Local Anesthesia
ByDr.Alaa Al-sahlany
M.Sc. Derm.
Nov. 30,2016
Local anesthesia vs General anesthesia
Disadvantage compared to general anesthesiaAdvantage compared to general anesthesia
• Some limitation on the extent and duration of a procedure
Reduced morbidity (especially in patients who are poor anesthesia risks)
The possibility of greater patient discomfort from the injections• Reduced cost
Reduced procedure time and faster recovery
Mechanism of action
Blocking sodium channels in the axon cell membrane prevents sodium from entering the nerve cell nerve cell is not depolarized the action potential is blocked
Speed of anesthesia
Smaller unmyelinated C-type nerve fibers that conduct pain sensation followed by intermediate fibers that carry sensations of heat and cold and lastly he myelinated A-type fibers that carry pressure sensation and motor fibersClinically, this is evident when an area seems fully anesthetized for scalpel of surgery, but the patient still feels the pressure of the surgeon’s fingers
The dissociation constant (pKa) of each anesthetic determines the proportion of lipid-soluble and water-soluble forms at a given pH.
A low pKa leads to rapid onset of anesthesia(inverse relation), as more of the anesthetic will be in the non-ionized lipid soluble form
Alkalinization of the anesthetic solution i.e. addition of sodium bicarbonate will (1) speed its onset of action as alkalinization increase the proportion of the anesthetic in the lipid-soluble form which can penetrate the cell membrane easily and (2)decrease the pain associated with injecting the anesthetic due to its acidic pH
Infected tissue is difficult to anesthetize i.e. the inflammatory response surrounding the infection acidifies the site reduces the proportion of the anesthetic in the non-ionized, lipid-soluble form.
Two types of local anesthetics:
(1)Ester has one letter( i) hydrolyzed by plasma pseudocholinesterase, and the metabolites are excreted by the kidneyCan cause allergy : the metabolite para-aminobenzoic acid (PABA) is responsible for the allergic reactions seen with ester anesthetics
Patients with a deficiency of pseudocholinesterase, who are often diagnosed after prolonged paralysis following administration of standard doses of succinylcholine, are at an increased risk of ester anesthetic toxicity.
(2) Amide has two letter ( i): metabolized by the hepatic cytochrome P450 enzyme system, and the metabolites are excreted by the kidneys.
Patients with severe liver disease may be at increased risk of amide anesthetic toxicity.
UseDuration
Onset
Group
Name
Skin (in form of cream) and mucous membrane (in form of spray) and for local infiltration and nerve block
30min-2 hours
The fastest
Amide (the local anesthetic of choice in pregnancy, category B)
Lidocaine (xylocaine)
Local infiltration and nerve block
2-5 hours
(the longest)
Amide
Etidocaine, Bupivacaine
Nasal mucosa (because it is a vosoconstrictive and hemostatic)
Ester
CocaineEster
Benzocaine, procaine, tetracaineAnesthetic potency depends on lipid solubility as the anesthetic penetrates the nerve cell membrane more easily
Duration of action depends on the strength of anesthetic binding to the sodium channel .
All local anesthetics, except cocaine hydrochloride, cause vasodilation.This causes increased bleeding at the operative site and reduced duration of anesthetic action
The addition of epinephrine (adrenaline) has the beneficial effect of (1)constricting blood vessels, which prolongs the duration of anesthesia and (2)decrease the bleeding and (3)allows larger doses to be used safely
The vasoconstrictive effect of epinephrine, manifested by skin blanching, takes about 15 minutes to fully develop.
Epinephrine is a strong β- and α-agonist
Absolute contraindications to the use of epinephrine include hyperthyroidism and pheochromocytoma.
Patients taking β-blockers, monoamine oxidase inhibitors, tricyclic antidepressants, and phenothiazines are more sensitive to epinephrine
Epinephrine is clearly contraindicated for digital anesthesia in patients with peripheral vascular disease.
The use of epinephrine on digits has been controversial
High doses of epinephrine can induce laborSide effects of local anesthetics
ManagementClinical manifestations
B.P.
P.R.
Diagnosis
Trendelenburg position, reassurance
Sweating, hyperventilation, nausea, syncope
(Excess parasympathetic discharge due to patient anxiety)
Low
Low
Vasovagal reaction(the most common)
Reassurance (usually resolves in minutes)
Palpitation(excess α and β-adrenergic receptor stimulation)
High
High
Epinephrine reaction
Subcutaneous epinephrine, steroids, antihistamines, O2, i.v. fluid
• Stridor, bronchospasm, urticaria (Peripheral vasodilatation with reflex tachycardia)
Low
High
Anaphylactic reaction(amides rarely cause anphylaxis)
Depends on the severity
Circumoral and digital paresthesia followed by drowsiness, tremor, slurred speech, and finally seizure, coma, cardiopulmonary depression
Normal
Normal
Lidocaine overdose
There is some allergy cross-reactivity within the various ester anesthetics and within the amide anesthetics, but there is no cross-reactivity between the ester and amide anesthetic classes
Maximum recommended dosages of lidocaine are 5 mg/kg (without epinephrine), 7 mg/kg (if with epinephrine)
Cardiovascular and pulmonary symptoms develop at significantly higher doses than do early CNS symptoms
Prilocaine and benzocine can cause methemoglobinemia .
Types of local anesthesiaThere are many ways to deliver the local :anesthetics
Topical anesthesia
Topical anesthesia involves applying the anesthetics directly to skin or mucous membrane without injection, for example, applying cream to skin, spray to mouth, drops to the eyes…etc.Topical anesthetics for mucous membranes are far more effective than skin anesthetics, as the stratum corneum barrier is absent
One to two drops of tetracaine into each eye achieves complete conjunctival anesthesia after a few seconds
EMLA® cream is a mixture of 2.5% lidocaine and 2.5% prilocaine and applied as a thick layer under occlusion at least 1 hour before the procedure.
Local infiltration
It is done by injecting the anesthetics into dermis or subcutaneous tissue which leads to anesthesia of area being injected only (unlike nerve block anesthesia) e.g. when the surgeon try to anesthetize area to aspirate abscess.The actual injection of the anesthetic causes a significant stinging sensation that is usually far more painful than the needle insertion
Subcutaneous anesthetic injection is less painful than intradermal injection(evident by bleaching), but the onset of anesthesia is slower and the duration is shorter
Attempt should be made to minimize the pain of injecting the anesthetic by:
(1)Reassurance, (2)verbal distraction, (3)mechanical distraction such as a pinch or the use of vibration at the site of injection or (4)using a topical anesthesiaPinching works by stimulating cutaneous nerves, making them refractory to the following injection sensation
Nerve block anesthesia
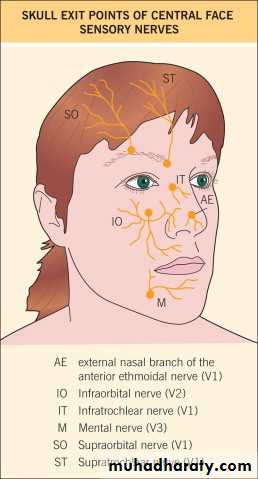
The nerve block is done by injecting the anesthetic near the nerve leading to anesthesia of all the area distal to the point of injection e.g. when the dentist block the infraorbital nerve before tooth extraction, this anesthetize the upper lip , cheek and lower eyelid.Injecting the anesthetic into the nerve will manifest as a sharp pain along the nerve and this may cause nerve injury and subsequent dysesthesia.
Anesthetic effect may take about 15 minutes to develop
Care must be taken not to inject the nearby blood vessels by withdrawing the plunger of syringe before injecting the anesthetic.Advantage: compared to local infiltration
(1) anesthetize large areas using the least amount of anesthetic, (2)minimizing patient discomfort (less injections)and (3) decreasing distortion of the operative site (little swelling) especially when you want to see the area being anesthetized looks natural.
Field block anesthesia
Involves injecting a ring of anesthetic around the proposed surgical site e.g. around a cyst will avoid puncturing the cyst.
Advantage:
(1)anesthetizing large areas using less amount of anesthetic and (2)minimizing distortion of the surgical site
Disadvantage:
(1) practical only in areas where innervation arrives horizontally through the skin, such as is seen on the scalp, but not vertically from deeper tissues, as is seen on the eyelid.(2)There will be no hemostasis at the incision site
Tumescent anesthesia
Tumescent anesthesia involves the subcutaneous infusion of large amounts of lidocaine with epinephrine using a pump(the lidocaine is diluted with about 1000 ml of normal saline)It has been used most extensively for liposuction under local anesthesia and hair transplantation
The solution is injected until firm tumescence of the tissue has been achieved
Doses as high as 35–50 mg/kgAnesthesia and epinephrine-induced hemostasis develop within about 20 minutes and last for several hours
Cryoanesthesia
By rapid cooling of the skin surface using (1) cryogen sprayed onto the skin surface, (2)a cold glass placed directly onto the site being treated or (3) cold air blown onto the skin surface with a coupling gel in placeTalkesthesia
Anesthesia by talking to the patient and distracting his attentionDefinitions
Tumescensce: swellingCryo:cold