Urinary Tract
Infections
KIDNEY INFECTIONS
Dr. AMMAR FADIL

General principles
• Urinary tract infections (UTIs)
is inflammatory response of the urothelium to
bacterial invasion.
are common
affect men and women of all ages,.
The diagnosis of UTI is based on
symptomatology, urinalysis, & urine culture
findings
.
2\43

Definitions
• Pyuria
– is the presence of white blood cells (WBCs) in the
urine in dipstick or
10 WBC/HPF
in sediment of
centrifuged urine. occur either due to
– bacterial infection or
– sterile pyuria absence of bacteriuria carcinoma in
situ, TB infection, & stones
• Bacteriuria
– is the presence of bacteria in the urine which is
normally free of bacteria. symptomatic or
asymptomatic
3
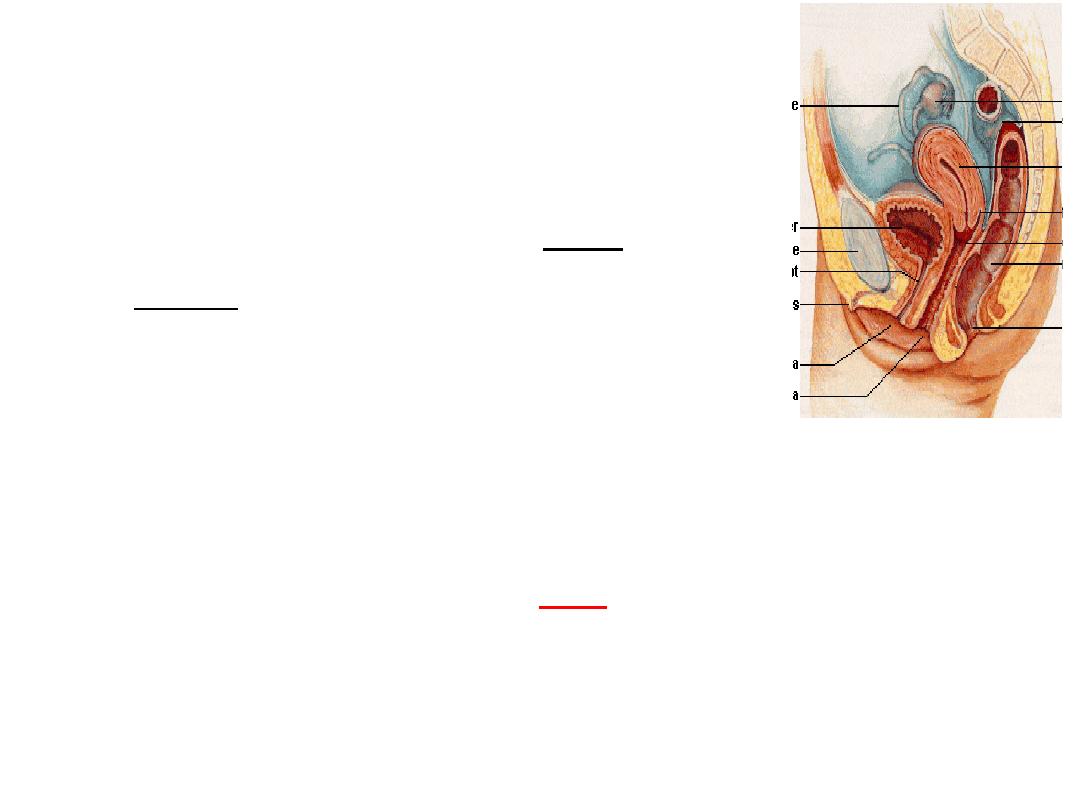
Routes of infection
• Ascending route (commonest)
bacteria derived from the large
bowel, colonize the perineum,
vagina, and distal urethra.
They ascend along the urethra to the
bladder (risk is increased in
♀ as the
urethra is shorter), causing cystitis,
& from the bladder they
may
ascend, via the ureters, to involve the kidneys
(pyelonephritis
).
14

Routes of infection
• Hematogenous route
Infection of the kidney is uncommon. Occurs in
patients with Staphylococcus aureus
bacteremia & TB
5

Predisposing Factors
1.stasis & obstruction:
– prostatic enlargement
– vesico ureteric reflux of urine VUR
– neurogenic bladder (spinal cord injury, DM)
2. foreign body:
– catheter
– stone
6

3.Decreased resistance
:
– diabetes mellitus
–
malignancy
–
immunosuppression
4. congenital anomaly
UPJ obstruction,
APCKD.
7
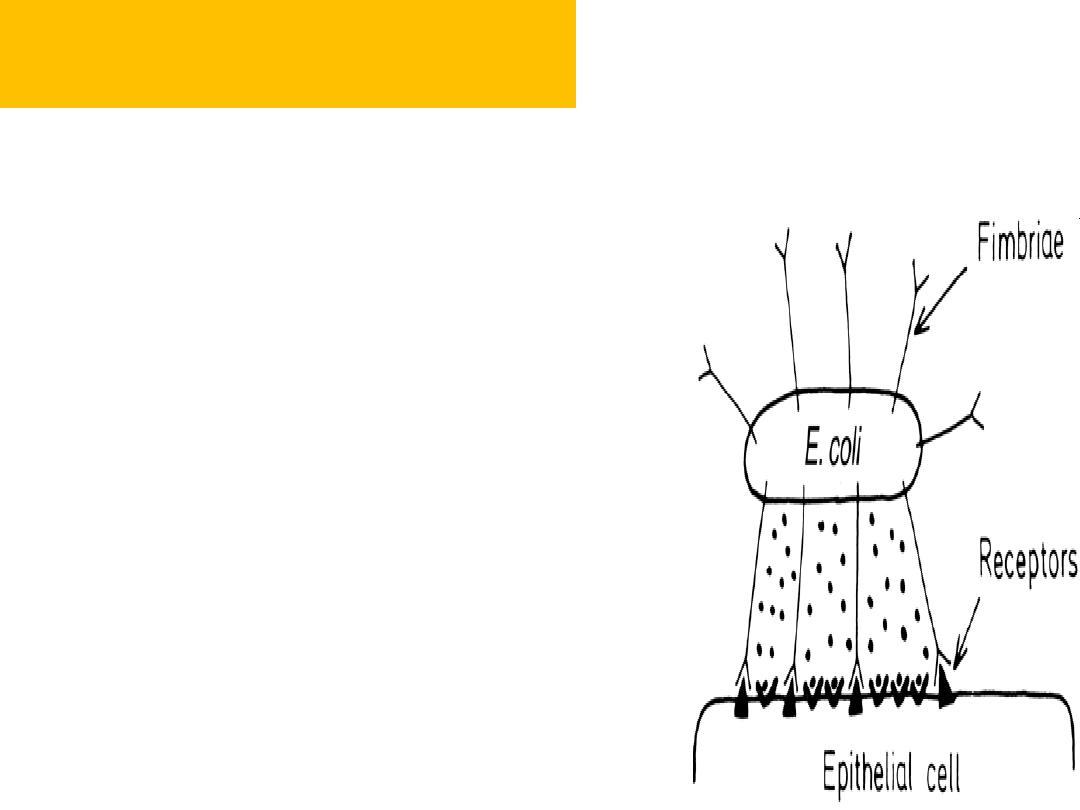
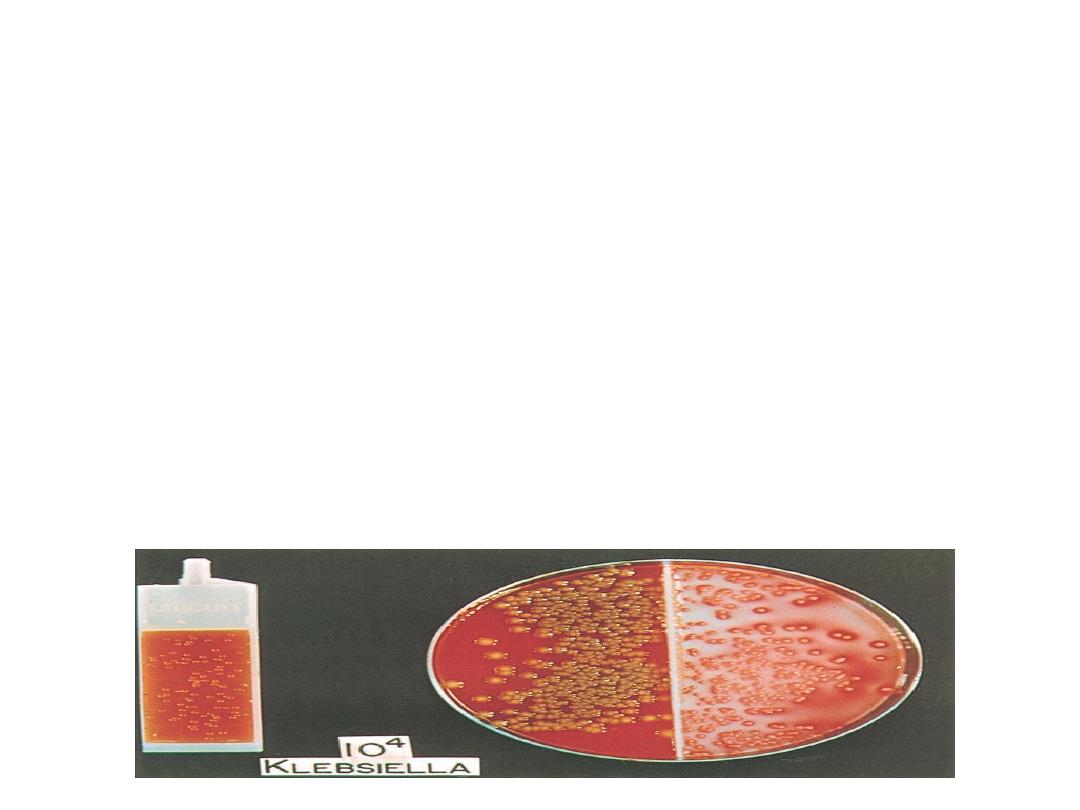
Urinary pathogens
• Most UTIs are caused by facultative anaerobes
usually originating from the bowel flora.
“
KEEPS
”
– K lebsiella
– E . Coli (85%)
– Enterococci
– Proteus mirabilis, pseudomonas
– S .saprophyticus , S. Fecalis
8

UTI
• Isolated UTI
– has an interval of at least 6 months between
infections.
• Recurrent UTI
– is >2 infections in 6 months, or 3 within 12
months.
• Unresolved infection
– is failure of the initial treatment course to
eradicate bacteria from the urine.
• antimicrobial resistance,
• patient noncompliance with therapy,
• insufficient antibiotic dosing
9
UTI basic investigation
• Urine dipstick MSU is used as a first-line
screening.
• GUE: the observation of WBC, bacteria & RBC
• Urine culture is the gold standard for the
diagnosis of UTI.
Imaging studies are not required in most cases of UTI
10

Further investigation
• US:
calculi & hydronephrosis
PVR
• VCUG
vesicoureteral reflux Dx.
11
Further workup
is needed in
upper tract infection (fever, flank pain,
malaise, that suggest
acute pyelonephritis, a
pyonephrosis, or perinephric abscess
Pregnant patient
Unusual infecting organism (e.g.,
Proteus),
suggesting the possibility of an ??
–
Recurrent UTIs
12
Lower UTI
cystitis
UTI
Upper UTI
Pyelonephritis
13
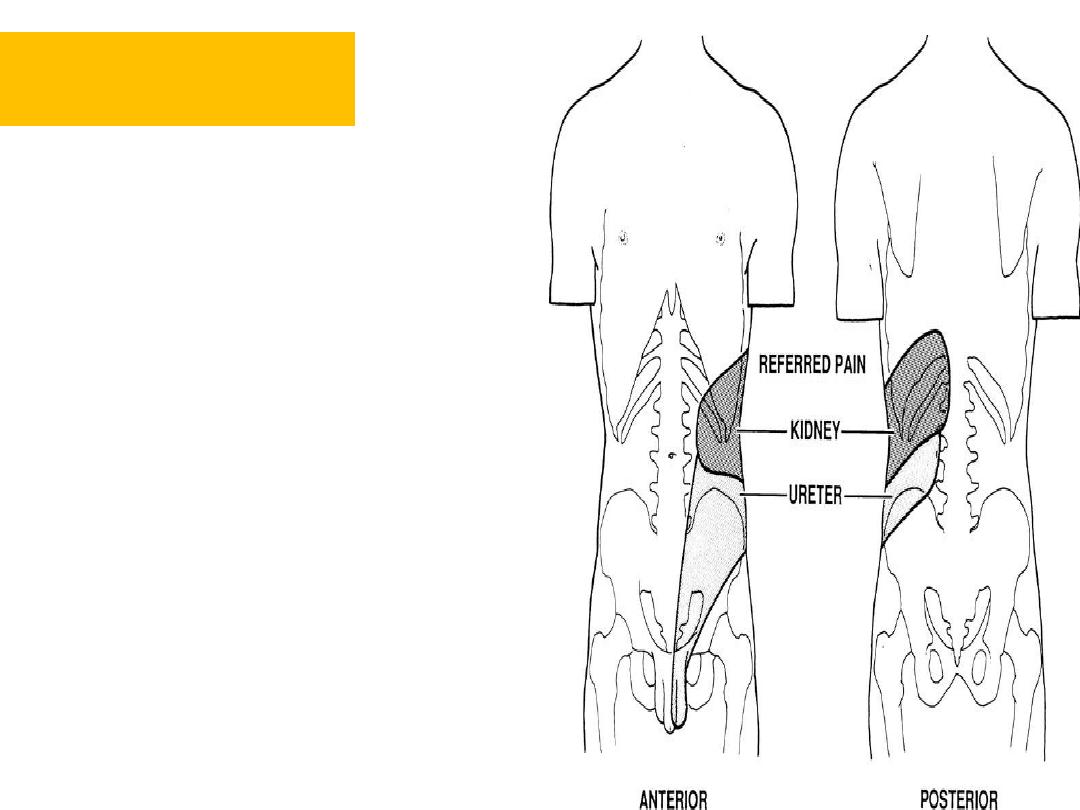
Acute pyelonephritis
• pyelonephritis is defined as
inflammation of the kidney
and renal pelvis
• A clinical diagnosis is based
on the presence of fever, flank
pain, and tenderness. It may
affect one or both kidneys.
14
Symptoms
The onset is usually abrupt.
fever(38.5 to 40 C),rigor & flank pain
symptoms of
cystitis
(dysuria, frequency, urgency, suprapubic
pain) These are usually suggestive of a lower
urinary tract infection that led to the ascending
infection, which resulted in the subsequent acute
pyelonephritis
.
Nausea and vomiting are common.
15
16
• Renal angle
tenderness.
Physical sign

Investigation
• GUE:
increased pus cells, WBC casts, & RBC.
Bacteria are often seen.
• Urine culture & sensitivity test.
• Blood tests may show a leukocytosis.
• RFT
• U/S & KUB: to see if there is an underlying
upper tract abnormality (such a ureteric stone)
17

Treatment
• involves the administration of antibiotics
according to the clinical presentation and
most likely causative organism, before
culture sensitivities are available
18
Treatment
patients who have a fever but are not
systemically unwell, outpatient oral Rx
1
st
choice is Fluoroquinolones
ciprofloxacin 500 mg PO bid, or
levofloxacin 750 mg PO qd)
2
nd
Trimethoprim-sulfamethoxazole
If the patient is systemically unwell, admit to
hospital and start IV fluids & parenteral
antibiotics
19

Parenteral antibiotics
We use one of the following:
1. 3
rd
generation cephalosporine
(
cefotaxime or ceftriaxone, ceftazidime
).
These are active against gram-negative bacteria. also has
activity against Pseudomonas aeruginosa.
2. I.V Fluoroquinolones (e.g., ciprofloxacin)
They exhibit good activity against
Enterobacteriaceae & P. aeruginosa
3.ampicilline & gentamycin
Parenteral antibiotics for 3 days then switch to oral for total
10-14 d
.
20
Treatment
However, if the patient does not respond
within 3 days to this regimen of IV antibiotics
(confirmed on sensitivities), a CT urogram
is essential.
• The lack of response to treatment suggests the
possibility of a
pyonephrosis
(i.e., pus in the
kidney, which, like any abscess, will only
respond to drainage)
21

Pyelonephritis of pregnancy
usually occurs
during 3
rd
trimester
when hydronephrosis & stasis in the
urinary tract are most pronounced .
Complications:
abortion or premature birth.
Rx:
Pregnant women should be
hospitalized and treated initially with
parenteral antimicrobial agents 3
rd
generation cephalosporine
22

Urinary infection in childhood
• It is one of the most common bacterial diseases in
children;
• is important to recognise because it may damage the
growing kidney.
• symptoms are often non-specific but the child
may pass cloudy or offensive urine.
Pain or screaming on micturition
child fails to thrive
unexplained pyrexia.
The older child may complain of loin pain
23
VUR
• VUR of urine is detectable in about 35% of
children with recurrent UTI
•
Up to 50% of children with UTI have an underlying anatomical abnormality (e.g.
reflux or obstruction).
24
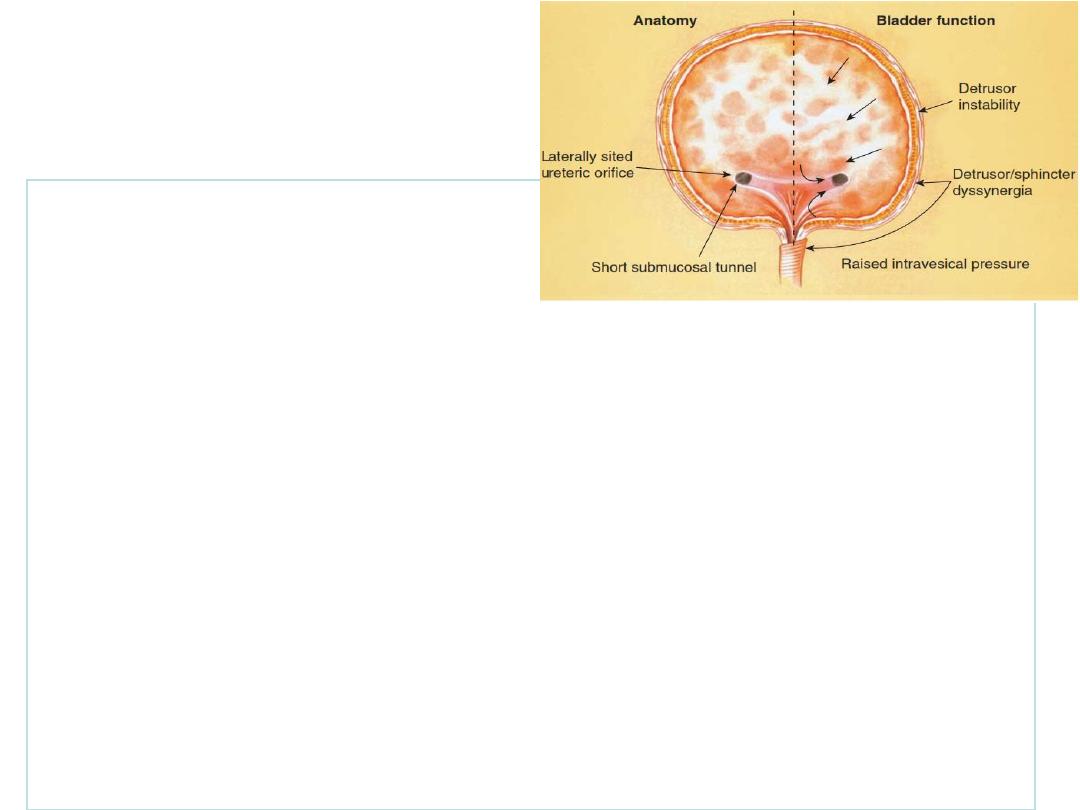
Pathogenesis of
VUR
• VUR
retrograde flow of urine from the bladder into the upper
urinary tract.
• The ureter passes obliquely through the bladder wall (1–2
cm), where it is supported by muscular attachments that
prevent urine reflux during bladder filling and voiding.
• Reflux occurs when the intramural length of ureter
is too short .The degree of reflux is graded I
–V.
25

Complications VUR
• Recurrent UTI
• reflux nephropathy with hypertension &
progressive renal failure.
– reflux nephropathy is the most common cause
of end-stage renal failure in children
26
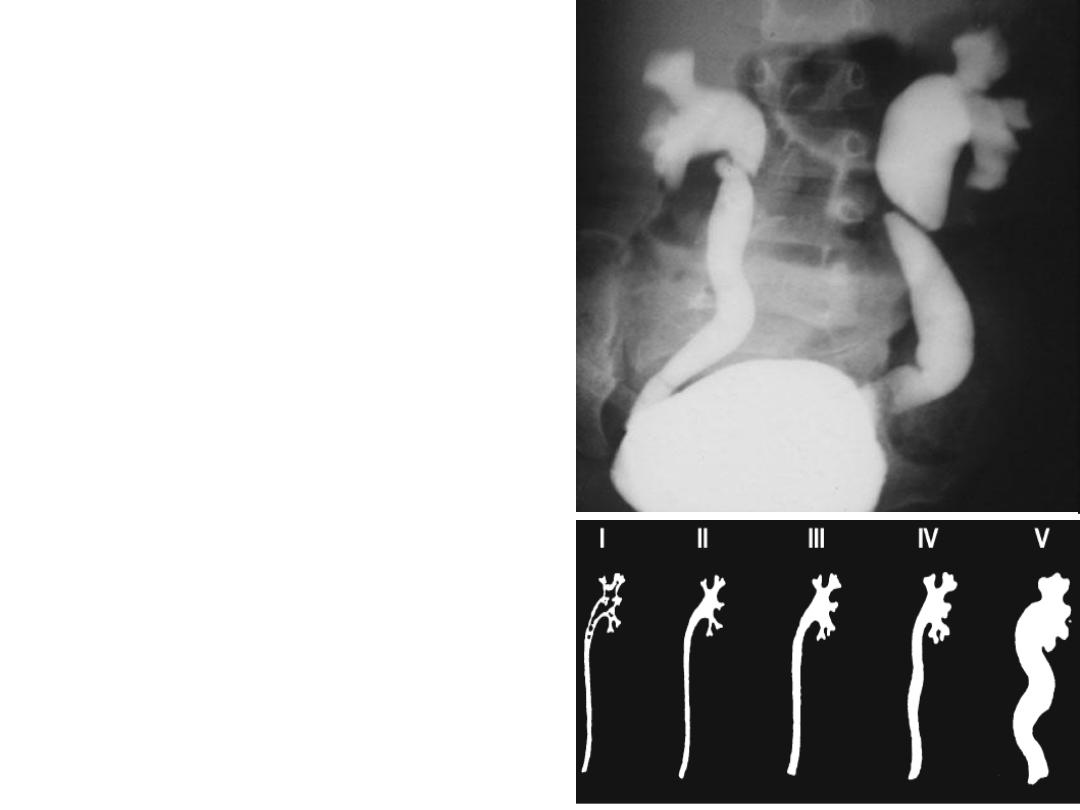
Dx VUR
VCUG to diagnose &
grade reflux
– Urinalysis
Urine culture a pure
growth of more than 10
5
organisms/ml.
– ultrasound scan
27

Treatment
• Medical treatment
Continuous antibiotic prophylaxis: e.g trimethoprim 1
–2
mg/kg/day, usually as a single night-time dose.
Endoscopic
• subureteric injections
(Bulking agent) e.g Deflux
• Surgery
Surgical reimplantation of the ureters is
reserved for those in whom
conservative measures fail.
28
Chronic pyelonephritis
Refers to the small, contracted, atrophic kidney
that has been produced by bacterial infection,
It can be a radiological or pathological diagnosis.
chronic pyelonephritis is the end result of
longstanding reflux or obstruction. These
processes damage the kidneys, leading to
scarring.
29
Clinical Presentation
•
Most of the changes of chronic
pyelonephritis seem to occur in infancy,
because the growing kidney is most
susceptible to scarring
.
•
in adults renal damage is rare in non
obstructive UTIs
•
There are no symptoms of chronic
pyelonephritis until it produces renal
insufficiency, and then the symptoms are similar
to chronic renal failure.
30

Pyonephrosis
• This is an infected hydronephrosis, the
infection being severe enough to cause
accumulation of pus with the renal pelvis
and calyces of the kidney.
• causes include ureteric obstruction by
stone and PUJ obstruction.
31
Pyonephrosis
• Clinical presentation: patients very ill ,high fever
,flank pain ,chills ,renal tenderness, Previous
history of urinary calculi, infection or surgery.
• Management antibiotics and drainage of
infected pelvis ( ureteral catheter, nephrostomy)
32
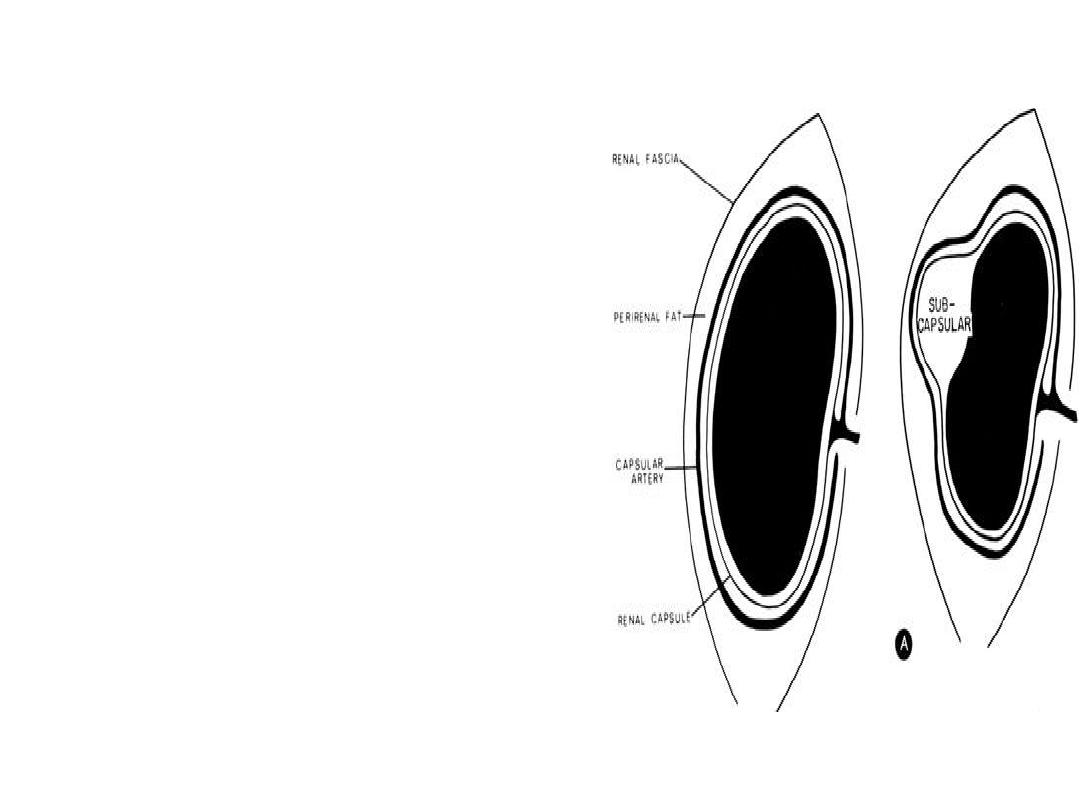
perinephric abscess
• develops as a
consequence of extension
of infection outside the
parenchyma of the
kidney.
Patients with pyonephrosis,
particularly when a
calculus is present in the
kidney, are susceptible to
perinephric abscess
formation.
33

Perinephric abscess
These patients are often diabetic, &
associated conditions such as an
obstructing ureteric calculus.
treatment is surgical drainage
34

Renal tuberculosis
The kidney is among the most common sites for
extrapulmonary tuberculosis.
Renal tuberculosis (TB)
is caused by Mycobacterium tuberculosis.
arises from haematogenous spread
from a distant focus which is impossible to identify.
are usually confined to one kidney.
the latent period between exposure &
reactivation of disease is 10- 40 yr
35
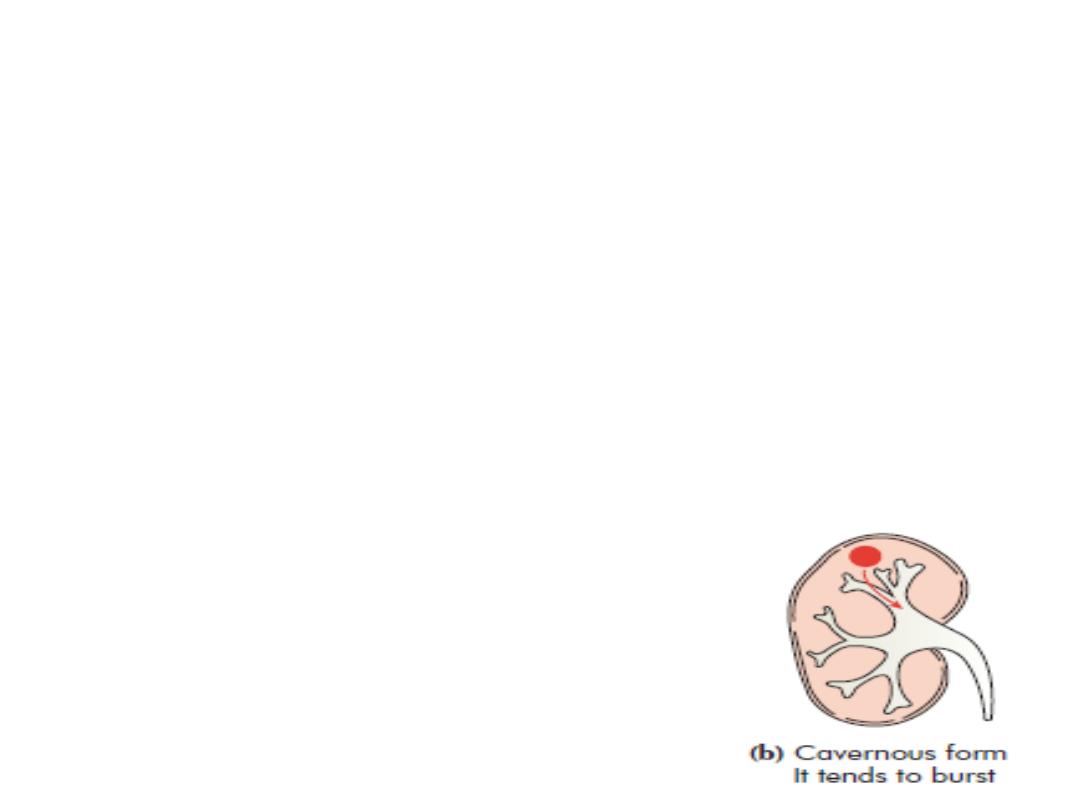
Kidney
Hematogenous spread causes granuloma
formation in the renal cortex, associated with
caseous necrosis of the renal papillae and
deformity of the calyces, leading to release of
bacilli into the urine. This is followed by
healing fibrosis and calcification, which
causes destruction of renal architecture and
autonephrectomy.
36

Ureters
• Seeding of the urine may also result in
involvement of the bladder and male
genital organs
• TB Spread is directly from the kidney and
can result in stricture formation.
• Bladder Infection is usually secondary to
renal infection. Disease progression
causes fibrosis and contraction (resulting
in a small capacity ‘thimble’ bladder),
37

• Renal tuberculosis is often associated
with tuberculosis of the bladder and
typical tuberculous granulomas may be
visible in the bladder wall
38

Clinical features
• Because of the slow progression and variable
course of the disease, there is no classic
presentation.
• Renal symptoms gross hematuria; dull flank
discomfort; and ureteral colic secondary to
passage of clots, debris, or calculi.
• Constitutional complaints such as fevers, chills, night sweats,
weight loss, and malaise are uncommon.
39

• It is only when the bladder is involved
that the patients become severely
symptomatic.
• Frequency is the most common
presenting symptom and is often
progressive and occurs during the day
and at night. Pain, urgency, and dysuria
are also common.
40

physical examination
• A chronic draining fistula tract from
previous renal surgery.
• Patients with chronic epididymitis
unresponsive to therapy should also be
evaluated.
41

Investigation
• Urine: At least 3 early morning urines . A
typical finding is sterile pyuria (leukocytes,
but no growth). Ziehl
–Neelsen staining will
identify these acid- & alcohol fast bacilli
(cultured on Lowenstein
–Jensen medium).
pyuria C\S no growth of bacteria ?
42

investigations
• KUB: Findings include renal
calcification (cement kidney)
• IVU: irregular calyces,
hydronephrosis
caused by stricture of the
ureter
.
• CXR and sputum
• Tuberculin skin test
• Cystoscopy: bladder studded with
granulomas which cluster
particularly around the ureteric
orifices
.
43

Treatment
• Medical Rx is with 6 months of isoniazid,
rifampicin, and pyrazinamide
• If the kidney has no function it is best to
perform a nephroureterectomy .
44
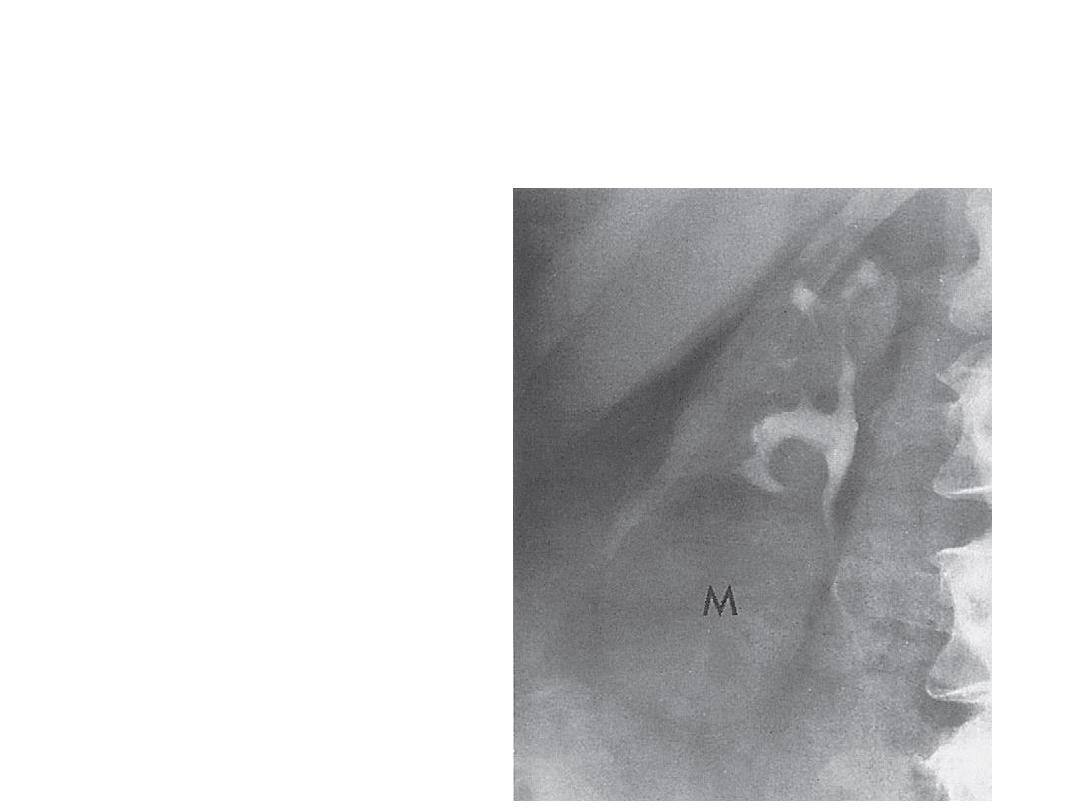
Investigation
• Urinary sediment
may show pus cells,
proteinuria.
• IVP: irregularity of
the kidney outlines
with blunting and
dilation of calyces
45

Management
• treating infection, if present; and
monitoring and preserving renal
function.
46
