خامس اسنان/ لثة
د. رؤى م(1)24/ 11/ 2016
خامس اسنان/ لثة
د. رؤى م(1)
24/ 11/ 2016
Clinical periodontology
Clinical diagnosis
Proper diagnosis is essential. Periodontal diagnosis should first determine whether disease is present; then identify its type, extent, distribution, severity; and finally provide an understanding of the underlying pathological processes and its cause.The following recommended sequence of procedures for the diagnosis of periodontal disease:
History
Medical history
Dental history
Examination of lymph nodes
Oral examination
Mouth odors it is caused by volatile sulfur compounds which could be involved in the transition from health to gingivitis and then periodontitis.
Oral hygiene.
Wasting disease of the teeth wasting is defined as any gradual loss of tooth substance characterized by formation of smooth, polished surfaces, without regard to the possible mechanism of this loss. The forms of wasting are erosion, abrasion, and attrition.
Hypersensitivity
Tooth mobility
Increased mobility is caused by one or more of the following factors:
Loss of tooth support
Trauma from occlusion
Extention of inflammation from the gingiva or from the periapex into the periodontal ligaments
Periodontal surgery
Pregnancy, menstrual cycle or use of hormonal contraceptive because of physiochemical changes in the periodontal tissues
Pathological process of the jaws that destroy the alveolar bone and/or the roots of the teeth (osteomyelitis and tumors)
Trauma from occlusion it is a tissue injury produced by occlusal forces. The periodontal findings are then used as a guide for locating the responsible occlusal relationship.
Periodontal findings that suggest the presence of trauma:
Excessive tooth mobility
Widened periodontal space and loss of lamina dura.
Vertical or angular bone destruction.
Infrabony pocket.
Pathological migration
Root resorption.
Proximal contact relations
Sensitivity to percussion it is feature of acute inflammation of the periodontal ligament
Dentition with the jaws closed can detect condition like irregularly aligned teeth, extruded teeth, improper proximal contacts, and areas of food impaction, all of which may favor plaque accumulation.
Examination of the periodontium: a chart to record the periodontal findings provide a guide for examination and evaluating the response to treatment.
Plaque and calculus
Gingiva , gingival index and sulcus bleeding index.
the bleeding on probing occure if the gingiva inflamed and the pocket epithelium is atrophic or ulcerated. Depending on severity, bleeding can vary from atenous red line along the gingival sulcus to profuse bleeding. Sometime bleeding appears immediately after removal of the probe other times it may be delayed a few seconds, therefore, the clinician should recheck for bleeding 30-60 seconds after probing.
Microbial analysis the sample must be collected from four individual deepest periodontal pocket in each quadrant by mean of sterile paper-point to detect pathognomonic bacteria
Periodontal pocket
Periodontal pockets are generally painless but may give rise to symptom such as localized or sometimes radiating pain or sensation of pressure after eating which gradually diminishes, foul taste in localize area sensitivity to hot and cold.
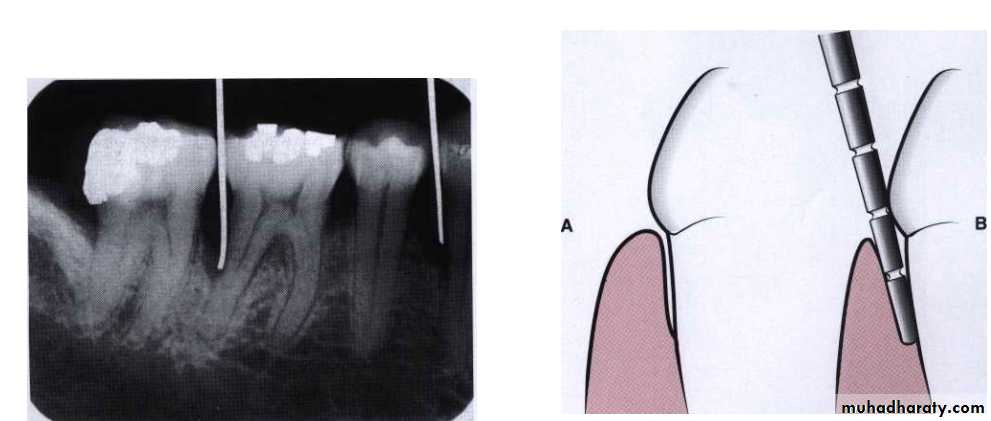
Detection of pocket: the only accurate method of detecting and measuring periodontal pockets is careful exploration with a periodontal probe.
Probing technique: The probe should be inserted parallel to the vertical axis of the tooth and walked circumferentially around each surface of each tooth to detect the areas of deepest penetration.
Level of attachment versus pocket depth
Pocket depth is the distance between the base of the pocket and gingival margin while the level of attachment is the distance between the base of the pocket and fixed point on the crown (cementoenamel junction), change in the level of attachment can be due only to gain or loss of attachment.Palpation: palpation the oral mucosa in the lateral and apical areas of the tooth may help locate the origin of radiating pain that the patient cannot localize.
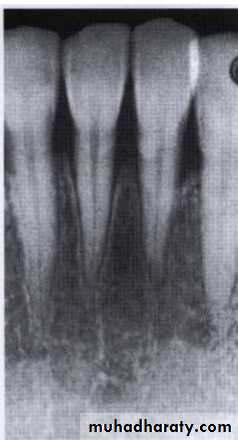
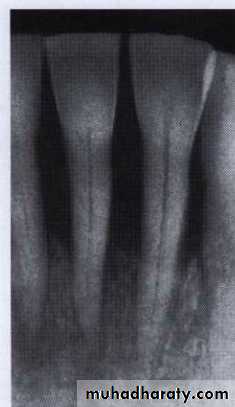
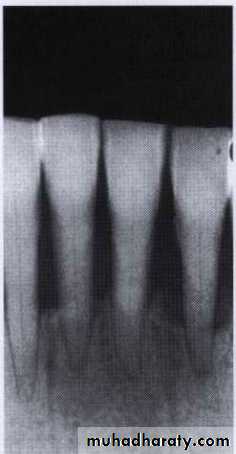
Radiographical diagnosis
The radiograph reveals alterations in calcified tissue shows the effect of past cellular experience on the bone and roots. The radiograph does not reveal minor destructive changes in bone therefore slight radiographic changes in the periodontal tissue mean that the disease has progressed beyond its earliest stages the earliest signs of periodontal disease must be detected clinically. Moreover the radiographical image tends to show less severe bone loss than that actually present.
Radiographic changes in periodontitis:
Break in the continuity of lamina dura these result from the extension of gingival inflammation into the bone causing widening of the vessel channels and a reduction in calcified tissue at the septal margin.A wedge-shaped radiolucent area is formed at the mesial or distal aspect of the.
crest of the septal bone
The destructive process extends across the crest of the interdental septum and the height is reduce
The height of the interdental septum is progressively reduced by extension of inflammation and the resorption of bone.
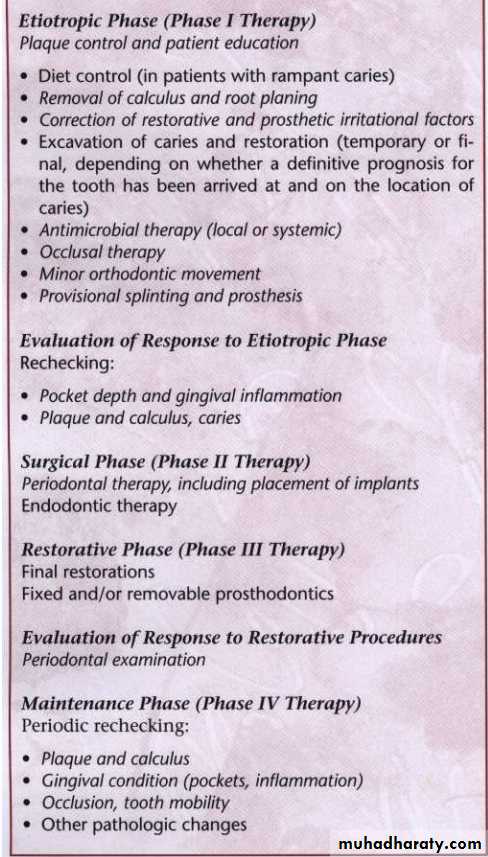
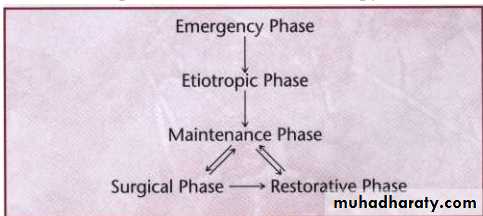
Phase I therapy
It is the first step in the procedure that constitute periodontal treatment. The objectives is to alter or eliminate the microbial etiology and contributing factors for gingival and periodontal disease. It is achieved by:Complete removal of calculus
Correction of defective restoration
Treatment of carious lesions
Institution of a comprehensive daily plaque control regimen
Phase I therapy has many specific goals:
Evaluation and alteration of patient systemic risk factors.
Plaque control performed by the patient.
Removal of microbial plaque and calculus from the surface of the teeth.
Appropriate use of antimicrobial agents and devices including necessary plaque sampling and antibiotic sensitivity test.
Control or eliminating of contributing local factors which including:
Treatment of poorly fitting restorations
Correction of poorly fitting prosthetic devices
Restoration of carious lesion
Odontoplasty
Tooth movement
Treatment of food impaction areas
Treatment of occlusal trauma
Extraction of hopeless teeth
Reevaluation
Reevaluation of the periodontal case should occur about 4 weeks after the completion of scaling and root planning procedures. This permits time for both epithelial and connective tissue healing, correction of conditions such as overhanging margins and sufficient practice with oral hygiene skill so that the dentist can accurately assess the periodontal condition at the end of phase I therapy.
Healing consists of the formation of a long junctional epithelium rather than new connective tissue attachment to the root surface. Transient root hypersensitivity and recession of gingival margins frequently accompany the healing process.
Refer to specialist:
Extent of disease . the deeper the pocket the stronger indication for referal
Root length
Hypermobility
Difficulty of scaling and root planning: presence of deep pocket and furcation make it difficult.
Restorative work: if there is extensive planning work.
Age of the patient: younger with extensive attachment loss, the more aggressive disease .
Resolution by shrinkage.
Plaque control
Carefully performed daily home plaque control, combined with frequent professionally delivered plaque removal, has been demonstrated to reduce supra gingival plaque and decrease the total number of periodontal pathogen.
Self-performed plaque control
Tooth brush
For most patient short headed brushes with straight-cut, round-ended, soft to medium nylon bristles arranged in three or four rows of tufts are recommended. However, if the patient perceives any benefit from a particular brush design characteristic, use of that brush should be encouraged.
Powered toothbrushes
Children and adolescents
Children with physical or mental disabilities
Hospitalized patients
Patients with fixed orthodontic appliances
Dentifrices
Aid in cleaning and polishing tooth surfaces. They are used mostly in the form of pastes, although tooth powders and gel are also available. They are made up of abrasives such as silicon oxides, aluminum oxides; water humectants; soap; flavoring; therapeutic agent such as fluorides and pyrophosphates and coloring agents and preservatives.
Tooth brushing methods:
The methods can be categorized primarily according to the pattern of motion when brushing move:
The roll method (modified stillman technique)
Vibrating method (bass,stillman,charter technique)
Circular method (the fones technique)
Vertical method (the leonard technique)
Horizontal method (the scrub technique)
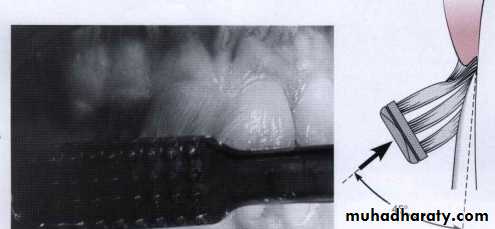
Bass method
Place the bristles at the gingival margin establishing an angle of 45 degree to the long axis of the teeth using short back-and-forth motions without dislodging the tips of the bristles. This motion forces the bristle ends into the gingival sulcus area as well as partially into the interproximal embrasures. To help reach the lingual surfaces of the anterior teeth insert the brush vertically.
Bass method has certain advantages over other techniques, as follows:
The short back-and-forth motion is easy to master because it is a simple movement familiar to most patients who brush using ascrub technique.It concentrates the cleaning action on the vertical and interproximal portions of the teeth, where microbial plaque is most likely to have accumulated.
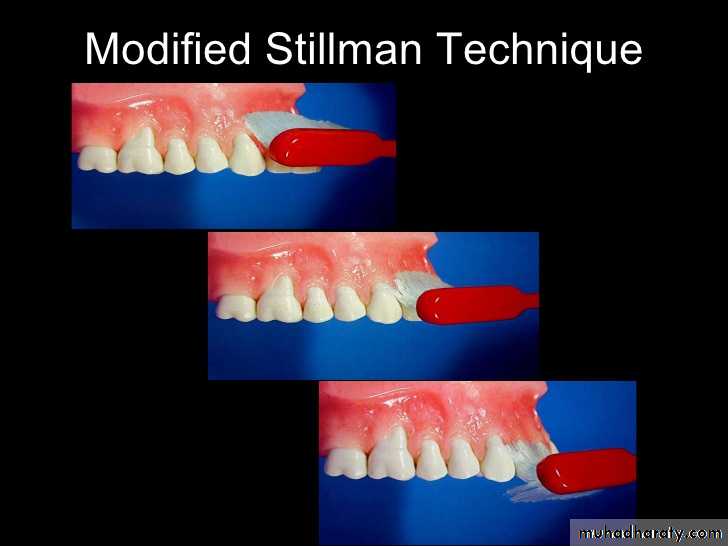
The modified stillman method:
Brush be placed with bristle ends resting partly on the cervical portion of the teeth and partly on the adjacent gingiva at an oblique angle to the long axis of the teeth. The brush move about 20 short back-and-forth strokes while simultaneously moving it coronally along the attached gingiva, the gingival margin and tooth surface. A soft or medium brush should be used with this technique to minimize trauma to the gingiva.
This method may be recommended for cleaning in areas with progressing gingival recession and root exposure to minimize abrasive tissue destruction.
Charter method
This method requires placement of a soft or medium brush on the teeth with the bristles pointed toward the crown at 45-degree angle to the long axis of the teeth.
The charter method provides gentle plaque removal. So it recommended for cleaning in areas of healing wounds after periodontal surgery.
Interdental cleaning aids
The specific aids required for interproximal cleaning depend on various criteria such as the size of the interdental space, the presence of furcation involvement, tooth alignment, and presence of orthodontic appliance or fixed prosthesis.Among the numerous aids available dental floss and interdental cleaners such as wooden or plastic tips and interdental brushes are commonly recommended. It is important to remember that brushing alone is not sufficient for plaque removal and that some interproximal devices need to be used routinely by the patient in the daily plaque control regimen.
Caries control for the periodontal patient
Dental caries, particularly root caries can be problem for periodontal patient because of attachment loss associated with the disease process and periodontal therapeutic procedures. The major difference between root and crown caries is the amount of organic material in the root surface is greater than in enamel, so once the demineralization has occurred the organic matrix is exposed resulting in destruction of the root surface. Fluoride works primarily by topical effects to prevent and reverse the caries process. It has been demonstrated that the use of fluoride dentifrice containing 5000 ppm fluoride was more effective in reversing active root lesion than fluoride level of 1100 ppm found in conventional toothpaste..Chemical plaque control
Chlorhexidine
The agent that has shown the most positive results to date. The initial finding that two daily rinses with 10 ml of a 0.2 aqueous solution of chlorhexidine digluconate almost completely inhibited the development of dental plaque , calculus, and gingivitis.
Its side effects:
Primarily brown staining of the teeth, tongue, and resin restoration.
Transient impairment of test perception
Chemical plaque control has been shown to be effective for both plaque reduction and improved wound healing after periodontal surgery specially when prescribed for use after surgery for periods 1 to 4 weeks.
Professional plaque control
Scaling and root planning
Scaling: It is removal of plaque and calcified deposits from the crown of the tooth.
Root planning: it is removal of plaque and calcified deposits from the root surface of the tooth, removal of altered cementum from subgingival root surface and debridement of the soft tissue lining the pocket.
Scaling and curettage instruments are classified as follows:
Sickle scaler used to remove supragingival calculus.
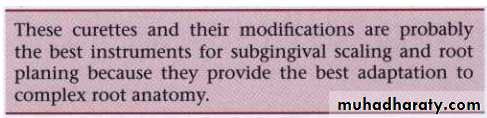
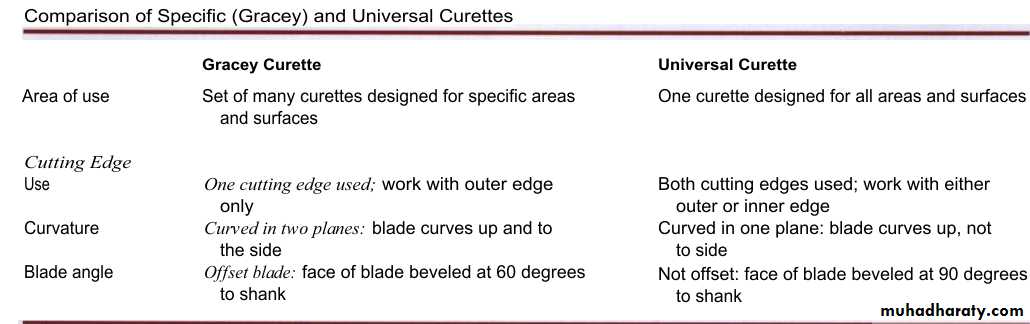
Currettes used for sugingival scaling, root planning and removal of the soft tissue lining the pocket
Universal curettes can be inserted in most areas of dentition, the face of the blade is at a 90-degree angle (perpendicular)
Gracy curettes: are representative of the area-specific curettes, a set of several instruments designed and angled to adapt to specific anatomic areas of dentition.
The gracy curattes differ from the universal curattes in that the blade is not at a 90-degree angle to the lower shank.
Hoe, chisel and file scaler used ti remove subgingival calculus and alter cementum but their use is limited
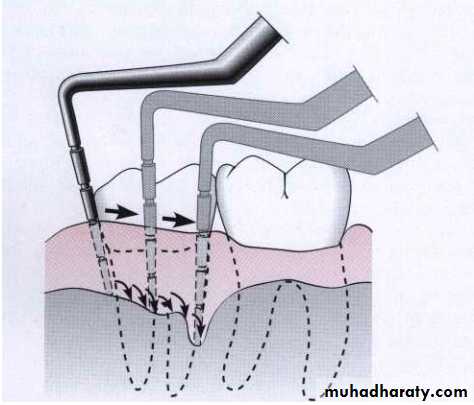
Ulterasonic and sonic instruments used for scaling and cleansing tooth surfaces and curetting the soft tissue wall of the periodontal pocket.
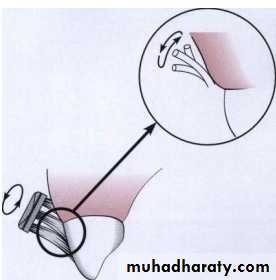
Periodontal endoscope used to visualized deep subgingivally in pockets and furcations enabling the detection of deposits.
Cleansing and polishing instruments such as rubber cups, brushes, and dental tape are used to clean and polish tooth surfaces. Also available are air-powder abrasive system for tooth polishing.
Scaling and root planning are done either by manual instrumentation or by sonic and ultrasonic instrumentation.
However effective instrumentation is governed by:
Poroper position of the patient and the operator.
Illumination and retraction for optimal visibility
Sharp and clean instruments are fundamental prerequisties.
Knowledge of instrument design enable the clinician to efficiently select the proper instrument for the procedure and the area in which it will be performed.
Proper grasp, figure rest, angulation must be understood.
Maintaining a clean field.
Instrument stabilization.
Supra and sub gingival irrigation
In the treatment of periodontal disease, irrigation is used as a lavage to flush away the bacteria that are in contact with periodontal tissue. It is a nonspecific reduction of plaque bacteria. There are two type of irrigation supragingival and subgingival irrigation.
Irrigator devices
Monojet or multistreamed jet tips are available for supragingival irrigation as well as blunted cannulae with end or side parts for subgingival irrigation. Continuous flow of water during irrigation causes constant tissue compression and may impair removal of bacteria.Supragingival irrigation
Pulsating monojet irrigators are preferred for supragingival irrigation. The therapeutic effects of supragingival irrigation with water has limited effects on supragingival plaque mass or the composition of the subgingival microflora. The minimal effective dosage for once daily supragingival irrigation with chlorhexidine digluconate has been established to be 400ml of a 0.02% solution.
Chemotherapeutic agent in treatment of periodontal disease
In certain types of periodontal disease including advance periodontitis, refractory periodontitis and aggressive periodontitis adjunctive chemotherapeutic agents may be necessoryto control the disease process.Chemotherapeutic agents: chemical substances that provides a clinical therapeutic benefit.
Guidelines for use antibiotics in periodontal therapy:
Clinical diagnosis dictate the need for possible antibiotic therapy as an adjunct in controlling active periodontal disease.
Continuing disease activity
When microbiological sampling is performed
When they have been shown to have avalue in reducing the need for periodontal surgery
The selection of Antibiotic based on microbial composition and .
patient's medical status.
Antibiotic should not be used as a monotherapy.
Tetracycline
tetracycline can reduce collagen and bone destruction as well as the antibiotic effect that can reduce periodontal pathogens in periodontal tissues. Tetracycline used as adjunctive in treatment of localized aggressive periodontitis
((doxycycline 100mg twice daily the first day then 100mg once daily for one week))
Metronidazole
Clinically used to treat gingivitis, acute necrotizing ulcerative gingivitis, chronic periodontitis and aggressive periodontitis.250mg twice daily for one week.