• Respiratory System
• Pathology• Lecture no II
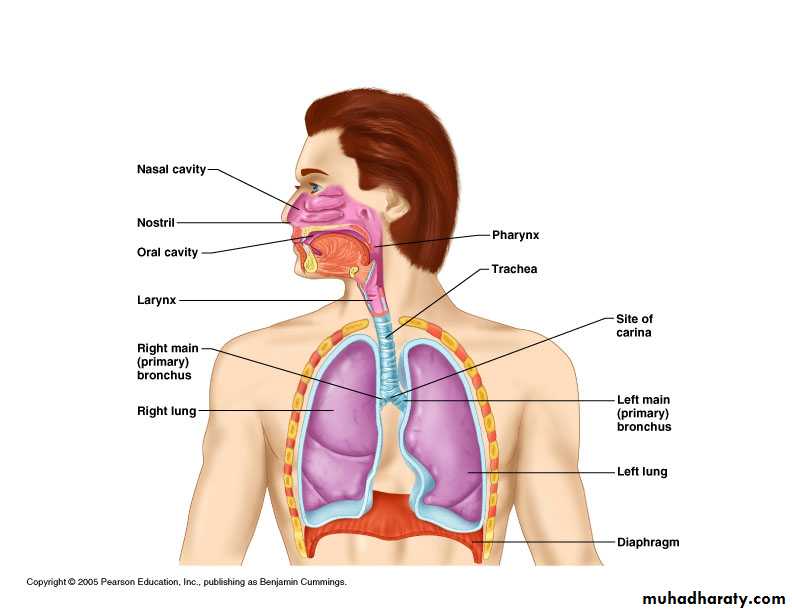
Respiratory Anatomy Review
Conducting airwaysTrachea, bronchi, bronchioles, terminal bronchioles
Acinus- consists of respiratory bronchioles, alveolar ducts, and alveoli
Vasculature
Lungs have dual blood supply: pulmonary and bronchial arteries.
Pulmonary arteries give way to an investing network of capillaries
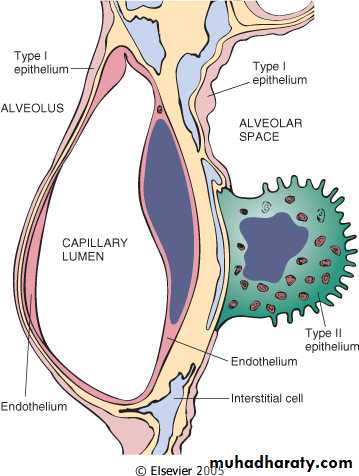
Type I and II pneumocytes
Macrophages
Congenital Anomalies
Conducting airway anomalies: stenosis, atresia, and tracheoesophageal fistulaCan present with dyspnea, infection, failure to thrive
Pulmonary hypoplasia- failure of lungs to fully develop
Caused by oligohydramnios, and reduced fetal respiratory movements (many etiologies )
Pulmonary sequestration
Lung tissue without connection to tracheobronchial tree
Extra and intralobar types
Blood supply is not from PA but from aortic branch
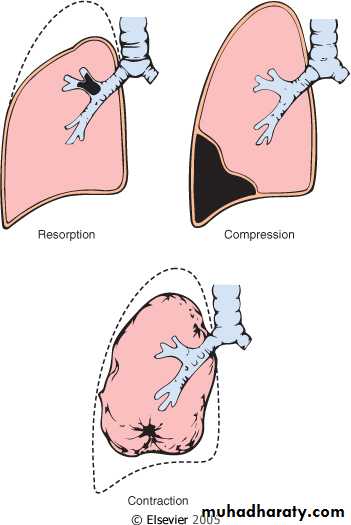
Atelectasis (Lung Collapse)
Atelectasis- collapse of previously inflated lung, producing areas with airless parenchymaThree different types: resorption, compression, and contraction atelectasis
Patients can present with dyspnea, chest pain, loss of conciousness, and cyanosis
Compression atelectasis can cause sudden death and needs to be treated immediately
Resorption Atelectasis
Caused by obstruction of conducting airway (e.g. mucus plugs, foreign bodies, neoplasm )Air in parenchyma distal to obstruction is slowly reabsorbed
, causing mediastinal shift to the site of atelectasis
Compression Atelectasis
Clinically most significantCaused by compression of lung parenchyma by a , liquid( fluid or blood ) , or gas within the pleural space
or elevation of the diaphragm. –ascitis
Pneumothorax
Tension pneumothorax
Hemothorax
Effusion - Cardiac failure
Mediatinal shift away from atelectasis
Contraction Atelectasis
Caused by fibrosis of lung parenchyma preventing expansionChanges can be focal or diffuse
Usually not treatable
Fibrosis can be caused by radiation, infection, toxic injury, or systemic disease
Pulmonary Edema
Two primary etiologies: hemodynamic and microvascular injuryHemodynamic edema- increased vascular hydrostatic pressure or decreased oncotic pressure (Starling forces)
Microvascular injury- increased permeability of capillaries secondary to injury of endo- or epithelial cells
Edema is usually localized, but diffuse edema can occur leading to more serious complications
Grossly the lungs appear boggy, heavy, and have a brown color. Patients present with SOB.
Acute Respiratory Distress Syndrome (ARDS)
ARDS is caused by diffuse damage to the pulmonary capillary vasculature with subsequent sequelae.ARDS is a syndrome caused by a lot of insult from diseases or conditions (infection, trauma, chemical injury, pancreatitis, gas toxicity, etc.)
Usually they are multiple contributing factors to the development of ARDS
The majority of ARDS cases are due to sepsis, pulmonary infections, gastric aspiration, and mechanical trauma
Remember ARDS is a syndrome and not a single disease entity
Acute Respiratory Distress Syndrome (ARDS)
Clinical manifested as• Acute onset of dyspnea no responding to oxygen therapy .
• Decrease arterial oxygen pressure ( hypoxemia )
• Bilateral pulmonary infiltration on chest X ray examination . In the absence of heart failure .
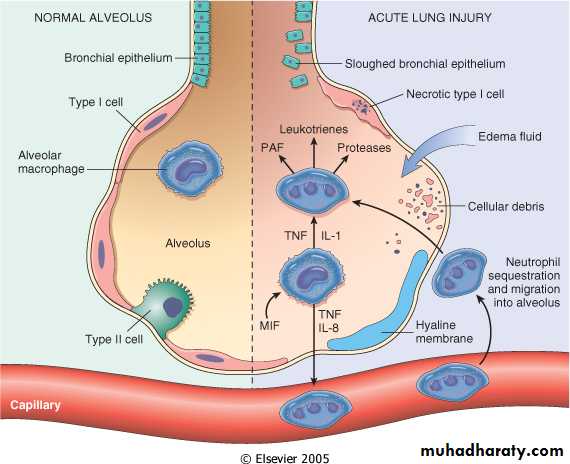
Pathogenesis of ARDS
Capillary damage with increased permeability
Increase in inflammatory proteins
Migration of inflammatory cells (i.e. neutrophils)
End result is diffuse damage to capillaries, alveoli, and terminal bronchioles
ARDS and Diffuse Alveolar Damage
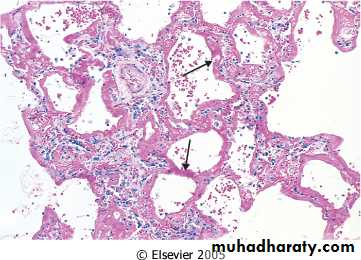
The pathologic correlate to ARDS is Diffuse Alveolar Damage (DAD)Histology shows: hyaline membranes, proteinaceous debris, and desquamated cells
ARDS Outcomes
There are approximately 150,000 cases of ARDS per year with a mortality rate of about 60%.Even in patients that survive ARDS, there are still long term complications. They are scarring, contraction atelectasis, and consolidation. These long term changes are usually focal.
Obstructive and Restrictive Diseases
Obstructive and Restrictive Disease are two large classes of pulmonary disease.Based on pulmonary function and derangement
Obstructive disease- increased resistance to airflow. FEV1 is decreased while FVC is normal ( FEV1 to FVC ratio is decrease)
Restrictive disease- ability of lungs to expand is compromised. Total lung volume is decreased. FVC is decrease and FEV1 decease proportionaly (so the FEV1 to FVC ratio near normal )
In summary Obstructive and Restrictive Pulmonary Diseases
Diffuse pulmonary diseases are divided into:
1. Obstructive disease:
characterized by limitation of airflow owing to partial or complete obstruction at anylevel from trachea to respiratory bronchioles.
Pulmonary function test:
limitation of maximal
airflow rate during forced expiration (FEVI).
2. Restrictive disease: characterized by reduced expansion of lung parenchyma with decreased total lung capacity while the expiratory flow rate is near normal.
Occur in:
1. Chest wall disorder.
2. Acute or chronic, interstitial and infiltrative diseases,
e.g. ARDS and pneumoconiosis.
Obstructive and Restrictive Diseases
Emphysema, chronic bronchitis, bronchiectasis, and asthma are obstructive diseasesRestrictive diseases are wide ranging and are either extrinsic to the lung (e.g. neuromuscular, kyphosis, obesity) or intrisic (e.g. DAD, fibrosis, sarcoidosis )
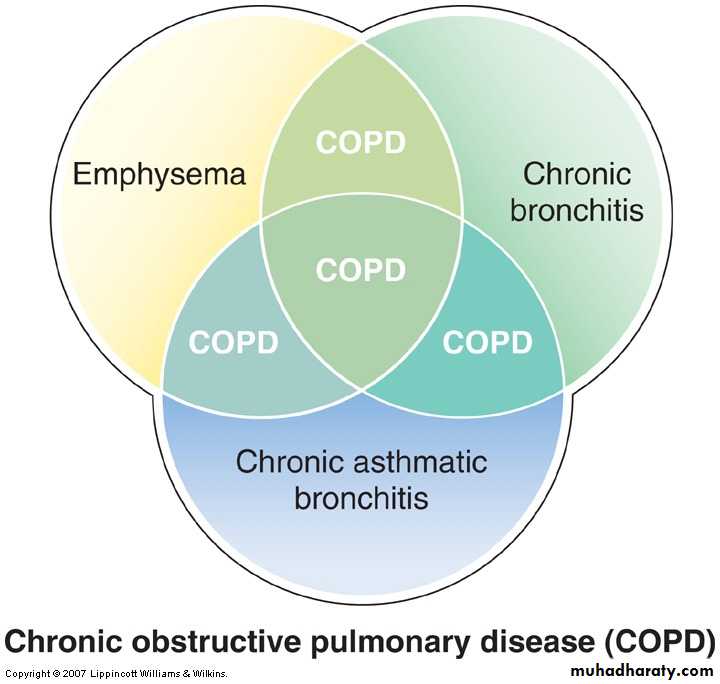
Chronic Obstructive Pulmonary Disease (COPD)
Share a major symptom: dyspnea with chronic or recurrent obstruction to airflow within the lung.
The incidence of COPD has increased dramatically in the past few decades.
Chronic Obstructive Pulmonary Disease (COPD)
Related diseasesChronic bronchial outflow obstruction
Overlapping features
Chronic Obstructive Pulmonary Disease (COPD)
COPD is the clinical term given to those with overlapping emphysema and bronchitisThe vast majority of people with COPD are smokers (90%), and the other 10% have a high exposure rate to second hand smoke or live in an area with increased rates of air pollution
COPD is becoming increasingly prevalent due to the increase in pollution and smoking
COPD is the fourth leading cause of morbidity in the word .