1
Lecture 5
Pathogenesis of Viral Diseases
Steps in Viral Pathogenesis
.
1- Entry and Primary Replication
Virus must first attach to and enter cells of one of the body surfaces—skin, respiratory
tract, gastrointestinal tract, urogenital tract, or conjunctiva. Most viruses enter their hosts
through the mucosa of the respiratory or gastrointestinal tract (Table 30–2). Major
exceptions are those viruses that are introduced directly into the bloodstream by needles
(hepatitis B, human immunodeficiency virus [HIV]), by blood transfusions, or by insect
vectors (arboviruses).
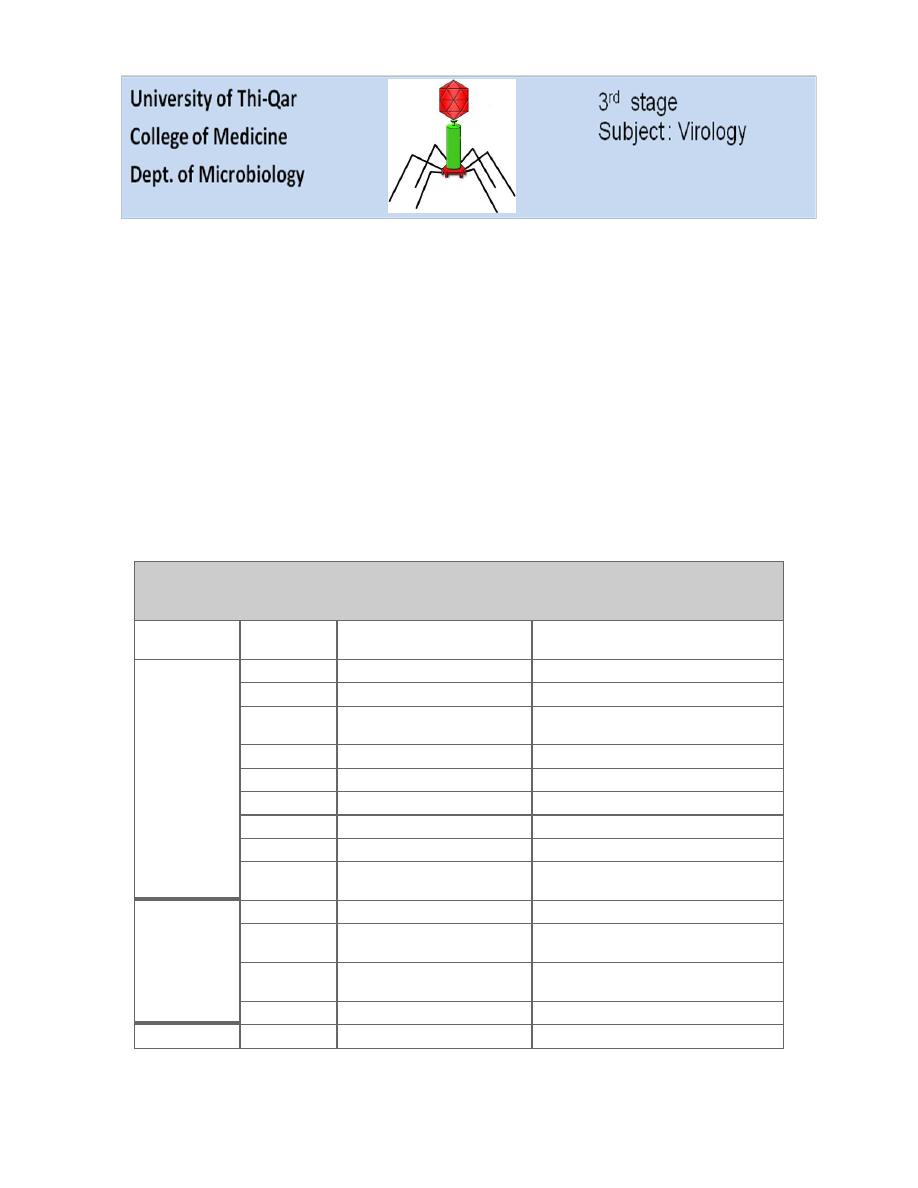
Table 30–2. Common Routes of Viral Infection in Humans.
Route of Entry
Virus Group
Produce Local Symptoms at
Portal of Entry
Produce
Generalized
Infection
Plus
Specific Organ Disease
Respiratory tract Parvovirus
B19
Adenovirus
Most types
Herpesvirus
Epstein-Barr
virus,
herpes
simplex virus
Varicella virus
Poxvirus
Smallpox virus
Picornavirus
Rhinoviruses
Some enteroviruses
Togavirus
Rubella virus
Coronavirus
Most types
Orthomyxovirus Influenza virus
Paramyxovirus Parainfluenza viruses, respiratory
syncytial virus
Mumps virus, measles virus
Mouth, intestinal
tract
Adenovirus
Some types
Herpesvirus
Epstein-Barr
virus,
herpes
simplex virus
Cytomegalovirus
Picornavirus
Some enteroviruses, including poliovirus
and hepatitis A virus
Reovirus
Rotaviruses
Skin
2
Mild trauma
Papillomavirus Most types
Herpesvirus
Herpes simplex virus
Poxvirus
Molluscum contagiosum virus, orf
virus
Injection
Hepadnavirus
Hepatitis B
Herpesvirus
Epstein-Barr virus, cytomegalovirus
Retrovirus
Human immunodeficiency virus
Bites
Togavirus
Many species, including eastern equine
encephalitis virus
Flavivirus
Many species, including yellow fever virus
Rhabdovirus
Rabies virus
Viruses usually replicate at the primary site of entry. Some, such as influenza viruses
(respiratory infections) and rotaviruses (gastrointestinal infections), produce disease at
the portal of entry and have no necessity for further systemic spread. They spread locally
over the epithelial surfaces, but there is no invasion of underlying tissues or spread to
distant sites.
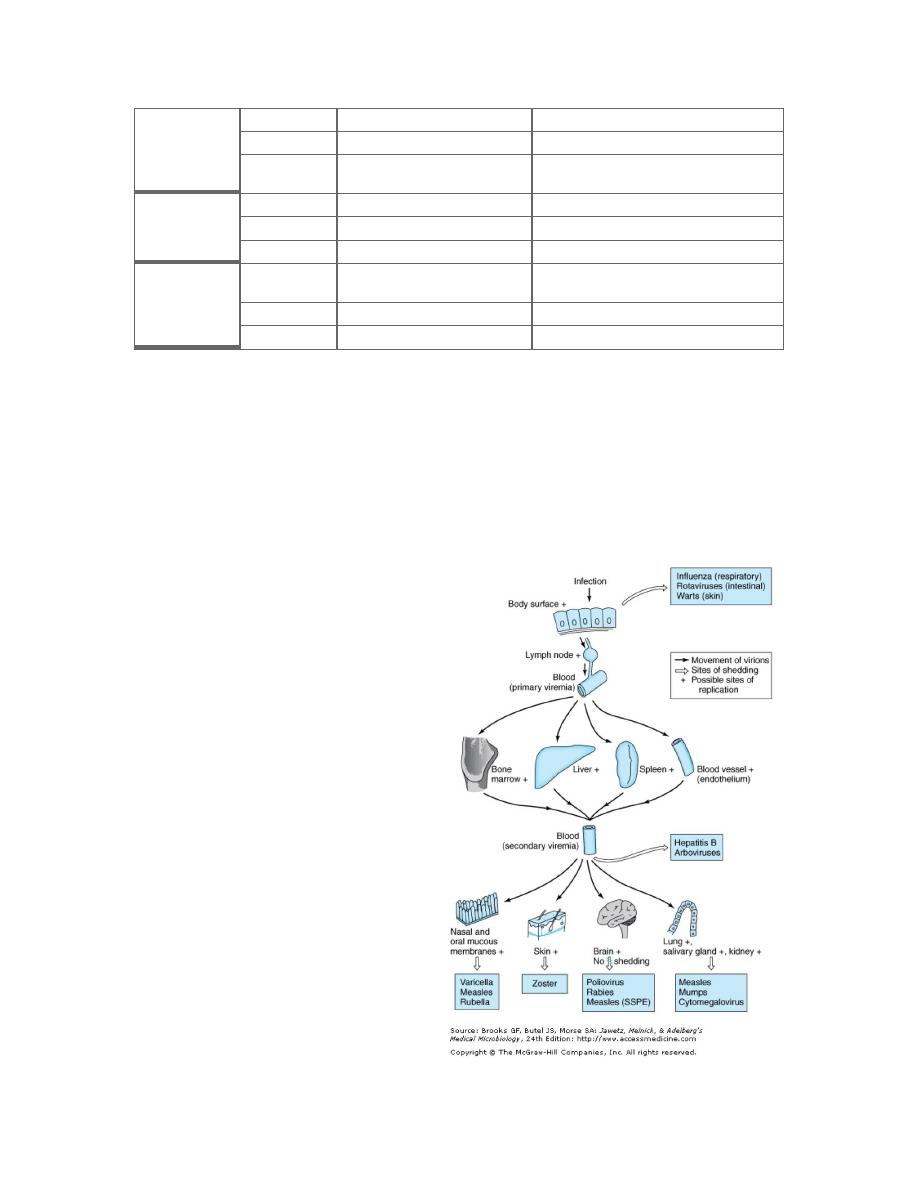
2- Viral Spread and Cell Tropism
Many viruses produce disease at sites
distant from their point of entry (e.g.,
enteroviruses, which enter through the
gastrointestinal tract but may produce
central nervous system disease). After
primary replication at the site of entry,
these viruses then spread within the host.
Viremia: the presence of virus in the
blood. Virions may be free in the plasma
(e.g., enteroviruses, togaviruses) or
associated with particular cell types
(e.g., measles virus) (Table 30–3). The
viremic phase is short in many viral
infections. In some instances, neuronal
spread is involved; this is apparently
how rabies virus reaches the brain to
cause disease and how herpes simplex
virus moves to the ganglia to initiate
latent infections.
3
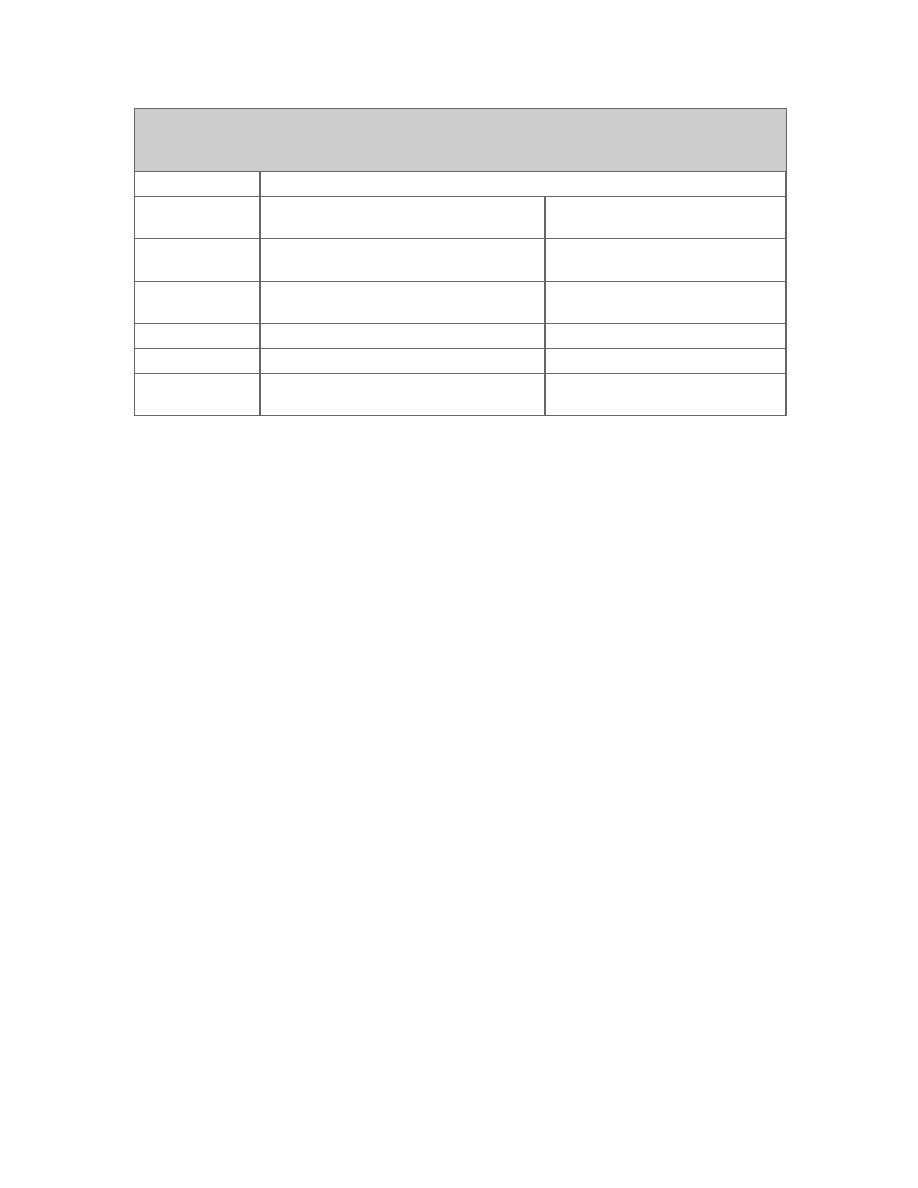
Table 30–3. Viruses Spread Via the Bloodstream.
1
Examples
Cell
Type
Associated
DNA Viruses
RNA Viruses
Lymphocytes
Epstein-Barr virus, cytomegalovirus, hepatitis
B virus, JC virus, BK virus
Mumps, measles, rubella, human
immunodeficiency virus
Monocytes-
macrophages
Cytomegalovirus
Poliovirus, human immunodeficiency
virus, measles virus
Neutrophils
Influenza virus
Red blood cells
Parvovirus B19
Colorado tick fever virus
None
(free
in
plasma)
Togavirus, picornavirus
Viruses tend to exhibit organ and cell specificities. Thus, tropism determines the pattern
of systemic illness produced during a viral infection. As an example, hepatitis B virus has
a tropism for liver hepatocytes, reflect the presence of specific cell surface receptors for
that virus.
Factors affecting viral gene expression are important determinants of cell tropism. (The
JC polyomavirus enhancer is much more active in glial cells than in other cell types).
Proteolytic enzymes: Certain paramyxoviruses are not infectious until an envelope
glycoprotein undergoes proteolytic cleavage. Multiple rounds of viral replication will not
occur in tissues that do not express the appropriate activating enzymes.
Viral spread may be determined in part by specific viral genes (reovirus have spread from
the gastrointestinal tract is determined by one of the outer capsid proteins).
3- Cell Injury and Clinical Illness
Destruction of virus-infected cells in the target tissues and physiologic alterations
produced in the host by the tissue injury are partly responsible for the development of
disease. Some tissues, such as intestinal epithelium, can rapidly regenerate and withstand
extensive damage better than others, such as the brain. General symptoms associated with
many viral infections, such as malaise and anorexia, may result from host response
functions such as cytokine production.
4- Recovery from Infection
The host either succumbs or recovers from viral infection. Recovery mechanisms include
both innate and adaptive immune responses. Interferon and other cytokines production,
humoral and cell-mediated immunity, and possibly other host defense factors are

4
involved. The relative importance of each component differs with the virus and the
disease.
In acute infections, recovery is associated with viral clearance. However, there are times
when the host remains persistently infected with the virus.
5- Virus Shedding
The last stage in pathogenesis is the shedding of infectious virus into the environment.
This is a necessary step to maintain a viral infection in populations of hosts. Shedding
usually occurs from the body surfaces involved in viral entry. Shedding occurs at
different stages of disease depending on the particular agent involved. In some viral
infections, such as rabies, humans represent dead-end infections, and shedding does not
occur.
Viral Persistence: Chronic & Latent Virus Infections
Viral infections are usually self-limiting. Long-term virus-host interaction may take
several forms.
Chronic infections are those in which replicating virus can be continuously
detected, often at low levels; mild or no clinical symptoms may be evident.
Latent infections are those in which the virus persists in an occult (hidden or
cryptic) form most of the time. Viral sequences may be detectable by molecular
techniques in tissues harboring latent infections.
Inapparent or subclinical infections are those that give no overt sign of their
presence.
Chronic infections depend upon the age of the host when infected. In humans, for
example, rubella virus and cytomegalovirus infections acquired in utero characteristically
result in viral persistence that is of limited duration, probably because of development of
the immunologic capacity to react to the infection as the infant matures. Infants infected
with hepatitis B virus frequently become persistently infected (chronic carriers); most
carriers are asymptomatic. In chronic infections with RNA viruses, the viral population
often undergoes many genetic and antigenic changes.
Herpesviruses typically produce latent infections. Herpes simplex viruses enter the
sensory ganglia and persist in a noninfectious state (Figure 30–4). There may be periodic
reactivations during which lesions containing infectious virus appear at peripheral sites
(eg, fever blisters).
Chickenpox virus (varicella-zoster) also becomes latent in sensory ganglia. Recurrences
are rare and occur years later, usually following the distribution of a peripheral nerve
(shingles). Other members of the herpesvirus family also establish latent infections,
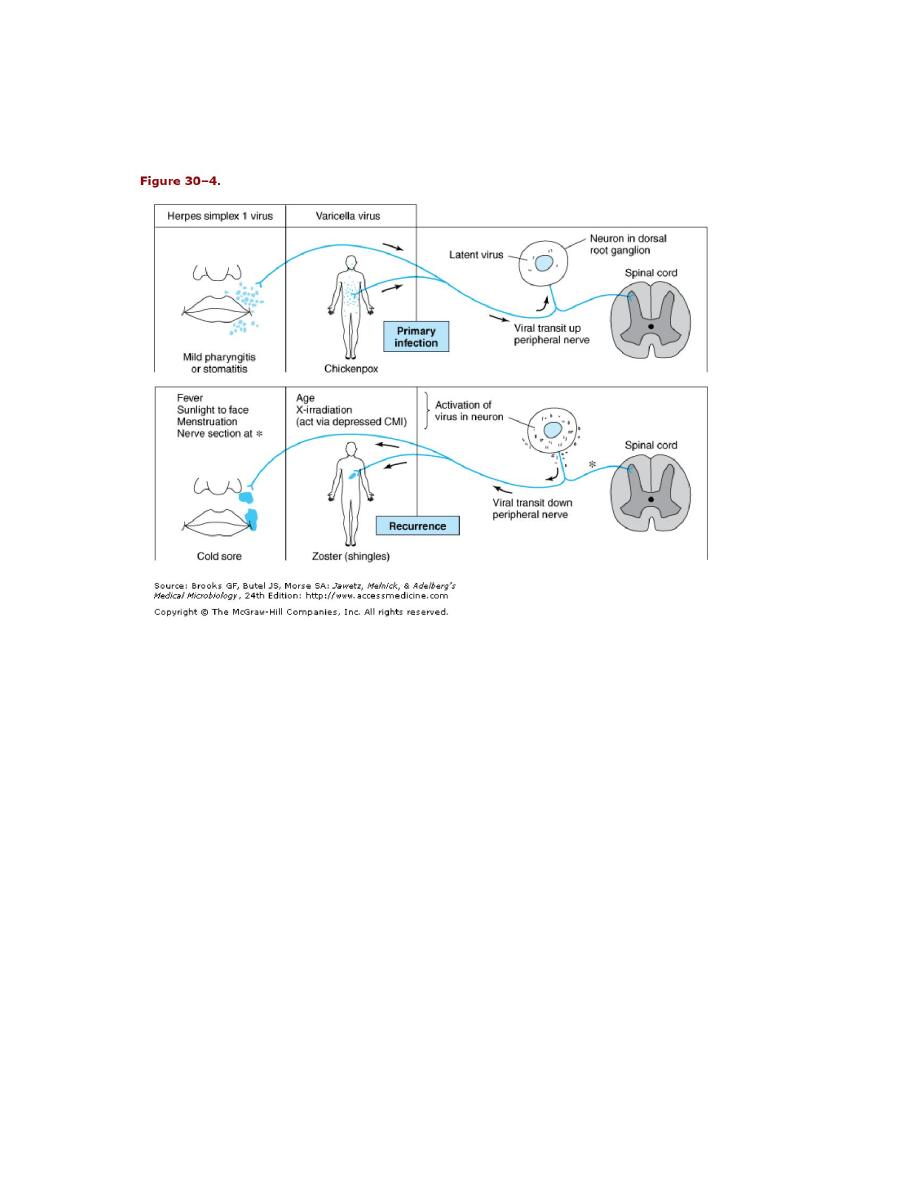
5
including cytomegalovirus and Epstein-Barr virus. All may be reactivated by
immunosuppression as in persons receiving immunosuppressant therapy.
Persistent viral infections are associated with certain types of cancers in humans (see
Chapter 43) as well as with progressive degenerative diseases of the central nervous
system of humans.
Spongiform encephalopathies are a group of chronic, progressive, fatal infections of the
central nervous system caused by unconventional, transmissible agents called prions.
Prions are thought not to be viruses. The best examples of this type of "slow" infection
are scrapie in sheep and bovine spongiform encephalopathy in cattle; kuru and
Creutzfeldt-Jakob disease occur in humans.
6
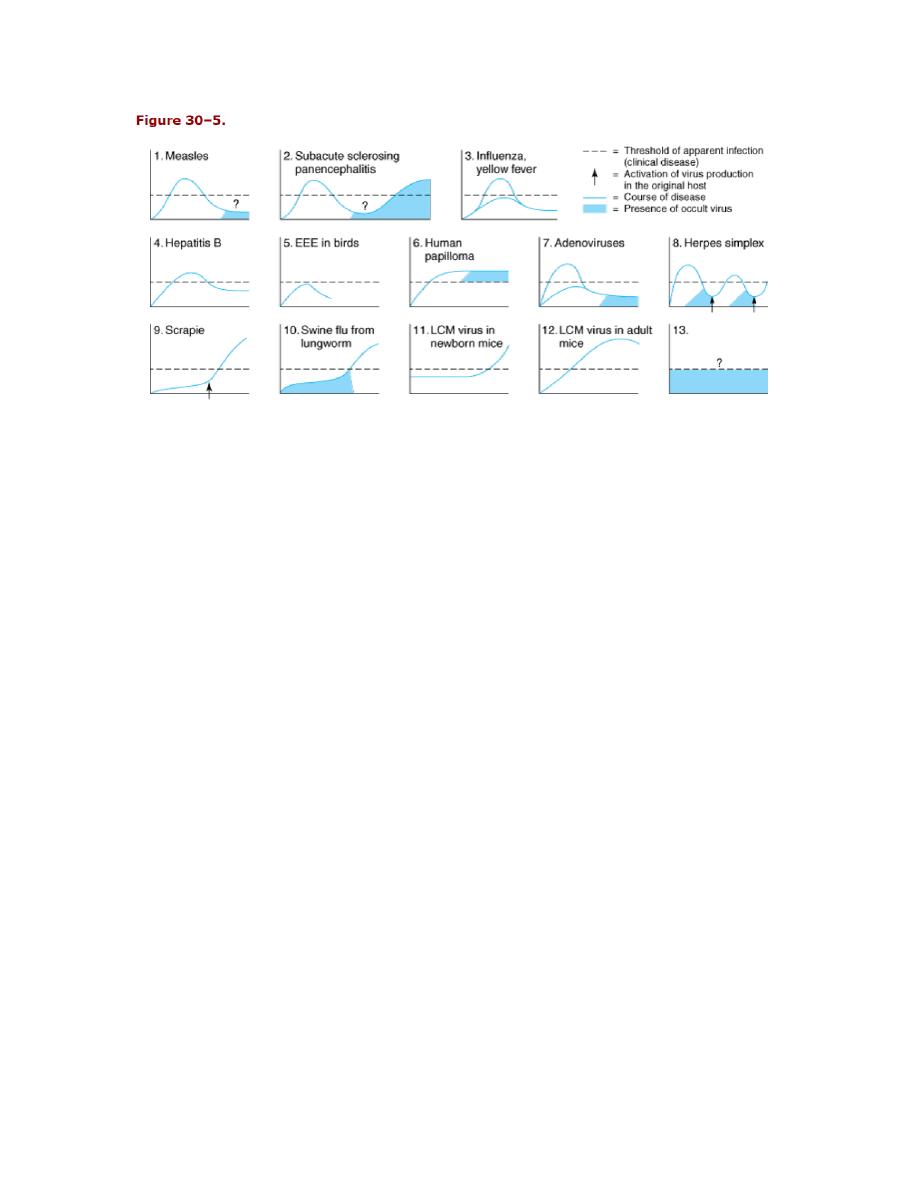
Different types of virus-host interactions: apparent (clinical disease), inapparent
(subclinical), chronic, latent, occult, and slow infections.
