COPD
Lecture IIIEmphysema
Before
AfterEmphysema
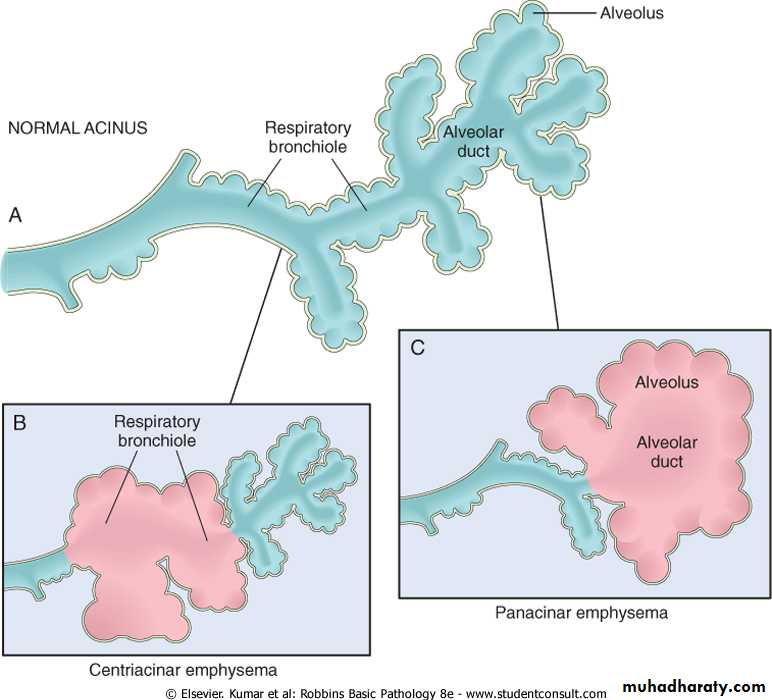
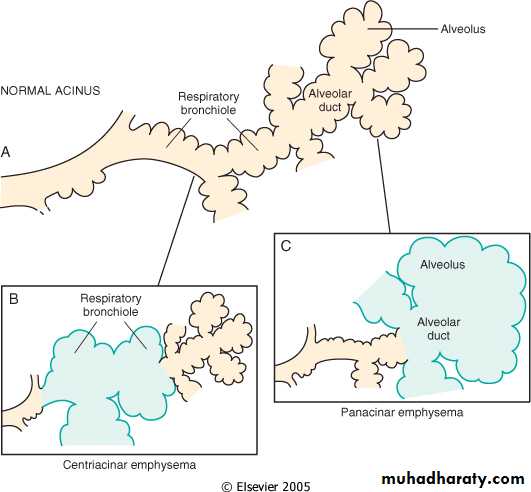
An obstructive lung disease with permanent enlargement of the distal airspaces (i.e. acinar unit) with alveolar septae destructionDestruction of the distal septae and end bronchiole reduce the overall elasticity of the lung
Loss of elasticity reduces expiratory recoil and traps air in the acini
Patients usually present after the age of 50, have severe dyspnea, and on radiograph have hyperinflated lungs. Major symptoms of emphysema appear at the terminal stage of the disease (i.e. cor pulmonale and respiratory insufficiency)
Types of Emphysema
There are four different types of emphysema: centriacinar, panacinar, paraseptal, and irregular.Centriacinar and panacinar are the only two of real clinical significance and make up over 95% of all clinically significant emphysema cases
Paraseptal- distal acinus is affected. Characteristically found in distal portions of lung near pleura and adjacent to fibrosis or scarring. May be the type of emphysema underlying spontaneous pneumothorax
Irregular- named so because acini has variable involvement. Is also associated with scarring. Thought to be the most common form of emphysema, but is “silent” or clinically insignificant
Centriacinar Emphysema
Make up approximately 95% of all clinically significant cases of emphysema. Associated with cigarette smokingCentral portion of acini are affected while distal portions can be unharmed
First seen in upper lobes of the lungs
When severe enough, the whole acini is affected, resembling panacinar emphysema
Panacinar Emphysema
Associated with alpha1 antitrypsin deficiencyThe entire acinus is affected
Most severe in the base of the lungs
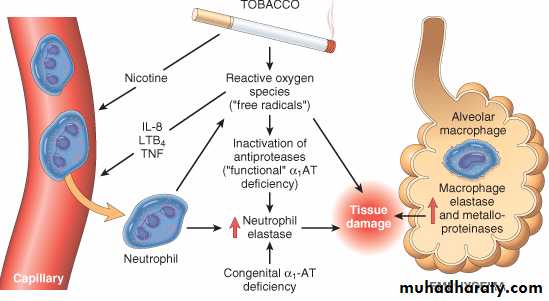
Pathogenesis of Emphysema
Is not completely understood.Alveolar wall destruction and airspace enlargement invokes excess protease or elastase activity unopposed by appropriate antiprotease regulation (protease-antiprotease hypothesis)
2 key mechanisms:
1. excess cellular proteases with low antiprotease level
2. excess ROS from inflammation
-Smokers have accumulation of neutrophils in their alveoli.
-Smoking stimulates release of elastase.-Smoking enhances elastase activity in macrophages, macrophage elastase is not inhibited by 1-antitrypsin.
-Tobaco smoke lead to relase of reactive oxygen species with inactivation of proteases.
Pathogenesis of Emphysema
The protease-antiprotease hypothesis explains the effect of cigarette smoking in the production of centriacinar emphysema.
Emphysema
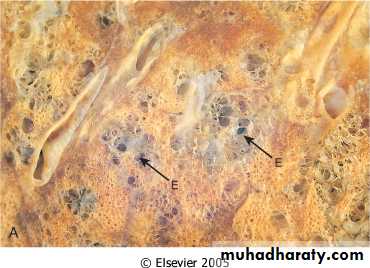
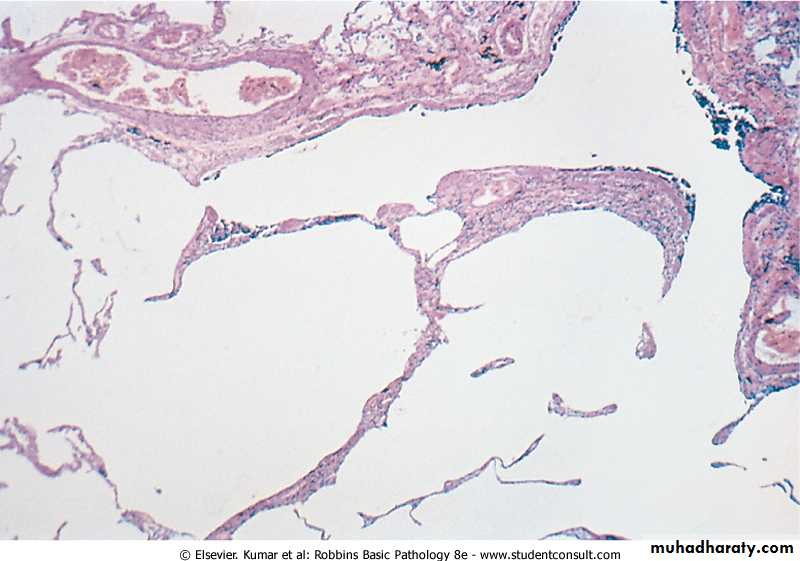
MorphologyThe diagnosis depend largely on the macroscopic appearance of the lung.
The lungs are pale, voluminous.
Histologically, thinning and destruction of alveolar walls creating large airspaces.
Loss of elastic tissue.
Reduced radial traction on the small airways.
Alveolar capillaries is diminished.
Fibrosis of respiratory bronchioles.
Accompanying bronchitis and bronchiolitis.
Clinical Characeristics of Emphysema
• Predominant Emphysema• Age (yr)
• 50-75
• Dyspnea
• Severe; early
• Cough
• Late; scanty sputum
• Infections
• Occasional
• Respiratory insufficiency
• Terminal
• Cor pulmonale
• Rare; terminal
• Airway resistance
• Normal or slightly increased
• Elastic recoil
• Low
• Chest radiograph
• Hyperinflation;
• Appearance
• Pink puffer
-Dyspnea is usually first sign
-Stereotypical patient is barrel
chested, thin, and breathes
through pursed lips
-Death usually comes from
hypercapnia with respiratory
acidosis, right sided heart
failure, or pneumothorax
Gross Picture of Emphysema
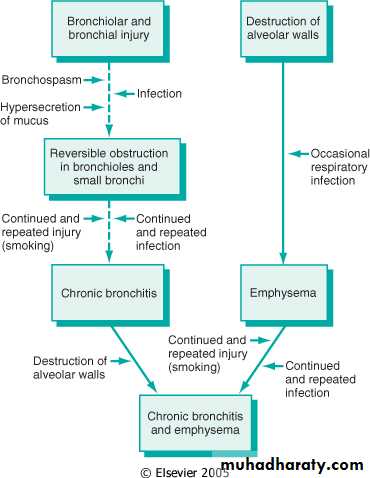
Chronic BronchitisClinically defined disease. Criteria are: persistent cough with sputum production for three months duration in at least two consecutive years
Commonly combined with other obstructive diseases (i.e. asthma and emphysema)
Long term effects are many and serious
COPD
Cor pulmonale
Metaplasia of bronchiole epithelium CANCER
Clinical Characteristics of Bronchitis
• Predominant Bronchitis• Age (yr)
• 40-45
• Dyspnea
• Mild; late
• Cough
• Early; copious sputum
• Infections
• Common
• Respiratory insufficiency
• Repeated
• Cor pulmonale
• Common
• Airway resistance
• Increased
• Elastic recoil
• Normal
• Chest radiograph
• Prominent vessels;
• Appearance
• Blue bloater
Must have cough and sputum production
Smoking is the overwhelming cause
Long standing disease leads to hypercapnia, cyanosis, pulmonary hypertension, cor pulmonale, and heart failure
Very prone to infections of the respiratory tract which further cripple pulmonary function
Pathogenesis of Chronic Bronchitis
Initiating event is inhalation of irritant (e.g. smoke)
Irritation leads to mucus production, hypertrophy of bronchioles, and glandular hypertrophy.
Mediated by epidermal growth factor (EGF)
Changes are also seen in the small airways at an early stage
Infection is a secondary cause that functions in maintaining the bronchitis and exacerbating it
Reid Index > 0.4
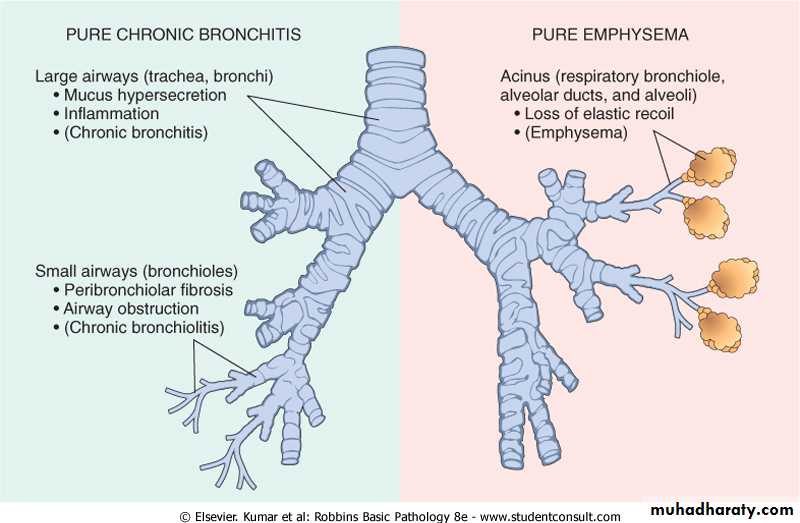
Chronic bronchitis vs. Emphysema
Asthma
Chronic relapsing inflammatory disorder characterized by hyperactive airways leading to episodic, reversible bronchoconstriction owing to increased responsiveness of the tracheobronchial tree to various stimuli.
It has been divided into two basic types:
1. Extrinsic asthma.
2. Intrinsic asthma.
Bronchial asthma
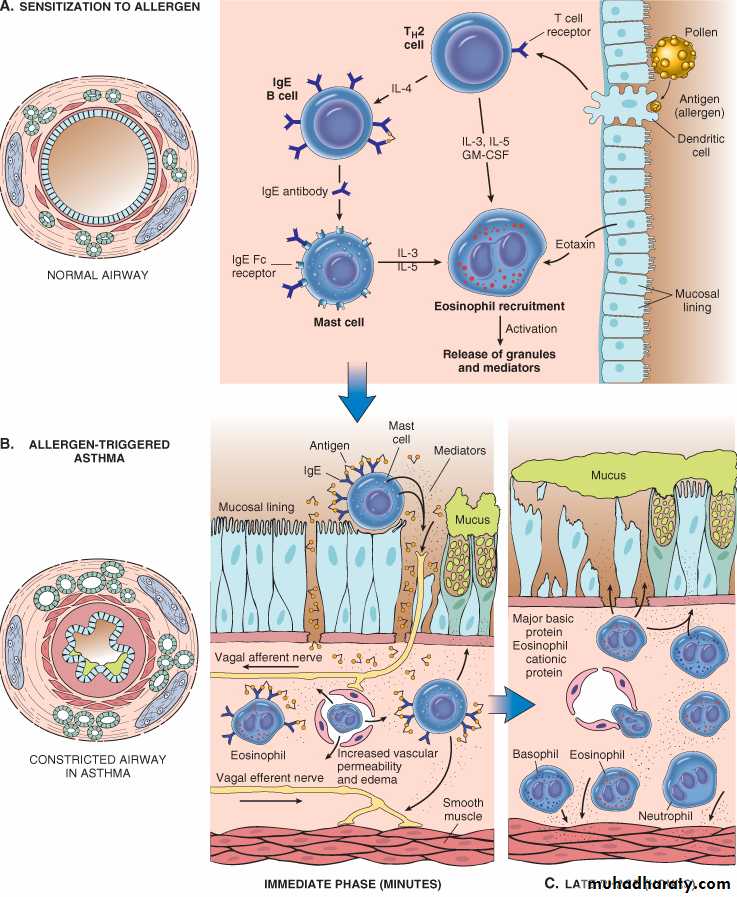
Extrinsic AsthmaInitiated by type 1 hypersensivity reaction induced by exposure to extrinsic antigen.
Subtypes include:
a. atopic (allergic) asthma.
b. occupational asthma.
c. allergic bronchopulmonary aspergillosis.
Develop early in life
Intrinsic Asthma
Initiated by diverse, non-immune mechanisms, including ingestion of aspirin, pulmonary infections, cold, inhaled irritant, stress and exercise.
No personal or family history of allergic reaction.
Develop later in life
CLASSIFICATION OF ASTHMA
Extrinsic Asthma
Atopic (allergic) asthma is the most common form, begins in childhoodOther allergic manifestation: allergic rhinitis, urticaria, eczema.
Skin test with antigen result in an immediate wheel and flare reaction
Other family member is also affected
Serum IgE and eosinophil are increased
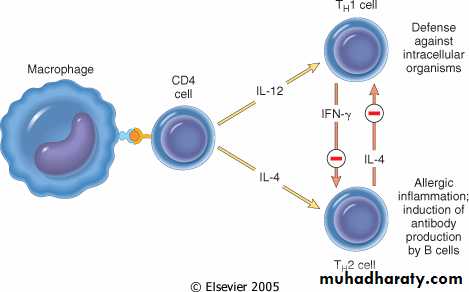
immune related, TH2 subset of CD4+ T cells
Pathogenesis of Bronchial Asthma
EXAGGERATED BROCHOCONTRICTION
Two components:
1. Chronic airway inflammation.
2. Bronchial hyperresponsiveness.
The mechanisms have been best studied in atopic asthma.
Pathogenesis of Atopic Asthma
A classic example of type 1 IgE-mediated hypersensitivity reaction.In the airway – initial sensitization to antigen (allergen) with stimulation of TH2 type T cells and production of cytokines (IL-4, IL- 5, and IL-13).
Cytokines promote:
1. IgE production by B cell.2. Growth of mast cells.
3. Growth and activation of eosinophils.
Non-Atopic Asthma
Triggered by respiratory tract infection including viruses and inhaled air pollutants e.g. sulfur dioxide, ozone.
Positive family history is uncommon.
Serum IgE – normal.
No other associated allergies.
Skin test – negative.
Hyperirritability of bronchial tree.
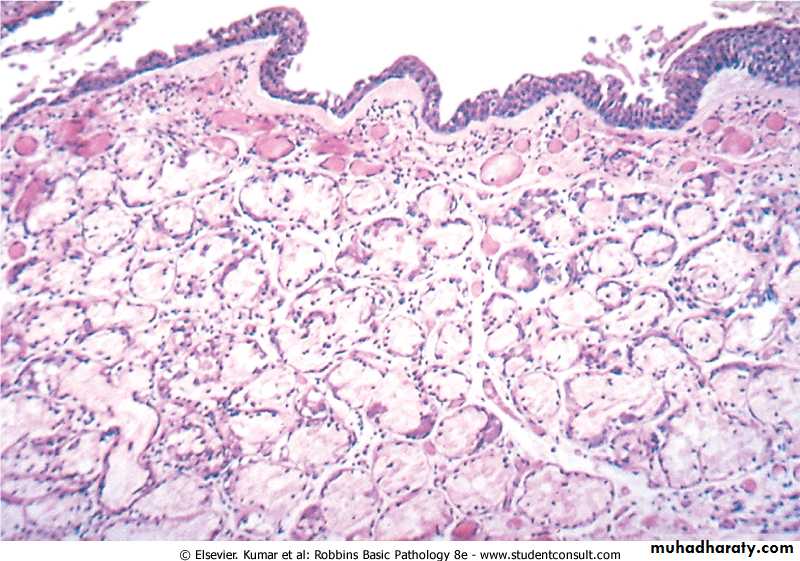
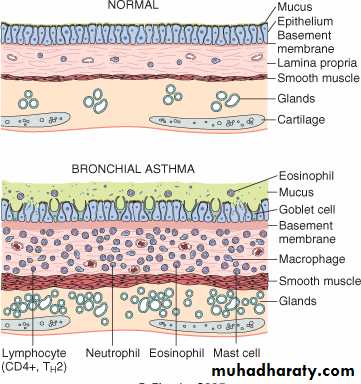
Morphology of Asthma
• Grossly: - lung over distended (over inflation), occlusion of bronchi and bronchioles by thick mucous.• Histologic finding:
• mucous contain Curschmann spirals, eosinophil and Charcot-Leyden crystals.
• Thick BM.
• Edema and inflammatory infiltrate in bronchial wall.
• Submucosal glands increased.
• Hypertrophy of the bronchial wall muscle.
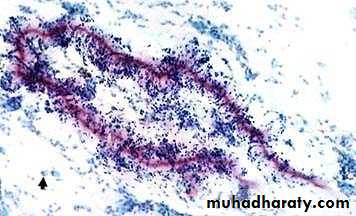
Curschmann spirals
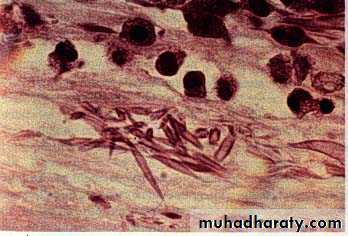
Coiled, basophilic plugs of mucus formed in the lower airways and found in sputum and tracheal washingsCharcot-Leyden crystals.
Eosinophilic needle-shaped crystalline structures.Clinical Coarse
Classic asthmatic attack – dyspnea, cough, difficult expiration, progressive hyperinflation of lung and mucous plug in bronchi. This may resolve spontaneously or with Rx.Status asthmaticus – severe cyanosis and persistent dyspnea, may be fatal.
May progress to emphysema.
Superimposed bacterial infection may occur.
Bronchiectasis
Chronic necrotizing infection of the bronchi and bronchioles leading to or associated with abnormal dilatation of these airways.Bronchial dilatation should be permanent.
Conditions associated with Bronchiectasis
• 1. Bronchial obstruction
• Localized:
• - tumor, foreign bodies or mucous impaction
• Generalized:
• - bronchial asthma
• - chronic bronchitis
• Congenital or hereditary conditions:
• - Congenital bronchiactasis
• - Cystic fibrosis.
• - Intralobar sequestration of the lung.
• - Immunodeficiency status.
• - Immotile cilia and kartagner syndrome.
• Necrotizing pneumonia.
• Caused by TB, staphylococci or mixed infection.
Bronchiectasis
Etiology and pathogenesisObstruction and infection.
Bronchial obstruction (athelectasis of airway distal to obstruction) – bronchial wall inflammation.
These changes become irreversible:
1. If obstruction persist.
2. If there is added infection.
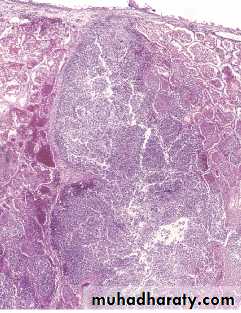
Morphology of Bronchiectasis
Usually affects lower lobes bilaterally (vertical airways).
Dilated airways up to four times of normal, reaching the pleura.
Tube-like enlargement (cylindroid) or fusiform (saccular).
Acute and chronic inflammation, extensive ulceration of lining epithelium with fibrosis.
Bronchiectasis
Bronchiectasis
Clinical course:Sever persistent cough with sputum (mucopurulent, ) sometime with blood.
If sever, obstructive pulmonary function develop.
Rare complications: metastatic brain abscess and amyloidosis.Emphysema:
Dilated air spaces beyond respiratory arteriols
Chronic Bronchitis:
Persistent productive cough for at least 3 consecutive months in at least 2 consecutive years, smoking relatedAsthma: Dyspnea and wheezing
Bronchiectasis:Chronic necrotizing infection of the bronchi
and bronchioles leading to permenant dilatation of these airways