~1
~
Third Stage Internal Medicine Dr. Fadhil
Clinical Immunology 3
Inflammation & The Inflammatory Response
Inflammation is the response of living tissue to damage.
Types of inflammation:
• -Acute inflammation
• -chronic inflammation
The cause of acute inflammation may be due to physical damage, chemical substances,
micro-organisms or other agents.
Acute inflammation is short-lasting, lasting only a few days. If it is longer lasting however,
then it is referred to as chronic inflammation. Various examples of acute inflammation such
as sore throat, reactions in the skin to a scratch or a burn or insect bite, and acute hepatitis.
The Inflammatory Response
3 Steps:
1. Tissue damage = release of chemical signals~
– Mast cells release chemicals known as Histamine & Prostaglandins that trigger
inflammation
2. Vessels dilation increases permeability of capillaries~
– Increased blood flow; leukocytes leak out to infected area
– Delivery of clotting factors & antimicrobial proteins
3. Phagocytosis of pathogens~
– WBC’s engulf microbes or damaged tissue
– Fever: leukocyte-released chemicals increase body temperature
The inflammatory response consist of changes in blood flow, increased permeability of
blood vessels and escape of cells from the blood into the tissues. The changes are essentially the
same whatever the cause and wherever the site.
The inflammatory response cont.
• Immediate, early response
Vasodilation
Vascular permeability
~2
~
Emigration of leukocytes into tissues
• Reactions of leukocytes in inflammation
Recognition of microbes and dead tissues
Removal of the offending agents
Macrophage activation
Leukocyte-mediated tissue injury
CLINICAL FEATURES OF ACUTE INFLAMMATION
1-skin--flushing, fever, sweating, swelling
2-CNS--headache, confusion, anorexia
3-respiratory--Increased respiratory rate, hypoxia
4-heart--Tachycardia, hypotension, flow murmur
5-endocrine—Release of catecholamine, glucocorticoid hormones& insulin from pancreas.
6-LNs- enlarged lymph nodes, lymphocytosis
7-Bone marrow- Increased production of neutrophils and macrophages.
Cardinal signs of acute inflammation
Celsus described the local reaction of injury in terms that have come to be known as the
cardinal signs of inflammation.
These signs are:
rubor (redness)
tumor (swelling)
calor (heat)
dolor (pain)
functio laesa, or loss of function (In the second century AD, the Greek physician Galen
added this fifth cardinal sign)
Briefly, the steps involved in the acute inflammatory response are:
1. Small blood vessels adjacent to the area of tissue damage initially become dilated
with increased blood flow, then flow along them slows down.
2. Endothelial cells swell and partially retract so that they no longer form a
completely intact internal lining.
3. The vessels become leaky, permitting the passage of water, salts, and some small
proteins from the plasma into the damaged area (exudation). One of the main
proteins to leak out is the small soluble molecule, fibrinogen.
~3
~
4. Circulating polymorphs neutrophil initially adhere to the swollen endothelial cells
(margination), then actively migrate through the vessel basement membrane
(emigration), passing into the area of tissue damage
5. Later, small numbers of blood monocytes (macrophages) migrate in a similar way,
as do Iymphocytes.
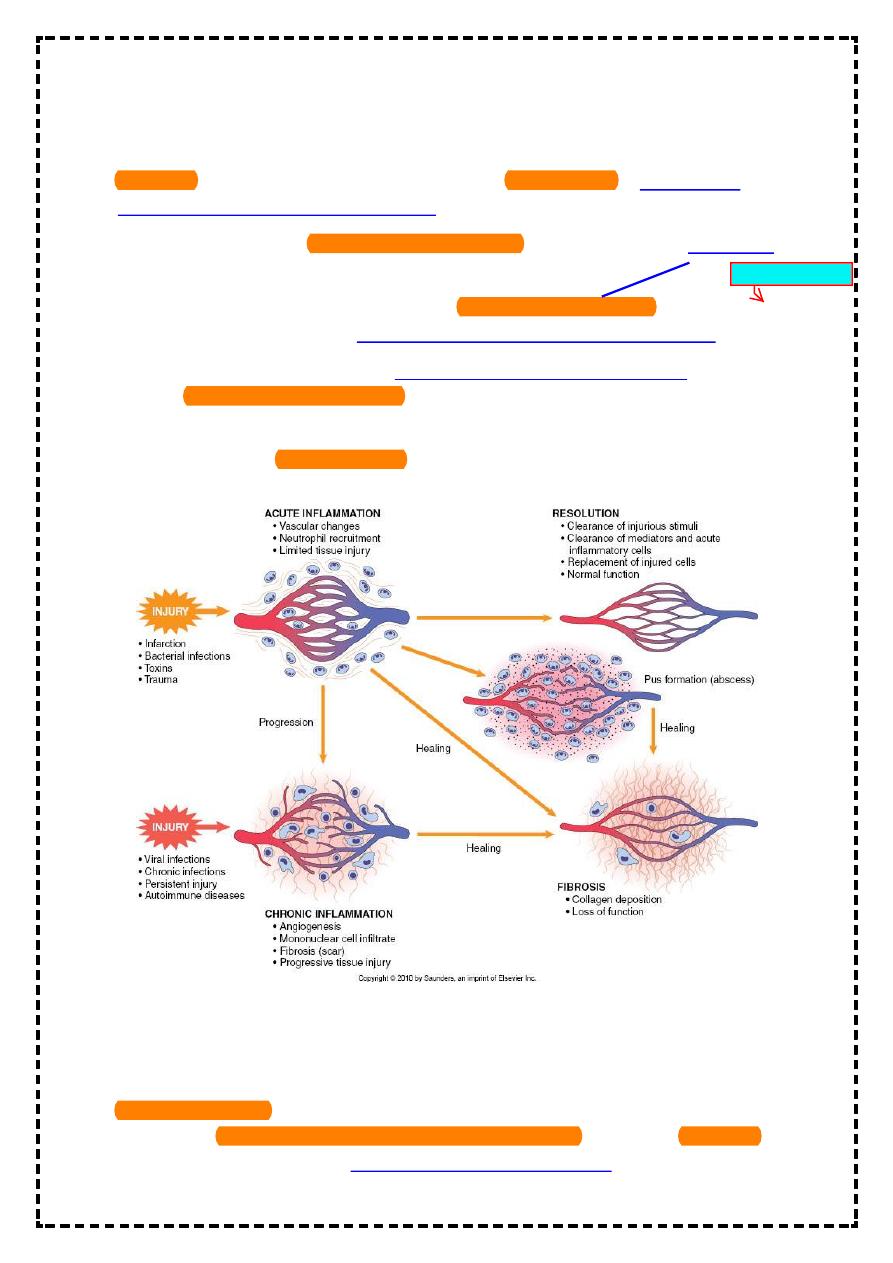
Resolution of inflammatory response is crucial for normal healing.
This involves active down-modulation of inflammatory stimuli &repair of the damage to nearby
local tissues.
• Extravasated neutrophils undergo apoptosis& phagocytosed by macrophages together
with microorganism.
• Macrophages also synthesizes collagenase &elastase which breakdown local connective
tissue & aid in the removal of debris.
• Macrophages derived cytokines &platetate derived growth factors attract fibroblasts
&promote the synthesis of new collagen, while angiogenic factors stimulate new vessel
formation.
Sepsis and septic shock
• Septic shock is the clinical manifestation of overwhelming inflammation.
• Failure of normal inhibitory mechanisms results in excessive production of pro-
inflammatory cytokines by macrophages.
• This result in hypotension, hypovolemia, hypoperfusion& tissue edema.
• Uncontrolled neutrophil activation causes the release of proteases and oxygen free
radicals within blood vessels.
• Direct activation of the coagulation pathway combines with endothelial cell disruption to
form clots within the damaged vessels.
• This is what we call disseminated intravascular coagulation(DIC) which considered a
medical emergency.
• The clinical consequences include cardiovascular collapse, acute respiratory distress
syndrome, multiorgan failure and often death.
• Septic Shock: Most frequently results from infection with Gram-negative bacteria
because lipopolysaccharide is particularly effective at activating the inflammatory
cascade.
Chronic Inflammation
• Failure to remove an inflammatory stimulus results in chronic inflammation.
• In other word, chronic inflammation can be defined as inflammation which continue past
1 month
~4
~
• Marked by
-a loss of function
- Fibroblast activity continues forming granuloma
• Persisting microorganisms stimulate the ongoing accumulation of neutrophils,
macrophages& activated T-lymphocytes.
• If this is associated with local deposition of fibrous connective tissues, a granuloma may
form.
This is a characteristic of infections such as tuberculosis and leprosy, in which the M.O. is
protected by a cell wall which shields it from killing, inspite of phagocytosis.
• In most cases, the development of active immune response is beneficial to the host&
result in either clearance or control of infection with minimal local damage.
• However ,vigorous or prolonged immune response may cause significant tissue damage.
These are known as hypersensitivity reactions & may involve either antibody or cell-
mediated responses.
INVESTIGATIONS
Leukocytosis is common. Platetate count may be increased. Chronic inflammation
is commonly associated with normochromic normocytic anemia.
• C-Reactive Protein ( CRP ) is the most widely used clinical measure of acute inflammation,
but levels of fibrinogen, ferritin &complement component may also be increased as part
of the acute phase response, while albumin levels are reduced.
Microorganism
~5
~
• CRP is an acute phase reactant which opsonizes invading pathogens. Levels of CRP
increase within 6-houres of an inflammatory stimulus & may rise up to 1000 folds.
• Plasma half life of CRP is 19 hours, so levels fall in just few days once the stimulus is
removed.
• In contrast to CRP, the ESR is an indirect measure of the acute phase response. It
measures the rate of fall of erythrocytes through plasma, causing aggregation of red cells.
• Abnormal red cell morphology can make rouleoux formation impossible.
• For these reasons, inappropriately low ESR occurs in spherocytosis, sickle cell anemia&
microcytic anemia.
IMAGING TECHNIQUES
• A chest-x ray and abdominal CT-scan may identify the source of unknown infection or
malignancy.
• Abdominal or pelvic ultrasound may identify hepatic lesions, abdominal nodes and local
abdominal or pelvic abscesses.
• An MRI scan is more appropriate for the diagnoses of soft tissue or bone/joint infections.
• Echocardiography is used to look for vegetation & assess valve function in suspected
bacterial endocarditis. White cell scans are rarely indicated, but may be useful in
identification of the site of pyogenic infections.
• An isotope scan may identify the evidence of malignancy or bone infection.
Familial Mediterranean Fever(FMF)
• This is the most common of the familial periodic fevers, predominantly affecting
Mediterranean people, including Arabs, Turks, Sephardic Jews and Armenians.
• It results from mutation of the pyrine gene, which is thought to regulate neutrophils-
mediated inflammation.
• FMF is characterized by painful attacks of fever associated with peritonitis , pleuritis and
arthritis. It lasts from a few hours to four days.
• During acute episodes CRP levels are markedly increased.
• The majority of individuals have their first attack before the age of 20. The major
complication of FMF is AA amyloidosis.
• Colchicine significantly reduces the number of febrile episodes in 90% of patients, but
does not stop an established attack.
