
Urinary stone disease
Dr. Ammar Fadil

Urolithiasis
– urinary stones have been noted in human
remains as old as 7000 years
o
Ten- 12% of the population affected by
urinary stone.
– 50% chance of recurrence by 5 years
2
A.F
• Urolithiasis, kidney stones,
renal stones, & renal
calculi are used
interchangeably.
• Nephrocalcinosis is a term
that refers to increased
calcium content in the
parenchyma of the kidney.
3
A.F
Causes are Multifactorial
Intrinsic factors:
– Hereditary polygenic
– Age peak incidence 20’s to 40’s
– ♂:♀ = 3:1 (equal in childhood)
Extrinsic factors
Urinary stones
o
are polycrystalline aggregates consisting of varying amounts of crystal & organic matrix components
4
A.F

Extrinsic factors
• The highest incidence occurs after peak
summertime temperatures
• because of higher urinary concentration in
the summer (increased urinary
crystallization).
• increased exposure to sunlight leads to
increased vitaminD3 and increased urinary
Ca++ excretion (hypercalciuria)
5
A.F
A.F
6
• Low daily intake of water is thought to be the
most significant cause of renal stones
– fluid intake <1200 mL/day
predisposes to stone
formation.
• High animal protein intake
increases risk of stone disease increase urinary
calcium and uric acid excretion and decrease citrate
excretion
• High salt intake causes hypercalciuria.
Increasing water hardness (high calcium content) may reduce risk of stone formation, by decreasing urinary oxalate.

A.F
7
• Increased fiber intake has been correlated with a
reduced risk of stone formation, most likely because
of increased urinary citrate
.
• Carbohydrate and fat consumption do not appear to
increase stone formation
.
• Contrary to conventional teaching, low-calcium diets
predispose to calcium stone disease, and high-calcium
intake is protective.
• Prolonged immobilization
Result in skeletal decalcification and an increase in
urinary calcium favoring stone formation

• Chemotherapeutic drugs = cell lysis and
hyperuricosuria
• Medications acetazolamide, Steroids
• Obesity is an independent risk factor for
nephrolithiasis, particularly for women
• Genetic cystine stone
• Inadequate urinary drainage and urinary
stasis. stones are liable when urine not pass
freely
Acquired: BPH, stricture (vesical stone)
Congenital: PUJO, horseshoe kidney
8
A.F

Pathophysiology
• It begins with supersaturation of the urine by
stone-forming constituents. Crystals can act
as nidi, upon which ions from the
supersaturated urine form microscopic
crystalline structures.
• Supersaturation alone is not sufficient for
crystallization to occur in urine, owing to the
presence of urinary inhibitors. (citrate …etc)
9
A.F
• Once formed, crystals
may flow out with the
urine or become
retained in the kidney at
anchoring sites that
promote growth and
aggregation, ultimately
leading to stone
formation.
10
A.F

unanswered questions
• Why did I form stone?
– Its impossible to give an exact answer, certain specific
factors are known to be associated with an increased
probability of stone formation.
• why do most stones present in a unilateral
fashion?
– If urinary constituents are similar in each kidney
• Why don’t small stones pass down the ureter early
in their development?
• Why do some people form one large stone and
others form multiple small calculi?
•
The dev
•
elopment of urinary calculi is most likely a multifactorial
11
A.F

As clinicians we are concerned
with an expedient diagnosis & efficient
treatment.
12
A.F

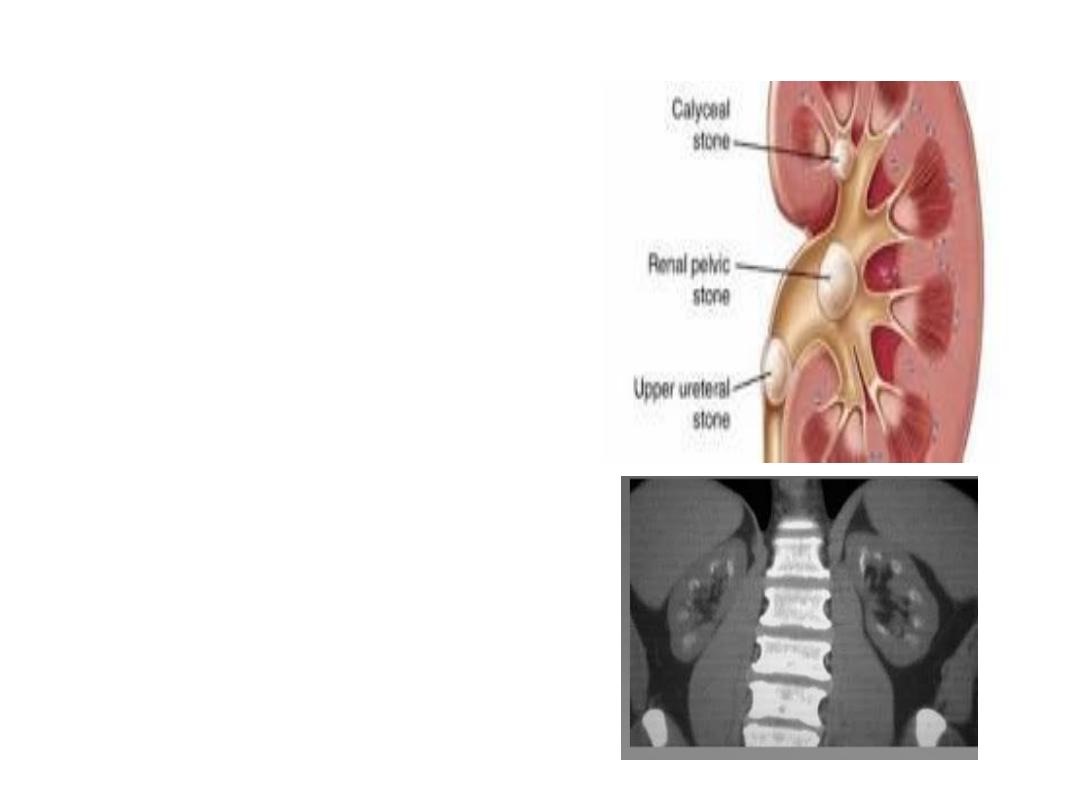
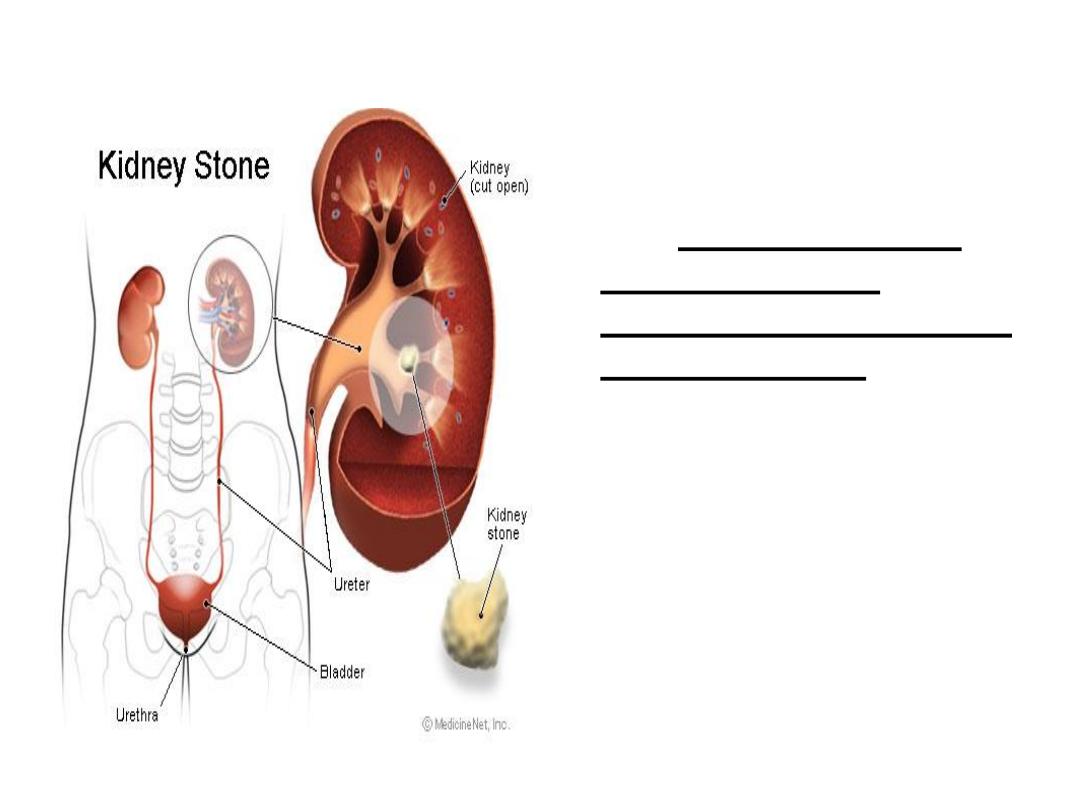
Classification
Stones may be classified according to
size,
Location,
X-ray appearance,
shape &
composition
13
A.F
• Stone size
Stone size is usually given in one
dimensions, and stratified into those
measuring up to 5, 5-10,10-20, & > 20 mm in
largest diameter.
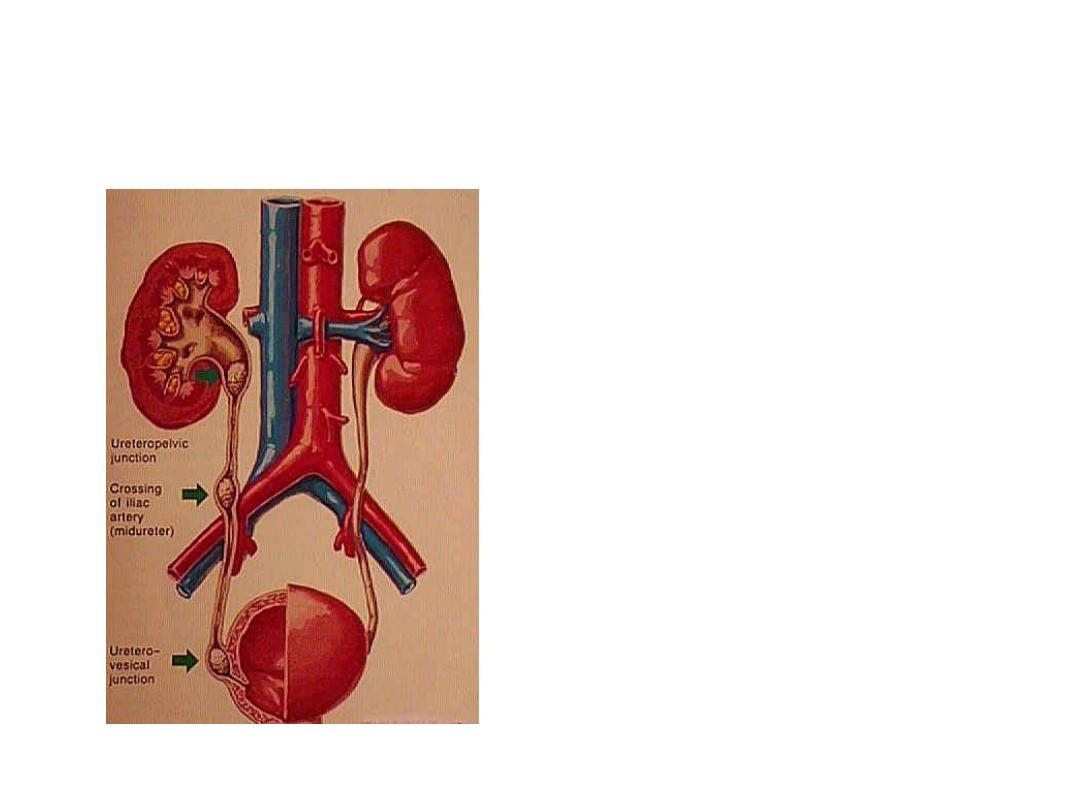
• Stone location
– Calyceal : upper, middle or lower calyx;
– renal pelvis;
– Ureter : upper, middle or distal ureter; &
– urinary bladder
.
14
A.F

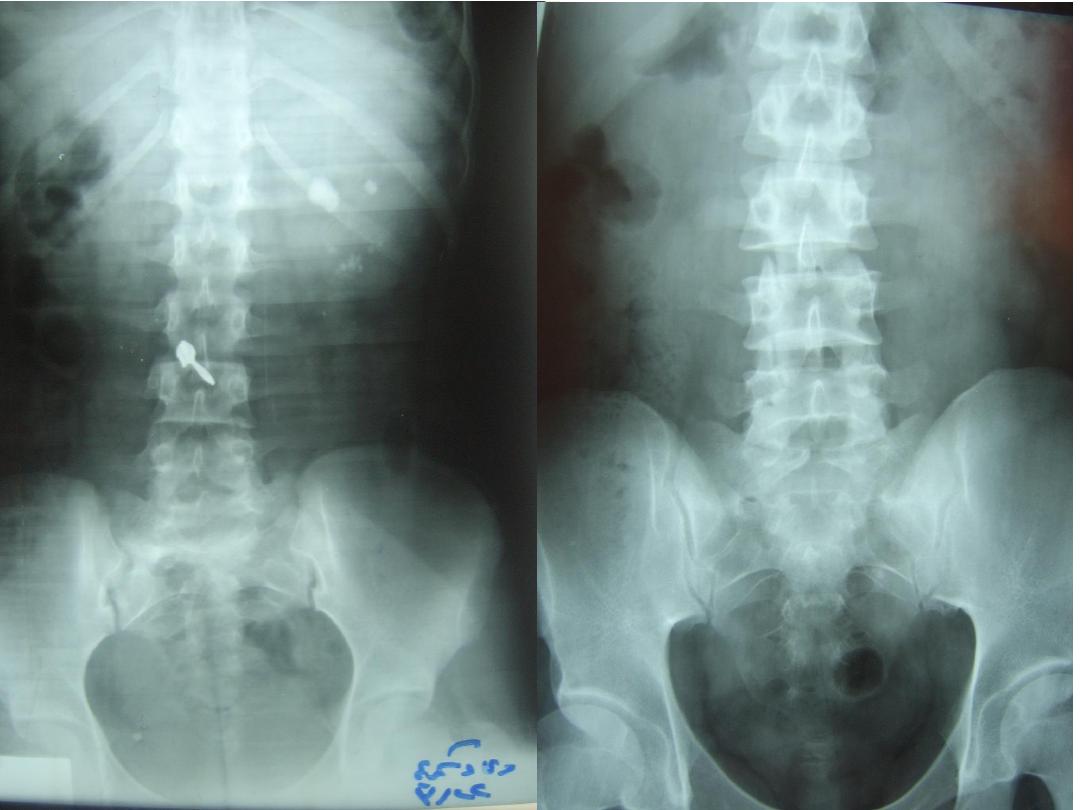
• X-ray characteristics (Appearance on X ray)
Stones can be classified according to plain X-
ray appearance [kidney-ureter-bladder (KUB)
radiography
Radio-opaque
Opacity implies presence of substantial
amounts of calcium within the stone
15
A.F
Radiopaque
Radiolucent
Calcium phosphate
Calcium oxalate
Uric acid
Magnesium ammonium
phosphate
Cystine
16
A.F
A.F
17
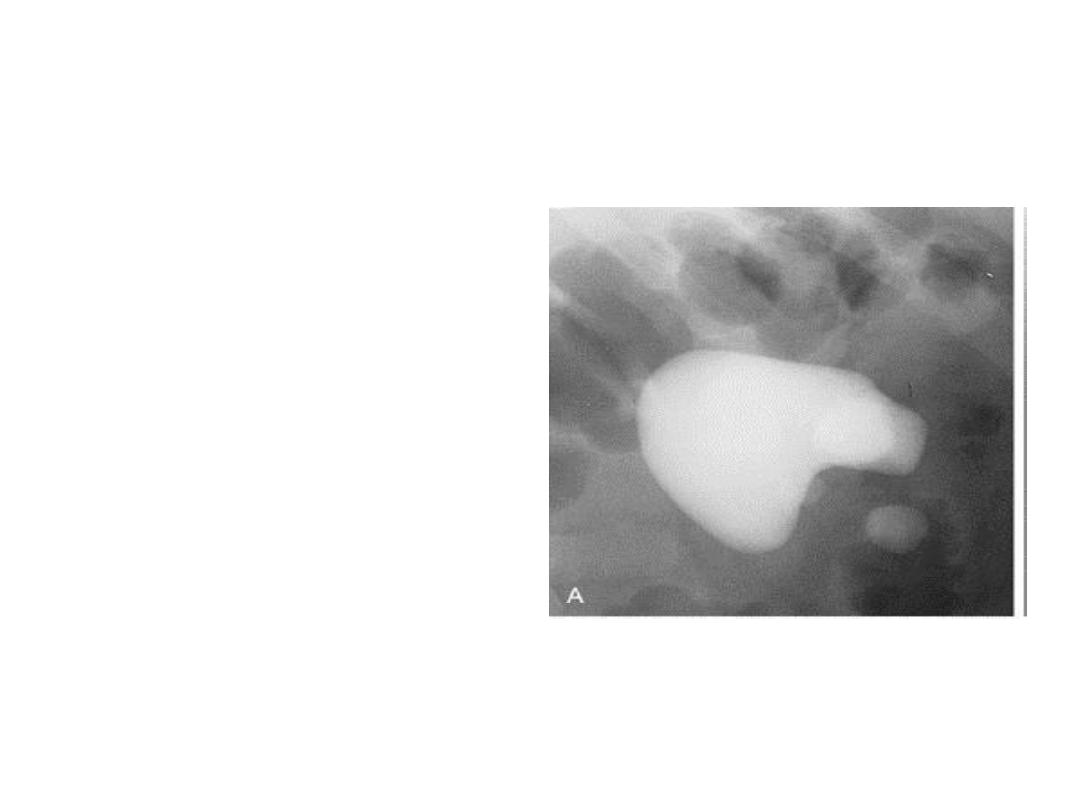
• Shape
Stones that grow to occupy the renal collecting
system (the pelvis and one or more renal calyx)
are known as
staghorn calculi
,
since they
resemble the horns of a Stag.
They are most commonly composed of
struvite
—magnesium ammonium
phosphate.
but may consist of uric acid, cystine, or calcium
oxalate
18
A.F

Stone composition % of all renal calculi*
• Calcium oxalate 85%
• MAP, Struvite (infection stones) 2–20%
• Calcium phosphate 10%
• Uric acid 5–10%
• Cystine 1%
• Mixed stones are often present
19
A.F
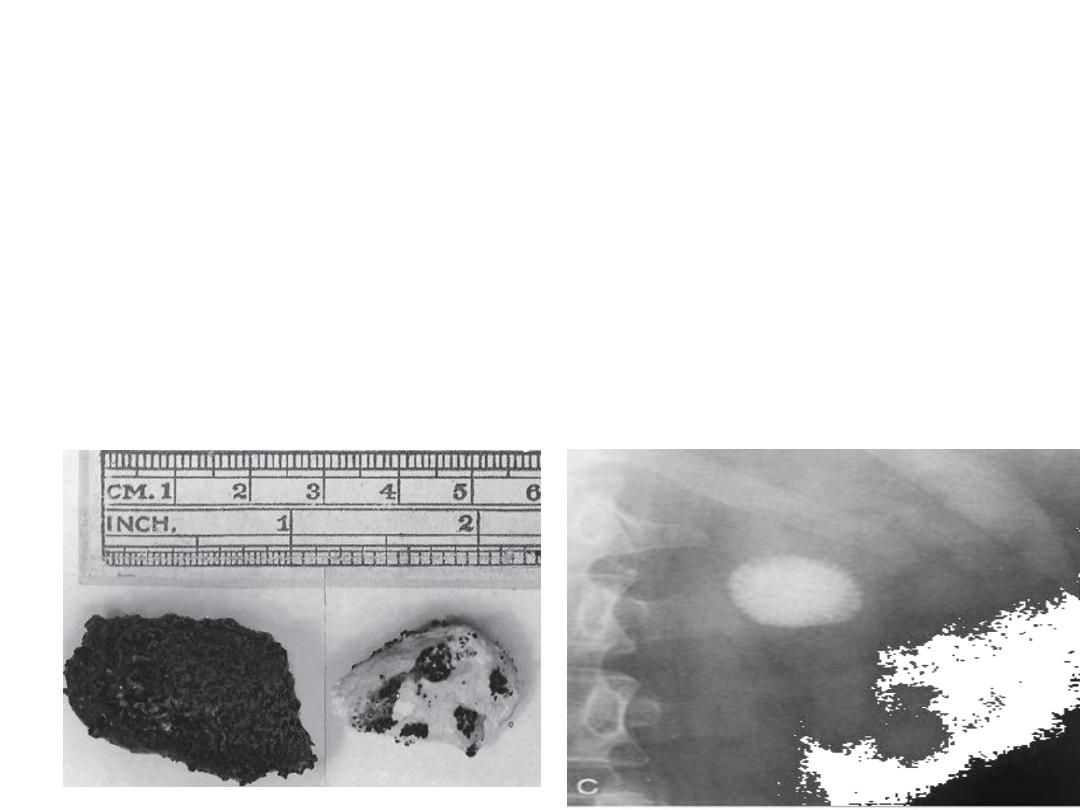
Caox
–
Hard with a sharp spiky surface, traumatizes the
urinary epithelium; the resultant bleeding usually
colors the stone a dark brown or black.
–
stippled appearance.
–
Idiopathic hypercalciuria (60-70%)
–
95% have normal serum Ca++
20
A.F
2. Calcium phosphate
• Most dense
(opaque) and
often have hard
appearance
21
A.F

3. Struvite stones
• Named after Russian geologist Von-struve
• Mixture of magnesium , ammonium & phosphate
• Infection stone
• Two conditions must coexist for crystallization
of struvite
– Urine pH >7.2
– high ammonium concentration derived from the
urea splitting organism (Proteus, Klebsiella,
pseudomonas) results in an alkaline urinary pH
22
A.F
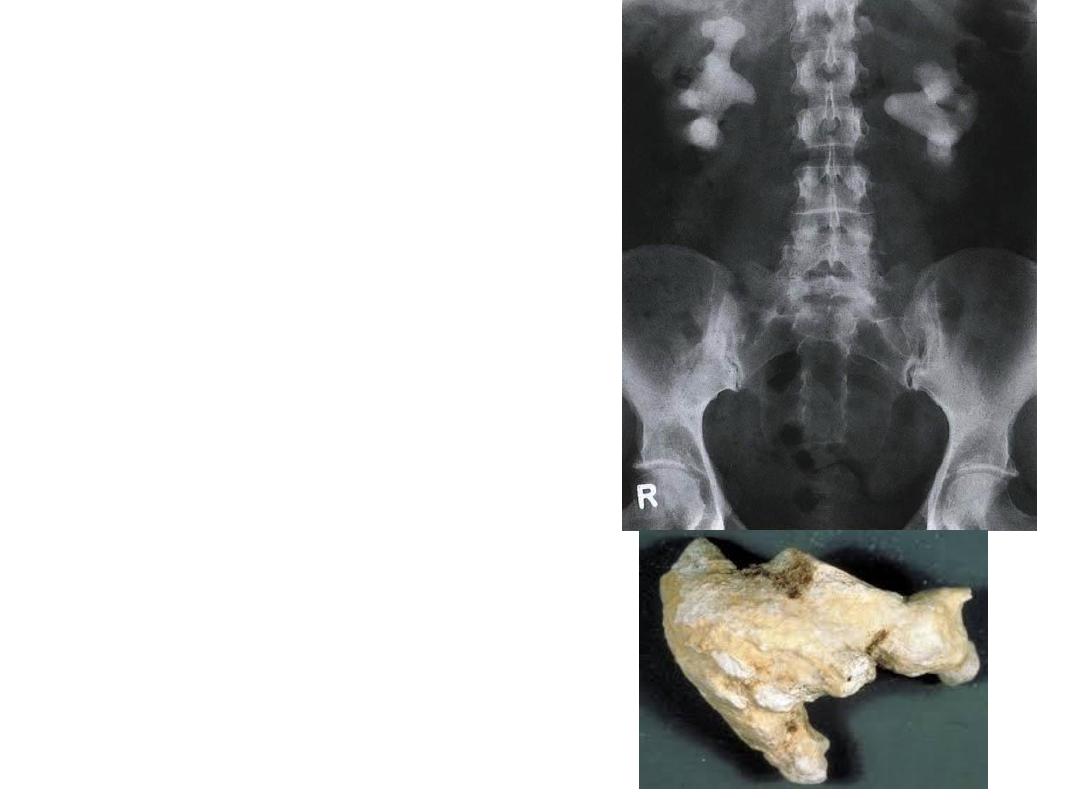
• This stone type accounts
for the majority of all
staghorn calculi
• Usually painless bs they
are smooth, white and
chalky appearance
• so grow to large size (pt
unaware) in contrast to
caox
23
A.F
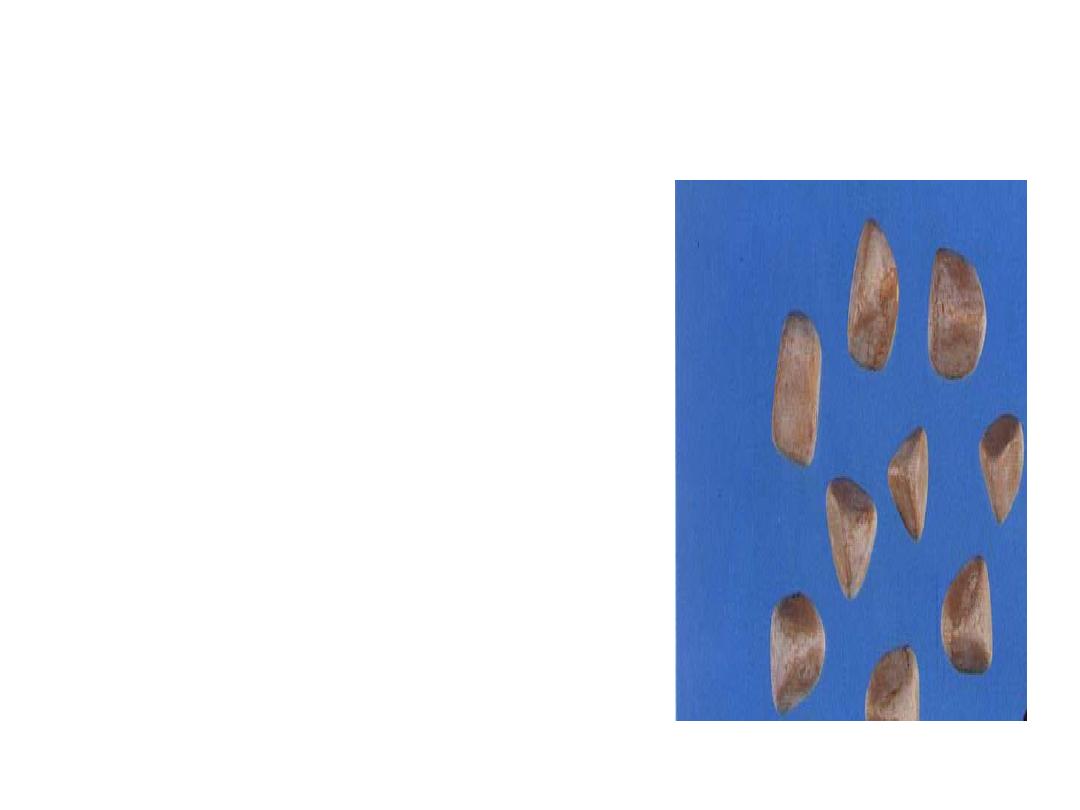
Uric acid stone
• Smooth & often multiple.
• colors range from yellow to
orange
• Lucent on KUB
• Filling defect on IVU
24
A.F
25
A.F

Cystine stones
• Account for about 1% of urinary calculi
• is secondary to an (inborn error of amino
acid metabolism inborn error of metabolism
resulting in abnormal intestinal (small
bowel) mucosal absorption and renal
tubular absorption.
26
A.F

C/f /kidney stone
• Kidney stones may present with symptoms or
asymptomatic found incidentally during
investigation of other problems.
• Presenting symptoms include pain or
Hematuria (microscopic 90 % or occasionally
macroscopic).
27
A.F

A.F
28
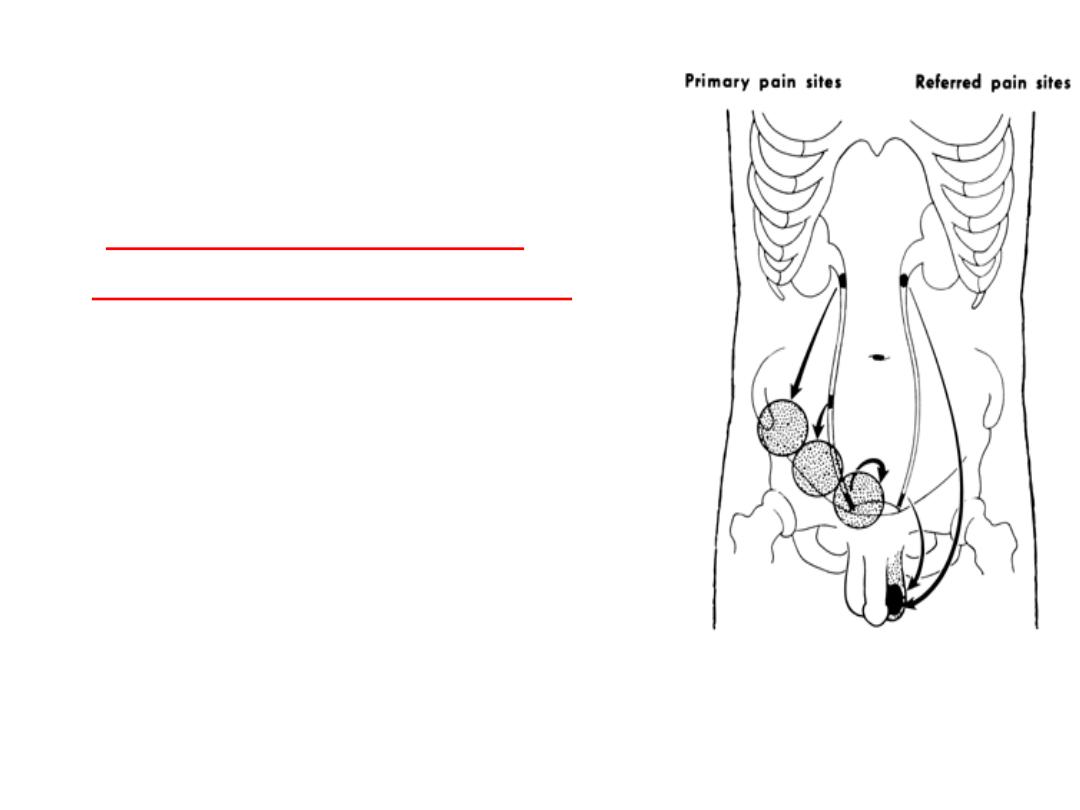
Fixed renal pain:
is located posteriorly in the renal angle,
anteriorly in the hypochondrium, or in both.
Renal angle (costovertebral angle) just lateral to
the sacrospinalis muscle beneath the 12
th
rib
posteriorly.
Acute flank pain renal colic
The majority of urinary
stones present with the
acute pain
Is caused by a stone
entering the ureter,
but it may occur with
• renal pelvis stone >1
cm obstructing the
PUJ
A.F
29
A.F
30
sudden onset of pain passing
from loin to groin, never
comfortable, always moving
(
due to acute obstruction &
stretching of collecting system
)
renal pain radiate along the
course of ureter and the
testicle since the nerve
supply to the kidney and
testis is the same
Pain of renal origin is frequently associated with
nausea & vomiting
because of reflex stimulation of
the celiac ganglion.
UTI is likely in presence of stones and is dangerous
when the kidney is obstructed.
+/
– fever, chills, rigors secondary to pyelonephritis
31
A.F
Renal pelvic/Struvite staghorn
• calculi classically
present with recurrent
UTI
• Or cause no
symptoms ? for long
periods, during which
there is progressive
renal damage.
• Bilateral staghorn,
uremia may be the
first indication of their
presence.
A.F
32
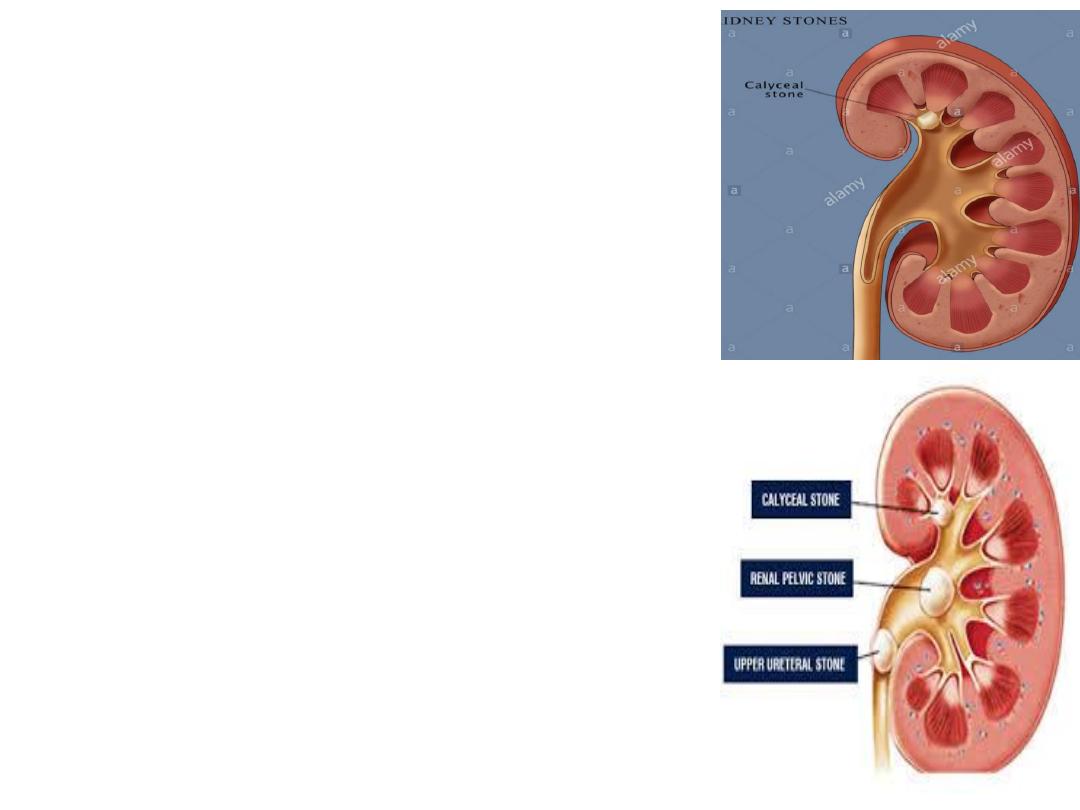
Calyceal stone
•
May cause flank discomfort
• May remain asymptomatic
for years
• May discover incidentally or
may present with symptomatic
ureteric or pelvic stone
A.F
33
Urinalysis
• Microscopic hematuria RBC >3/ HPF (usually)
• WBC>10/ HPF (sometime)
due to infection or irritation of urothelium
(
The mechanical
effect of stones irritating the urothelium may cause pyuria even in the
absence of infection)
• pH > 7.5: struvite
pH < 5.5: uric acid stone
•
Crystaluria
particular crystal types may give a clue as to the
composition of stones the patient is forming.
34
A.F
• Cystine and struvite crystals are always
abnormal.
• Other types of crystals are frequently
found in normal urinalysis.
35
A.F
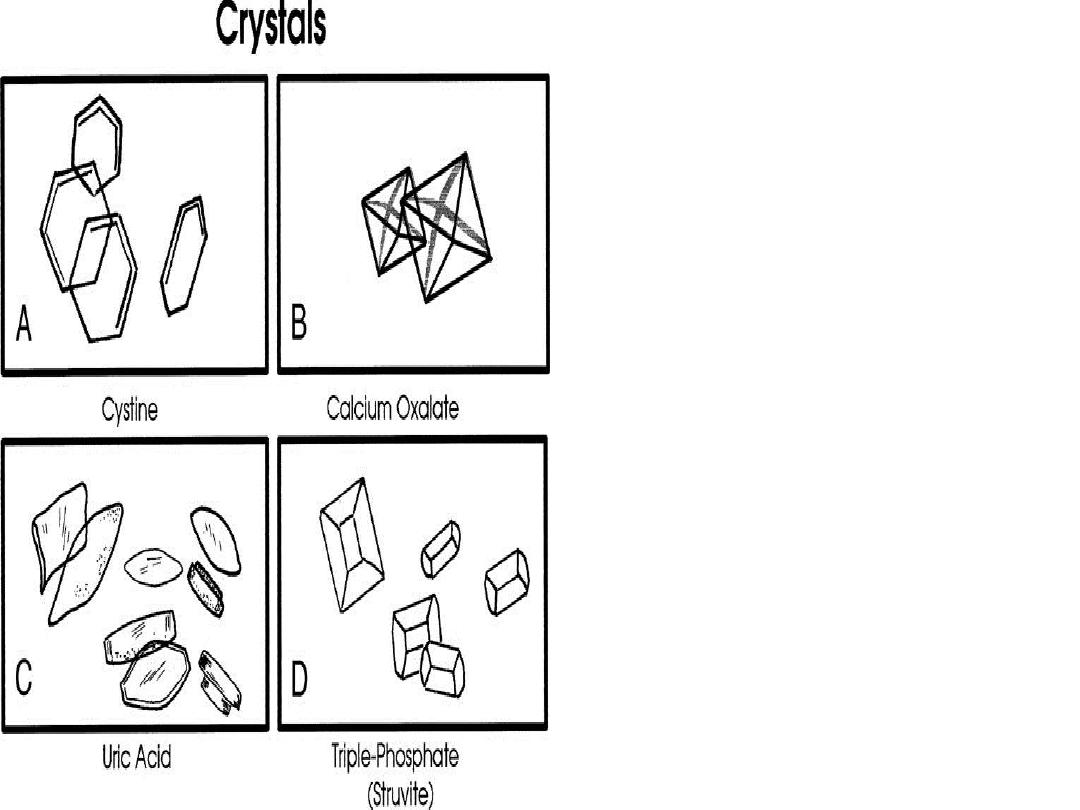
• “
Envelopes
shape=CAOX crys
• “coffin-lid” =struvite
• amorphous =uric acid
crystals
• Hexagonal crystals=cystin
36
A.F

Blood tests
• B.urea, S.creatinine
• S.calcium
• S.Uric acid
•
primary hyperparathyroidism (high serum calcium (>10.5 mg/dl) and low serum phosphorus
levels) need appropriate surgical teatment
.
37
A.F
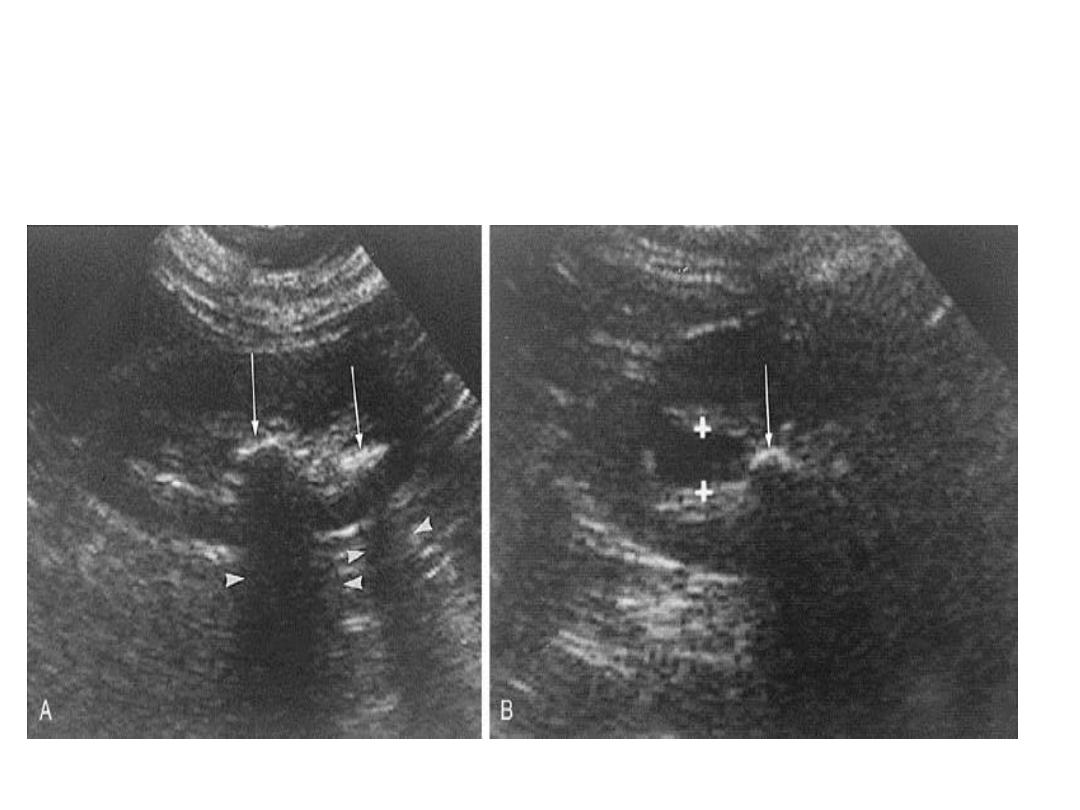
Imaging studies
1.Ultrasonography:
38
A.F

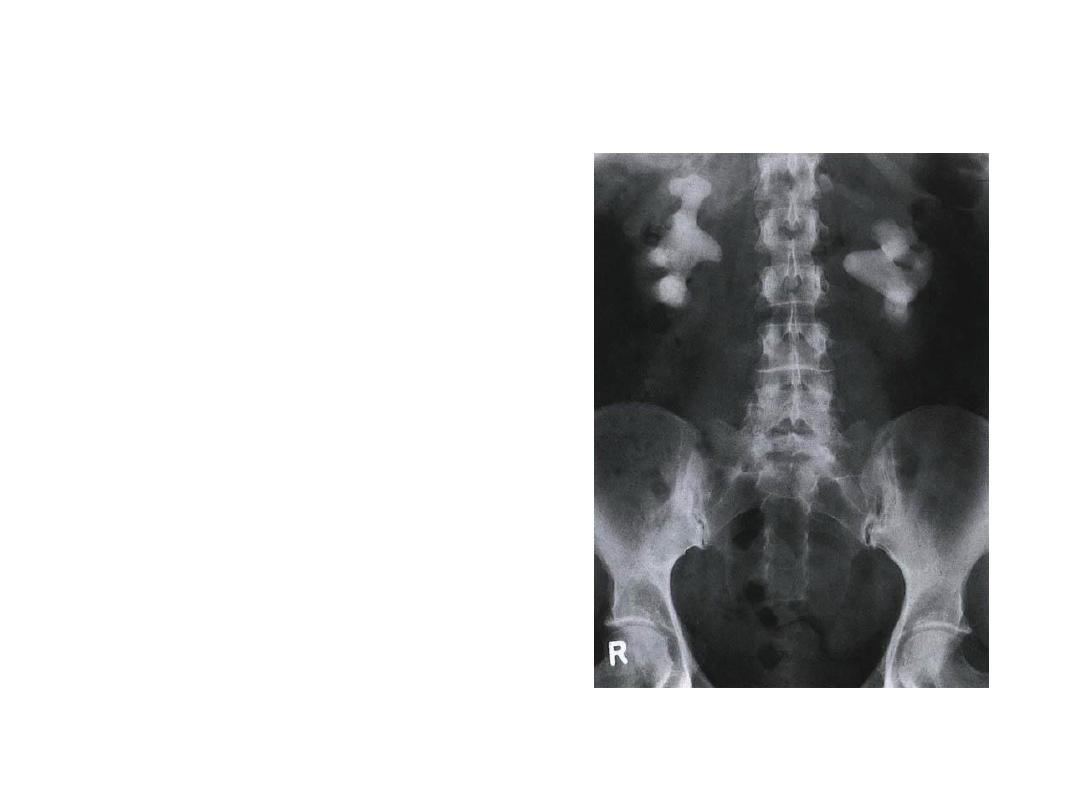
2.Radiography (KUB)
• Radiopaque stones:
calcium oxalate,
calcium phosphate,
struvite & cystine
• Radiolucent stones: uric
acid
39
A.F

• A combination KUB films &
ultrasonography
— is a useful test for
renal calculi.
40
A.F

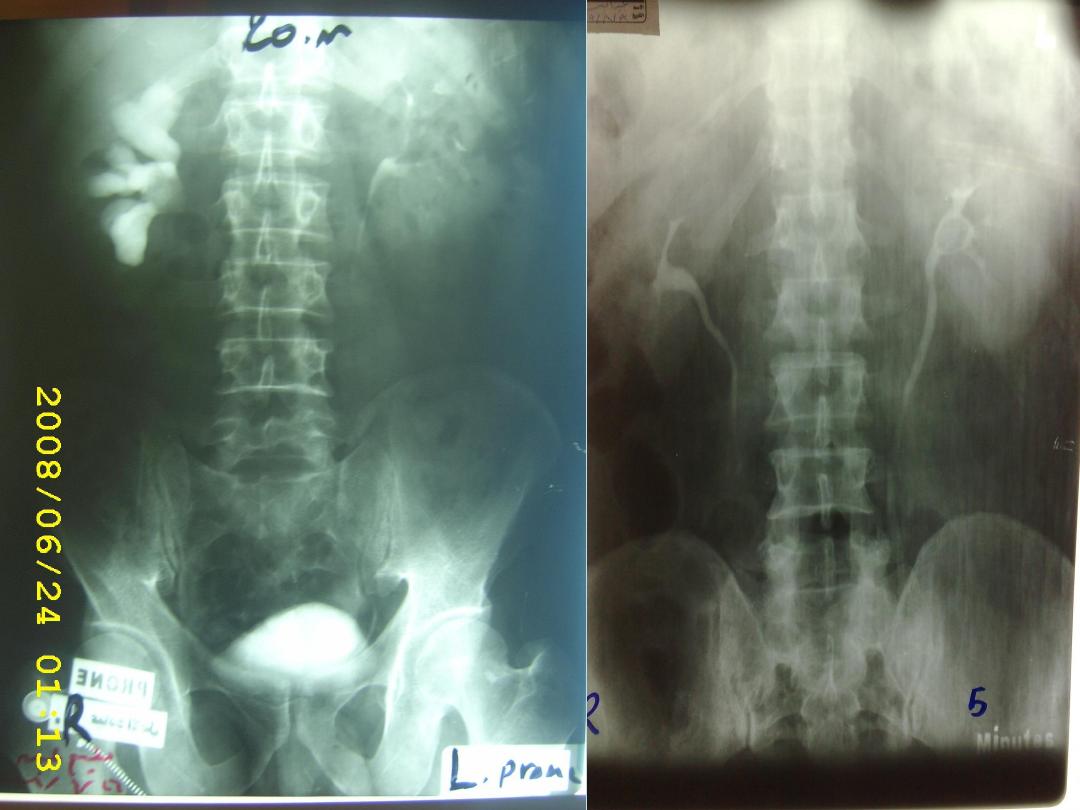
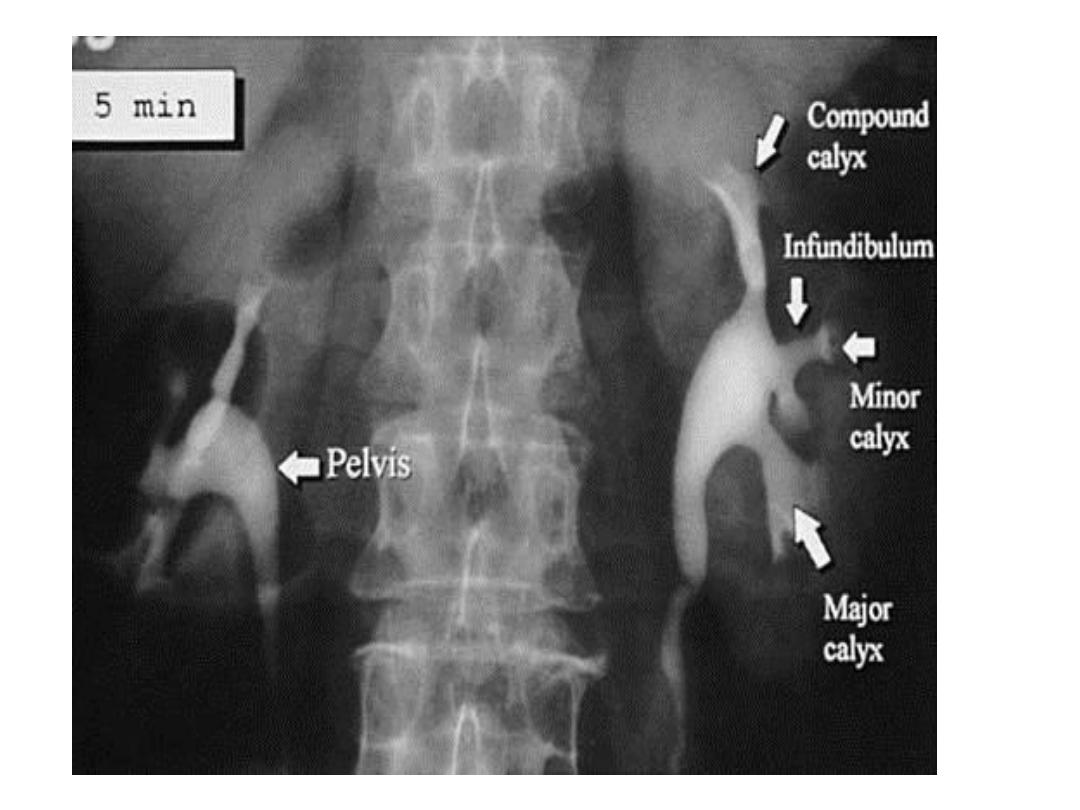
3.Intravenous urogram (IVU)
• is useful for evaluating
– the location of the stone,
– severity of obstruction from the calculus.
– functional information about the kidneys.
• is increasingly being replaced by CTU.
41
A.F
42
A.F
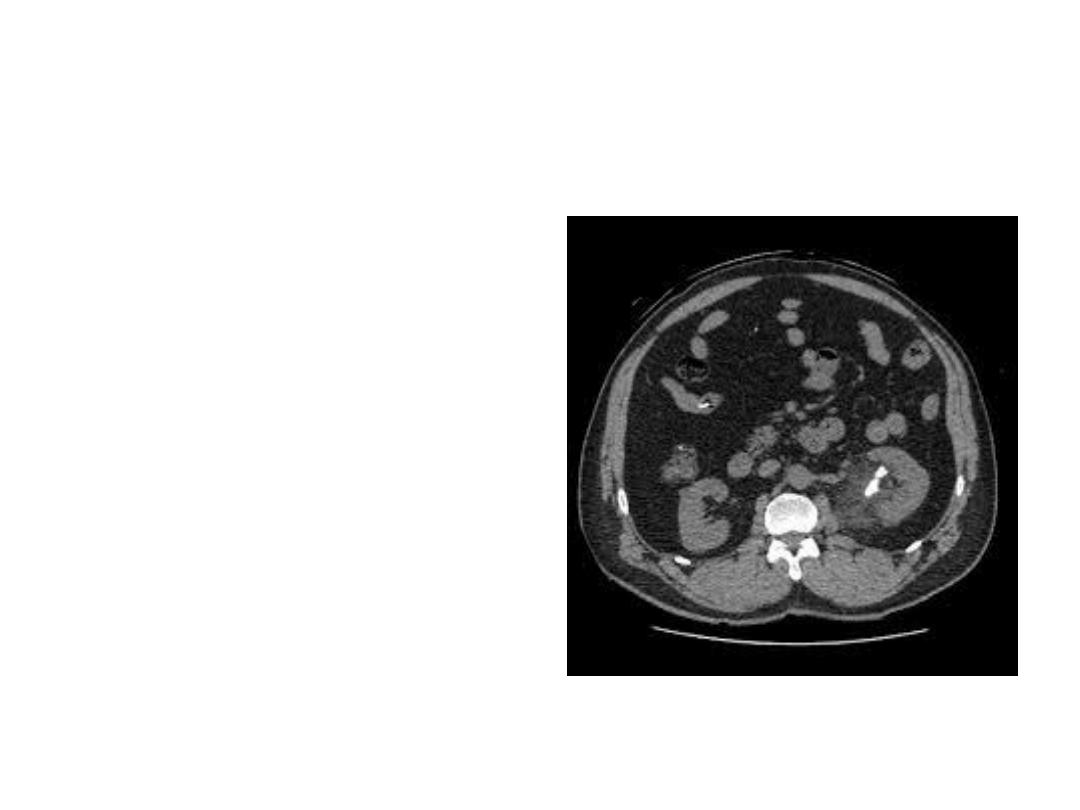
4.Computerized tomography
is a very accurate of
diagnosing all stones.
determination of
stone size & location
definition of
pelvicalyceal
anatomy.
A.F
43
