The immune system andthe oral cavity
5th Lecture For Third YearImmunology:
The Immune system is remarkably versatiledefense system that has evolved to protect animals from invading pathogenic microorganisms and cancer.
It is able to generate an enormous variety of cells and molecules capable of specifically recognizing of foreign invaders. And they act together in a dynamic network.
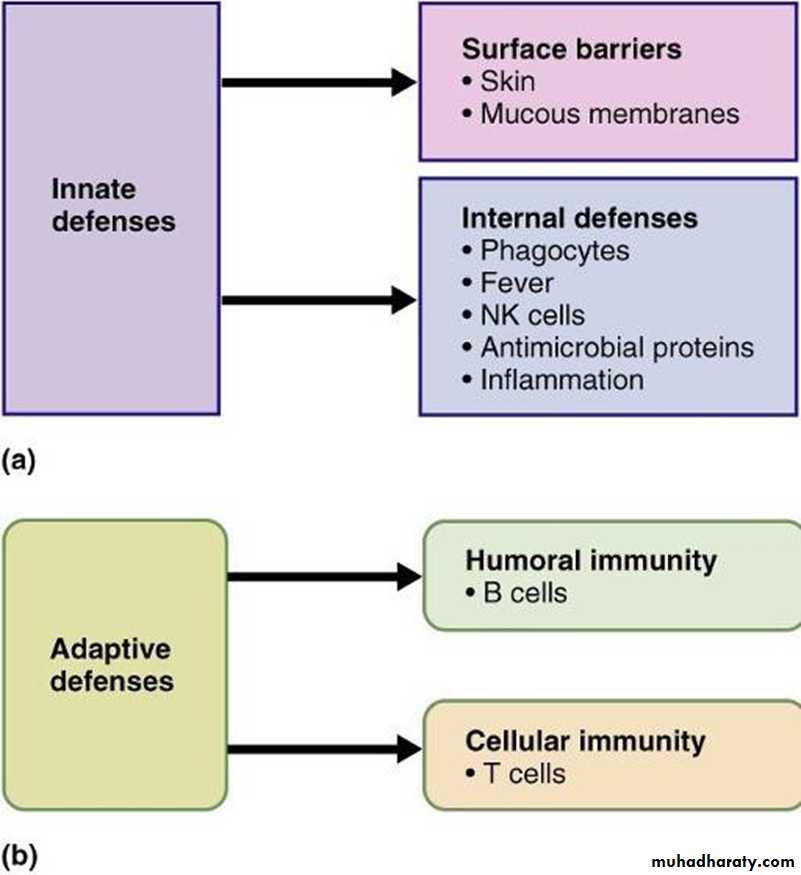
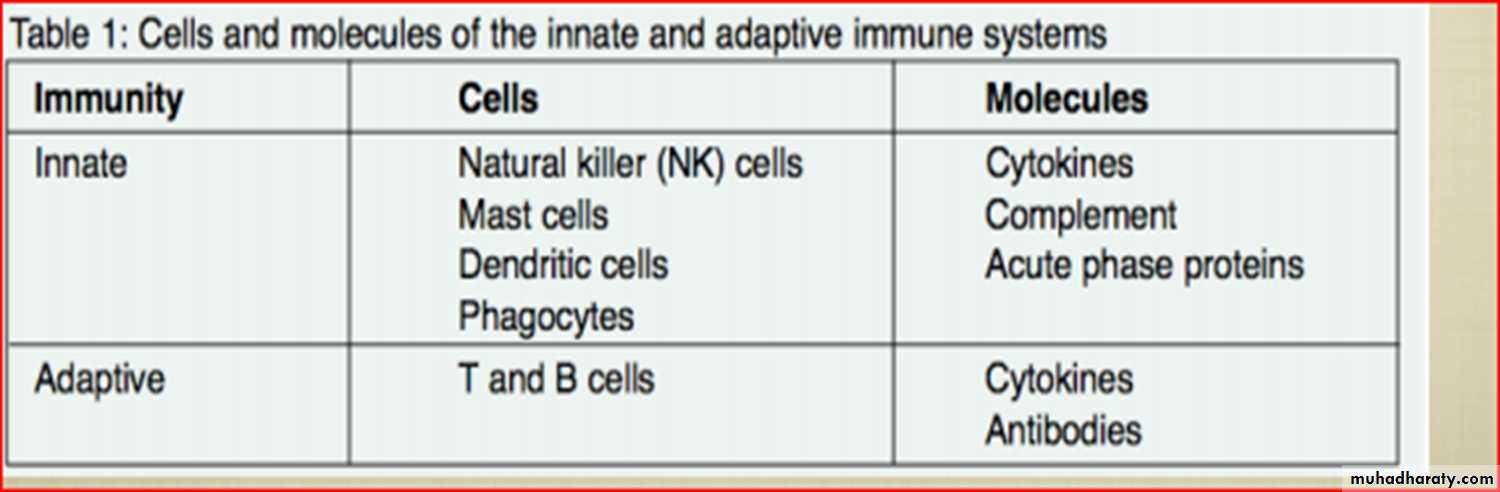
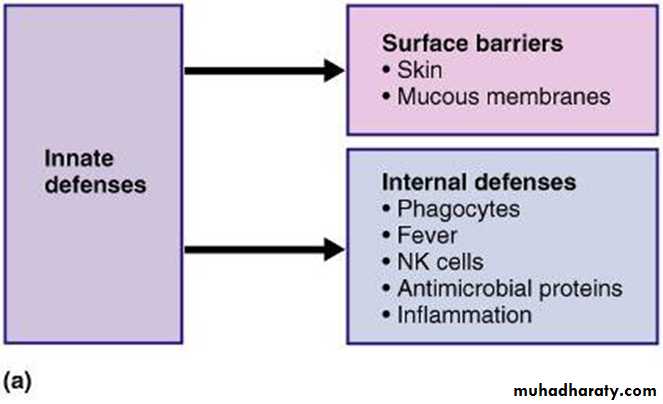
1. natural or innate immunity, comprising mainly
pre-existing antigen-non-specifc defences2. adaptive or acquired immunity, during which theimmune system responds in an antigen-specifc manner
to neutralize the threat effciently, and retains a memory of the threat so that any future encounter with the same threat will result in an accelerated and heightened protective response.
There are two kinds of immunological defence
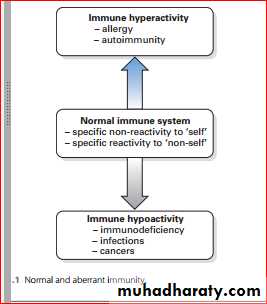
Immunologic Dysfunction
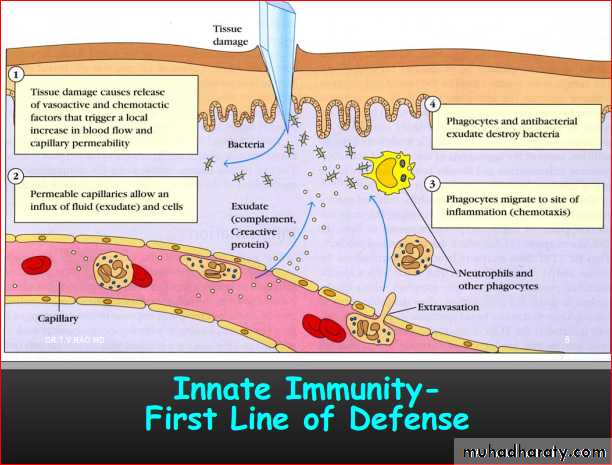
The innate immune system
These intrinsic defence mechanisms are present at birth prior to exposure to pathogens or other foreign macromolecules.They are not enhanced by such exposures and are not specifc to a particular pathogen.
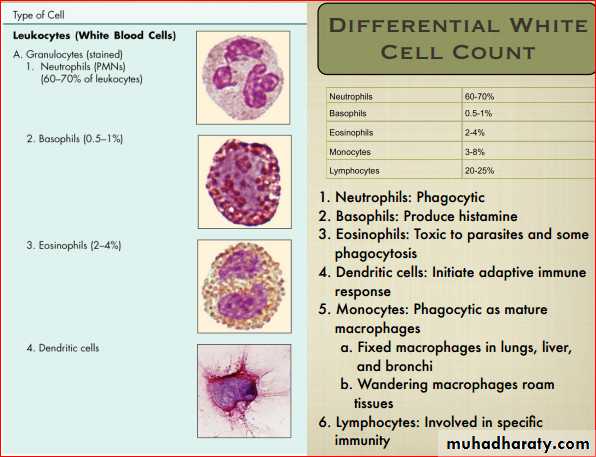
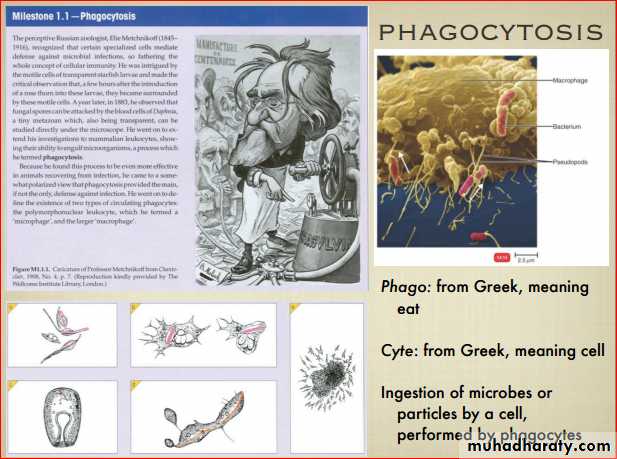
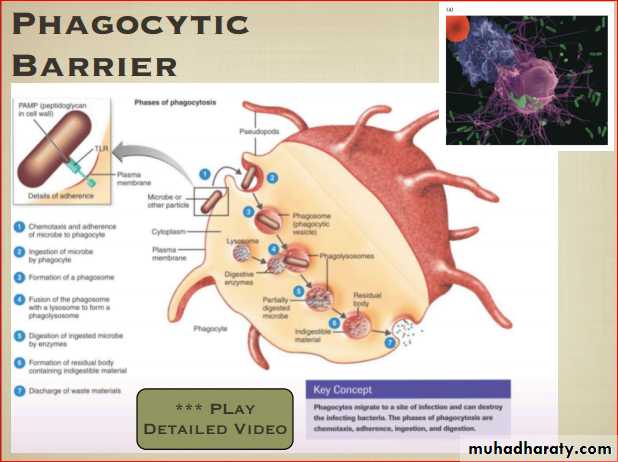
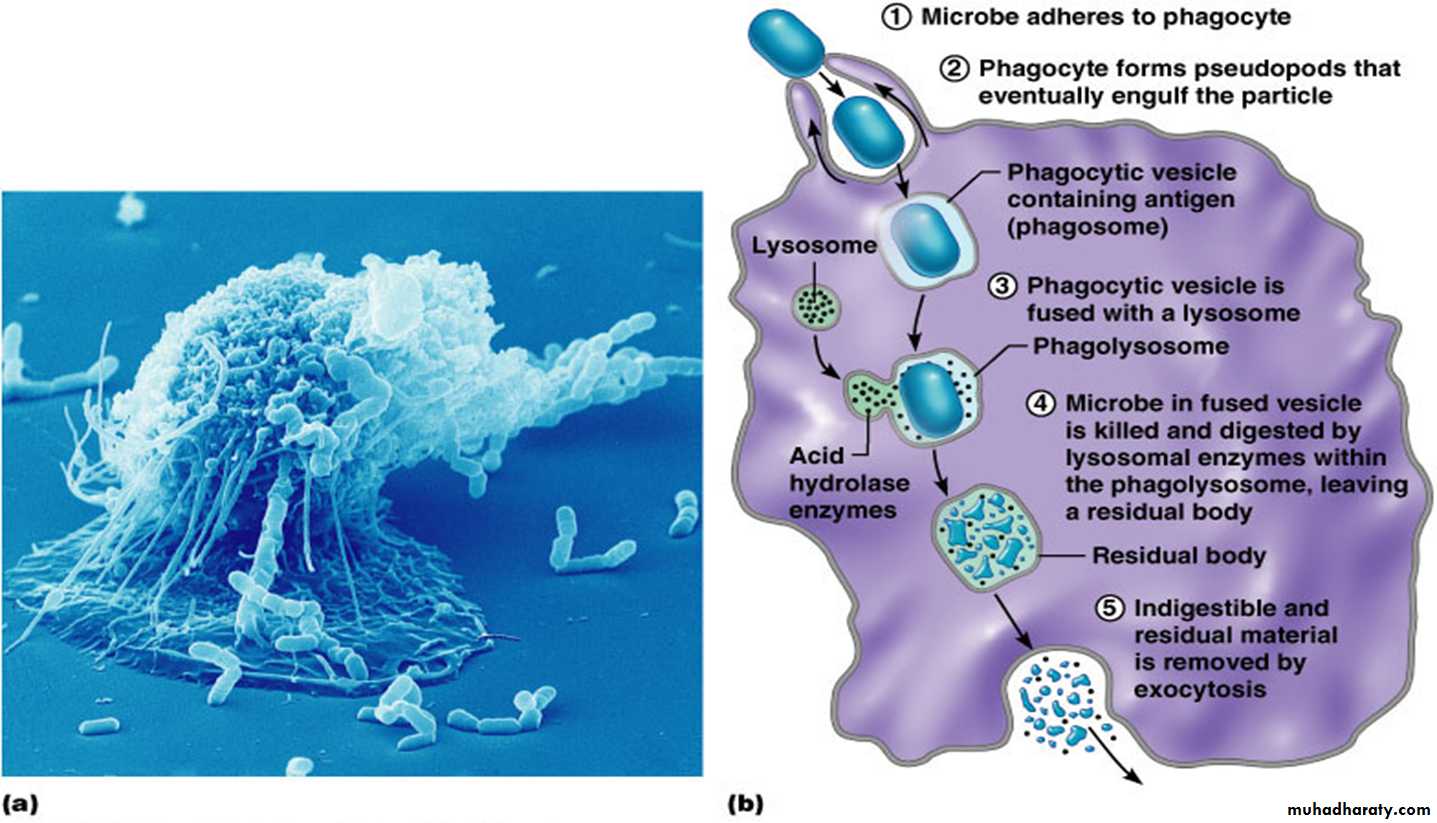
Phagocytosis
is a process by which phagocytic cells ingest extracellular particulate material, including whole pathogenic microorganisms. If the mechanical defences are breached, the phagocytic cells become the next barrier.These include polymorphonuclear leukocytes (polymorphs) and macrophage.
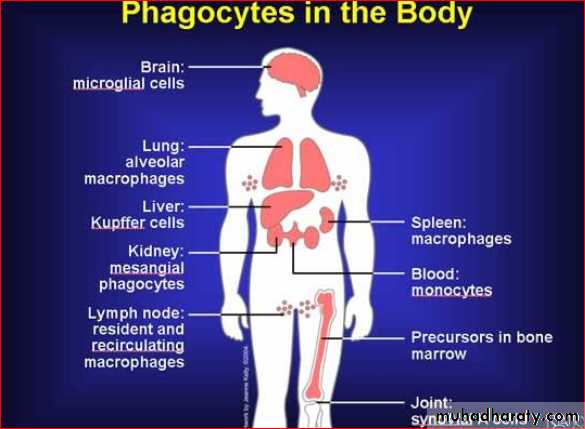
The former are short-lived circulating cells, which can invade the tissues, while the latter are the mature, tissue-resident stage of circulating monocytesSite of Microphage
Macrophages are found in areas of blood filtration where they are most likely to encounter foreign particles,e.g.
Liver = Kupffer cells
Brain = microglial cells
Lung = alveolar macrophages
Lymph node = resident and recirculating macrophages and dendritic cells
Synovium = synovial A cells
Kidney = mesangial phagocytes
Skin = Langerhans’ cells
Bone = Osteoclasts
Mode of action of Phagocytosis
Phagocytes attach to microorganisms by non-specifc cell membrane ‘threat’ receptors, after which pseudopodiaextend around the particle and internalize it into a phagosome. Lysosomal vesicles containing proteolytic enzymes fuse with the phagosome, and oxygen and nitrogen radicals are generated, which kill the microbe.
The phagocytes have several ways of dealing with the phagocytosed material.
macrophages may reduce molecular oxygen to form
microbicidal-reactive oxygen intermediates that are secreted into the phagosome
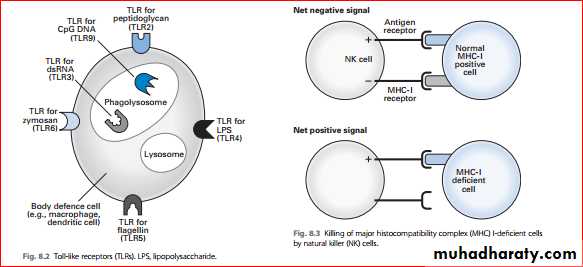
Pathogen-associated molecular patterns, pattern-recognition receptors and Toll-like receptors
The cells involved in innate immune responses such
1- phagocytes(neutrophils,monocytes,macrophages)
+
2- cells that release inflammatory mediators(basophils, mast cells and eosinophils)
--------------------------------------------------------------------------- recognize only a few highly conserved structures present in many different microorganisms. These cells recognize microbial structures called pathogen-associated molecular patterns (PAMPs) in order to activate the innate immune response.
what is PAMPs ?
are molecular components common to a variety of microorganisms but not found as a part of eukaryotic cells and include:-•lipopolysaccharide (LPS) in G- bacteria
• peptidoglycan, lipotechoic acids from the in G+ bacteria• bacterial DNA
• double-stranded RNA from viruses
• glucans from fungal cell walls.
A major class of signalling PRRs is Toll-like receptors (TLRs), so named because of their similarity to the protein coded by the Toll gene identifed in Drosophila melanogaster
This promotes the attachment of microbes to phagocytes
and their subsequent engulfment and destruction.Most defence cells (macrophages, dendritic cells, endothelial cells, mucosal epithelial cells, lymphocytes) have on their surface a variety of receptors called pattern-recognition receptors (PRRs) capable of binding specifcally to conserved portions of PAMPs so there is an immediate response against invading microbes.
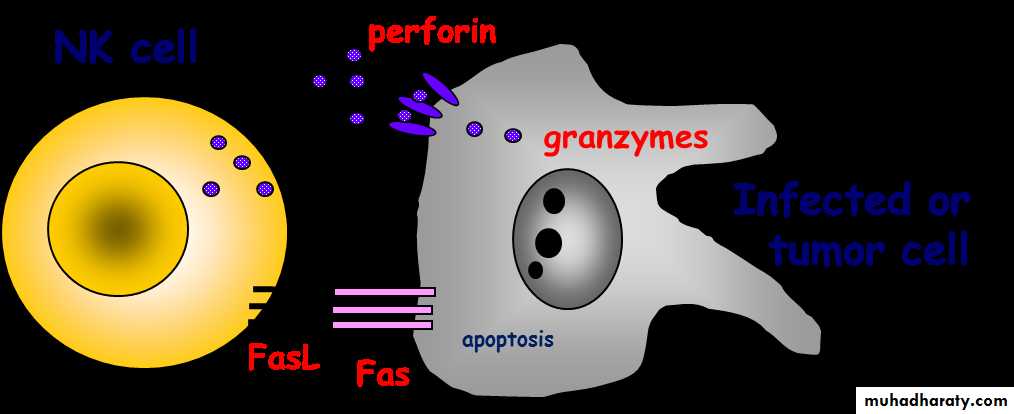
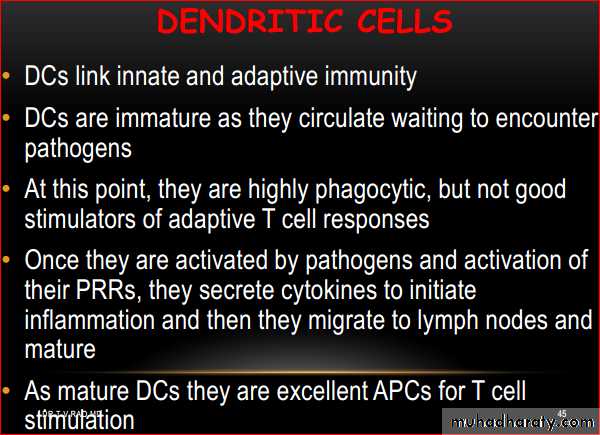
Natural killer cells
• Small population of large granular lymphocytes• Non specific for “non-self”
• Not phagocytic: attack is by release of perforins that perforate the target cell plasma membrane.
• Shortly after perforation the target nucleus disintegrates.
• Release chemicals that enhance the inflammatory response
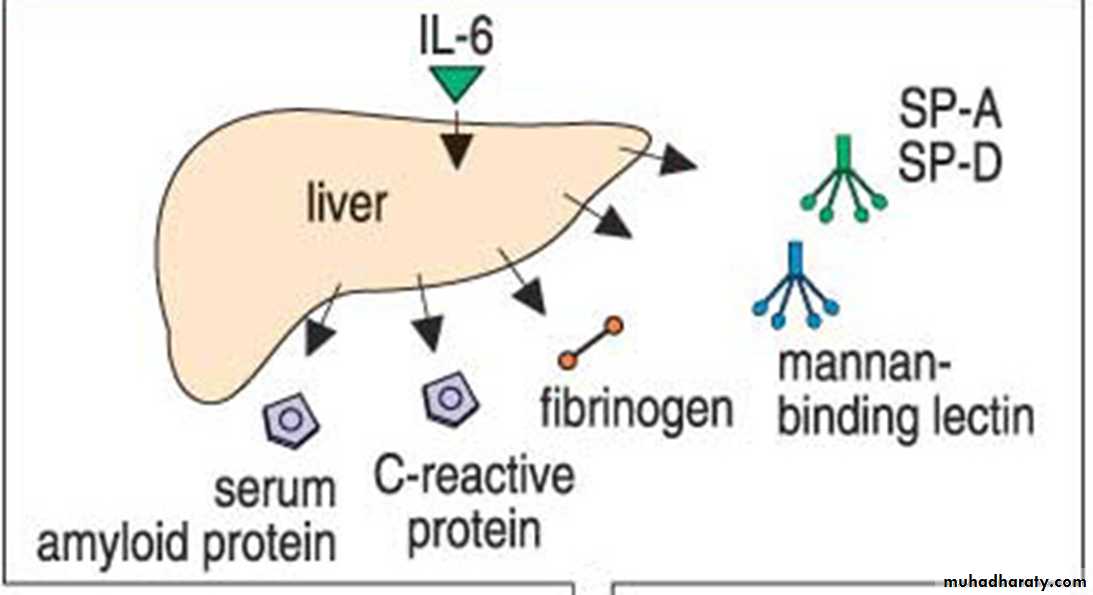
Acute-phase proteins
are serum proteins produced by the liver in response to tissue-damaging infections and other inflammatory stimuli such as cytokines (e.g. IL-1 and IL-6).The important role of Acute-phase proteins :-
1-It enhance the efficiency of innate immunity.
2- opsonization, coagulation, antiprotease activity and/or complement activation
The Compenant of Acute
-phase proteins
C-reactive protein
α1-Antitrypsin
Mannose-binding protein
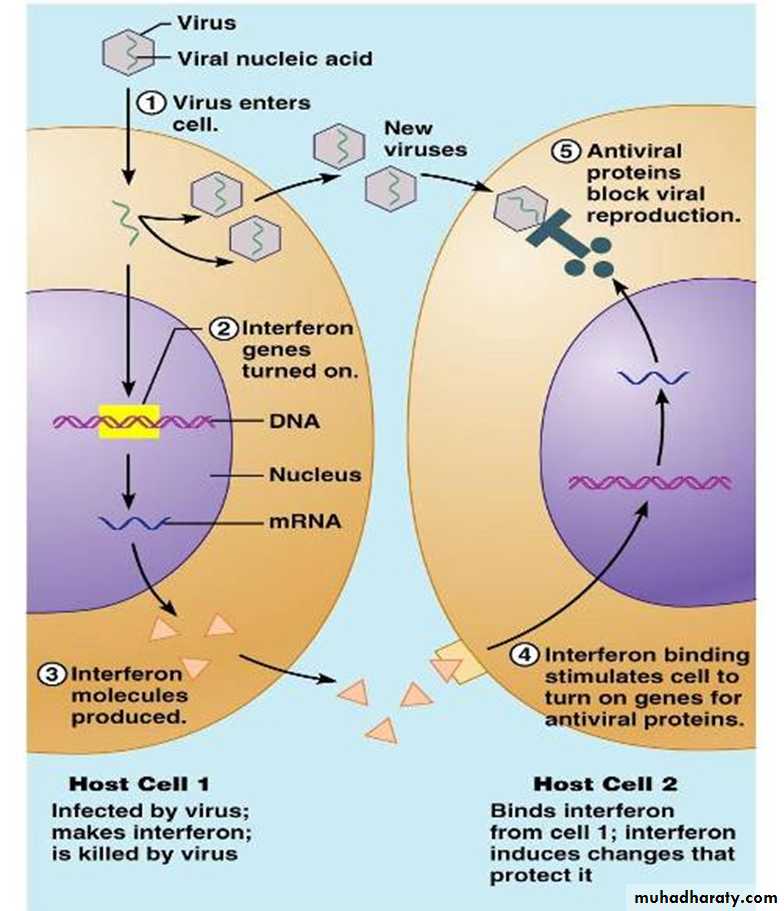
INTERFERON
Defense against viral infectionsCytokine produced & released by host cells invaded by virus
Prevents virus from infecting healthy cellStimulates uninfected cells to produce antiviral proteins
INF- & INF- are antiinflammatoryINF- is proinflammatory and enhances cell-mediated immunity
Effects of INTERFERONActivation of endoribonuclease and protein kinase
Destruction of viral mRNA
Inhibition of protein synthesis (EF-2 phosphorylation)
Upregulation of MHC class I
Enhancement of T cytotoxic activity
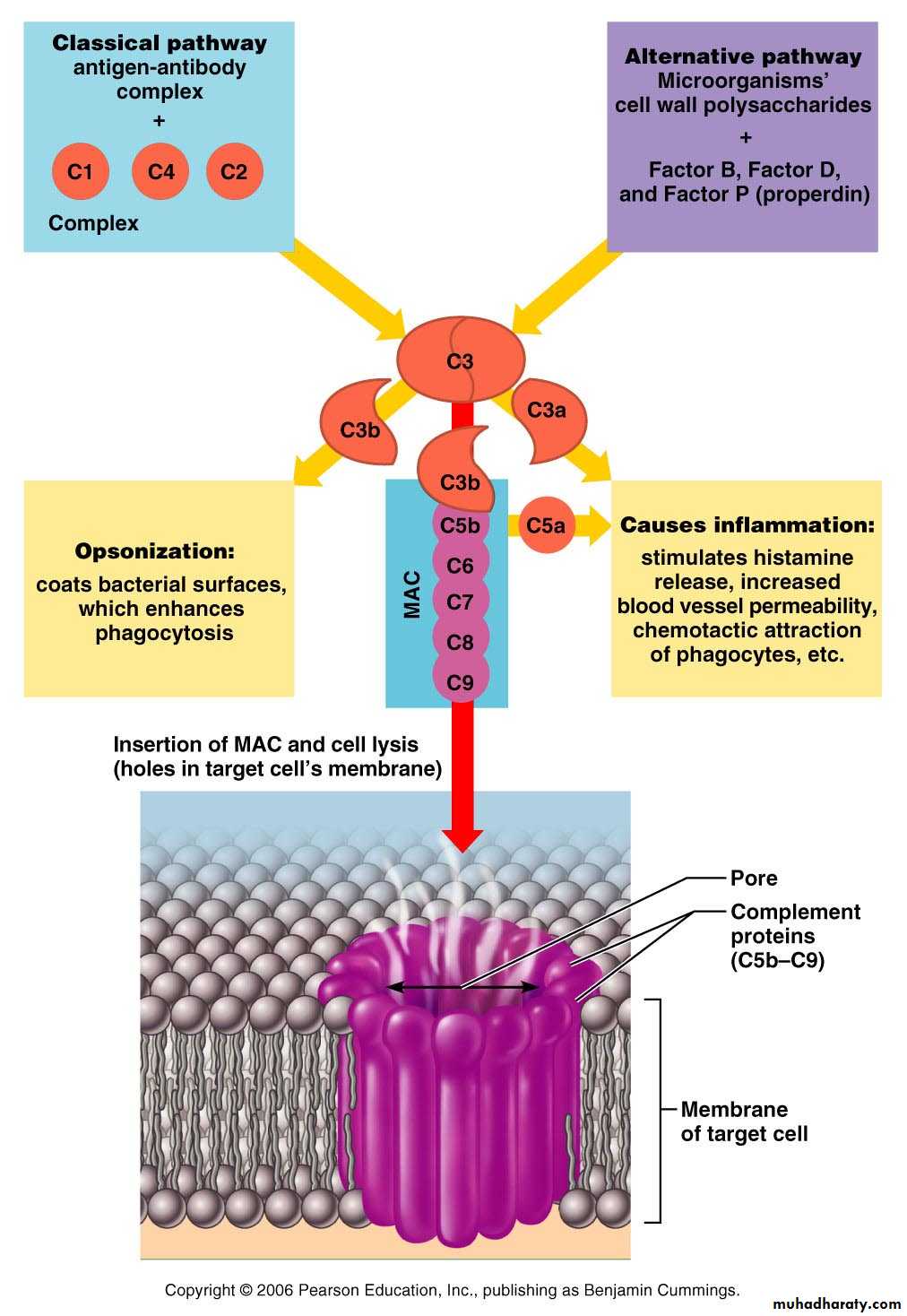
Activation of Natural Killer (NK) cellsComplement
is very much involved in the inflammatory response and is one of group of plasma proteins the key effector mechanisms of the immune system.It consists of at least 30 components– enzymes, regulators and membrane receptors – which interact in an ordered and tightly regulated manner to bring about phagocytosis or lysis of target cells
Complement components are normally present in body fluids as inactive precursor.
Complement activation enhances both innate & adaptive defensesInnate, Internal Defenses
Complement activation pathwaysClassical pathway: requires antibodies
Antibodies bind to target (antigen)
Complement protein C1 binds to the antibody-antigen complex (complement fixation)
Alternative pathway: complement factors interact with microorganism glycocalyx
Both pathways lead to a cascade of protein activation, leading to activation of C3• Innate, Internal Defenses; Complement
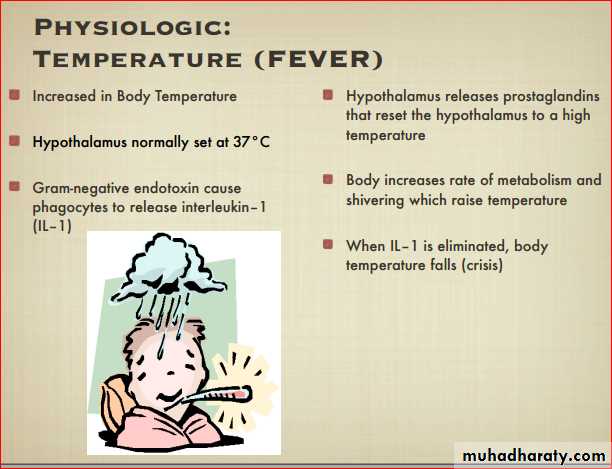
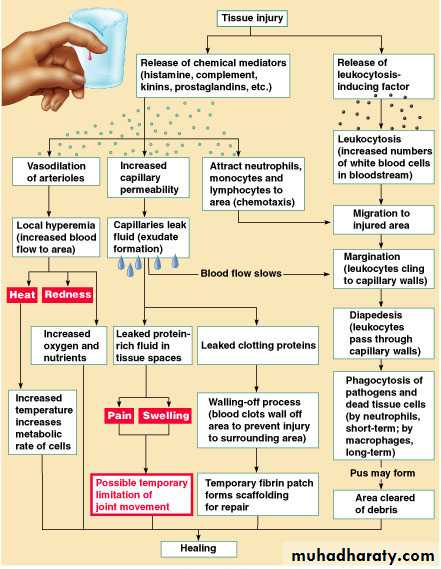
Innate, Internal Defenses: Inflammation
tissue response to injuryTriggered by injury – trauma, heat, chemical
irritation, infection, etc.
Beneficial effectsPrevents spread of injury
Disposes of cellular debris & pathogens
Promotes repair
• Innate, Internal Defenses: Inflammation
cardinal signs of inflammation
Redness
HeatSwelling
Pain
(functional impairment Rigor)
• Innate, Internal Defenses: Inflammation
Inflammatory response: signs are associated with vasodilation & increased vascular permeabilityDilation: redness, heat
Permeability: edema, (increased pressure) painPain also associated with bacterial toxins & some mediators (kinins, PGs)
Innate, Internal Defenses: Inflammatory ResponseMechanisms causing vasodilation & vascular permeability
Injured cells release inflammatory mediators
Histamines
Kinins
Prostaglandins
Complement
Cytokines (also activated by receptors on macrophages in response to microbial glycocalyx)
Innate, Internal Defenses: Inflammatory Response
Edema
Dilutes harmful substances
Provides nutrients (& O2) for repair
Enhances entry of clotting protein
Epithelial breaches also stimulate b-defensin release from epithelial cells
Events in Inflammation
Figure 21.3Innate, Internal Defenses: Inflammatory Response
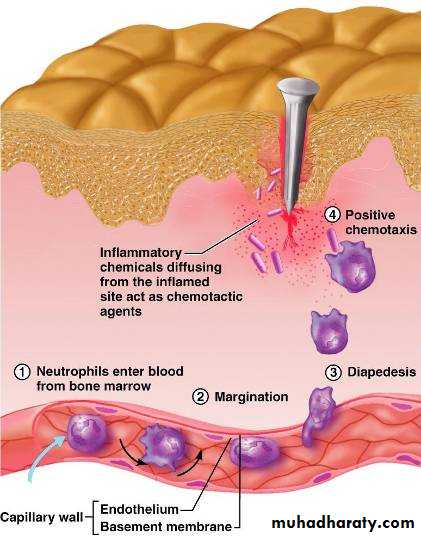
Phagocyte mobilization: infiltration of damaged area by neutrophils & macrophagesInnate, Internal Defenses: Inflammatory Response
Leukocytosis: leukocytosis inducing factors released by injured cells promote rapid release of WBCs from marrowMargination: increased vascular permeability causes decreased fluid in vessels; blood flow slows & neutrophils are able to move to vessel margins. Here endothelial markers (CAMs) allow neutrophils to cling to vessel walls (pavementing).
Innate, Internal Defenses: Inflammatory Response
Diapedesis: neutrophils migrate through capillary walls
Chemotaxis – inflammatory chemicals attract neutrophils to move up the chemical concentration gradient (neutrophils respond first)
As the process continues, monocytes diapedes into the area & become macrophages. With chronic inflammation, macrophages predominate
Inflammatory Response:Phagocytic Mobilization
Figure 21.4
Innate, Internal Defenses: Inflammatory ResponseMacrophages clean up cellular debris & pathogens
If pathogens were associated with the injury, activation of the complement cascade occurs & elements of adaptive immunity join the process