Pathology Dr.lamyaa-lecture2
1
Healing
Cell and tissue regeneration:-
• Cell renewal occurs continuously in labile tissues such as the bone marrow,
gut epithelium and skin. Damage to epithelia or an increased loss of blood
cells can be corrected by the proliferation and differentiation of stem cells
and,
.
• Tissue regeneration can occur in parenchymal organs with stable cell
populations, but with exception of the liver this is usually a limited process.
The surgical removal of the kidney elicits in the contralateral kidney a
compensatory response that consists of both hypertrophy and hyperplasia of
the proximal duct cells .
the regenerative response of the liver that occurs after surgical removal of
hepatic tissue is striking. Up to 60% of the liver may be removed in a procedure
called living –donor transplantation, in which a portion of the liver is resected
from a normal individual and is transplanted in recipient with end stage liver
disease, or after partial hepatectomies performed for tumor removal . in such
cases the tissue resection triggers proliferation of the remaining hepatocytes
(normal quiescent ).
• Expermintally, hepatocytes replication after partial hepatectomy is initiated
by cytokines (e.g tumor necrosis factors TNF and interleukin 6 (IL 6) . EGF
(epidermal growth factor receptors, or EGFR) with intirinsic tyrosine kinase
activity is mitogenic for hepatocytes.
• It should be emphasized that extensive regeneration or compensatory
hyperplasia can occur only if the residual tissue is structurally and
functionally intact , as after partial surgical resection . by contrast, if the
tissue is damaged by infection or inflammation regeneration is incomplete
and is accompanied by scaring.
Repair by connective tissue:
Healing or repair by connective tissue is encountered if
1. A severe or chronic persistent tissue injury that result in damage to
parenchymal cells as well as the stromal framework
2. Injuries affects nondividing cells
Pathology Dr.lamyaa-lecture2
2
• Under these conditions, repair occur by replacement of the non-
regenerated cells with the connective tissue, or by a combination of
regeneration of some cells and scar formation.
• Repair begin within 24 h of injury by the emigration of the fibroblasts and
the induction of fibroblast and endothelial cell proliferation.
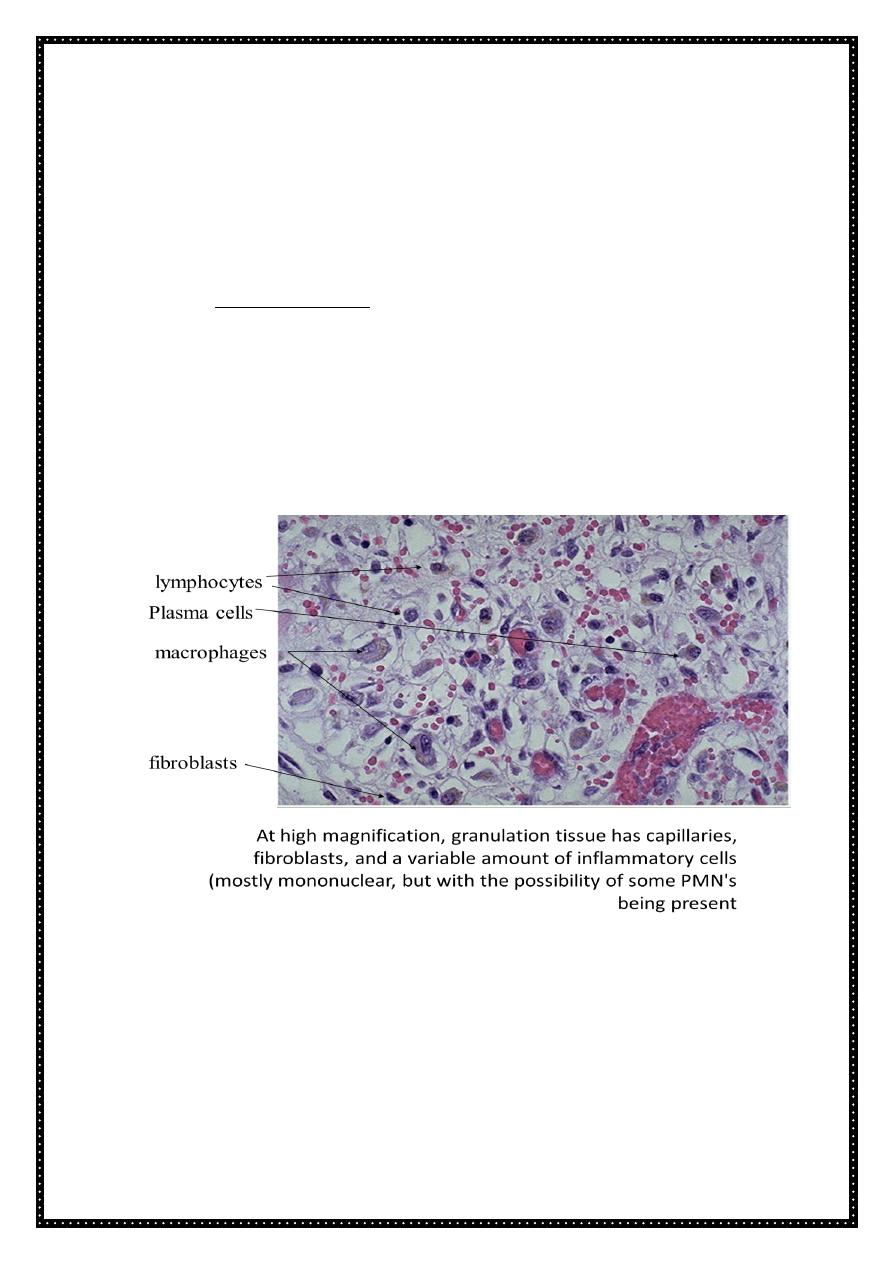
• By 3 to 5 days a specialized type of tissue that is characteristic of healing
called granulation tissue is apparent . the term granulation tissue derive
from the pink soft granular gross appearance, such as that seen beneath the
scab of a skin wound . it is microscopic appearances is characterized by
proliferation of fibroblast and new thin –walled , delicate capillaries
(angiogenesis), in a loose ECM granulation tissue then progressively
accumulated connective tissue matrix. Eventually resulting in the formation
of a scar which may remodel over time.
Repair by connective tissue deposition consist of four sequential processes:
1. Formation of new blood vessels (angiogenesis)
2. Migration and proliferation of fibroblasts
3. Deposition of ECM (scar formation)
4. Maturation and reorganization of the fibrous tissue (remodeling)
Pathology Dr.lamyaa-lecture2
3
Angiogenesis (neovascularization)
:
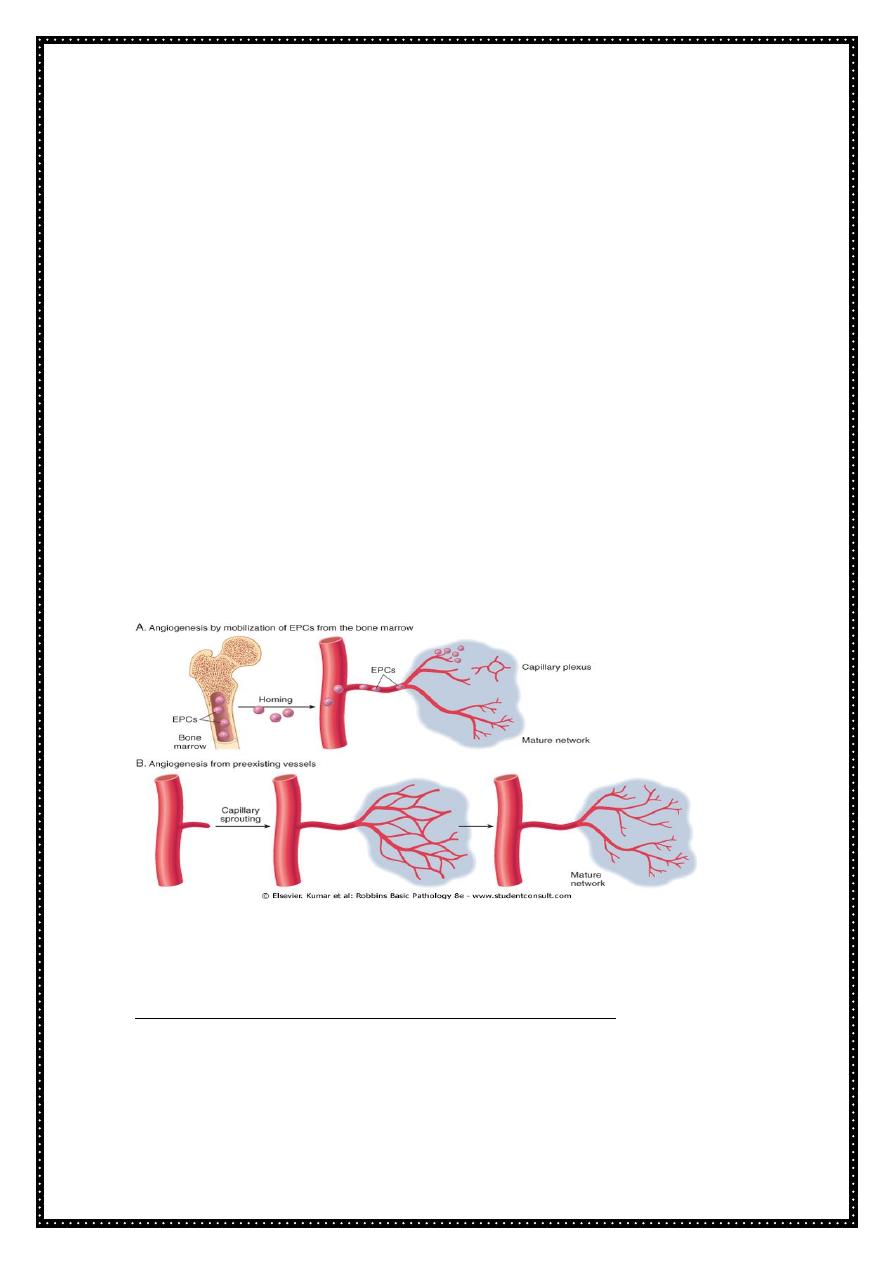
Angiogenesis occur by two mechanism:-
The preexisting vessels send out capillary sprouts to produce new vessels.
Angiogenesis is a critical process in healing at site of injury, in the
development of the collateral circulation at site of ischemia and in allowing
tumor to increase in size beyond the limits of their original blood supply.
It has recently been found that endothelial precursor cells may migrate from
the bone marrow to areas of injury and participate in angiogenesis at these
sites .
• New vessels formed during angiogenesis are leaky. This leakiness explains
why granulation tissue is often edematous, and account in part for the
edema that may persist in healing wounds long after the acute inflammatory
response has resolved.
• Several factor induce angiogenesis, but the most important are VEGF and
basic fibroblast growth factor (FGF-2). VEGF stimulate both proliferation and
motility of endothelial cells thus initiating the process of capillary sprouting
. in angiogenesis involving endothelial cell precursors from the bone marrow
and to induce proliferation and motility of these cells at the sites of
angiogenesis.
Migration of fibroblasts and ECM Deposition (scar formation):
Scar formation builds on the granulation tissue framework. It occurs in tow
steps:-
• Migration and proliferation of fibroblast into the site of the injury and
• Deposition of ECM by these cells
Pathology Dr.lamyaa-lecture2
4
The recruitment and stimulation of fibroblasts is driven by many growth factors
including PDGF (platelet derived growth factor). One source of these factor is
the activated endothelium but more importantly growth factors are also
elaborated by inflammatory cells, macrophages in particular are important
cellular constituents of granulation tissue, and beside clearing extracellular
debris and fibrin at the site of injury, they elaborate a host of mediators that
induce fibroblast proliferation and ECM production. Mast cells and lymphocytes
can contribute directly or indirectly to fibroblast proliferation and activation.
Deposition of ECM by these cells:
As healing progresses, the number of proliferating fibroblast and new
vessels decreases, however, the fibroblast progressively become more
synthetic and hence there is increased deposition of ECM.
Collagen synthesis in particular is critical to the development of strength in
a healing wound site . collagen synthesis by fibroblasts begins early in
wound healing and continues for several weeks, depending on the size of
the wound.
The same growth factor that regulate fibroblast proliferation also
participate in stimulating ECM synthesis.
As the scar matures there is progressive vascular regression , which
eventually transforms the highly vascularized granulation tissue into a pale
largely avascular scar.
Many growth factors are involved in the above processes including TGF-B ,
PDGF, and FGF as well as cytokines (IL- & TNF).
ECM and tissue remodeling:
• ECM continues to be modified and remodeled. The outcome of the repair
process is in part a balance between ECM synthesis and degradation,
• the degradation of collagens and other ECM components is accomplished
by a family of matrix metalloproteinase (MMP), which are dependent on
zinc ion for their activity .MMPS include interstitial enzymes that degrade
collagen, fibronectin, proteoglycans, synovial cells ) and their synthesis and
secretion are regulated by growth factors, cytokines and other agents. Their
synthesis may be suppressed pharmacologically with steroids.
• Cutaneous wound healing:
This is a process that involves both epithelial regeneration and the formation of
connective tissue scar and is thus illustrative of the general principles that apply
to wound healing in all tissues. The events are orchestrated by interplay of
growth actors and ECM.
Cutaneous wound healing has three main phases:-
• Inflammation
Pathology Dr.lamyaa-lecture2
5
• Formation of granulation tissue
• ECM deposition and remodeling
Event in wound healing overlap to a great extent and cannot be completely
separated from each other.
Based on the nature of the wound, the healing of the cutaneous wounds can
occur by first or second intention.
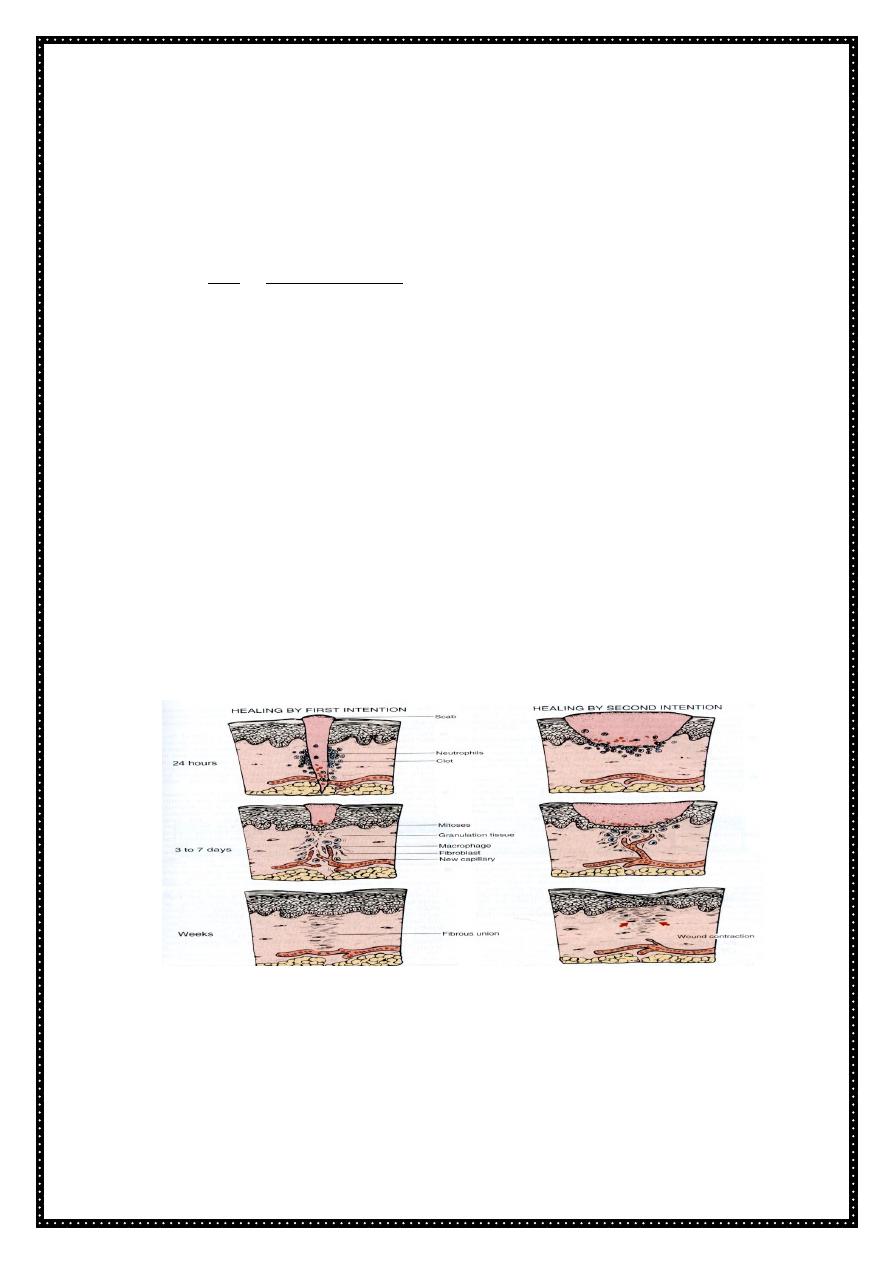
• Healing by first intention :-
One of the simplest example of the wound repair is the healing of a clean
uninfected surgical incision approximated by surgical sutures. This is referred
to as primary union or healing by first intention.
The incision causes only focal disruption of the epithelial basement membrane
continuity and death of a relatively few epithelial and connective tissue cells.
As a result, epithelial regeneration predominates over fibrosis. a small scar is
formed but there is minimal wound contraction.
• The narrow incisional space first fill with fibrin clotted blood.
• Within 24 hr , neutrophils are seen at the incision margin migrating toward
the fibrin clot.
• Within 24 to 48 hrs, epithelial cells from both edges have begun to migrate
and proliferate along the dermis. The cells meet at the midline, beneath the
surface scab yielding a thin but continuous epithelial layer.
Wound healing by primary and secondary union.
• By day 3 neutrophils have been largely replaced by macrophages and
granulation tissue progressively invade the incision space. Epithelial cell
proliferation continues yielding a thickened epidermal covering layer
• By day 5, neovascularization reach its peak as granulation tissue fill the
incisional space. The epidermis recover its normal thickness as
Pathology Dr.lamyaa-lecture2
6
differentiation of surface cells yields a mature epidermal architecture with
surface keratinization
• During the second week there is continued collagen accumulation and
fibroblast proliferation that bridge the incision. The leukocytes infiltrate ,
edema and increase vascularity are diminished
• The long process of blanching begins accomplished by increasing collagen
deposition within the incisional scar and the regression of vascular channels.
•
By the end of the first month, the scar comprises acellular connective tissue
largely devoid of inflammatory cells and covered by an essentially normal
epidermis . the tensile strength of the wound increases with time . however
the epidermal appendages destroyed in the line of the incision are
permanently loss
.
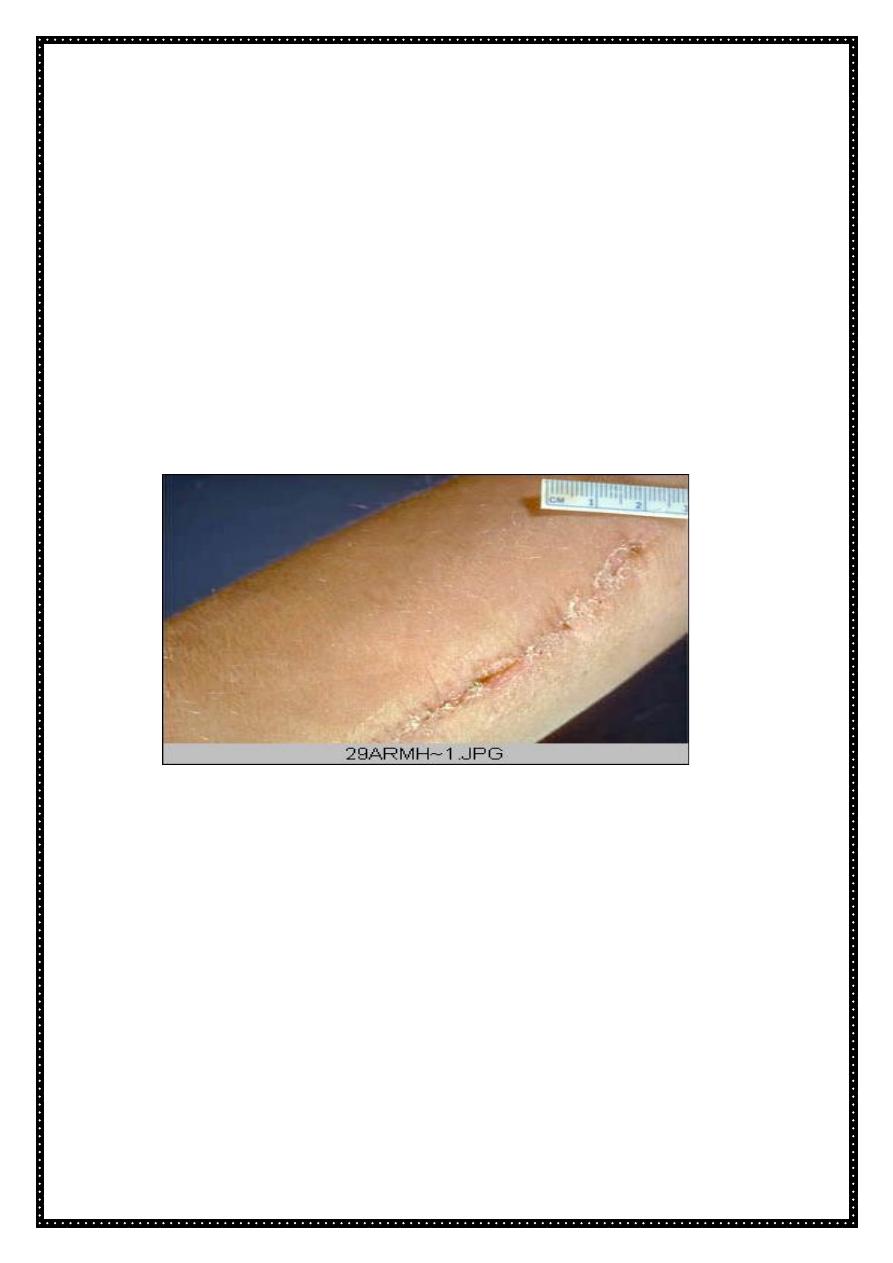
Arm, healing surgical incision. This image demonstrates healing by
first intention which occur in clean, un infected wounds that have
apposed edges.
• Healing by second intention (healing by secondary union):-
1. When cells or tissue loss is more extensive
2. the repair process is more complex,
3. the inflammatory reaction is more intense,
4. there is abundant development of granulation tissue and
5. the wound contracts by the action of myofibroblast.
6. This is followed by the accumulation of ECM and formation of a large scar.
7. This mode of healing occurs in :
• Large wound
• Abscesses
• Ulceration
Pathology Dr.lamyaa-lecture2
7
• After infarction in parenchymal organs
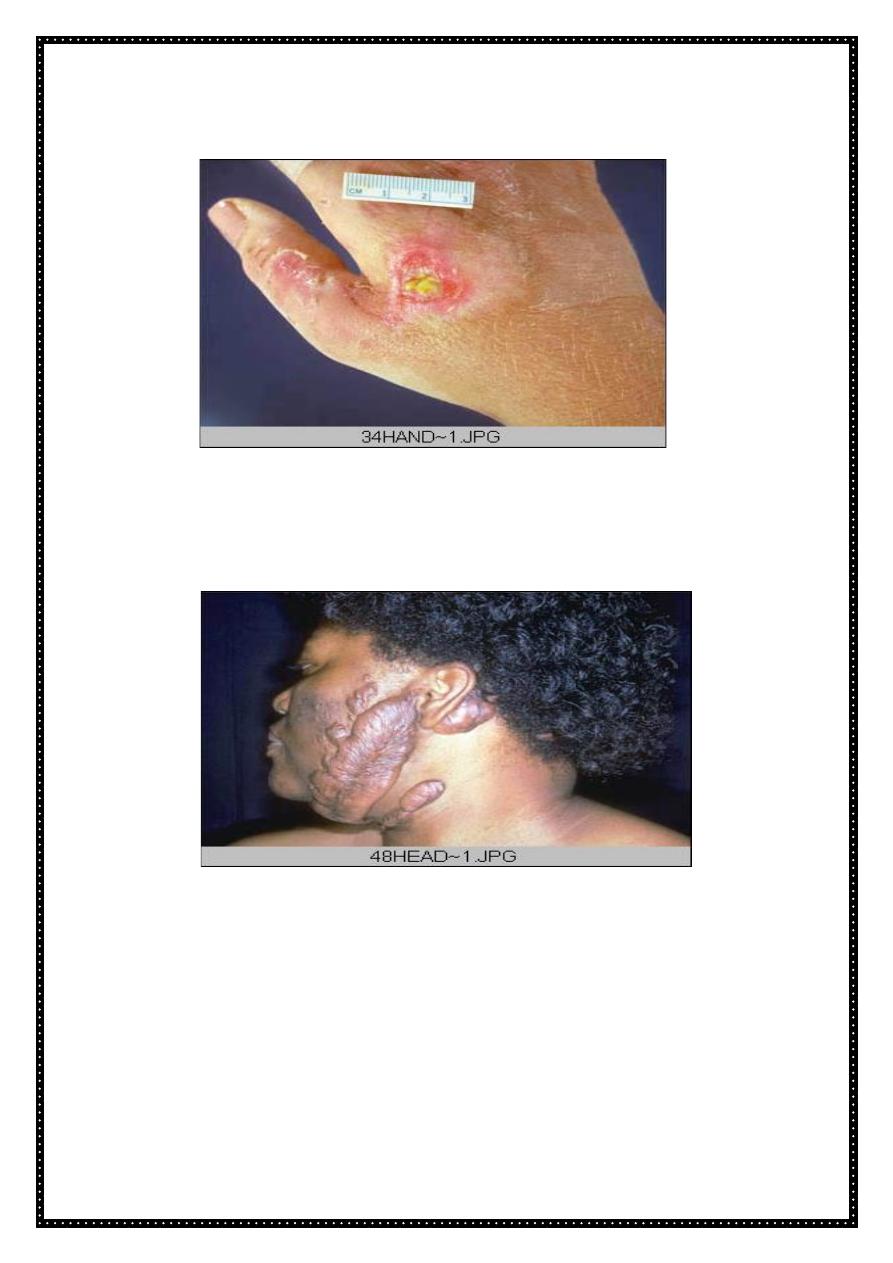
Wound with large tissue defect healed by secondary intention. Note the
red granular appearance of the granulation tissue. A whitish- greenish-
yellow neutrophilic exudates represent an inflammatory response to
bacterial invasion of the wound.
Keloid
Keloid nodular masses of of hyperplastic scar tissue, occur when the wound
healing process runs unchecked. They are more commonly in people of
African descent. surgical excision leads to repeated keloid formation.
•
Factors influencing wound healing:
A. Local
1. Type, size& location of wound.
2. Adequacy of blood supply.
3. Infection.
4. Movement
Pathology Dr.lamyaa-lecture2
8
5. Presence of foreign body material.
6. Exposure to ionizing radiation, & ultraviolet light.
B.Systemic
1. Circulatory status.
2. Metabolic status.
3. Systemic infection.
4. Diabetes mellitus.
5. Hormones.
6. Hematological diseases; neutropnia.
7. Renal failure.
8. Tumor cachexia
Local factors:
Type, size and location of the wound
1. A clean, aseptic surgical wound heals faster than a wound produced by
blunt trauma with abundant necrosis and irregular edges.
2. Small wounds heal faster than large ones.
3.
Wounds that occur in richly vascularized areas such as the face heal
faster than those that occur in poorly vascularized areas such as the foot
.
• Adequacy of blood supply
1. Wound with poor blood supply heal slowly e.g. Leg wounds in patients with
varicose veins.
2. Ischemia due to pressure produces bedsores. The same mechanism
(pressure) prevents their healing. Ischemia due to arterial obstruction also
prevents healing.
• Infection
1. Wounds provide a portal of entry for microorganisms. Infection delays or
prevents healing.
• Movement
1. Early motion subjects the wound to persistent trauma.
2. Exercise also increases the circulating levels of glucocorticoids, which inhibit
repair.
• Exposure to ionizing radiation & ultraviolet light
1. Irradiation of the wound blocks cell proliferation, retards granulation tissue
formation & interferes with blood supply. The outcome is slow healing.
2. Exposure of wounds to ultraviolet light accelerates the rate of healing.
Systemic factors:
• Circulatory status
Pathology Dr.lamyaa-lecture2
9
1. Cardiovascular status determines the blood supply to the injured area,
which is important for wound healing. Poor healing attributed to old age is
often due largely to impaired circulation.
• Metabolic status
1. Protein calorie malnutrition impairs healing.
2. Vit. C deficiency (scurvy) impairs wound healing. This is because vit.c is
involved in synthesis of collagen Thus in vit.c deficiency the collagen fibers
show less cross-linking than normal & is more readily degraded.
3. Zinc is required for collagen synthesis, so its deficiency will lead to delay
wound healing.
• Systemic infection
Leads to delay wound healing (multifactorial).
• Diabetes mellitus
Wounds in diabetics often become infected & in turn, infection makes the
control of diabetes difficult, resulting in sever retardation or failure of healing.
• Hormones
Corticosteroides impair wound healing due to
1. inhibition of collagen synthesis,
2. general depression of protein synthesis &
3. anti-inflammatory effect, with scanty macrophage infiltrates & so lack of
macrophage-derived growth factors.
Complications of wound healing:
• Wound dehiscence and Incisional hernias. A wound after a laparotomy may
burst open. This occurs in 0.5-5% of all abdominal operations. Increased
mechanical stress on the wound from vomiting, coughing, or ileus is a factor
in over 90% of cases.
Incisional hernia is a late consequence of a weak abdominal scar.
• Ulceration. Wounds ulcerate because of inadequate blood supply &
vascularization. For example, leg wounds typically ulcerate.
Non-healing wounds develop in areas devoid of sensation, such as trophic or
neuropathic ulcers, which may be seen in patients with spinal cord injury,
• Excessive scar formation (Keloid). An excessive deposition of extracellular
matrix at the wound site results in hypertrophic scar or keloid. Histologically,
there are abundant, broad & irregular collagen bundles, with more
capillaries and fibroblasts than would be expected for a scar of the same
age.
Pathology Dr.lamyaa-lecture2
11
•
Excessive contraction (contracture). A decrease in wound size depends on
the presence of myofibroblasts
.
