1
LEC 4-5
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
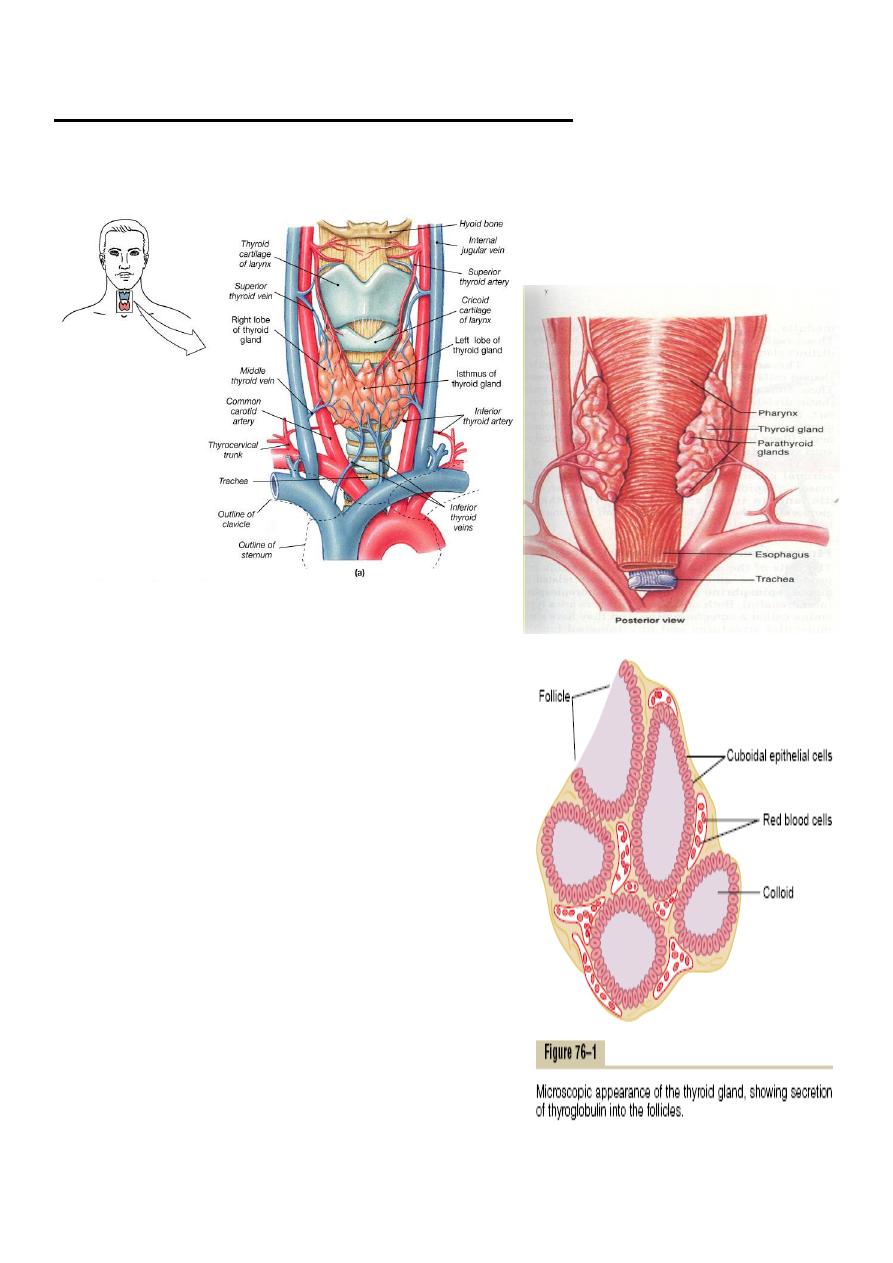
The Thyroid Gland
Lies near the thyroid cartilage of the larynx
Two lobes connected by an
isthmus

2
The thyroid gland
Formation & secretion of thyroid hormones :
The main hormones secreted by the thyroid are thyroxine(T4)
&triiodothronine(T3) T3 is also formed in the peripheral tissues
by deiodination of T4.both hormones are iodine containing
amino acids.T3 is more active than T4.
Iodiedpump :
The first stage in the formation of thyroid hormones is transport
of iodieds from the blood into the thyroid glandular cells &
follicles this is called iodiedtrapping , in normal gland the iodied
pump concentrates the iodied to about 30 times its
concentration in blood. the rate of iodide trapping is influenced
by several factors , the most important is the concentration of
TSH
Thyroglobulin & chemistry of thyroxin &triiodothyronin
formation
-Thyroglobulin is a large glycoprotein molecule has a
molecular weight of about 335,000.the molecule of
thyroglobulin contains 70 tyrosine amino acids &they are
the major substrates that combine with iodine to form
thyroid hormones .thus thyroid hormones form within the
thyroglobulin molecule .
-Thyroglobulin is synthesized in the thyroid cells & secreted
into the colloid .the first step in the formation of thyroid
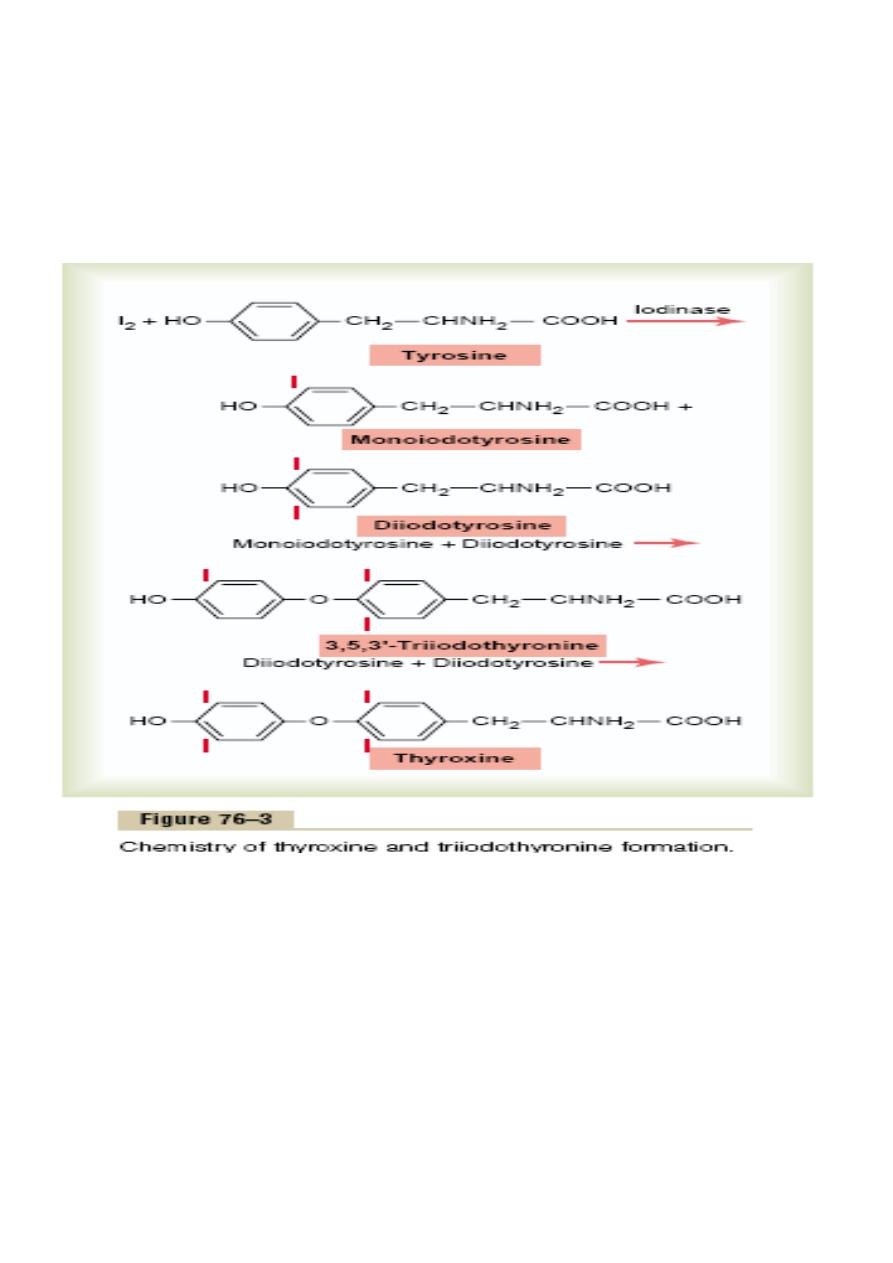
3
hormones is conversion of iodide ions to an oxidized form
of iodine , this oxidation of iodine is promoted by the
enzyme peroxidase . tyrosine is first iodized to
monoiodotyrosine (MIT) this is next iodinated to form
diiodotyrosin (DIT).
Two DIT molecules then undergo an oxidative condensation
to form T4.or one molecule of MIT couples with one
molecule of DIT to form triiodothyronine
Each thyroglobulin molecule contains 30 thyroxin
molecules & a few triiodothyronine molecules.in this form
thyroid hormones are stored in the follicles for 2-3 months.
Release of thyroxin &triiodothyronine from the thyroid
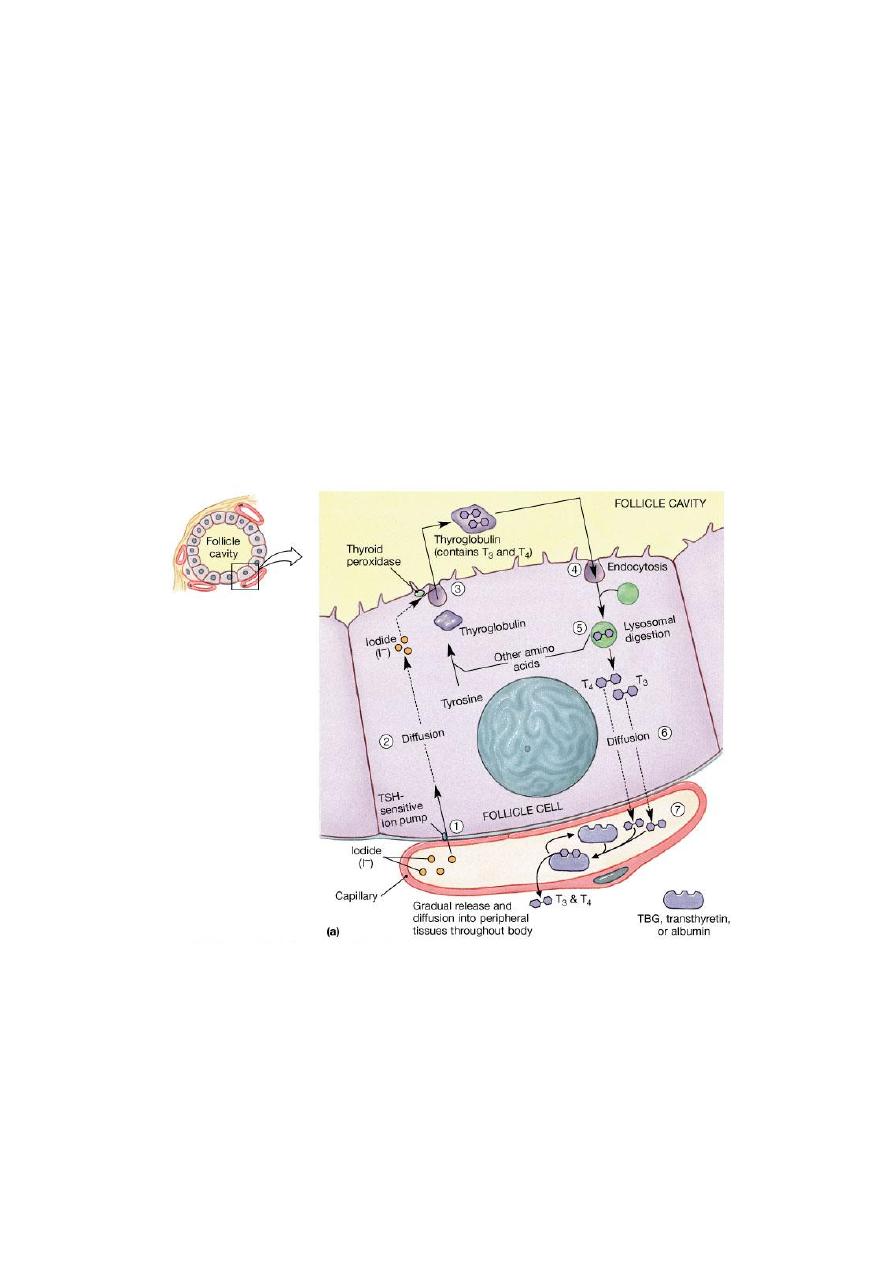
4
gland.
The human thyroid secrets about 80µg (103 nmol)T4,& 4µg
T3(7nmol).the thyroid cells ingest colloid by endocytosis .in the
cells the globules of the colloid merge with lysosomes .the
peptide bonds between the iodinated residuse& the
thyroglobulin are broken by the proteases in the lysosomes
&T4, T3,MIT,DIT are librated into the cytoplasm. the iodinated
tyrosins are deiodinated by deiodinase enzyme ,T4&T3 pass into
the circulation.
Figure 18.12 The Thyroid Follicles
Physiologic functions of thyroid hormones
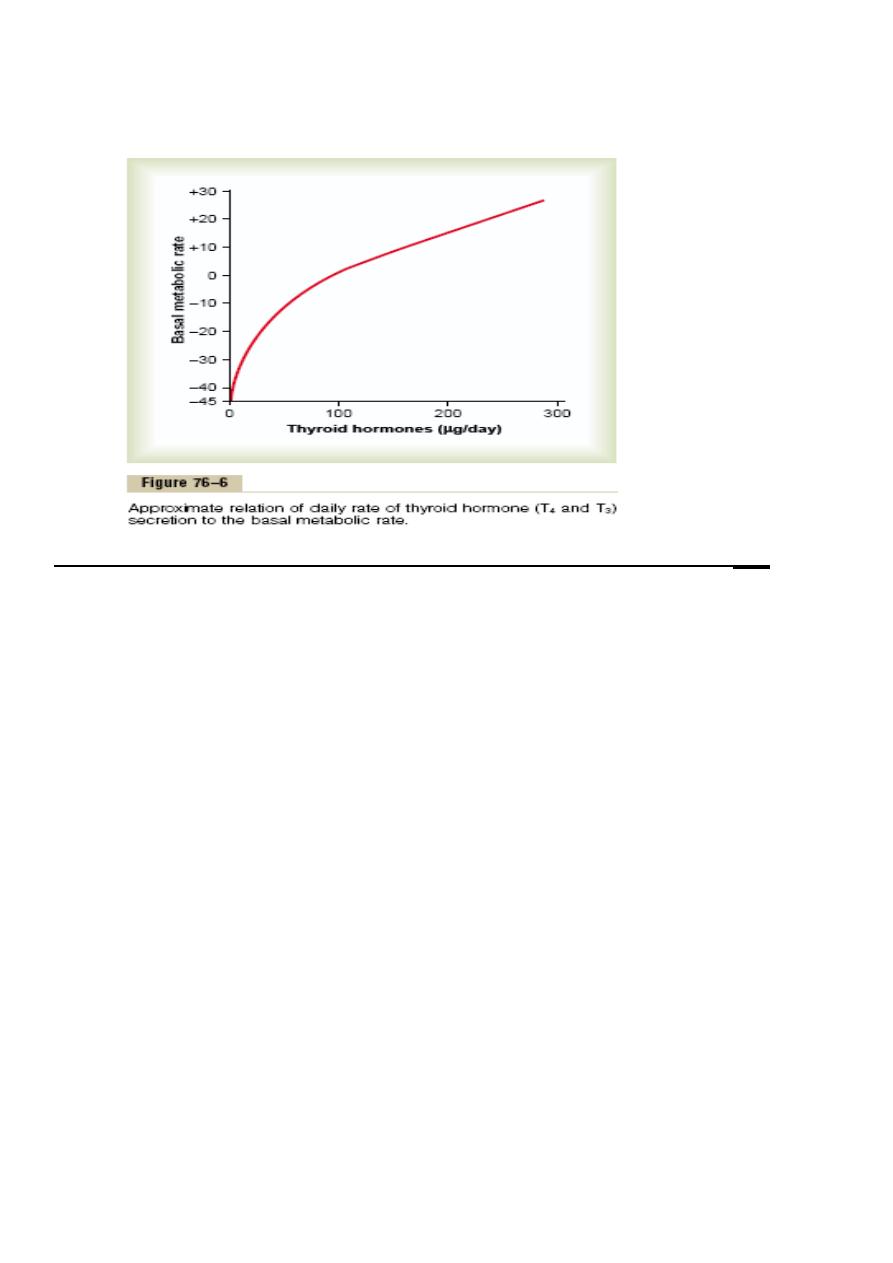
Thyroid hormones increase cellular metabolic activity the BMR
increase to 60-100% above normal when large quantities of
5
hormone are released .the rate of utilization of foods for energy
is accelerated ,the rate of protein synthesis is increased .
thyroid hormones increase the number& activity of the
mitochondria .
thyroid hormones increase active transport of ions through cell
membranes.
1.Effect of thyroid hormones on growth:
The effect of thyroid hormones on growth manifest in growing
children.
• In those who are hypothyroid the rate of growth is
retarded.
• In those who are hyperthyroid excessive skeletal growth
occur causing the child to become taller at an earlier age.
• An important effect is to promote growth & development
of the brain during fetal life &for first few years of
• postnatal life.
2.effects of thyroid hormones on specific bodily mechanisms:
1. Stimulation of carbohydrate metabolism , it causes rapid
uptake of glucose by cells , increased glycolysis , enhanced
gluconeogenesis , increased insulin secretion.
2. Stimulation of fat metabolism, decreases the
concentrations of cholesterol,phospholipids, and
triglycerides in the plasma
3. Increased requirement for vitamins.
6
4
.
Increased BMR.
5
.
Decreased body weight.
مهم
3.Effect of thyroid hormones on cardiovascular system
1. Increased blood flow and cardiac output . Increased
metabolism in the tissues causes more utilization of oxygen
than normal & releases greater than normal metabolic end
products from the tissues , these effects cause
vasodilatation so it increase blood flow & as a consequence
cardiac output is increased .
2. Increased heart rate thyroid hormone seems to have a
direct effect on the excitability of the heart.
3. Increased heart strength ,The increased enzymatic activity
caused by increased thyroid hormone production
apparently increases the strength of the heart when only a
slight excess of thyroid hormone is, but when increased
markedly the strength of heart muscle decrease because of
long-term excessive protein catabolism..
7
4. Normal arterial pressure : The mean arterial pressure
usually remains about normal after administration of
thyroid hormone. Because of increased blood flow
through the tissues between heartbeats, the pulse pressure is
often increased, with the systolic pressure elevated in
hyperthyroidism 10 to 15 mm Hg and the diastolic pressure
reduced a corresponding amount.
4. Increased respiration : the increase in utilization of oxygen &
formation of co2 increases the rate & depth of respiration .
5. Increased G.I.T motility : thyroid hormone increases both the
rate of secretion of digestive juices & the motility of G.I.T .
Diarrhea often result from hyperthyroidism while constipation
from hypothyroidism .
6. Excitatory effects on the C.N.S : the hyperthyroid subject
have extreme nervousness , anxiety .
7. Effect on the function of the muscles: increased thyroid
hormone weakens the muscles because of protein catabolism ,
while hypothyroidism causes the muscle to become relax slowly
after contraction .
•
Muscle Tremor. One of the most characteristic signs of
مهم
hyperthyroidism
is a fine muscle tremor
8. Effect on sleep
: Because of the exhausting effect of thyroid
hormone on the musculature and on the central nervous system, the
hyperthyroid subject often has a feeling of constant tiredness, but
because of the excitable effects of thyroid hormone on the synapses, it
is difficult to sleep..
8
9. Effect on other endocrine glands
: increased thyroid hormones
increase the rate of secretions of most endocrine glands . Increased
thyroxin secretion increases the rate of glucose metabolism
everywhere in the body and therefore causes a corresponding need for
increased insulin secretion by the pancreas.
Effect on other endocrine glands
Also, thyroid hormone increases man metabolic activities
related to bone formation and, aa consequence, increases the
need for parathyroid hormone. Thyroid hormone also increases
the rate at which adrenal glucocorticoids are inactivated by the
liver. This leads to feedback increase in adrenocorticotropic
hormone production by the anterior pituitary and, therefore,
increased rate of glucocorticoid secretion by the adrenal glands.
Effect of Thyroid Hormone on Sexual Function
For normal sexual function, thyroid secretion needs to be
approximately normal. In men, lack of thyroid hormone is likely
to cause loss of libido; great excesses of the hormone, however,
sometimes cause impotence.
In women, lack of thyroid hormone often causes menorrhagia
and polymenorrhea— that is, respectively, excessive and
frequent menstrual bleeding.
9
In the hyperthyroid woman, oligomenorrhea, which means
greatly reduced bleeding, is common, and occasionally
amenorrhea results.
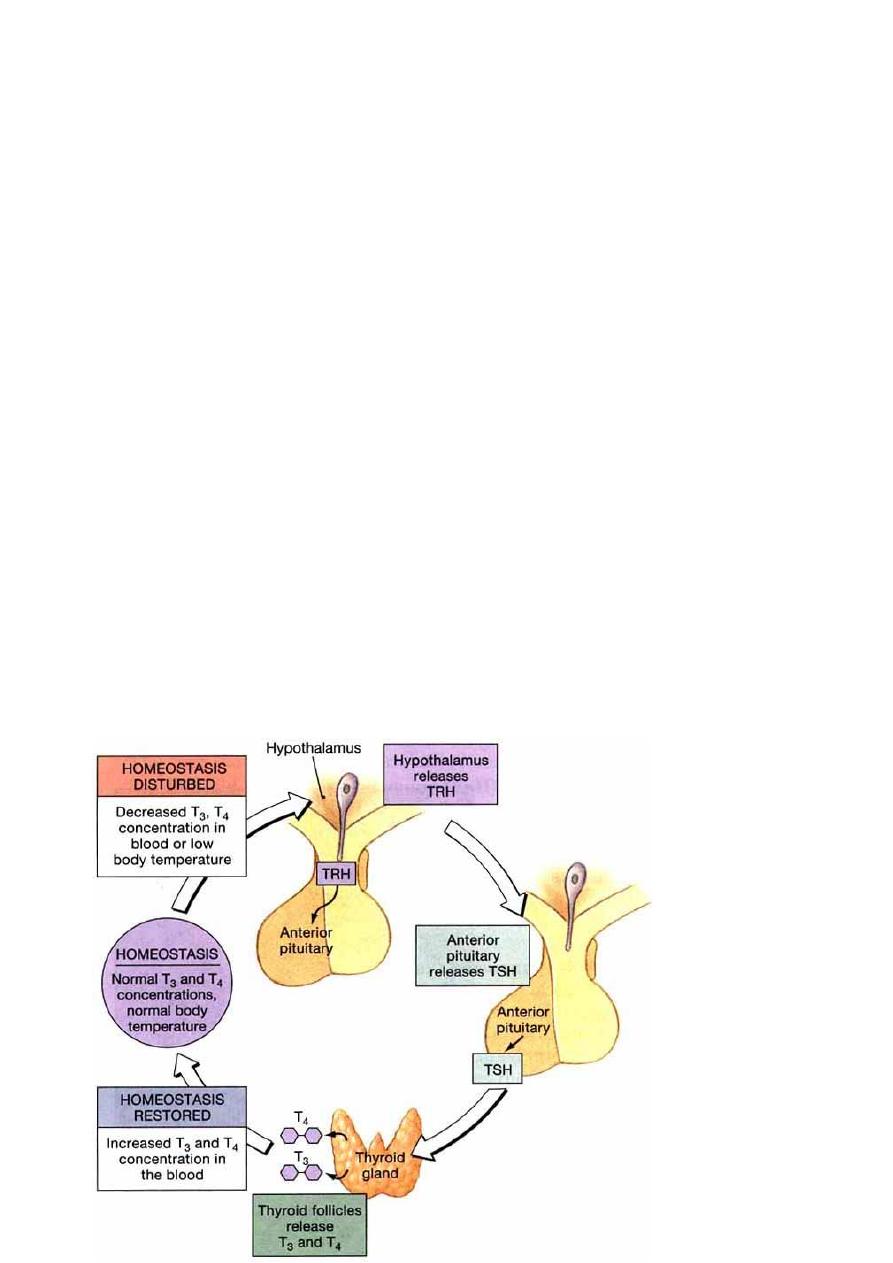
Regulation of thyroid hormone secretion
The anterior pituitary secretion of TSH is controlled by TRH
which secreted by nerve endings in the median emninence of
the hypothalamus , then TRH is transported to the anterior
pituitary by way of hypothalamic – hypophysial portal blood .
TRH is a tripeptideamide , it stimulates the anterior pituitary to
secrete TSH .
TSH also called thyrotropin , is a glycoprotein with a molecular
weight of about 28000 , this hormone increases the secretion of
thyroxin & tri-iodothyronine by the thyroid gland .
increased
thyroid
hormone in
body fluids ,
decreases
secretion of
TSH by the
anterior
pituitary .

10
Diseases of the thyroid gland
Hyperthyroidism :
The thyroid gland is increased 2 – 3 times normal size and
increase thyroid secretion .
Symptoms :
1. Excitability .
2. Intolerance to heat .
3. Increase sweating .
4. Weight loss .
5. Diarrhea .
6. Muscle weakness .
7. Nervousness .
8. Fatigue .
9. Tremor of hands .
Hypothyroidism :
Decreased thyroid hormone secretion .
symptoms :
1. Fatigue and sleep up to 12 -14 h / day .
2. Slow heart rate and decreased cardiac output , decreased
blood volume .
3. Increased body weight .
4. Constipation .
11
5. Mental sluggishness .
6. Husky voice .
7. Decreased hair growth .
Thyroid Disorders
Grave’s disease
• Severe form of hyperthyroidism
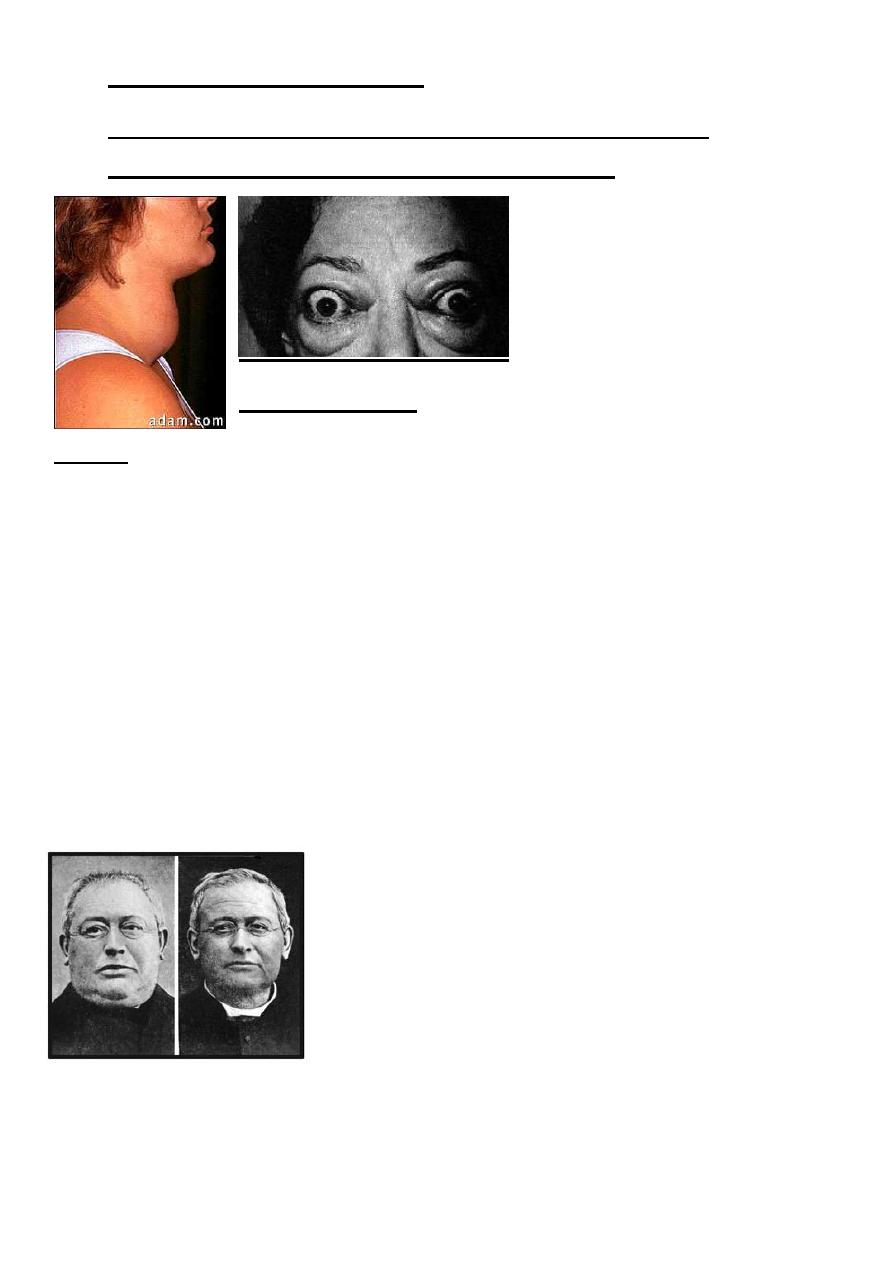
12
• More common in women
• Symptoms: strained and tense facial expression,
exophthalmia, goiter, nervous irritability
Exophthalmos
goiter
Myxedema
• Face becomes swollen, weight increases and memory
begins to fail
• Treatment is daily thyroid hormone
• Follow-up tests to measure TSH blood levels are important
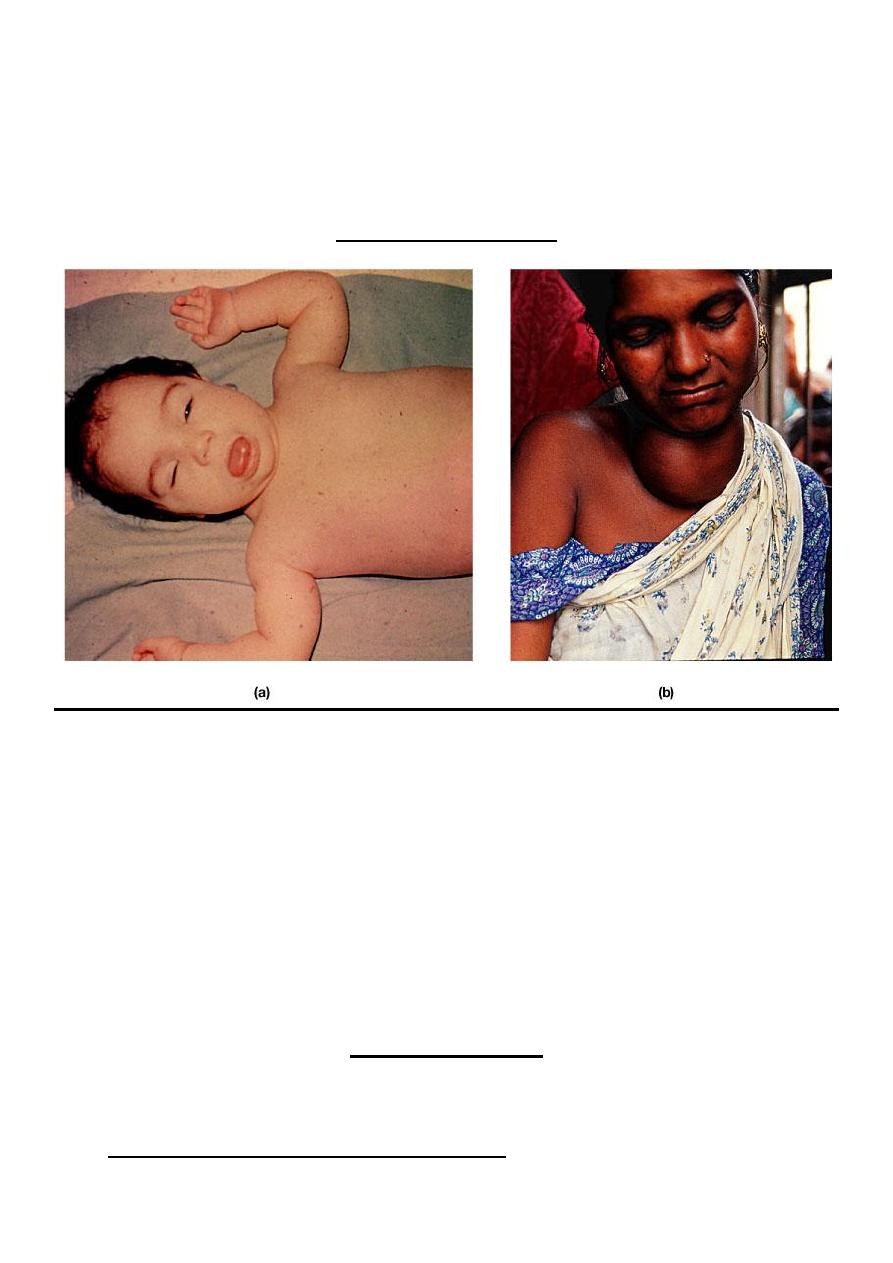
Cretinism
13
Develops early in infancy or childhood-
-Lack of mental/physical growth resulting in mental
retardation and malformation
-Sexual development and physical growth does not reach
beyond 7-8 year old children
Normal development cannot be completely restored w/ tx.-
By: Mohamad J Rawi
9/11/2016
14
PHYSIOLOGY
lec. 6-7 Dr. Sajeda Al-Chalabi
parathyroid gland
calcium & phosphate regulation in the extra cellular fluid & plasma
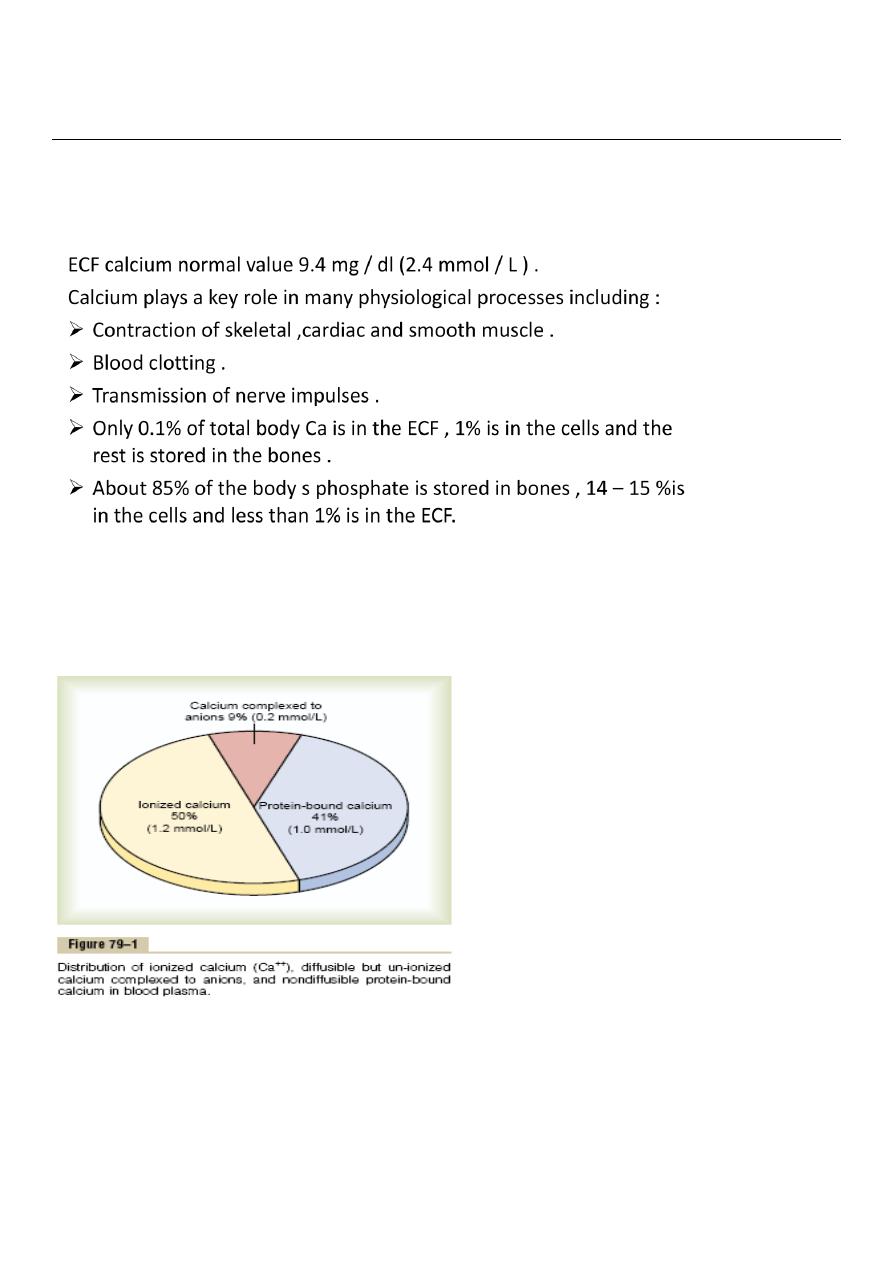
The calcium in the plasma is present in three forms :
1. About 41%( 1mmol / L) of calcium is combined with the plasma
proteins and in this form is non-diffusible through the capillary
membrane.

15
2. About 9% ( 0.2 mmol / L) is combined with an ionic substances (
citrate & phosphate ) . is diffusible through the capillary membrane
3. 50 % is ionized . is diffusible through the capillary membrane, the
plasma and interstitial fluids have a normal calcium ion concentration
of about 1.2 mmol/L (or 2.4 mEq/L) This ionic calcium is the form that is
important for
most functions of calcium in the body.
Inorganic phosphate in extra cellular fluid
Inorganic phosphate in the plasma is mainly in two forms: HPO4
and H2PO4 The concentration of HPO4 is about 1.05 mmol/L, and the
concentration of H2PO4 - is about 0.26 mmol/L.
when the pH of the extracellular fluid becomes more acidic, there is a
relative increase in H2PO4 and a decrease in HPO4-, whereas the
opposite occurs when the extracellular fluid becomes alkaline.
The average total quantity of inorganic phosphorus represented by
both phosphate ions is about 4 mg/dl, varying between normal limits
of 3 to 4 mg/dl in adults and 4 to 5 mg/dl in children.
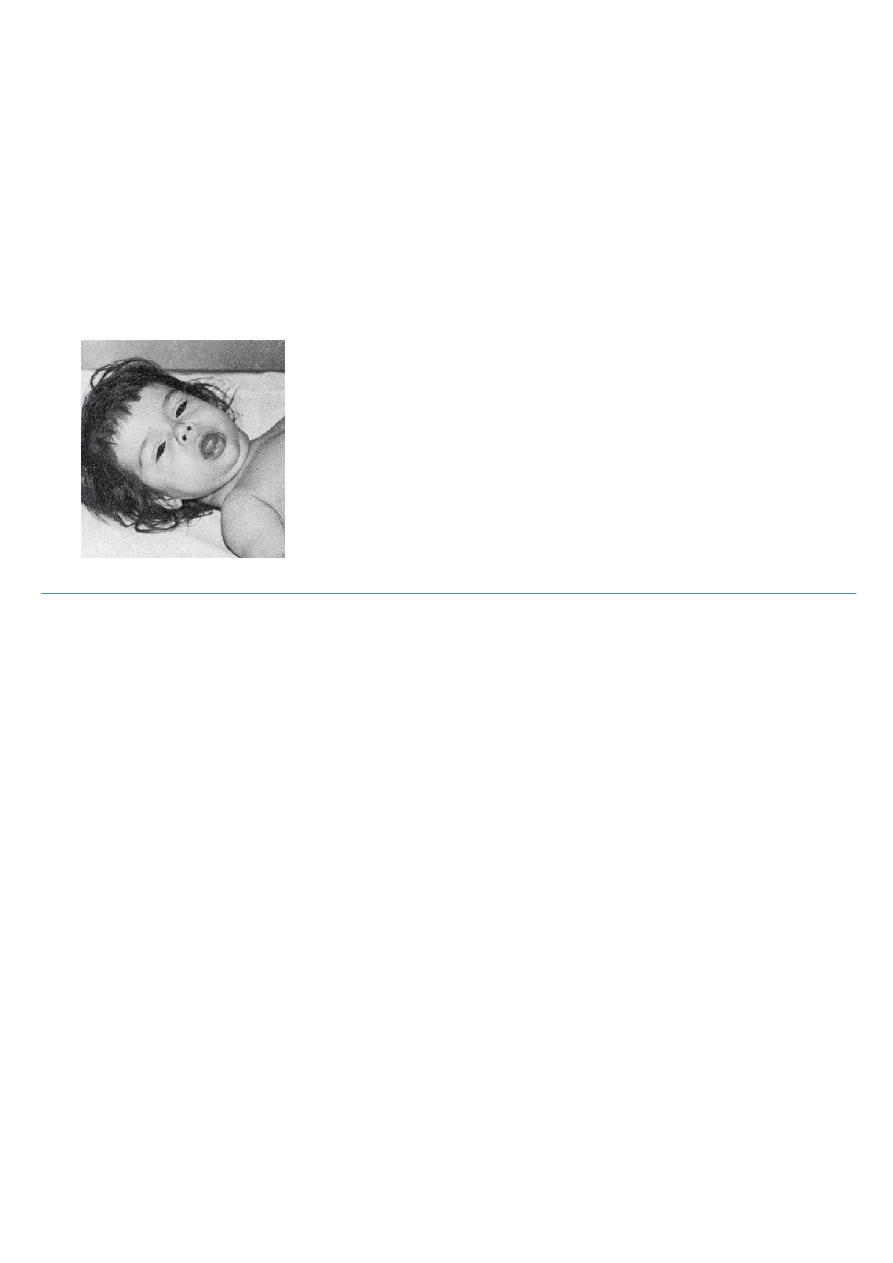
Non –bone physiologic effect of altered Ca & phosphate concentrations
in the body fluids.
Hypocalcemia causes nervous system excitement & tetany .
Hypercalcemia decreases nervous system & muscle activity .
When ECF concentration of Ca ions falls below normal the nervous
system becomes more excitable , because this causes increased

16
neural membrane permeability to Na ions allowing easy initiation
of action potential .
At plasma Ca 50% below normal , the peripheral nerve fibers become
so excitable that they discharge spontaneously initiating nerve
impulses that pass to the peripheral skeletal muscles to cause tetanic
muscle contraction .
It also causes seizures because of its action of increasing excitability of
the brain .
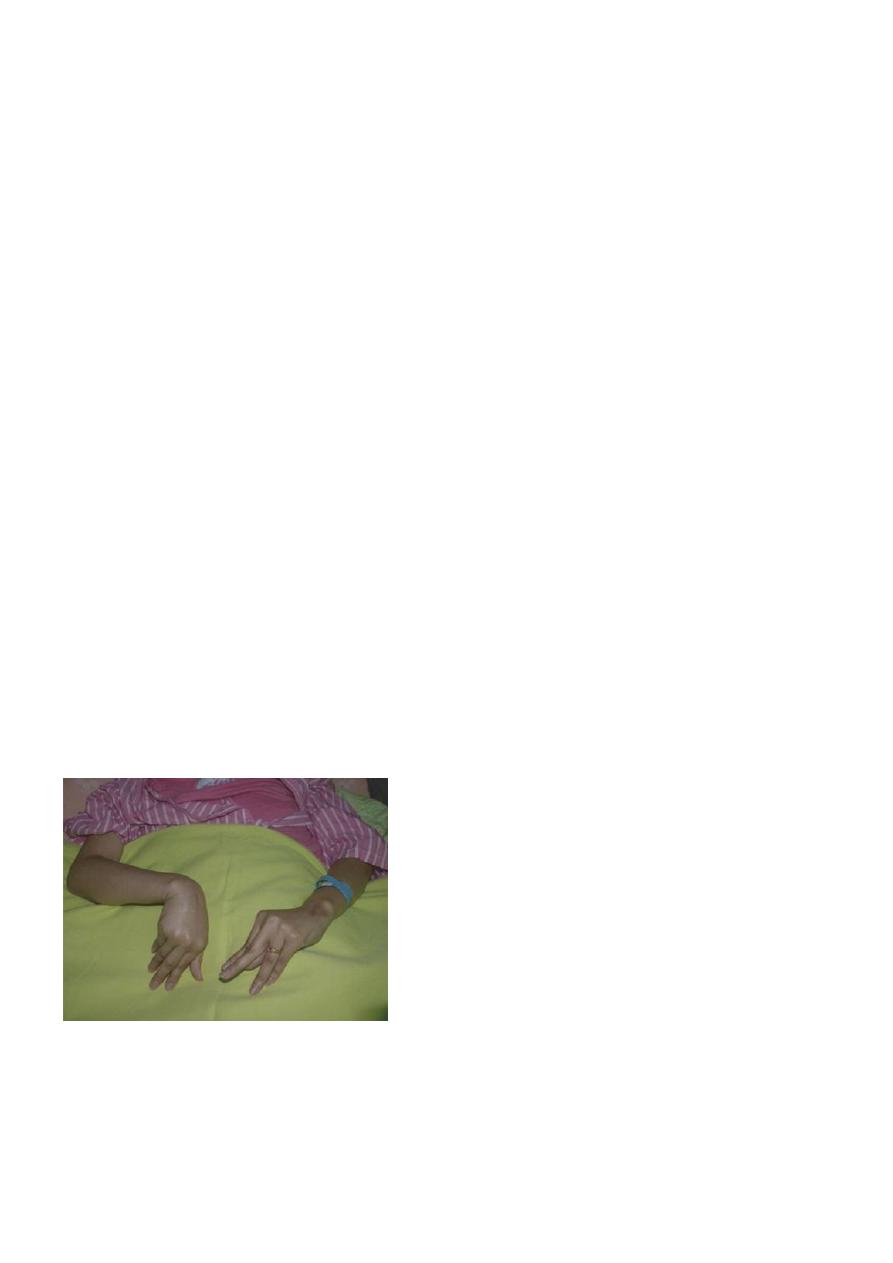
this pic. Shows carpopedal spasm .
Tetany occurs when the blood concentration of Ca falls from 9.4 mg /
dl to about 6 mg / dl , which is only 35% below normal & is usually
lethal at about 4 mg / dl .
When calcium level in the body fluids rises above normal , the
nervous system becomes depressed & reflex activities of the
nervous system are sluggish , also decrease the QT interval of the
heart , constipation and lack of appetite .
17
These effects occur when the level of calcium rises above 12 mg / dl .
when the level of calcium rises above 17mg /dl in blood , calcium ,
phosphate crystals precipitate throughout the body .
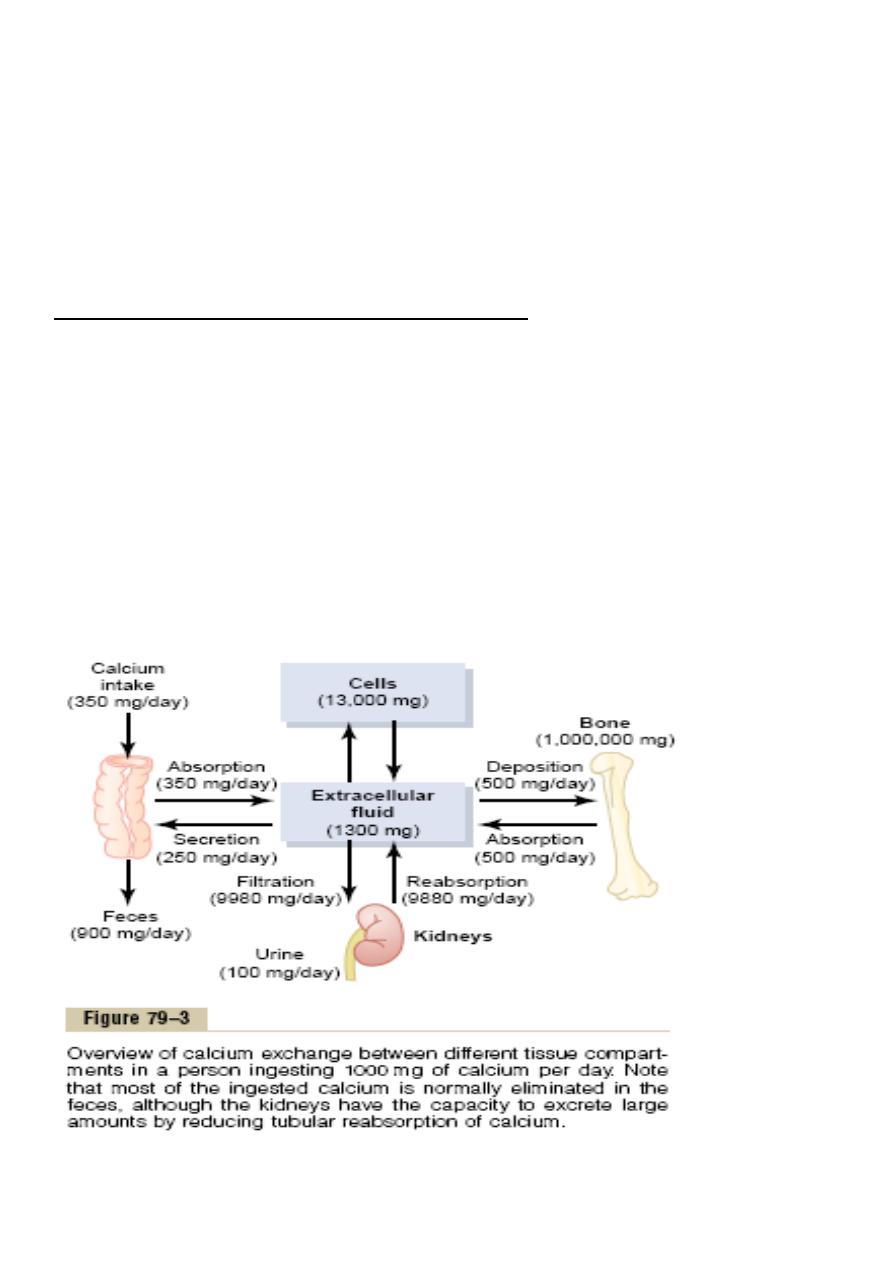
Absorption & excretion of calcium and phosphate
Intestinal absorption & fecal excretion .
the usual rates of intake are about 1000 mg / day for calcium &
phosphate , Ca ions are poorly absorbed from the intestine , vitamin D
promotes its absorption by the intestine. about 35%( 350 mg / day ) of
ingested calcium is usually absorbed , the remaining is excreted in the
feces .
an additional 250 mg of calcium enters the intestine via secreted
G.I.T. juices thus90% ( 900 mg / day ) of daily intake of calcium is
excreted in feces .

18
Intestinal absorption of phosphate occurs very easily. Except
for the portion of phosphate that is excreted in the feces in
combination with nonabsorbed calcium, almost all the dietary
phosphate is absorbed into the blood from the gut and later
excreted in the urine.
Renal excretion of calcium & phosphate
About 10% ( 100 mg / day ) of ingested calcium is excreted in urine .
About 41%of plasma calcium is bound to plasma proteins and
therefore not filtered by the glomerular capillaries . The rest is
combined with anions such as phosphate ( 9% ) or ionized 50% and is
filtered through the glomeruli into the renal tubules .
Normally renal tubules absorb 99% of the filtered calcium & about
100mg / day is excreted in urine . About 90%of calcium in the
glomerular filtrate is reabsorbed in the proximal tubules , loop of Henle
and early distal tubules , then in the late distal tubular and early
collecting ducts ,reabsorption of remaining 10% is very selective ,
depending on calcium ion concentration in blood .
When concentration is low , this reabsorption is great , so that almost ,
no calcium is lost in urine . Conversely , even a minute increase in
blood calcium ion concentration above normal increases excretion
markedly.
Renal phosphate excretion is controlled by an overflow mechanism
that is when phosphate concentration in the plasma is below the
critical value of about 1 mmol / L, all the phosphate in the glomerular
filtrate is reabsorbed & no phosphate is lost in the urine .
But above this critical concentration , the rate of phosphate loss is
directly proportional to the additional increase .
19
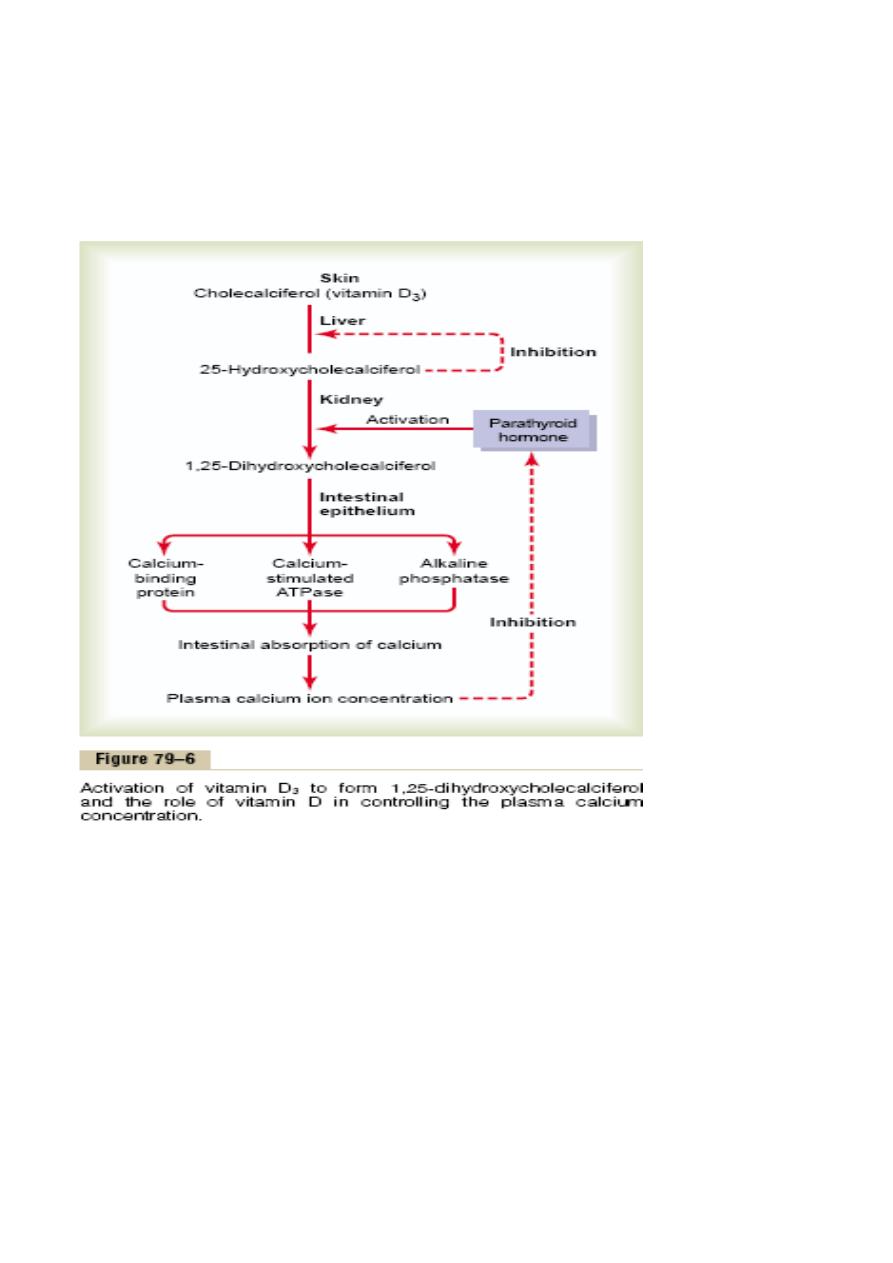
Vitamin D
Vitamin D3 ( cholecalciferol ) is found in the skin .
This is activated &converted to 25-hydroxycholecalciferol in the liver &
this has a negative feedback effect on the conversion reactions .
25-hydroxycholecalciferol in the proximal tubules of the kidneys is
converted to 1, 25-dihydroxycholecalciferol .this is the most active
form of vitamin D .this conversion requires PTH .
20
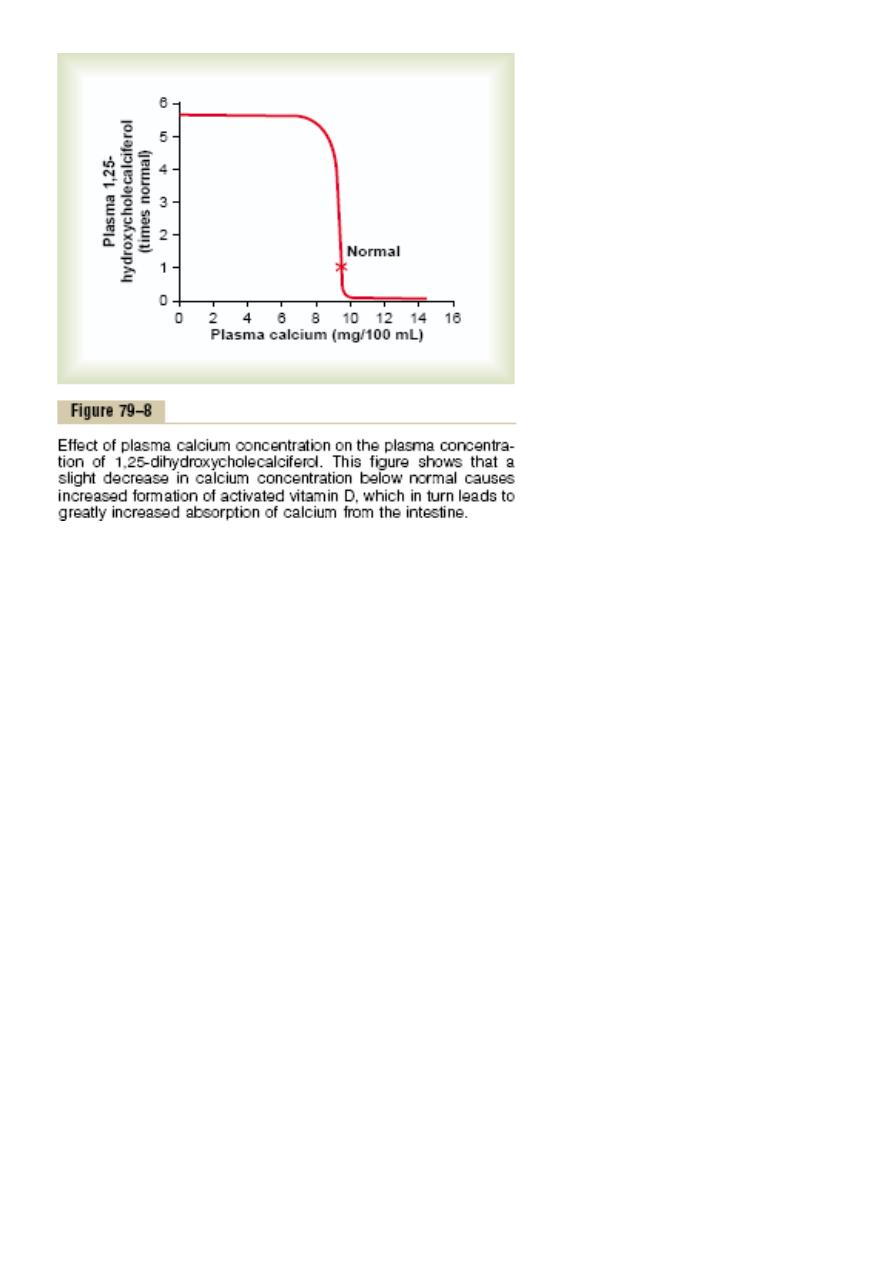
This demonstrates that plasma concentration of 1, 25-
dihydroxycholecalciferol is inversely affected by the concentration of
calcium in the plasma.
There are 2 reasons for this :
First : the calcium ion itself has a slight effect in preventing the
conversion of 25-hydroxycholecalciferol to 1, 25-
dihydroxycholecalciferol .
Second : the rate of secretion of PTH is greatly decreased when
plasma calcium ion concentration rises above 9 – 10 mg / 100ML ,
therefore , at calcium concentration below this level ,PTH
promotes the conversion of 25-hydroxycholecalciferol to 1, 25-
dihydroxycholecalciferol in the kidneys .
At higher plasma calcium concentration when PTH is decreased , the
25-hydroxycholecalciferol is converted to 24, 25-
dihydroxycholecalciferol that has no vitamin D effect .

21
Actions of vitamin D
1. It promotes intestinal calcium absorption .
2. It promotes phosphate absorption by the intestines .
3. It decreases renal calcium and phosphate excretion .
4. It plays an important role in both bone absorption & bone
deposition .
Parathyroid hormone
Normally there are 4 parathyroid glands in humans , they are located
immediately behind the thyroid gland and behind each of the upper
&each of the lower poles of the thyroid.
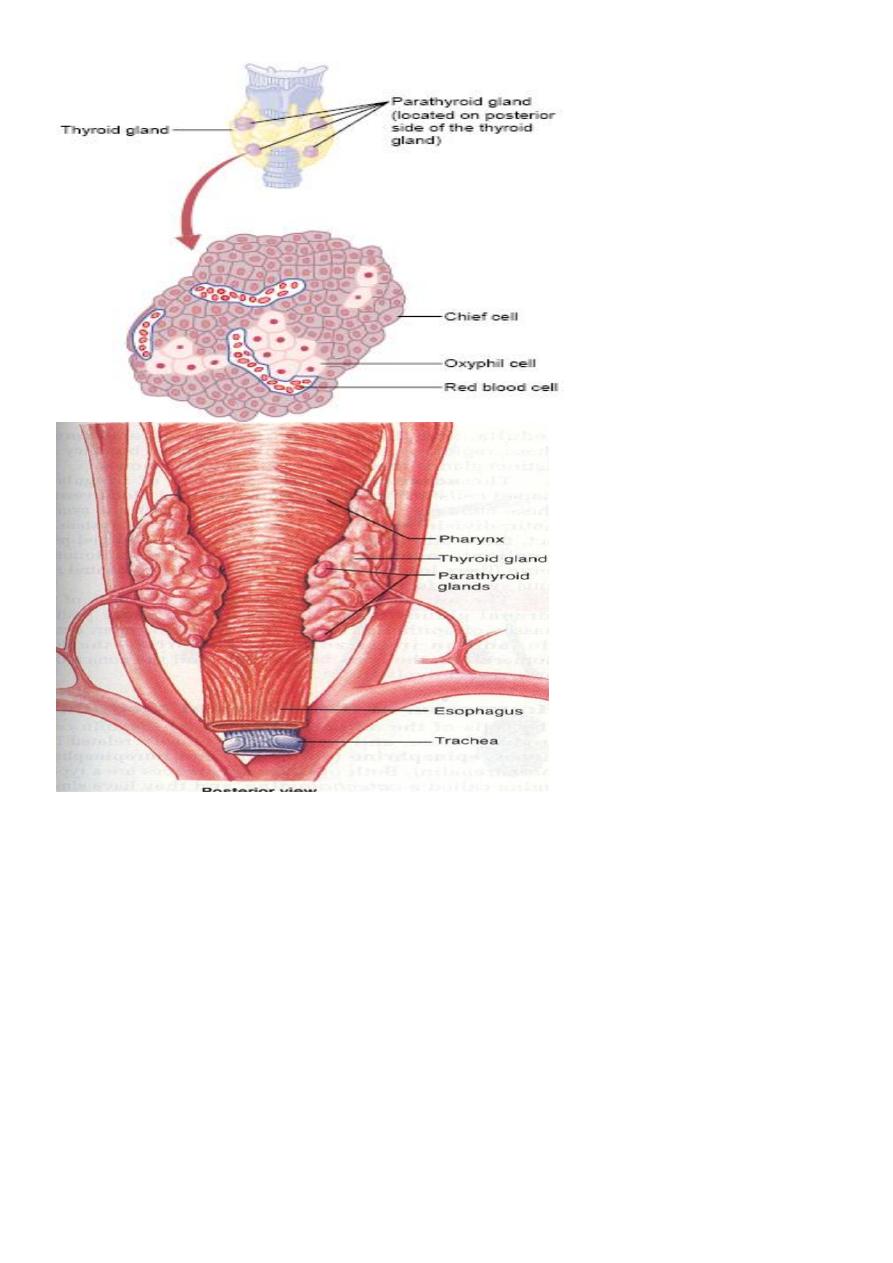
22
The parathyroid gland contains mainly chief cells which secret PTH
.PTH is a polypeptide with 84 amino acids .
Effect of PTH on calcium & phosphate concentration in
ECF
1. PTH increases calcium &phosphate absorption from the bone .
2. It decrease the excretion of the calcium by the kidney .
3. It increases renal phosphate excretion .
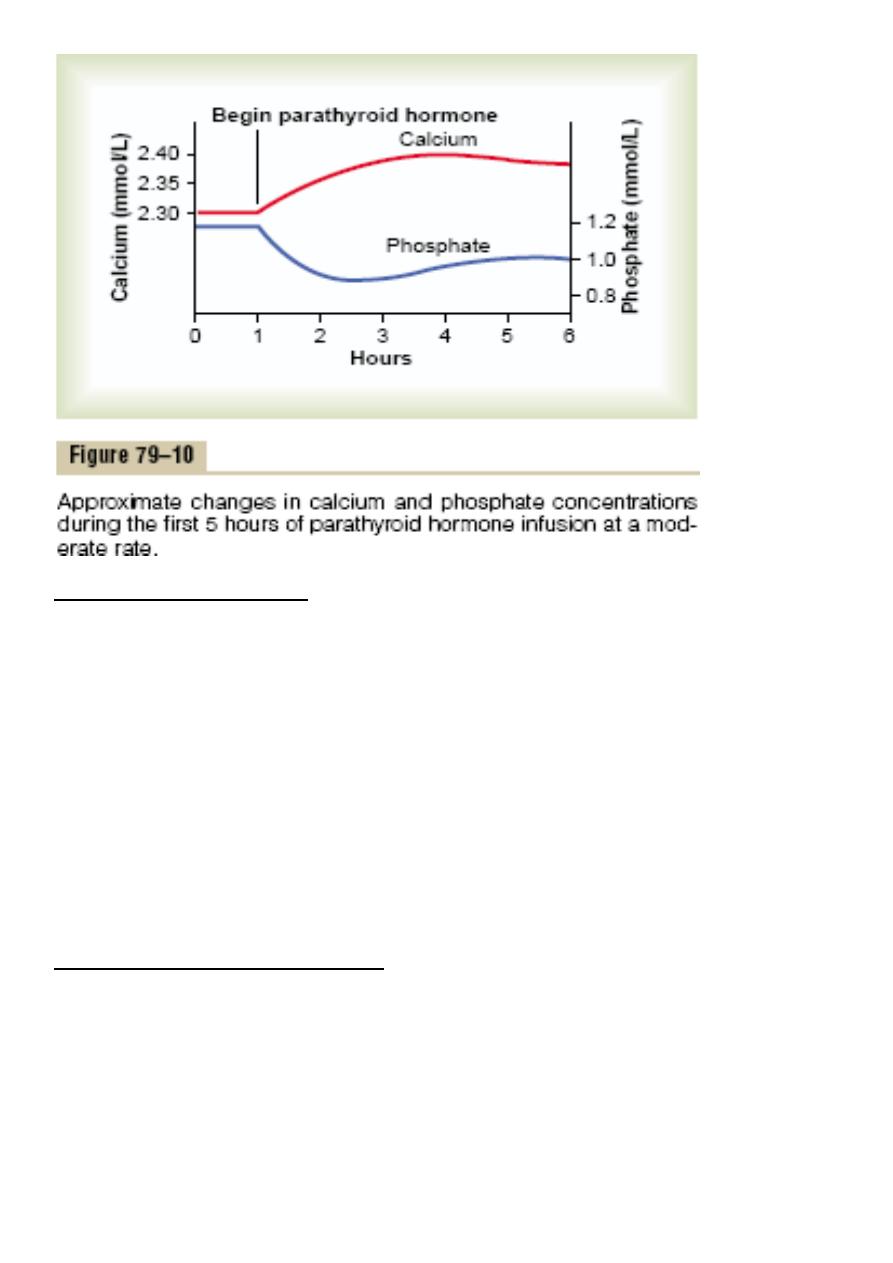
23
Effect of PTH on bone .
PTH has 2 effects on bone in causing absorption of calcium &
phosphate ;
One Is rapid phase that begins in minutes & increasing progressively for
several hours , this phase results from activation of the already existing
bone cells to promote calcium and phosphate absorption .
The second phase is a much slower one requiring several days or even
weeks , it result from proliferation of the osteoclasts followed by
increased osteoclastic reabsorption .
Effect of PTH on renal tubules .
PTH increases renal tubular reabsorption of calcium , at the same
time it decreases phosphate reabsorption .

24
The increase of calcium absorption occurs mainly in the late distal
tubules , the collecting tubules & the ascending loop of Henle to a
lesser extent.
Effect of PTH on intestine .
PTH increases intestinal absorption of calcium & phosphate by
increasing the formation of 1, 25-dihydroxycholecalciferol in the
kidneys for vitamin D .
Control of PTH secretion by calcium ion concentration
Even the slightest decrease in calcium ion concentration in ECF causes
the parathyroid glands to increase their rate of secretion within
minutes , if the decreased calcium continue , the glands will
hypertrophy , sometimes five folds .
The parathyroid glands enlarge in rickets , in pregnancy and in lactation
.
Conversely conditions that increase Ca ion concentration above
normal cause decreased activity & reduced size of parathyroid gland
such condititions include :
1. Excess calcium in the diet .
2. Increased vit.D in the diet .
3. Bone absorption caused by disuse of bones .
calcitonin
It is a peptide hormone secreted by the thyroid gland , it decreases plasma
calcium concentration &has effects opposite to those of PTH .
synthesis & secretion of calcitonin occur in the Para follicular cells or C cells ,
lying in the interstitial fluid between the follicles of the thyroid gland .
25
The primary stimulus for calcitonin secretion is increased calcium ion
concentration in plasma .
The reduction of Ca ions concentration caused by calcitonin leads within
hours to a powerful stimulation of PTH secretion which over rides the calcitonin
effect .
Disease of Parathyroid
• Hyperparathyroidism
– Over-activity of parathyroid resulting in increased calcium in the
blood
– Leads of kidney stones, GI disturbances
– Bones become weak, deformed and fracture easily because calcium
is drawn from the bone
• Hypoparathyroidism
– Under-activity of parathyroid gland causing a low level of calcium in
blood
– Tetany, hyperirritability of nervous system, twitching
– Death can occur if the larynx and respiratory muscles are involved.
26
PHYSIOLOGY
lec. 8-9 Dr. Sajeda Al-Chalabi
Adrenal Gland
The two adrenal glands , each of which weighs 4 gm , lie at the superior
poles of the kidneys
The Adrenal Gland
27
Each gland is composed of 2 parts , the adrenal medulla and adrenal
cortex. The adrenal medulla ,central 20% of the gland , is functionally
related to the sympathetic nervous system , it secrets the hormones
epinephrine & norepinephrine in response to sympathetic stimulation
.
In turn these hormones cause almost the same effect as direct
stimulation of the sympathetic nerves in all parts of the body .
The adrenal cortex secretes corticoids . These hormones synthesized
from the steroid cholesterol ,and they all have the similar chemical
formulas .
The corticoids , mineralocorticoids ,glucocorticoids
and androgens
Two major types of adrenocortical hormones , the mineralocorticoids
& the glucocorticoids, are secreted by the adrenal cortex . In addition
small amount of hormones are secreted , especially androgenic
hormones which have the same effect of testosterone ( male sex
hormone ) .
Mineralocorticoids affect the electrolytes ( minerals ) of the ECF ,
sodium & potassium .
Glucocorticoids they increase blood glucose concentration .
The steroids include aldosterone & cortisols which are the principal
glucocorticoids .
Synthesis and secretion of the adrenocortical hormones
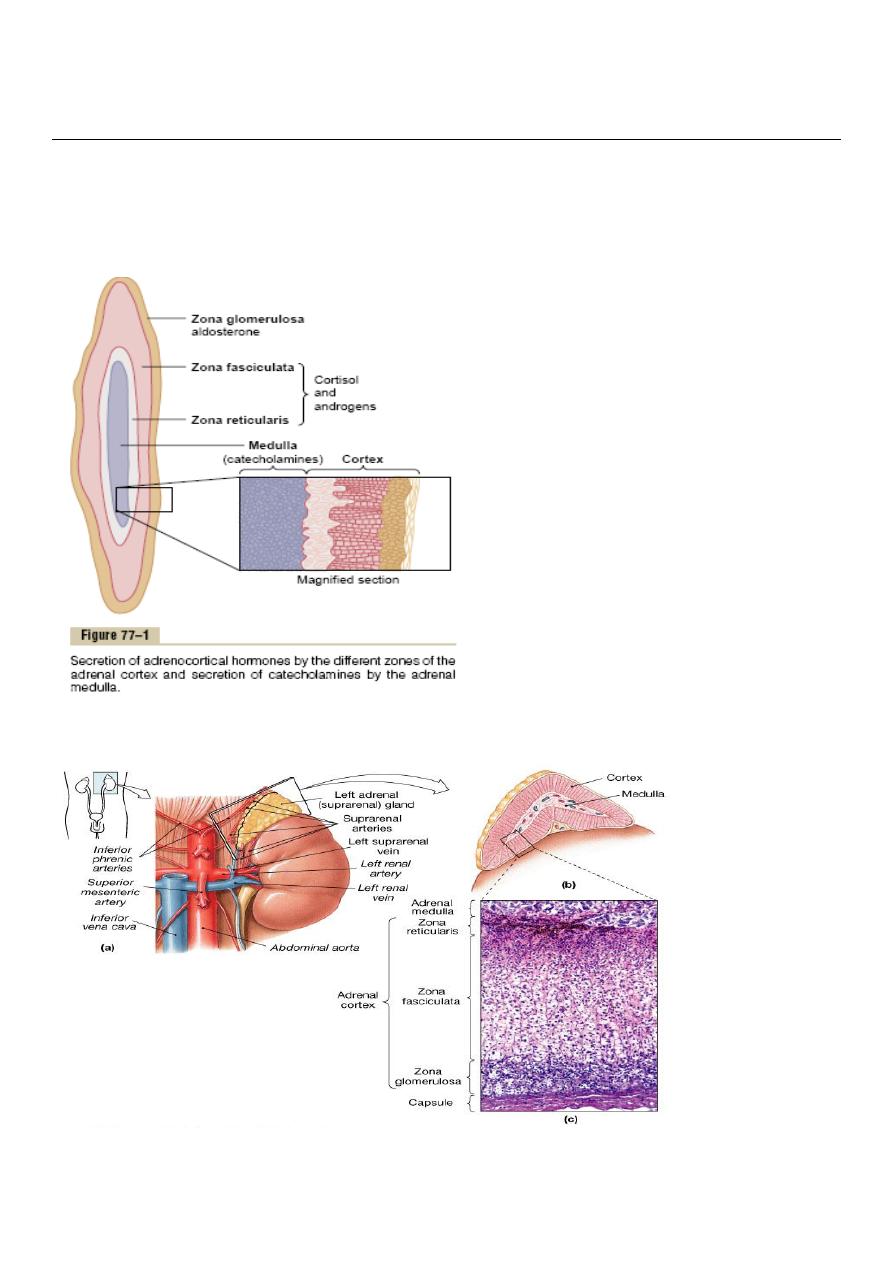
The adrenal cortex has 3 distinct layers .
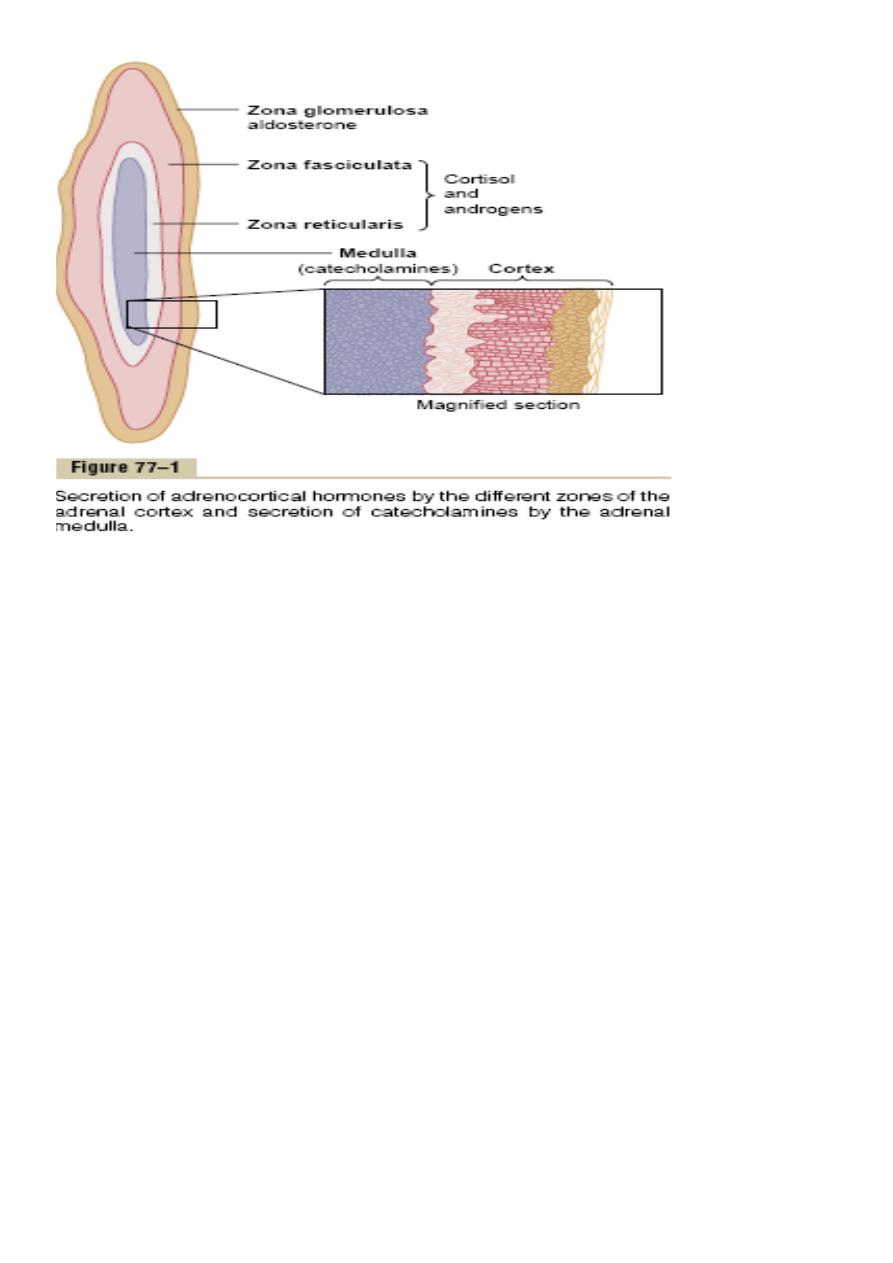
28
1. Zonal glomerulosa:
a thin layer of cells that lies just underneath the capsule , constitutes
about 15% of the adrenal cortex . These cells secrete aldosterone
because they contain the enzyme aldosterone synthase . The secretion
of these cells is controlled by the ECF concentration of angiotensin II &
potassium , both of which stimulates aldosterone secretion .
2. Zona fasiculata :
the middle and widest layer , constitutes about 75% of the adrenal
cortex and secretes the glucocorticoids , cortisole and corticosterone
as well as small amounts of androgens and estrogens . The secretion of
these cells is controlled by the hypothalamic – pituitary axis via ACTH .
3. Zona reticularis :
the deep layer of the cortex , secretes the adrenal androgens
dehydroepiandrosterone (DHEA) and androstenedione , as well as

29
small amounts of estrogens and some glucocorticoids. ACTH also
regulates secretion of these cells .
Mineralocorticoids include :
• Aldosterone (very potent account for 90 % of all
mineralocorticoids activity).
• Deoxycorticosterone (1 / 30 as a potent as aldosterone , but very
small quantities secreted).
• Corticosterone ( slight mineralocorticoid activity )
• 9
- Fluocorisol ( Synthetic, slightly more potent than aldosterone
) .
• Cortisol ( very slight mineralocorticoid activity, but large quantity
secreted ).
• Cortisone ( Synthetic, slight mineralocorticoid activity ) .
Glucocorticoids :
• Cortisol ( very potent, account for about 95% of all glucocorticoids
activity ).
• Corticosterone ( provides about 4% of total glucocorticoids
activity, but much less potent than cortisol ).
• Cortisone ( synthetic, almost as potent as cortisol ).
• Prednisone (synthetic, four times as potent as cortisol).
• Methyl prednisone ( synthetic, five times as potent as cortisol)
• Dexamethasone ( synthetic, 30 times as potent as cortisol ).

30
Approximately 90-95% of cortisol in the plasma binds to plasma
proteins , especially globulin called cortisol-binding globulin or
transcortin & to a lesser extent to albumin .
Cortisol has half life of 60-90 minutes .
Only about 60% of the circulating aldosterone combinds with the
plasma proteins, so about 40% in the free form . Aldosterone has short
half life of about 20 minutes .
Aldosterone’s mineralocorticoid activity is about 3000 times greater
than that
of cortisol, but the plasma concentration of cortisol is nearly 2000
times that of aldosteroneThe concentration of aldosterone in blood is
about 6nanograms/100 ml .
The concentration of cortisol in the blood averages 12 mg /100 ml.
Functions of the mineralocorticoids – aldosterone
Renal & circulatory effects of aldosterone :
1-Aldosterone increases absorption of sodium and secretion of
potassium by the renal tubular epithelial cells especially in the
principal cells of the collecting tubule and to a lesser extent in the
distal tubules and the collecting ducts. Therefore, aldosterone
causes sodium to be conserved in the ECF while increasing
potassium excretion in the urine .
2-Excess aldosterone increases ECF volume and arterial pressure but
has only small effect on the plasma sodium concentration, although,
has a potent effect in decreasing the rate of sodium excretion by the
kidneys, the concentration of sodium in the extra cellular fluids often
rises only a few milliequievelants.
The reason for this is that when sodium is reabsorbed , there is
simultaneous osmotic absorption of almost equivalent amount of

31
water also small increase in ECF sodium concentration stimulate
thirst and increased water intake .
Therefore the ECF volume , increases almost as much as the retained
sodium , but without much change in sodium concentration .
An aldosterone – mediated increase in ECF volume last for 1-2 days
also leads to an increase in arterial pressure , this increases kidney
excretion of both salt and water called pressure natriuresis and
pressure diuresis . This return to normal of salt and water excretion
by the kidneys as a result of pressure diuresis and natriuresis is
called aldosterone escape .
Conversely , when aldosterone secretion becomes zero , large
amounts of salt are lost in the urine , decreasing the ECF volume ,
the result is circulatory shock .
3. Excess aldosterone causes hypokalemia and muscle weakness .
Too little aldosterone causes hyperkalemia and cardiac toxicity .
Excess secretion of aldosterone causes serious decrease in plasma
potassium concentration , sometimes from the normal value of 4.5
mg / L to as low as 2 mg / L this condition is called hypokalemia .
When potassium ion concentration falls below about ½ normal
severe muscle weakness often develops .
Conversely , when aldosterone is deficient , the ECF potassium ion
concentration can rise above normal , when it rises 60 – 100 %
above normal cardiac toxicity occur , causes weakness of heart
contraction and development of arrhythmia .
4. Excess aldosterone increases tubular hydrogen ion secretion , with
resultant mild alkalosis .
Aldosterone causes secretion of hydrogen ions in exchange for sodium
in the intercalated cells of the cortical collecting tubules , this decrease
32
the hydrogen ion concentration in the ECF . This effect usually causes a
mild degree of alkalosis .
Aldosterone stimulates sodium and potassium transport in sweat
glands , salivary glands & intestinal epithelial cells
Aldosterone has almost the same effects on sweat glands and salivary
glands as it has on the renal tubules . Both these glands form a primary
secretion that contains large quantities of sodium chloride , but much
of this is reabsorbed by excretory ducts ,whereas potassium and
bicarbonate ions are secreted .
The effect on the sweat glands is important to conserve body salt in
hot environment and the effect on salivary glands is necessary to
conserve salt when excessive quantities of saliva are lost .
Aldosterone also greatly enhances sodium absorption by the intestines
especially in the colon which prevents lose of sodium in the stools . The
absence of aldosterone leads to diarrhea , with loss of salt from the
body .

33
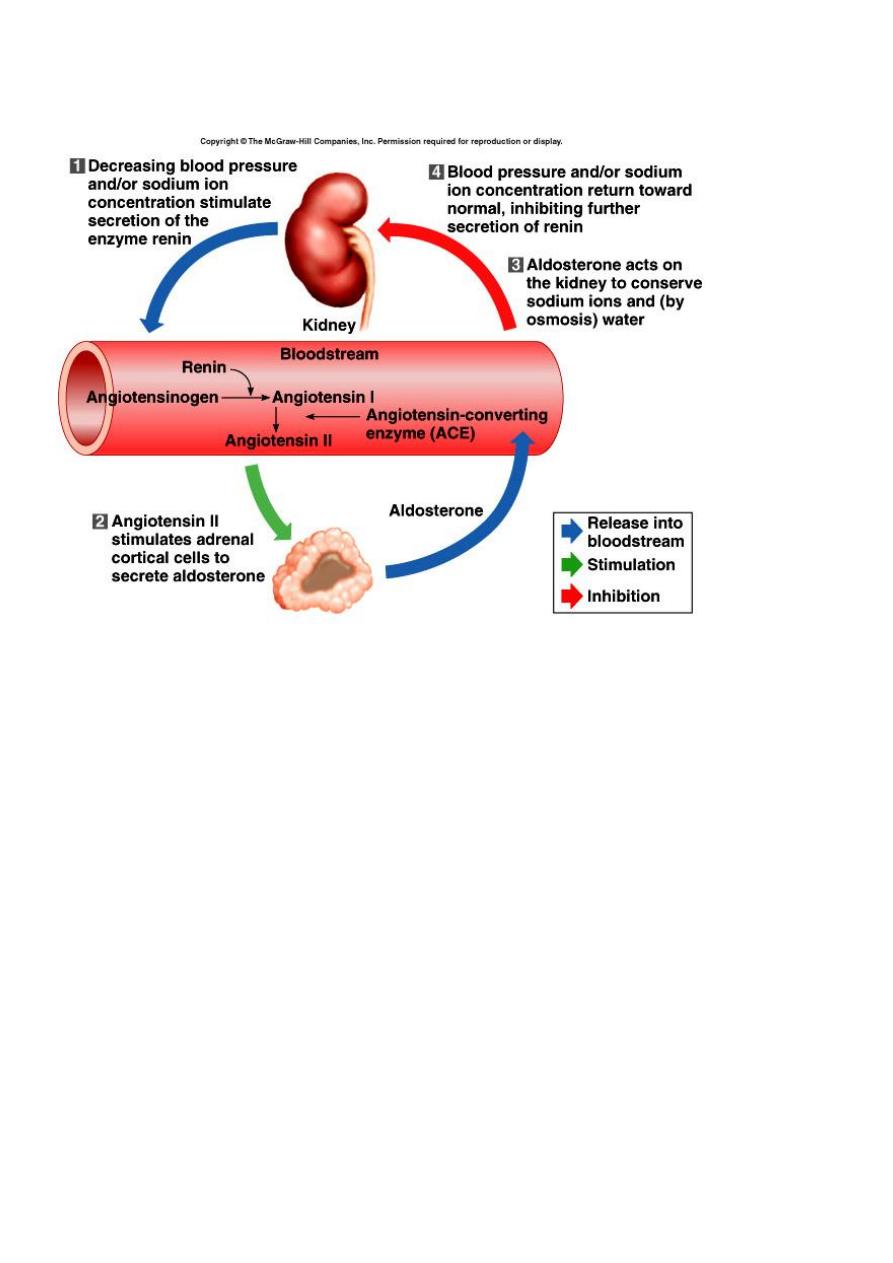
Regulation of aldosterone secretion
Four factors play essential roles in the regulation ;
1. Increased potassium ion concentration in the ECF greatly
increases aldosterone secretion .
2. Increase activity of the rennin – angiotensin system greatly
increases aldosterone secretion .
3. Increased sodium ion concentration in the ECF may slightly
decrease aldosterone secretion .
4. ACTH from the anterior pituitary gland is necessary for
aldosterone secretion , but has little effect in controlling the rate
of secretion .
Of these factors , K + concentration & the rennin – angiotensin system
are the most potent in regulating aldosterone secretion .
Activation of rennin – angiotensin system cause several fold increase in
aldosterone secretion .
In turn , the aldosterone acts on the kidneys ;
1. To help the excrete the excess potassium ions .
2. To increase blood volume & arterial pressure thus returning
rennin – angiotensin system toward normal , these feedback
control mechanisms are essential for maintaining life .
Functions of the Glucocorticoids
95% of the glucocorticoid activity of the adrenocortical secretion
results from the secretion of cortisol , known also as hydrocortisone , in
addition small but significant amount of glucocorticoid activity is
provided by corticosterone .

34
Effect of cortisol on carbohydrate metabolism
1. Stimulation of gluconeogenesis .
that is formation of carbohydrate from proteins & other substances
by the liver this result mainly from two effects of cortisol :
a. Cortisol increases the enzymes required to convert amino acids into
glucose in the liver cells .
b. cortisol causes mobilization of amino acids from the extra hepatic
tissues mainly from muscle .
2. Decreased glucose utilization by the cells .
3. Elevated blood glucose concentration & adrenal diabetes .
Effect of cortisol on fat metabolism
Mobilization of fatty acids , this helps shift the metabolic system of the
cells in times of starvation or other stresses from utilization of glucose
for energy to utilization of fatty acids .
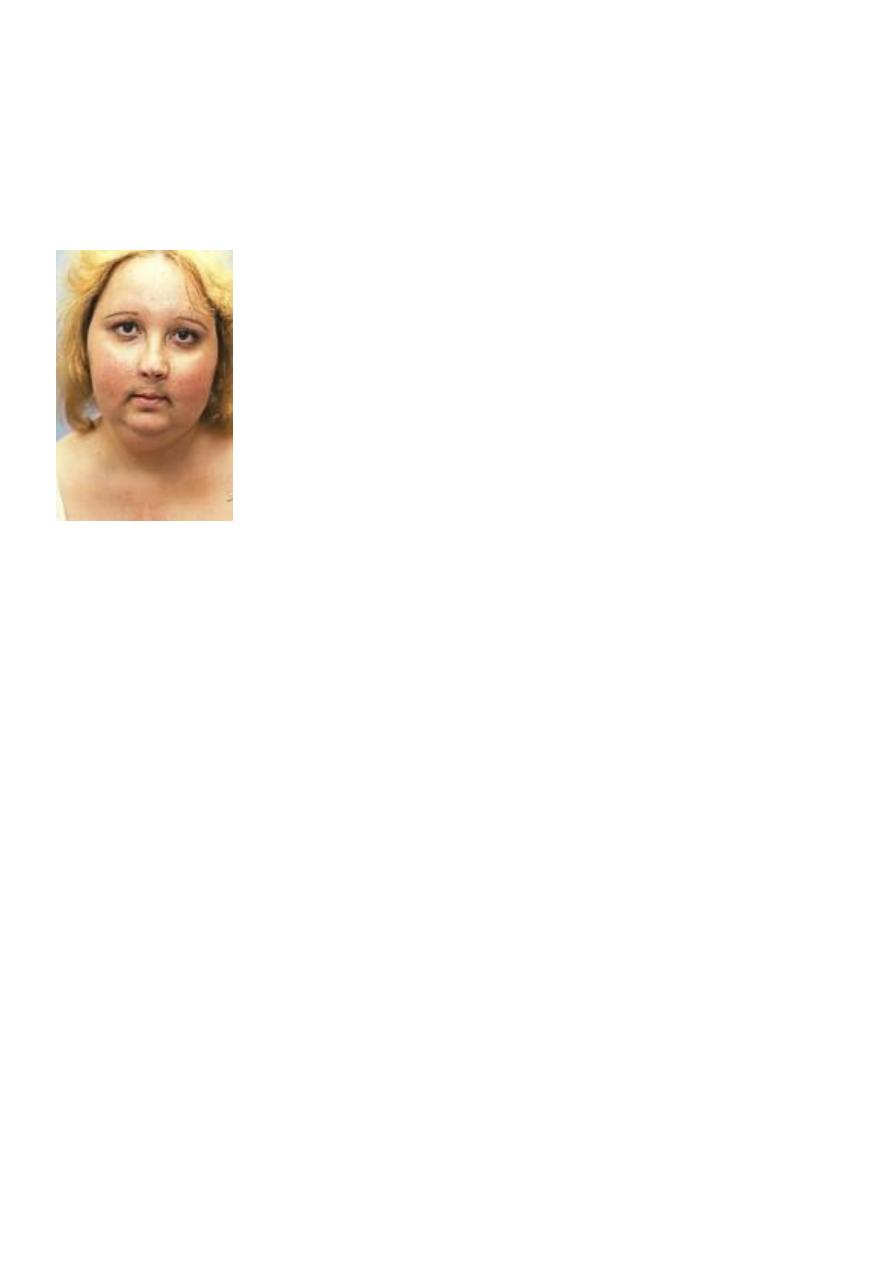
Many people with excess cortisol secretion develop type of obesity ,
with excess deposition of fat in the chest & head regions of the body
giving a buffalo like tor so and a rounded “ moon face “ this obesity
result from excess food intake .
Cortisol is important in resisting stress & inflammation
Almost any type of stress causes an immediate & marked increase in
ACTH secretion by the anterior pituitary followed by increased
adrenocortical secretion of cortisol .
Some different types of stress that increase cortisol release are the
following ;
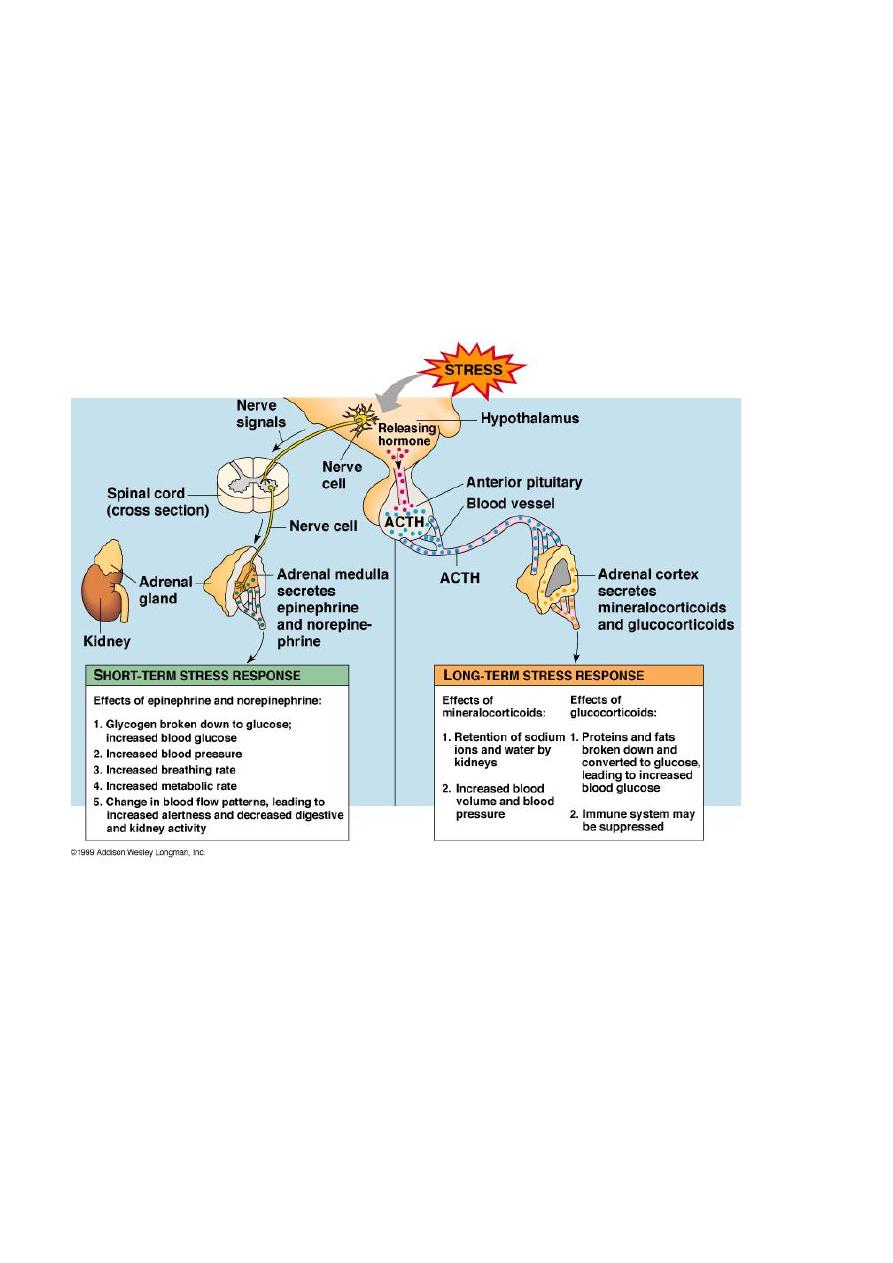
35
Trauma , infection , intense heat or cold , injection of norepinephrine
,surgery , injection of necrotizing substances beneath the skin , any
debilitating disease .
Glucocorticoids cause rapid mobilization of amino acids & fats from
their cellular stores making them immediately available both for
energy & for synthesis of other compounds including glucose needed
by different tissues of the body .
Anti-inflammatory effect of high levels of cortisol
When tissues are damaged by trauma ,by infection with bacteria , they
almost become inflamed , the administration of cortisol can usually
block this inflammation by ;
1. It can block the early stages of inflammation process .
36
2. If inflammation has already begun , it causes rapid resolution of the
inflammation & increased rapidity of healing .
Cortisol prevents shock or death in anaphylaxis .
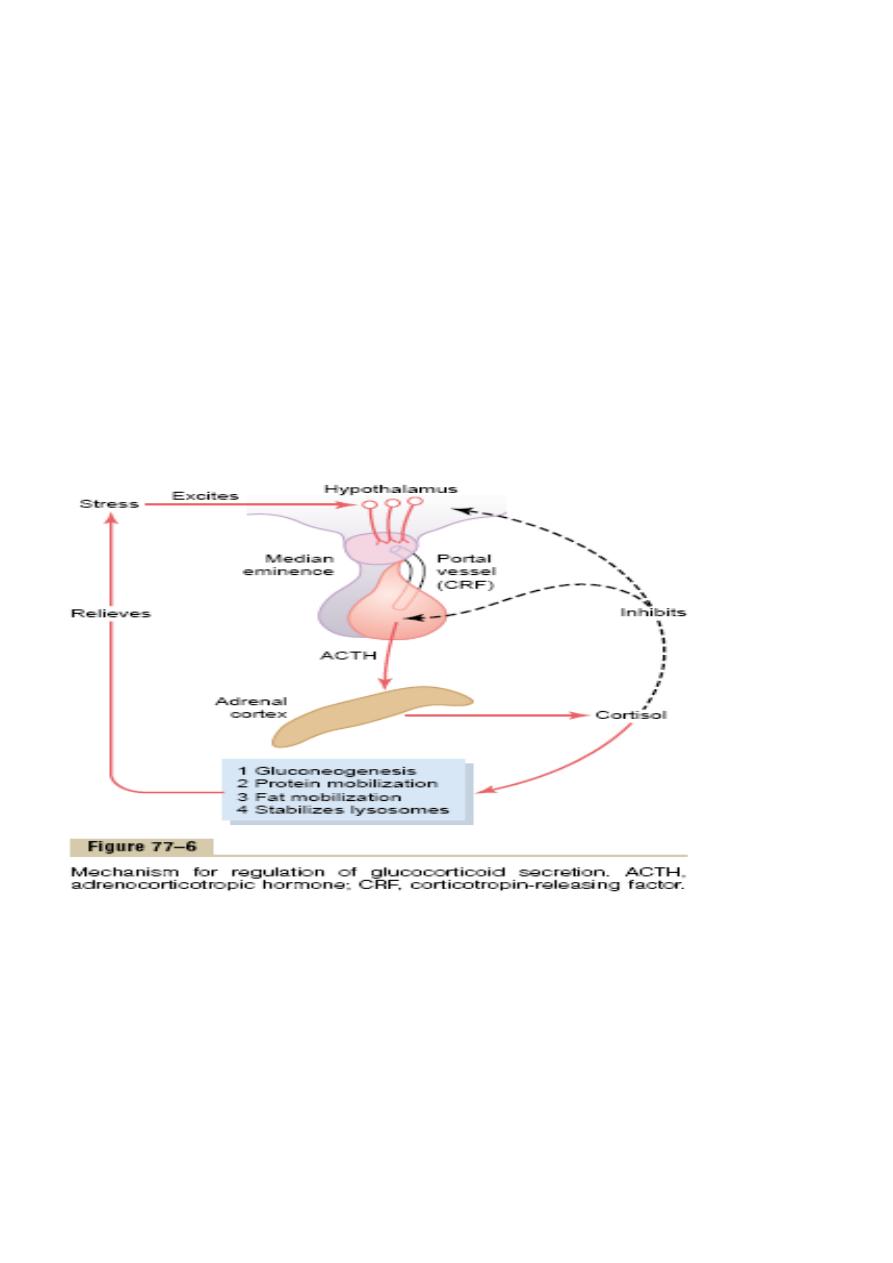
Regulation of cortisol secretion by ACTH from the
anterior pituitary
ACTH is a large polypeptide , has 39 amino acids .it is controlled by
Corticotropin –releasing factor ( CRF) from the hypothalamus .
ACTH act on adrenocortical cells to produce steroids ,
Stress stimuli activate the entire control system to cause rapid release
of cortisol & the cortisol in turn initiates a series of metabolic effects
.there is direct feedback of the cortisol to both the hypothalamus & the
anterior pituitary to decrease the concentration of cortisol in plasma .
37
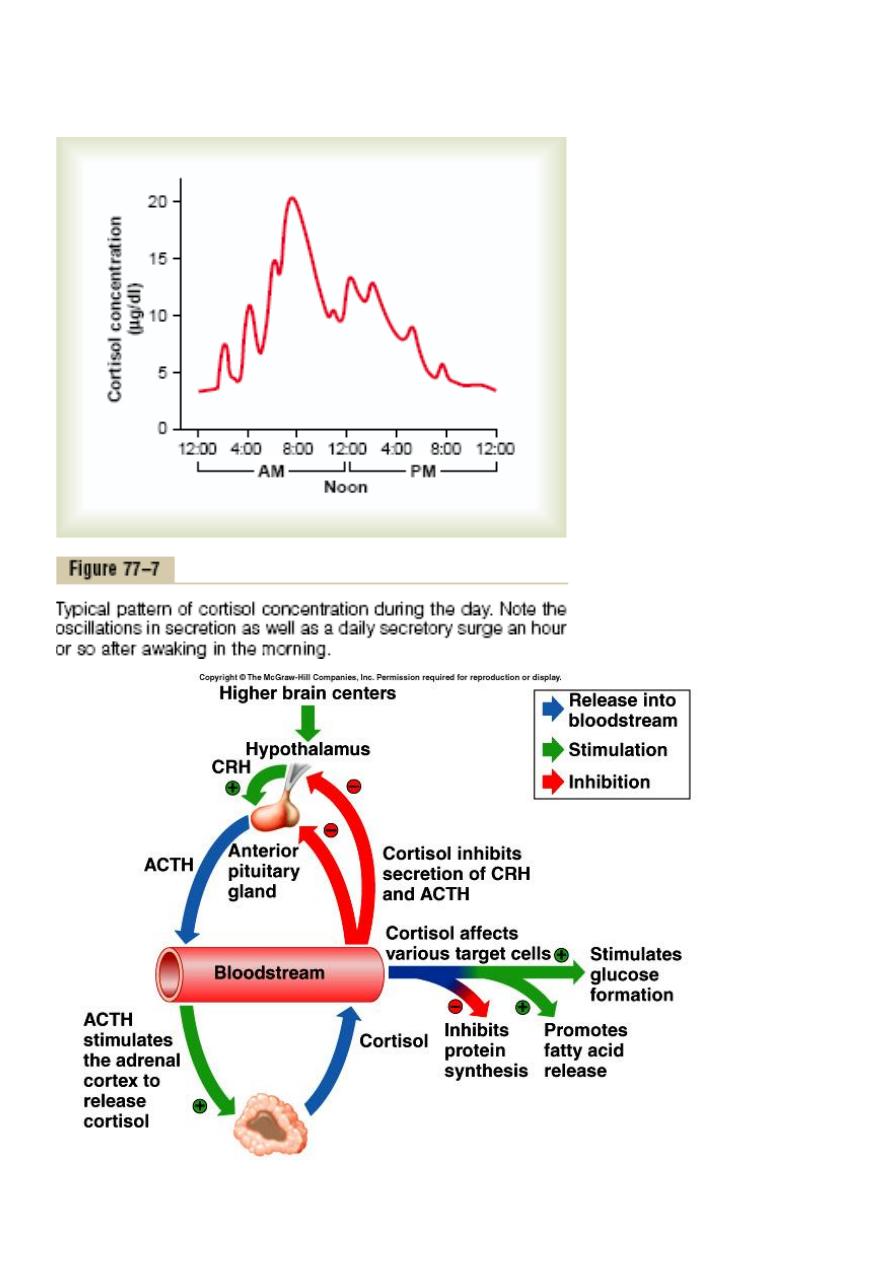
The secretory rate of CRF, ACTH & cortisol are high in early morning
but low in the late evening .

38
Adrenal Androgens
The most important male sex hormone is dehydroepiandrosterone
secreted by the adrenal cortex , also female sex hormones are secreted
in small quantities as estrogen & progesterone some of the adrenal
androgens are converted to testosterone in the extra-adrenal tissues.
Abnormalities of adrenocortical secretion
1. Hypoadrenalism __ Addison s disease is failure of adrenal cortex to
produce adrenocortical hormones .
2. Hyperadrenalism __ cushing s syndrome .
3. Primary aldosteronism __ conn s syndrome , tumor of zona
granulosa.
Disease of Adrenal glands
• Addison’s disease
– Decreased function of adrenal cortex
– Excessive pigmentation, low blood pressure when standing,
muscular weakness/fatigue, diarrhea, wt. loss, vomiting
– Tx. Replace
– hormone
39
• Cushing’s syndrome
– Hypersecretion of glucocorticoids
– Causes hyperglycemia, hypertension, poor wound healing,
bruising, “moon” face and obesity
40
