The Small & Large Intestine
AnatomySmall Bowel
The length : 300 - 850 cm
From duodenojejunal (DJ) flexure to the ileocaecal valve.
The jejunum:
Proximal 40%
Wider
Thicker
More prominent mucosal folds (valvulae conniventes)
The ileum:
Thicker& more fatty mesentery
More complex arterial arcades
Contains larger aggregates of lymph nodes (Peyer’s patches)
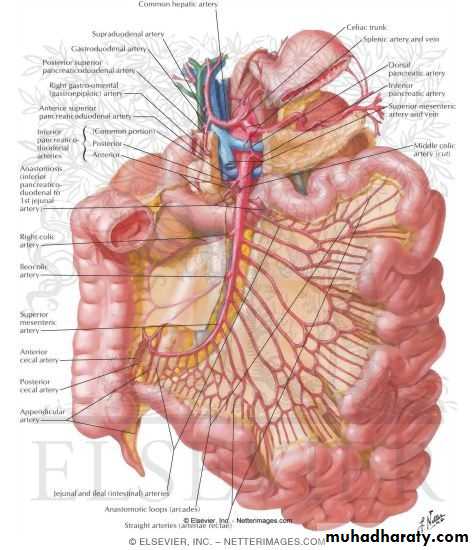
Blood supply
Arterial: superior mesenteric arteryVenous: superior mesenteric v. portal v.
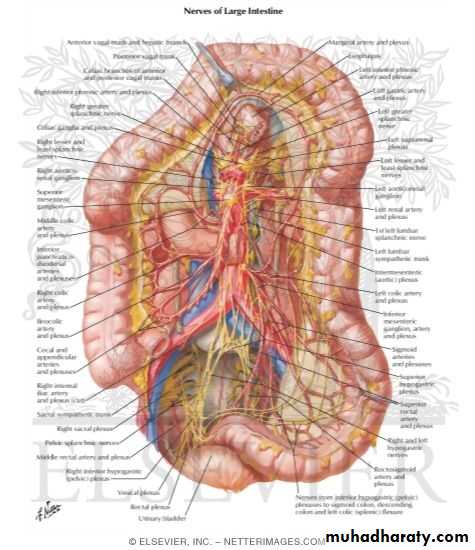
Nerve supply :
Parasympathetic secretomotor .
Sympathetic: - inhibit peristalsis
• - sensory
Peritoneal pain is somatic in nature & more precisely localized to the site of organ.
Visceral pain: Referred pain from the small intestine is usually felt in the periumbilical region (T10)
Blood , lymphatic vessels & nerves run in mesentery of small bowel.
Large Bowel
Length: 1.5 M from ileocecal valve to anus.Parts:
Cecum + appendix
Ascending colon up to hepatic flexure
Transverse colon with attached omentum, between hepatic & splenic flexures.
Descending colon
Sigmoid colon & rectum
Features:
- Fat tags (appendices epiploicae)
- The taenia coli are 3 flat bands of longitudinal muscle run from the appendix base to the rectosigmoid junction and they act to pull the colon into its typical sacculated state producing a series of haustrations.
Asc. & Desc. C. are fixed to retroperitoneum
Arterial supply
Superior mesenteric A: Rt colon as far as distal desc. colon.Inferior mesenteric A.
Marginal A of Drummond (formed from anastomosis of adjacent branches of both AA)
The ‘watershed’ area of the splenic flexure representing the junction between the superior and inferior mesenteric supply; is more liable to ischemic colitis.
Venous Drainage: portal vein.
Visceral pain from the part of the colon supplied by the superior mesenteric artery is in the periumbilical region, while pain from the colon distal to that point is felt suprapubically (T12–L1).
Physiology
Small Bowel:The jejunum: digestion and absorption of fluid, electrolytes, iron, folate, fat, protein and carbohydrate.
The terminal ileum (specific transporters): absorption of bile salts and vitamin B12 & fat-soluble vitamins A, D, E and K.
If the jejunum is resected, the ileum can assume all the required absorptive functions while the reverse is not.
Synthesis of plasma lipoproteins.
Synthesis of hormones which interact with the enteric nervous system.
Large Bowel:
Mainly water absorptionSalt Absorption (NaCl).
Fermentation of dietary fibre by colonic flora (anaerobic bacteria) leads to the generation of short chain fatty acids such as butyrate, which is an important energy source for colonic mucosa and may also contribute to daily energy requirements; Therefore ileostomy can result in diversion colitis.
Storage and evacuation of feces.
Colonic motility is variable: fecal residue reaches the cecum 4 hrs. after meal & 1-4 days to be passed from the rectum.
Inflammatory Bowel Diseases
SpecificUlcerative colitis.
Crohn’s disease.
Non-specific colitis/enteritis
Infective
Ischemic
Radiation
Diversion
Ulcerative colitis
Unknown etiology
Familial predisposition
No infective organism could be incriminated
Smoking has a protective effect.
Stress might lead to relapses
It was rare in eastern population however the incidence is increasing.
Sex ratio is equal
Uncommon before the age of 10, mostly between 20 and 40 yrs of age.
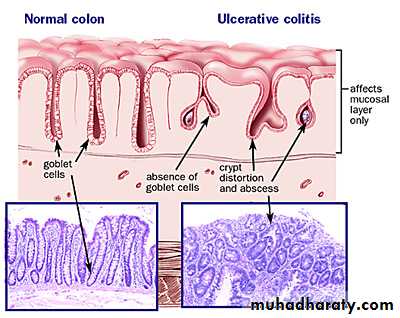
Pathology:
Nearly all cases starts in the rectum and extends proximally in continuity.Inflammation primarily affects the mucosa and sub mucosa.
There are multiple minute ulcers.
In chronic disease; inflammatory polyps (pseudo polyps) result from previous healed mucosal ulcerations leaving islands of spared mucosa which will become prominent.
In sever fulminant colitis, transverse colon may become acutely dilated with thin wall and may perforate (Toxic mega colon).
Microscopic examination
Increase inflammatory cells in the lamina propria
Infiltration of walls of crypts by inflammatory cells (crypt abscess).
Depletion of goblet cell mucin.
With time dysplasia & carcinoma in situ may develop.
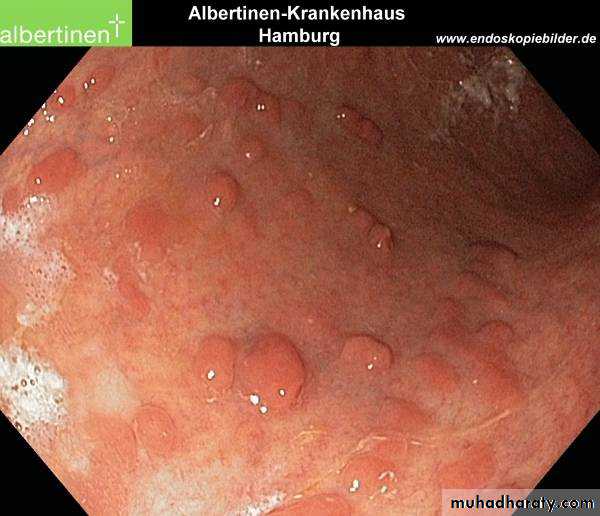
pseudopolyps
Symptoms:Chronic disease with relapses and remissions.
Proctitis:
- Disease confined to the rectum (95%).
- Tenesmus, rectal bleeding & mucous discharge.
More extensive colitis:
- Watery or bloody diarrhea.
- Systemic illness: malaise, fever, fluid / electrolytes losses, anemia and hypoproteinemia are common.
Disease severity:
Mild: - Fewer than 4 stools daily.Moderate:
- More than 4 stools daily
- Few systemic symptoms.
- Often raised ESR & CRP.
Severe:
More than 6 bloody stools a day.
Fever, tachycardia, anemia
Raised inflammatory markers.
Hypoalbuminemia.
Fulminant:
More than 10 bowel movements daily
Fever, tachycardia, continuous bleeding, anemia, hypoalbuminemia, abdominal tenderness and distension,
Progressive colonic dilation (toxic megacolon).
Investigations:
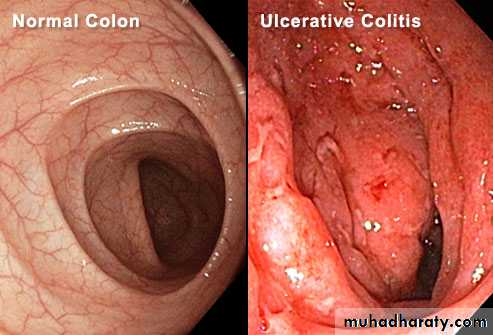
Sigmoidoscopy
Proctitis (Hyperemic mucosa, bleeds on touch and pus like exudates).
- Tiny ulcers are late signs.
Colonoscopy & Biopsy
- To establish the extent of the disease.
Differentiate between ulcerative colitis and Crohn’s colitis,
Monitor response to treatment,
Assess for malignant changes.
Plain x-ray
- Useful in toxic megacolon.transverse colon is dilated
large mucosal islands (edematous mucosal remnants between extensive ulcers).
No haustration
Barium enema
Loss of haustraPseudo polyps
Narrow shortened colon (in chronic disease / led pipe appearance)
tubular Lt colon
normal Rt colon
CT findings in pancolitis
Significant thickening of the colonic wallInflammatory stranding in the colonic mesentery
Stool Bacteriology to exclude infective colitis, e.g. Campylobacter, Shigella, amoebiasis, Clostridium difficile….
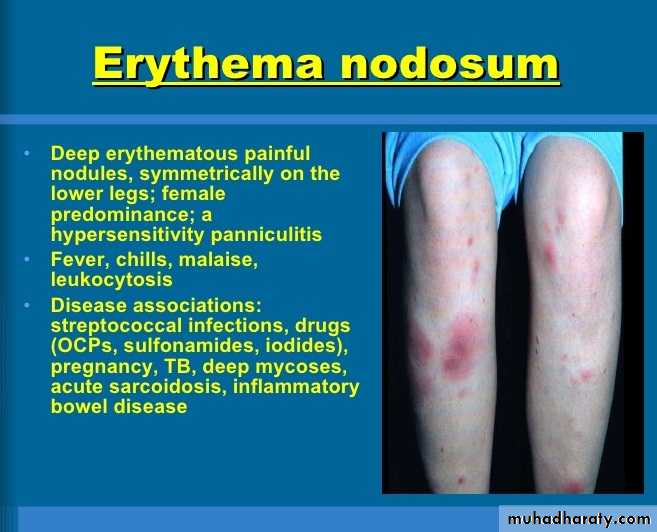
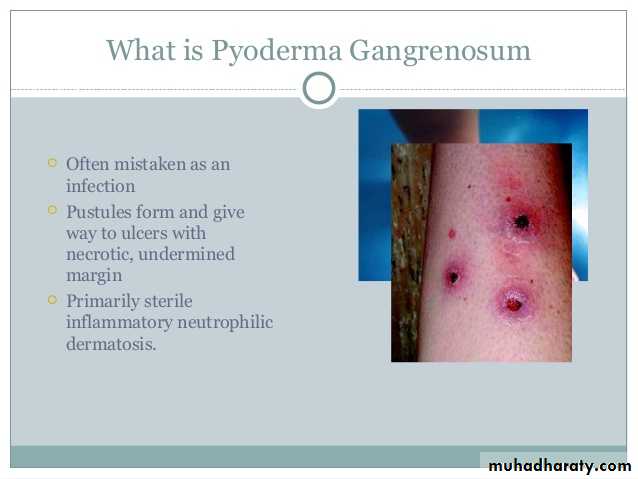
Extra-Intestinal manifestation:
Arthritis of large joints, sacro-iliitis and ankylosing spondylitis.Sclerosing cholingitis.
Skin lesions: erythema nodosum, and pyoderma gangrenosum.
Uveitis and episcleritis.
Cancer risk in UC:
More in pancoloitis & long standing disease.
At 10 years from diagnosis, it is around 1 %, may be as high as 20 % at 30 years.
cancers may be found in 40 % of colectomy specimens for colitis-associated dysplasia.
Erythema Nodosum: Deep painful erythematous nodules, symmetrical on both legsPyodermaganfrenosum
Treatment
Mild- moderate attacksSteroids:
Rectal enemas.
Oral prednisolone 20-40 mg per day for 3 to 4 weeks.
5-Aminosalicylic acid derivatives (Sulphasalazine..) 1 gm, 3 times daily.
Severe attacks
Admission to the hospital.Frequent measurement of abdominal girth.
Daily abdominal x-ray for follow of dilatation of the transverse colon of more than 5.5 cm.
The presence of mucosal islands, increasing colonic diameter or a sudden increase in pulse or temperature may indicate colonic perforation.
Stool chart to help assessment of response to therapy.
Maintenance of fluid and electrolytes.
Correction of anemia and nutritional deficiency, nothing by mouth.
I.v hydrocortisone 100-200 mg 4 times daily, Rectal steroids.
Sometimes Azathioprine or cyclosporine A, or infliximab.
Failure of treatment within 5-7 days – consider surgery.
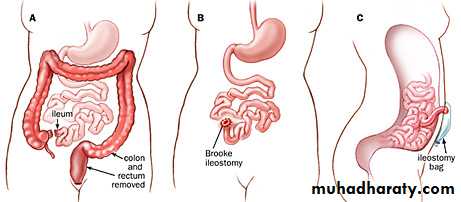
Indications for surgery:
Severe fulminating disease failing to response to medical therapy.
Chronic disease with anemia, frequent stools, urgency and tenesmus.
Steroid dependent disease.
Risk of neoplastic change.
Extra-intestinal manifestations.
Severe hemorrhage or obstruction (stenosis).
Types of operations:
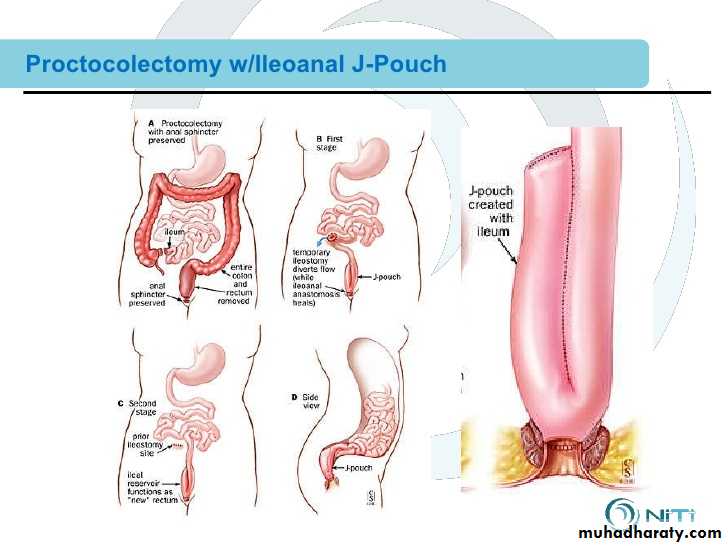
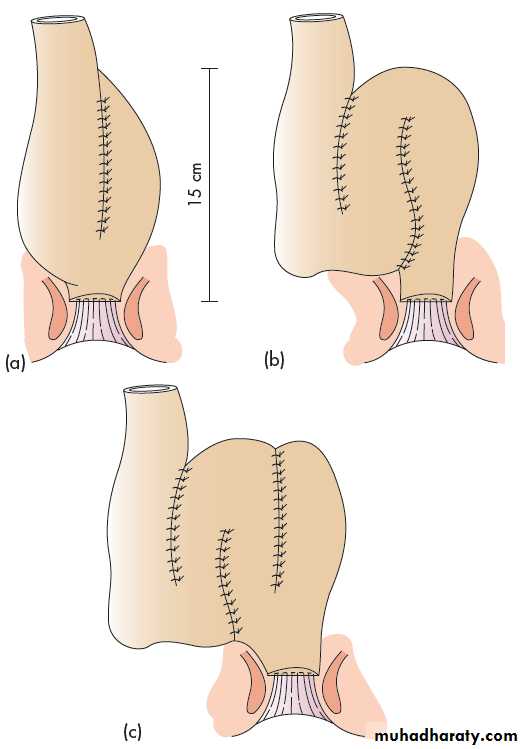
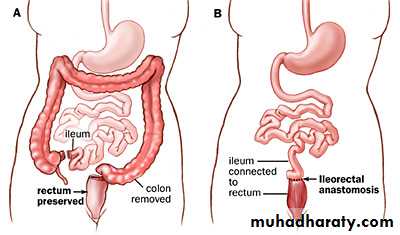
Proctocolectomy and permanent ileostomy.Restorative Procto-colectomy with ileo-anal pouch anastamosis:
‘J’ pouch‘S’ pouch
‘W’ pouch
+ temporary loop protective ileostomy.