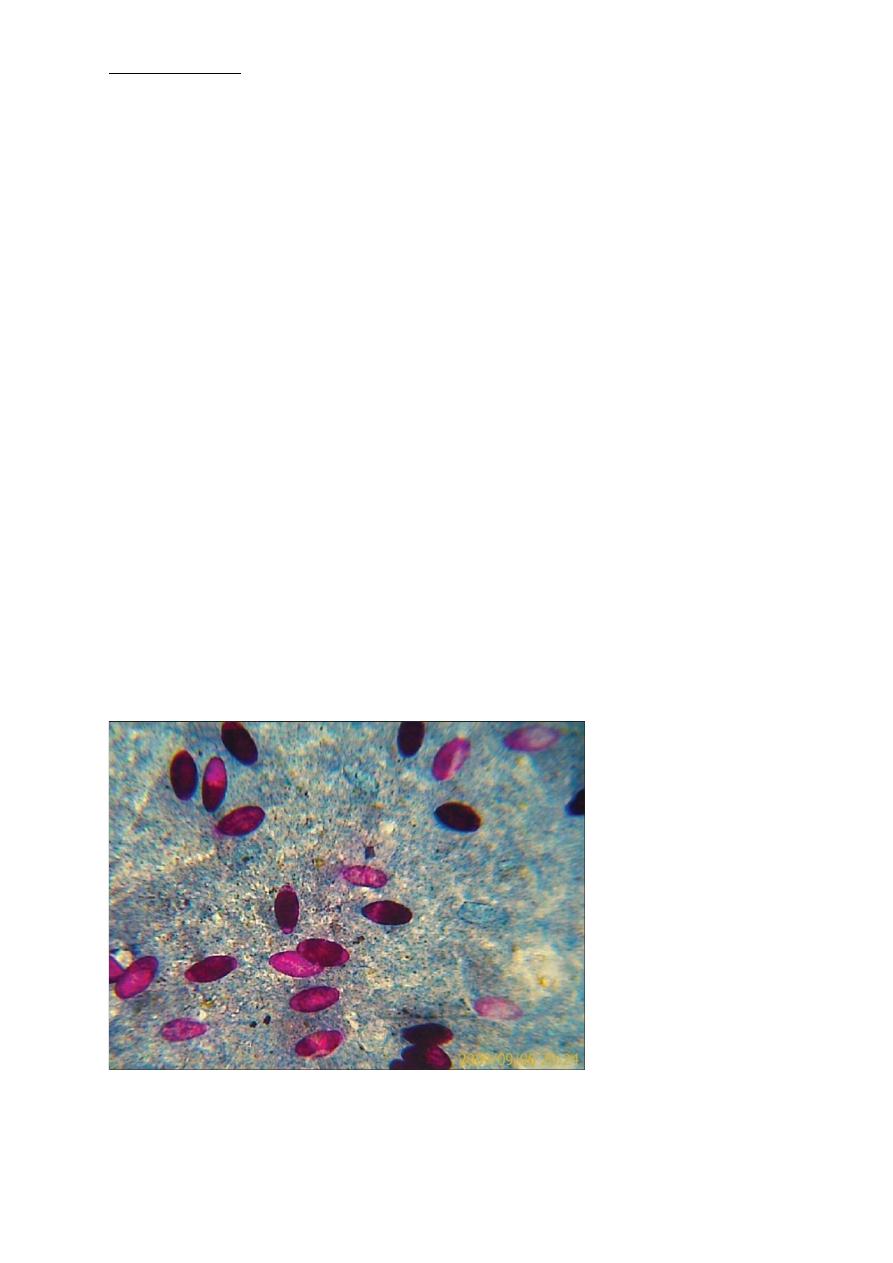
Microscopic photograph showing acid fast I. belli oocysts in stool smear
(×400). Oocysts appear pinkish red oval 20 and 33 micrometers in length and
between 10 and 19 micrometers wide
!
[Cystoisosporiasis]!
!
!
4!
4!
Charcot-Leyden Crystals in feces Charcot-Leyden crystals stained by
trichrome stain
Treatment:
Co-trimoxazole:
Trimethoprim-sulfamethoxazole
(TMP-SMX)
is
the
medication of choice for Cystoisospora infection. The typical treatment regimen
for adults is 960 mg, orally, twice a day, for 7 to 10 days.
Ciprofloxacin is a second-line alternative. It is less effective than Co-
trimoxazole but might have some activity against Cystoisospora. For adults, the
treatment regimen is 500 mg, orally, twice a day, for 7 days.
Prevention:
1. Prophylaxis with trimethoprim-sulfamethoxazole (TMP-SMX, 160 mg
and 800 mg, respectively) is effective in preventing isosporiasis in adults
with HIV infection
2. Do not drink untreated water and always wash fruits and vegetables
before eating them.
3. Take care of toilets hygiene.
4. Do not allow patients who have had C.belli to go swimming at least two
weeks after being free from diarrhoea.
