
1
Fifth stage
Medicine
Lec-3
د.بشار
13/11/2016
CNS INFECTIONS
depend on the location of the infection (the meninges or the parenchyma of the brain and
spinal cord), the causative organism (virus, bacterium, fungus or parasite), and whether the
infection is acute or chronic
Meningitis
Acute infection of the meninges presents with a characteristic combination of pyrexia,
headache and meningism.
Meningism consists of headache, photophobia and stiffness of the neck, often accompanied
by other signs of meningeal irritation, including Kernig’s sign (extension at the knee with
the hip joint flexed causes spasm in the hamstring muscles) and Brudzinski’s sign (passive
flexion of the neck causes flexion of the hips and knees
Bacterial meningitis
Many bacteria can cause meningitis but geographical patterns vary, as does age-related
sensitivity
Bacterial causes of meningitis

2
Clinical features
Headache, drowsiness, fever and neck stiffness are the usual presenting features. In severe
bacterial meningitis the patient may be comatose and later there may be focal neurological
signs.
When accompanied by septicaemia, it may present very rapidly, with abrupt onset of
obtundation due to cerebral oedema.
Complications of meningococcal septicaemia
• Meningitis
• Rash (morbilliform, petechial or purpuric)
• Shock
• Intravascular coagulation
• Renal failure
• Peripheral gangrene
• Arthritis (septic or reactive)
• Pericarditis (septic or reactive
In pneumococcal and Haemophilus infections there may be an associated otitis media.
Pneumococcal meningitis may be associated with pneumonia and occurs especially in older
patients and alcoholics as well as those without functioning spleens
Listeria monocytogenes is an increasing cause of meningitis and brainstem encephalitis in
the immunosuppressed, people with diabetes, alcoholics and pregnant women
Investigations
Lumbar puncture is mandatory unless there are contraindications
If the patient is drowsy and has focal neurological signs or seizures, is immunosuppressed,
has undergone recent neurosurgery or has suffered a head injury, it is wise to obtain a CT to
exclude a mass lesion (such as a cerebral abscess) before lumbar puncture because of the
risk of coning.
This should not, however, delay treatment of a presumptive meningitis.
If lumbar puncture is deferred or omitted, it is essential to take blood cultures and to start
empirical treatment
3
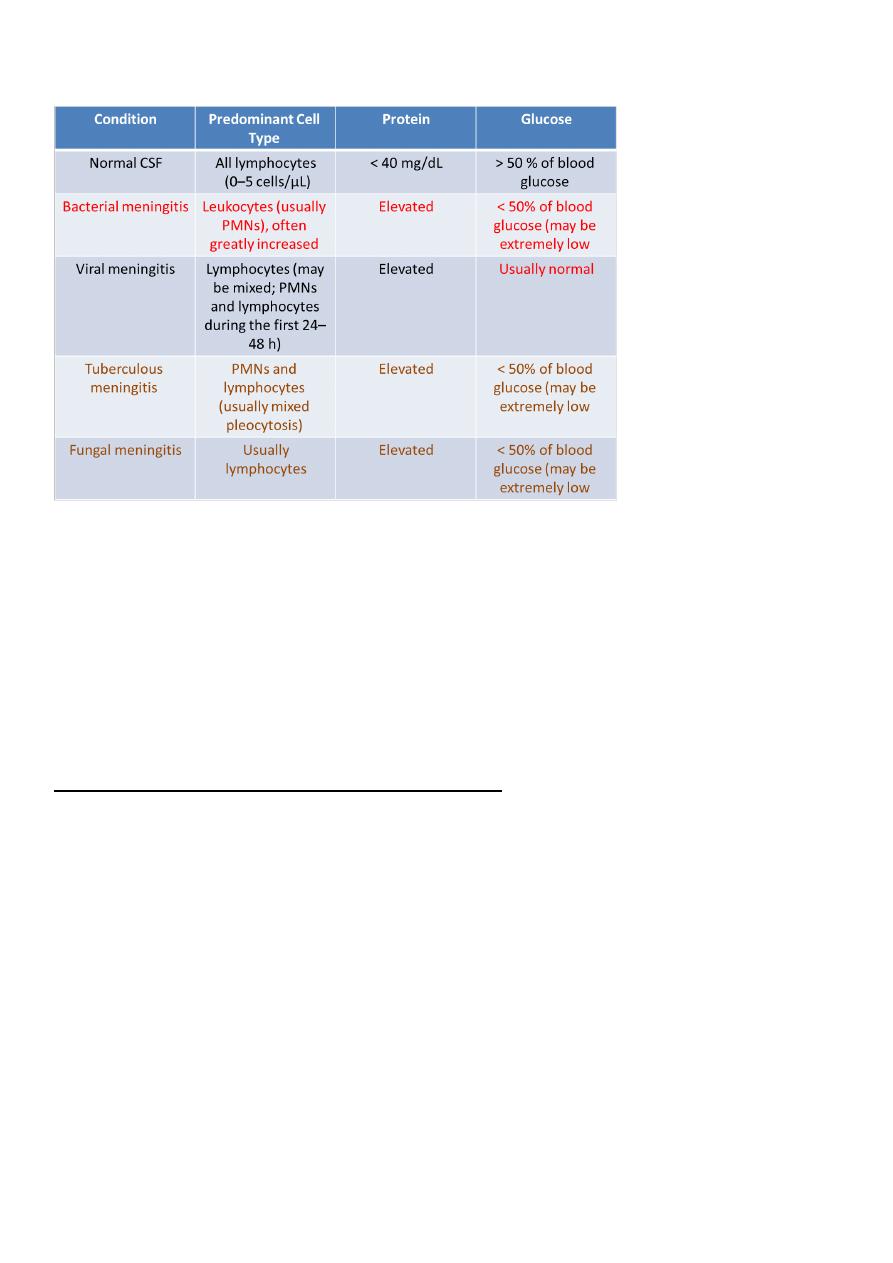
CSF Findings in Meningitis
Management
There is an untreated mortality rate of around 80%, so action must be swift.
If bacterial meningitis is suspected, the patient should be given parenteral benzylpenicillin
immediately (intravenous is preferable) and prompt hospital admission should be arranged.
The only contraindication is a history of penicillin anaphylaxis.
Treatment of pyogenic meningitis of unknown cause
1. Adults aged 18–50 yrs with or without a typical meningococcal rash
• Cefotaxime 2 g IV 4 times daily or
• Ceftriaxone 2 g IV twice daily
2. Patients in whom penicillin-resistant pneumococcal infection is suspected, or in areas
with a significant incidence of penicillin resistance in the community
As for (1) but add:
• Vancomycin 1 g IV twice daily or
• Rifampicin 600 mg IV twice daily

4
3. Adults aged > 50 yrs and those in whom Listeria monocytogenes infection is suspected
(brainstem signs, immunosuppression, diabetic, alcoholic)
As for (1) but add:
• Ampicillin 2 g IV 6 times daily or
• Co-trimoxazole 50 mg/kg IV daily in two divided doses
4. Patients with a clear history of anaphylaxis to β-lactams
• Chloramphenicol 25 mg/kg IV 4 times daily plus
• Vancomycin 1 g IV twice daily
5. Adjunctive treatment
• Dexamethasone 0.15 mg/kg 4 times daily for 2–4 days
• Corticosteroids significantly reduce hearing loss and neurological sequelae, but do not
reduce overall mortality
Chemotherapy of bacterial meningitis when the cause is known

5
Adverse prognostic features include
• hypotensive shock,
• a rapidly developing rash,
• a haemorrhagic diathesis,
• multisystem failure
• and age over 60 years.
Prevention of meningococcal infection
Close contacts of patients with meningococcal infection should be given 2 days of oral
rifampicin.
In adults, a single dose of ciprofloxacin is an alternative.
If not treated with ceftriaxone, the index case should be given similar treatment to clear
infection from the nasopharynx before hospital discharge.
Vaccines are available for most meningococcal subgroups but not group B, which is among
the most common serogroup isolated in many countries.
Tuberculous meningitis
Tuberculous meningitis most commonly occurs shortly after a primary infection in
childhood or as part of miliary tuberculosis
Clinical features of tuberculous meningitis

6
Onset is much slower than in other bacterial meningitis over 2–8 weeks.
If untreated, it is fatal in a few weeks but complete recovery is usual if treatment is started
early.
When treatment is initiated later, the rate of death or serious neurological deficit may be as
high as 30%.
The tubercle bacillus may be detected in a smear of the centrifuged deposit from the CSF
but a negative result does not exclude the diagnosis.
The CSF should be cultured but, as this result will not be known for up to 6 weeks,
treatment must be started without waiting for confirmation.
Brain imaging may show hydrocephalus, brisk meningeal enhancement on enhanced CT or
MRI, and/or an intracranial tuberculoma.
Management
As soon as the diagnosis is made or strongly suspected, chemotherapy should be started
using one of the regimens that include pyrazinamide.
The use of corticosteroids in addition to anti-tuberculous therapy has been controversial.
Recent evidence suggests that it improves mortality, especially if given early, but not focal
neurological damage.
Surgical ventricular drainage may be needed if obstructive hydrocephalus develops.
Viral meningitis
Viruses are the most common cause of meningitis, usually resulting in a benign and self-
limiting illness requiring no specific therapy.
A number of viruses can cause meningitis, the most common being enteroviruses.
Clinical features
Viral meningitis occurs mainly in children or young adults, with acute onset of headache
and irritability and the rapid development of meningism. The headache is usually the most
severe feature. There may be a high pyrexia but focal neurological signs are rare.
The diagnosis is made by lumbar puncture.

7
Management
There is no specific treatment and the condition is usually benign and self-limiting.
The patient should be treated symptomatically in a quiet environment. Recovery usually
occurs within days
Viral encephalitis
Clinical features
Viral encephalitis presents with acute onset of headache, fever, focal neurological signs
(aphasia and/or hemiplegia, visual field defects) and seizures. Disturbance of consciousness
ranging from drowsiness to deep coma supervenes early and may advance dramatically.
Meningism occurs in many patients.
Investigations
Imaging by CT scan may show low-density lesions in the temporal lobes but MRI is more
sensitive in detecting early abnormalities.
Lumbar puncture should be performed once imaging has excluded a mass lesion. The CSF
usually contains excess lymphocytes but polymorphonuclear cells may predominate in the
early stages. The CSF may be normal in up to 10% of cases.
Some viruses, including the West Nile virus, may cause a sustained neutrophilic CSF. The
protein content may be elevated but the glucose is normal.
The EEG is usually abnormal in the early stages, especially in herpes simplex encephalitis,
with characteristic periodic slow-wave activity in the temporal lobes.
Virological investigations of the CSF, including PCR for viral DNA, may reveal the causative
organism but treatment initiation should not await this.
Management
Optimum treatment for herpes simplex encephalitis (aciclovir 10 mg/kg IV 3 times daily for
2–3 weeks) hasreduced mortality from 70% to around 10%. This should be given early to all
patients suspected of suffering from viral encephalitis.

8
Some survivors will have residual epilepsy or cognitive impairment.
Anticonvulsant treatment may be needed and raised intracranial pressure may indicate the
need for dexamethasone.
Cerebral abscess
Bacteria may enter the cerebral substance through penetrating injury, by direct spread
from paranasal sinuses or the middle ear, or secondary to septicaemia. The site of abscess
formation and the likely causative organism are both related to the source of infection.
Initial infection leads to local suppuration followed by loculation of pus within a
surrounding wall of gliosis, which in a chronic abscess may form a tough capsule.
Haematogenous spread may lead to multiple abscesses.
Clinical features
A cerebral abscess may present acutely with fever, headache, meningism and drowsiness,
but more commonly presents over days or weeks as a cerebral mass lesion with little or no
evidence of infection.
Seizures, raised intracranial pressure and focal hemisphere signs occur alone or in
combination. Distinction from a cerebral tumour may be impossible on clinical grounds.
Investigations
Lumbar puncture is potentially hazardous in the presence of raised intracranial pressure
and CT should always precede it.
CT reveals single or multiple lowdensity areas, which show ring enhancement with contrast
and surrounding cerebral oedema.
There may be an elevated white blood cell count and ESR in patients with active local
infection.

9
Management and prognosis
Antimicrobial therapy is indicated once the diagnosis is made. The likely source of infection
should guide the choice of antibiotic.
Surgical drainage by burr-hole aspiration or excision may be necessary, especially where the
presence of a capsule may lead to a persistent focus of infection.
Epilepsy frequently develops and is often resistant to treatment.
Despite advances in therapy, the mortality rate remains at 10–20% and this may partly
relate to delay in diagnosis and initiation of treatment.
Transmissible spongiform encephalopathies
Include a number of veterinary and medical conditions that are characterised by the
histopathological triad of cortical spongiform change, neuronal cell loss and gliosis.
Associated with these changes, there is deposition of amyloid made up of an altered form
of a normally occurring protein, the prion protein.
Creutzfeldt–Jakob disease
Variant Creutzfeldt–Jakob disease
Gerstmann–Sträussler–Scheinker disease, fatal familial insomnia and kuru
