Toxoplasmosis
1
1
Toxoplasma gondii:
Toxoplasma gondii (T.gondii) is an obligate intracellular parasite found in
many species throughout the world causing a variety of clinical syndromes
in human and animals.
T.gondii was discovered in 1908 in a desert rodent called Ctenodactylus
gondii.
The discovery of the life cycle of the parasite has been completed only in
1970 when domestic cats were recognized as the definitive hosts. In 1980s
T.gondii was regarded as important opportunistic infection in immune
compromised subjects.
Stages of the parasite:
The organism exists in three life forms:
Oocysts
• It is resistant form.
• Formed as a result of gametogony (sexual cycle) in the cats’ intestine
(feline intestine).
• Released with the cat feces for periods of 1-3 weeks after cat
infection.
• Remains for 1 year in warm moist soil
• Sporulation occurs outside the cat within 1 to 5 days of excretion
depending upon oxygenation and temperature. They do not sporulate
below 4C° or over 37C°.
Morphology:
Unsporulated oocysts are subspherical to spherical and are 10 by 12 µm in
diameter.
Under light microscopy the non sporulated oocyst wall consists of two
colorless layers.
Sporulated oocysts are subspherical to ellipsoidal and are 11 by 13 µm in
diameter. Each sporulated oocyst contains two ellipsoidal sporocysts .
Sporocysts measure 6 by 8 µm; each sporocyst contains four sporozoites

Toxoplasmosis
2
2
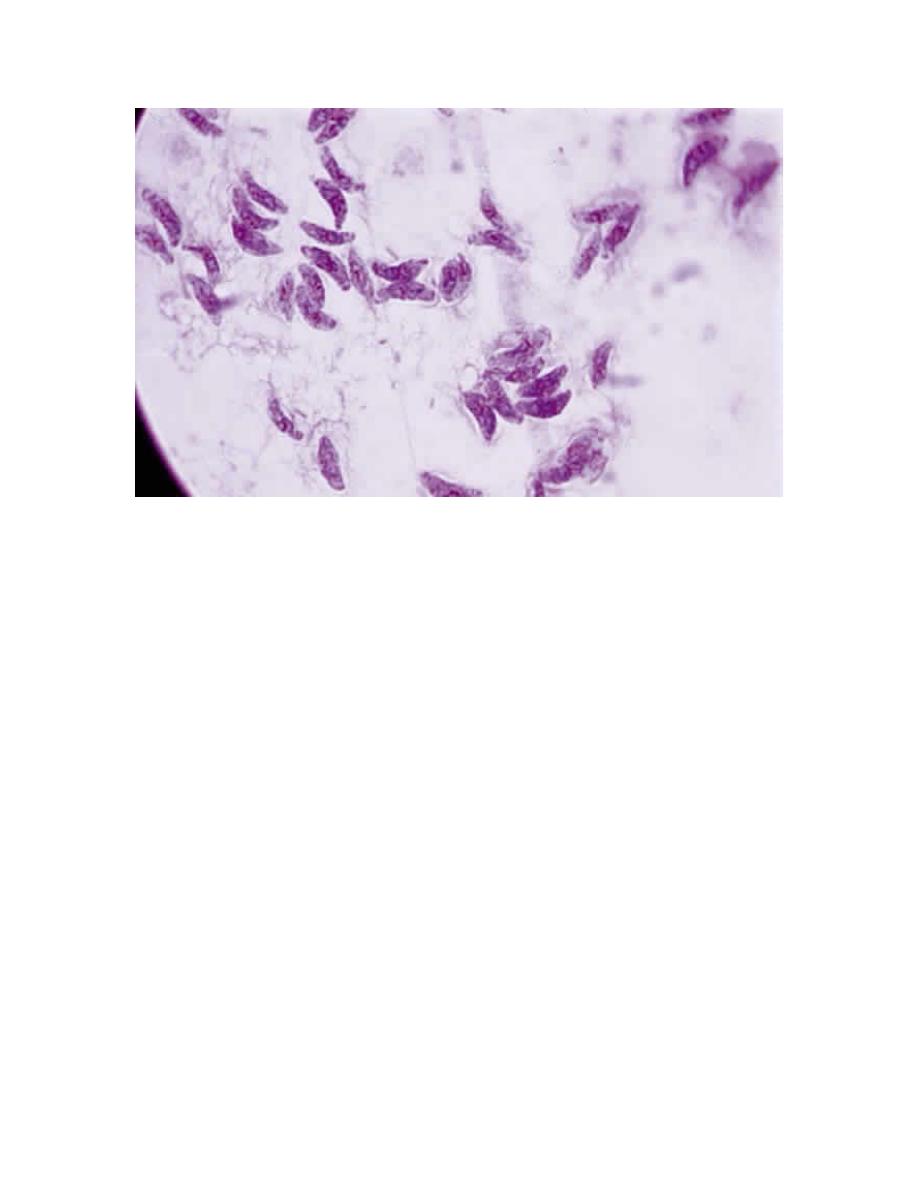
Tachyzoites:
• Intracellular microorganisms
• Presents in both cats (definitive host) and in human, mammals and
birds (Intermediate hosts).
• They are rapidly dividing forms observed in the acute phase of the
infection and in the reactivated infection.
• Their detection is a hallmark of active disease.
Morphology:
Crescent shape
2-4µm x4-6 µm in dimensions
Oval shape nucleus located at the blunt end of the parasite
They are stained with Giemsa stain, the cytoplasm appears blue and the
nucleus red.
A-‐ Unsporulated oocyst
B-‐
sporulated
oocyct
with
2
sporocysts
,
4
sporozoites
are
clear
in
one
sporocyst
Toxoplasmosis
3
3
Toxoplasma gondii. Tachyzoites from the peritoneal exudates of infected
mice stained with Giemsa (× 100).
Bradyzoites:
• Similar to tachyzoites in morphology
• But slower multiplication
• Found in tissue cysts
• Usually localized in muscles, brain and eyes
• They can live in the tissues of the host for long time and when
ingested in the undercookedor raw meat can transmit the infection.
• Tissue cysts are round, oval, 100-200 µm in diameter containing 100s
of bradyzoites.

Toxoplasmosis
4
4
Life cycle:
The only known definitive hosts for Toxoplasma gondii are members of
family Felidae (domestic cats and their relatives). Unsporulated oocysts are
shed in the cat’s feces. Although oocysts are usually only shed for 1-3
weeks, large numbers may be shed. Oocysts take 1-5 days to sporulate in the
environment and become infective. Intermediate hosts in nature (including
birds and rodents) become infected after ingesting soil, water or plant
material contaminated with oocysts. Oocysts transform into tachyzoites
shortly after ingestion by mammals (intermediate host). These tachyzoites
localize in tissues and develop into tissue cyst bradyzoites.
Cats become infected after consuming intermediate hosts harboring tissue
cysts containing bradyzoites. Cats may also become infected directly by
ingestion of sporulated oocysts.
Toxoplasmosis
5
5
Summary of modes of Toxoplasma transmission to humans:
Ingestion of undercooked infected meat (chicken, mutton, beef)
containing Toxoplasma cysts
Ingestion of the oocyst from contaminated hands or food
(vegetables)
Accidental skin penetration and inoculation of tachyzoites
Allograft organ transplantation: heart, kidney, liver, or bone
marrow (cyst or tachyzoite)
Congenital transplacental transmission (tachyzoite)
Consumption of raw milk (oocyst)
Inhalation of oocysts
Transcojunctival transmission( tachyzoite)
Water supply contamination (oocyst)
The tachyzoite occasionally may penetrate mucosal surfaces such
as the conjunctiva.
Geographic Distribution:
Serologic prevalence data indicates that toxoplasmosis is one of the most
common human infections throughout the world.
A high prevalence of infection in France has been related to a preference for
eating raw or undercooked meat, while a high prevalence in Central America
has been related to the frequency of stray cats in a climate favoring survival
of oocysts and soil exposure.
Studies showed that prevalence of Toxoplasma gondii infection among
young women in Mosul was around 49.85% while prevalence of infection
among pregnant ladies with history of abortion or dead fetus in Duhok was
59%.
Pathogenesis:
T.gondii is an intracellular coccidian parasite that disseminates via
blood and lymph to reach the different organs and tissues.
The rate of the organ or tissue to get parasite infection depends on the
vascular supply, immunity (local and general) and the regenerative
ability of the host cells.

Toxoplasmosis
6
6
The acute phase infection is characterized by wide spread of
tachyzoites that invade all nucleated cells, and after 5-6 parasitic
division the host cells will be lysed releasing the tachyzoites that
infect the surrounding cells and tissues leading to cellular death, tissue
necrosis and intense mononuclear inflammatory response in the
infected tissues.
After that, the infection goes into chronic dormant stage in which the
parasitic stage is bradyzoites enclosed in cysts that formed after 8
days from infection, located in body tissues as brain, skeletal muscles,
heart, eyes and other organs. Reactivation of infection occurs when
immunity declines as in AIDS patients.
Clinical presentation:
• Acquired infection with Toxoplasma in immunocompetent persons is
generally an asymptomatic infection. However, 10% to 20% of
patients with acute infection may develop cervical lymphadenopathy
and/or a flu-like illness. The clinical course is usually benign and
self-limited; symptoms usually resolve within a few days to weeks
• Immunodeficient patients often have central nervous system (CNS)
disease but may have retinochoroiditis, pneumonitis, or other systemic
disease.
• Congenital toxoplasmosis results from an acute primary infection
acquired by the mother during pregnancy. Congenital infection
develops in 30% to 50% of infants born to mothers with acquired
toxoplasmosis during pregnancy. The incidence of congenital
infection varies with the trimester during which the mother becomes
infected. The lowest incidence occurs in the first, and the highest
incidence is in the third trimester. However severe disease occurs at
early stages of the pregnancy with high rate of abortion. Many and
most of cases in late pregnancy are either mild or asymptomatic.
• Ocular toxoplasmosis: it is severe destructive intra ocular
inflammation, which is either due to rupture of cysts or due to allergic
reaction to the parasite. It may occur in the immunocompetent
Toxoplasmosis
7
7
patients, but more common in patients with HIV or other
immunocompromised individuals.
• Mental abnormalities due to T. gondii infection: About 40-70% of
asymptomatic newborns develop neurocognitive or neuro motor
abnormalities; and some of them are diagnosed as schizophrenia.
Immune response against T.gondii
T.gondii induces strong humoral and cellular immune response, which
will limit the extension of the infection saving life of the host.
Humoral immunity
• GIT mucosa releases secretory IgA Abs, which prevents parasite
adherence to the mucosal surface.
• IgG and IgM antibodies are important for effective opsonosation
and phagocytosis of tachyzoites.
• Antibodies can also inhibit cellular invasion by the tachyzoites
• Antibodies activate complement cascade, which kills the
tachyzoites.
• Humoral immunity including IgG and IgM antibodies has a
diagnostic importance
Cellular immunity
Cellular immune response is important to survive the acute phase via
the NK cells and macrophages and faces the chronic phases of the
infection and preventing the reactivation of the disease through both
CD8 and CD4 T lymphocytes immune response.
Laboratory Diagnosis
The diagnosis of toxoplasmosis may be documented by:
• Microscopic observation of parasites in patient specimens, such as
bronchoalveolar lavage material from immunocompromised patients,
or lymph node biopsy.
• Isolation of parasites from blood or other body fluids, by intraperitoneal
inoculation into mice or tissue culture. The mice should be tested for
the presence of Toxoplasma organisms in the peritoneal fluid 6 to 10
Toxoplasmosis
8
8
days post inoculation; if no organisms are found, serology can be
performed on the animals 4 to 6 weeks post inoculation.
• Detection of parasite genetic material by PCR, especially in detecting
congenital infections in utero.
•
Serologic testing is the routine method of diagnosis (antigen or
antibody detection):
!
Sabin Feldman dye test: (The gold standard test of T.gondii
diagnosis)
It is a serological method to diagnose toxoplasma gondii. This test is
rarely used these days because it is expensive and needs specialized
labs.
!
Antibody screening for diagnosis of toxoplasmosis:
The detection of Toxoplasma-specific antibodies is the primary
diagnostic method to determine infection with Toxoplasma. The
enzyme immune assay, as ELISA tests for IgG and IgM antibodies are
the tests most commonly used today.
Persons should be initially tested for the presence of Toxoplasma-
specific IgG antibodies to determine their immune status. A positive IgG
titer indicates infection with the organism at some time.
If more precise knowledge of the time of infection is necessary, then an
IgG positive person should have an IgM test performed. A negative IgM
test essentially excludes recent infection, but a positive IgM test is
difficult to interpret because Toxoplasma-specific IgM antibodies may
be detected by enzyme immune assays for as long as 18 months after
acute acquired infection.
If the patient is pregnant, and IgG/IgM positive, IgG avidity test should
be performed. Serological tests for detection of other antibodies are also
available as detection of IgE and IgA Abs.
Treatment
Medicines used for treatment of toxoplasmosis:
Pyrimethamine (Daraprim) first choice in non-pregnant patient
Spiramycin is first choice treatment during pregnancy
Toxoplasmosis
9
9
Prevention
Preventive measures to minimize human contact with the infectious form of
the parasite are important in controlling both the acquired and the congenital
form of the disease.
1. Cooking meat to temperatures in excess of 66°C destroys the tissue
cyst and prevents transmission.
2. Freezing meat to -20°C for 24 hours or more kills the cyst form of the
parasite.
3. Avoiding areas contaminated with cat feces, such as litter pans in
homes, and sandboxes and soil around houses where cats are present,
is an important preventive measure.
4. Hands should be washed with soap and water after handling raw or
undercooked meat or cats.
5. Pregnant women who are identified to be negative serologically for
toxoplasmosis should be advised not to come into contact with cats
and to get rid of cats during their pregnancy.
6. Laboratory workers should be advised to wear gloves when handling
infected needles and when working with viable Toxoplasma
organisms.
7. Blood transfusion constitutes another mode of transmission of T.
gondii. Persons who are Toxoplasma antibody-positive should be
excluded as donors of organs or blood transfusions to Toxoplasma
antibody-negative recipients.
8. Screening tests for toxoplasmosis are recommended to identify the
unimmunized woman of childbearing age and warn her against these
modes of transmission of toxoplasmosis.
