
1
5th stage
Pediatrics
Lec-
Dr.Athl Humo
23/11/2016
Infectious disease
Differential Diagnosis of Fever and Rash :
1. Maculopapuler:
Virus: measles, rubella, roseola, fifth disease, EBV
Bacteria: scarlet fever(group A streptococcus)
Rickettsiae
2. Diffuse erythema:
Bacteria: scarlet fever, toxic shock syndrome(staph. aureus), Staphylococcal
scalded skin syndrome(4S).
3. Urticarial:
Virus: EBV, HBV.
Bacteria: mycoplasma.
4. Vesiculobullous:
Virus: Herpes simplex, varicella-zoster.
Bacteria: staphyllococcal bullous impetigo.
5. Petechial:
Virus: adenovirus, atypical measles.
Bacteria: meningococcemia
Mumps
Mumps is an acute self-limited infection, now unusual in developed countries because of
widespread use of vaccination.
Although no longer common in countries with extensive vaccination programs, mumps
remains endemic in the rest of the world, warranting continued vaccine protection.
It caused by mumps virus which is a single-stranded RNA virus
.
2
Epidemiology :
Mumps infection occurred more often in the winter and spring months.
Mumps is spread from person to person by respiratory droplets.
Virus appears in the saliva from up to 7 days before to as long as 7 days after onset of
parotid swelling. The period of maximum infectiousness is 2 days before to 5 days
after onset of parotid swelling.
Clinical features :
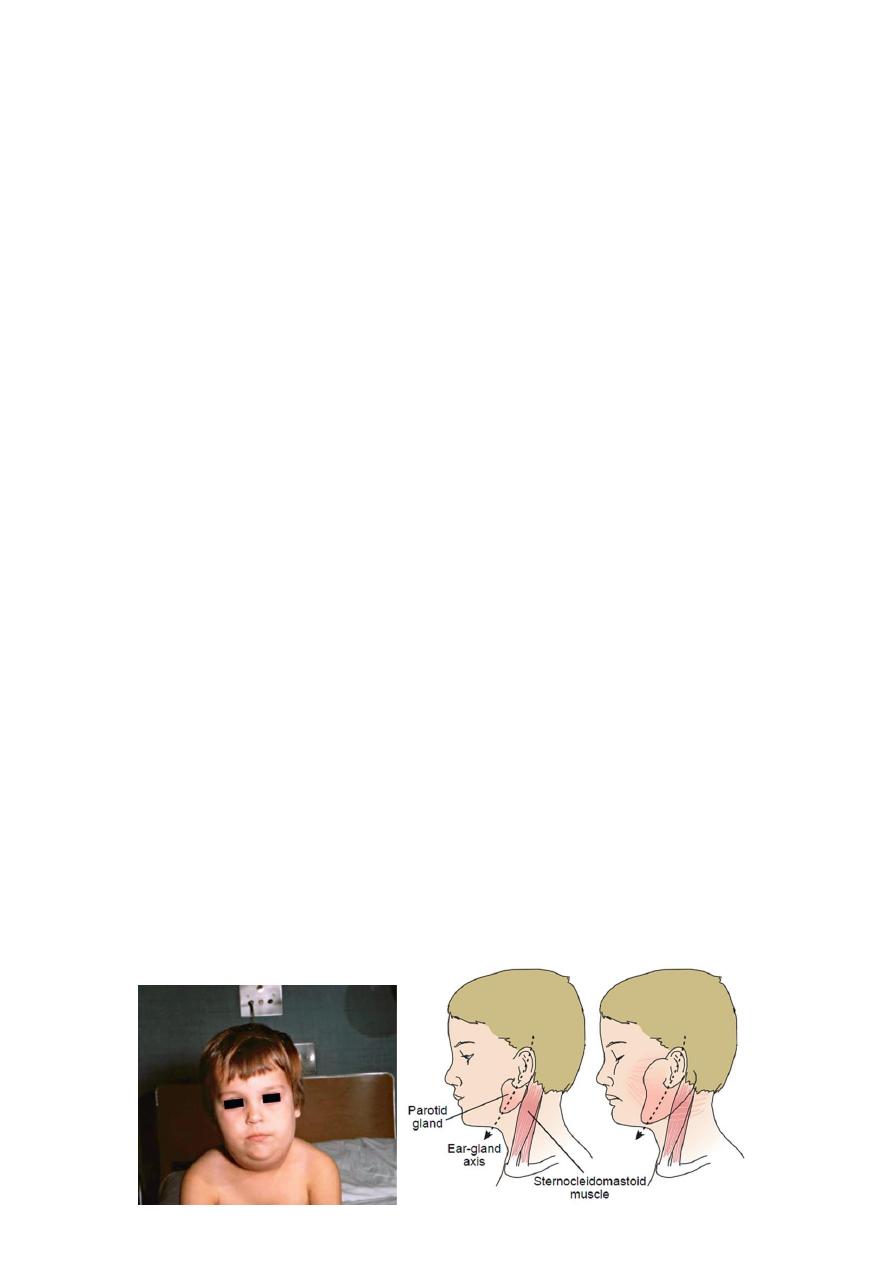
The incubation period is 16-18 days resulting in clinical presentation ranging from
asymptomatic or nonspecific symptoms to the typical illness associated with parotitis
with or without complications involving several body systems.
The typical presentation:
A prodrom 1-2 days and consisting of fever, headache, and vomiting.
Parotitis then appears and may be unilateral ,then becomes bilateral in about
70% of cases. The parotid gland is tender, and may be accompanied by ear
pain on the ipsilateral side. Sour or acidic foods may enhance pain in the
parotid. As swelling progresses, the angle of the jaw obscured and ear lobe
may be lifted upward and outward.
The opening of Stensen duct may be red and edematous.
The parotid swelling peaks in approximately 3 days, then gradually subsides
over 7 days. Fever and the other systemic symptoms resolve in 3-5 days.
A morbilliform rash is rarely seen.
Submandibular salivary glands may also be involved or may be enlarged without
parotid swelling.
Edema over the sternum due to lymphatic obstruction may also occur.
Schematic of a parotid gland infected with mumps
(right) compared with a normal gland (left)
3
Differential diagnosis :
Parotid swelling may be caused by many other infectious and noninfectious conditions.
Viruses that cause parotitis include: parainfluenza1 & 3 viruses, influenza A virus,
CMV, HIV…
Purulent parotitis, is usually caused by Staphylococcus aureus, unilateral,
extremely tender, and is associated with an elevated white blood cell count, and
may involve purulent drainage from Stensen duct.
Submandibular or anterior cervical adenitis due to a variety of pathogens may
also be confused with parotitis.
Other noninfectious causes of parotid swelling include: obstruction of the Stensen
duct, collagen vascular diseases such as SLE, and tumor.
Complications :
The most common complications of mumps are meningitis, with or without
encephalitis, and orchitis.
Uncommon complications include deafness, optic neuritis, facial palsy, pancreatitis,
pneumonia, nephritis and thrombocytopenia.
Maternal infection with mumps during the 1st trimester of pregnancy results in
increased fetal loss. No fetal malformations have been associated with intrauterine
mumps infection.
Meningoencephalitis :
Symptomatic meningoencephalitis. occurs in only 10-30% of mumps cases, but CSF
pleocytosis has been found in 40-60% of patients as subclinical more than apparent
meningitis.
The meningoencephalitis is usually benign, may occur before, along with, or
following the parotitis.
It most commonly manifests 5 days after the parotitis.

4
Orchitis
Involvement in young boys is rare, but in adolescent and after puberty, orchitis
occurs in 30-40% of male cases.
It begins within days following onset of parotitis in the majority of cases and is
associated with moderate to high fever, chills, and exquisite pain and swelling of the
testes.
Atrophy of the testes may occur, but sterility is rare even with bilateral involvement.
Prevention :
Immunization with the live mumps vaccine is the primary mode of prevention.
It is given as part of the MMR, 2 dose vaccine schedule, at 12-15 mo of age for the 1st
dose and 4-6 yr of age for the 2nd dose.
Measles (rubeola)
Measles (rubeola) is highly contagious, owing to widespread vaccination, endemic
transmission is decreased.
It is caused by a single- stranded RNA paramyxovirus.
Measles virus is transmitted by droplets or the airborne route.
Infected persons are contagious from about 3 days before to 6 days after the
appearance of rash and immunocompromised persons can have prolonged excretion
of contagious virus.
Clinical Manifestations :
Measles infection is divided into four phases: incubation, prodromal(catarrhal),
exanthematous (rash), and recovery.
The incubation period is 8 to 12 days from exposure to symptom onset.
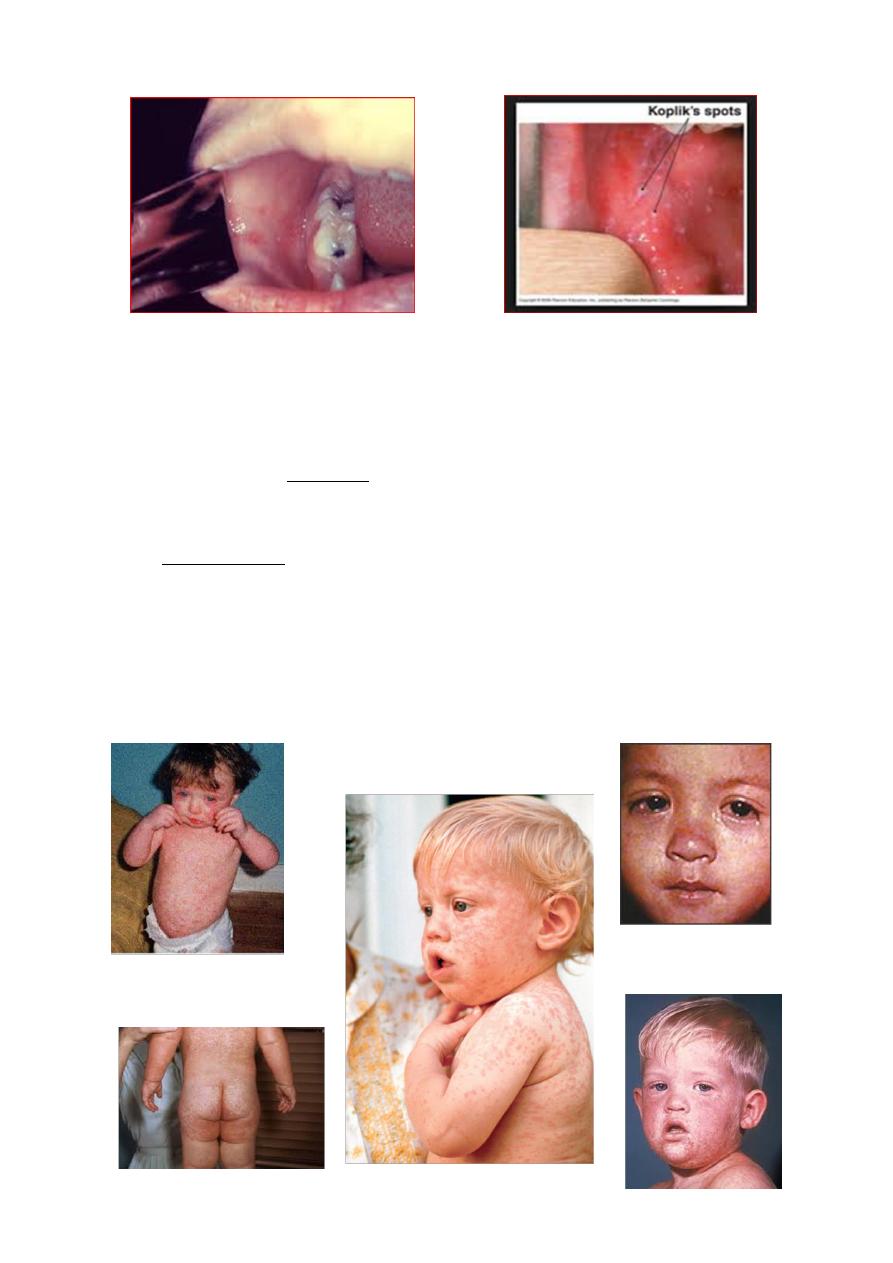
The prodromal period (3-day): characterized by cough, coryza, conjunctivitis,
photophobia, and increasing fever. The pathognomonic Koplik spots (gray-white,
sand grain-sized dots on the buccal mucosa opposite the lower molars) that last 12 to
24 hours, it present in 50-70%. The conjunctiva may reveal a characteristic transverse
line of inflammation along the eyelid margin (Stimson line).
Symptoms increase in intensity for 2-4 days until the 1st day of the rash (fever 40° C
to 40.5°C).
5
Koplik spots
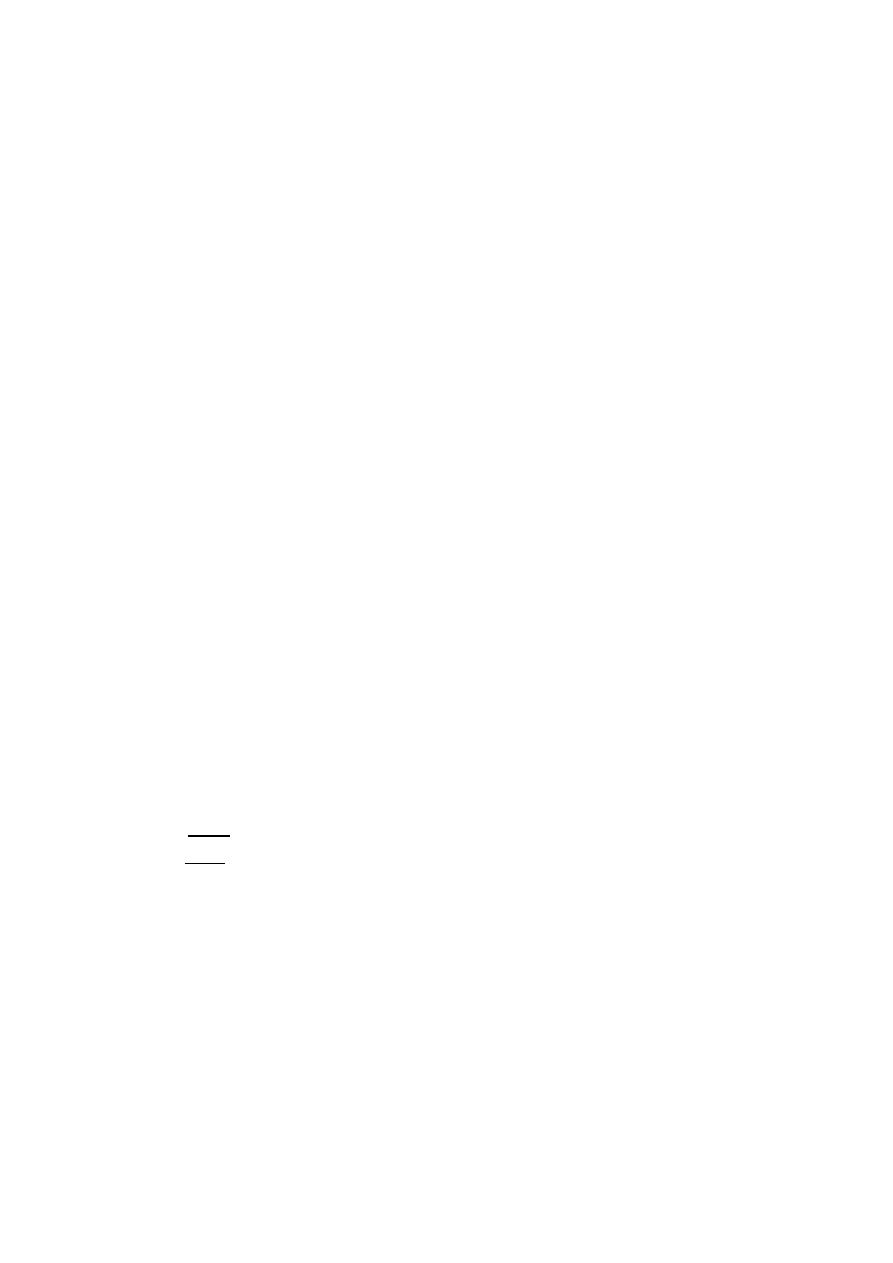
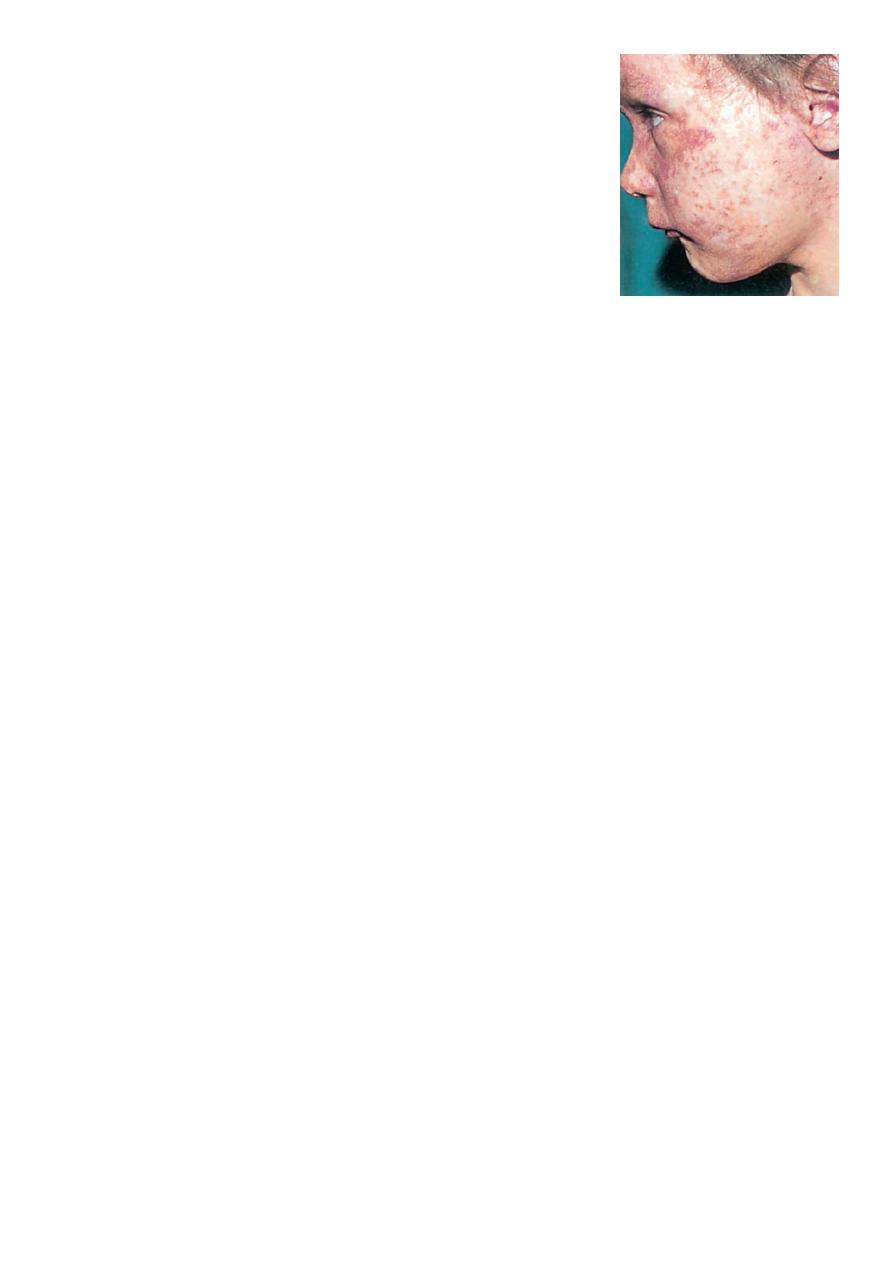
The exanthematous phase:
macular rash begins on the head (often above the hairline) and spreads over
most of the body in a cephalad to caudal pattern over 24 hours. Areas of the
rash often are confluent. The rash fades in the same pattern, and illness
severity is related to the extent of the rash. It may be petechial or hemorrhagic
(black measles). As the rash fades, it undergoes brownish discoloration and
desquamation.
Of the major symptoms of measles, the cough lasts the longest, often up to 10
days.
Cervical lymphadenitis, splenomegaly, and mesenteric LAP with abdominal
pain may be noted with the rash. Otitis media, pneumonia, and diarrhea are
more common in infants. Liver involvement is more common in adults.
6
Laboratory Studies :
The diagnosis of measles is almost always based on clinical and epidemiologic
findings.
Laboratory findings in the acute phase include Leukopenia.
Serologic confirmation is most conveniently made by:
identification of immunoglobulin IgM antibody in serum. IgM antibody
appears 1-2 days after the onset of the rash and remains detectable for about
1 mo.
demonstration of a 4-fold rise in IgG antibodies in acute and convalescent
specimens.
Viral isolation from blood, urine, or respiratory secretions can be accomplished by
culture.
PCR
Complications :
Otitis media is the most common complication of measles infection.
Interstitial (measles) pneumonia or may result from secondary bacterial infection.
Persons with impaired cell-mediated immunity may develop giant cell (Hecht)
pneumonia, which is usually fatal.
Myocarditis and mesenteric lymphadenitis are infrequent complications.
Encephalomyelitis (1 to 2 per 1000 cases) usually occurs 2 to 5 days after the onset of
the rash. Early encephalitis probably is caused by direct viral infection of brain tissue,
whereas later onset encephalitis is a demyelinating and probably an
immunopathologic phenomenon.
Subacute sclerosing panencephalitis is a late (after 8 to 10 years) neurologic
complication of slow measles infection that is characterized by progressive
behavioral and intellectual deterioration and eventual death.There is no effective
treatment.
Treatment :
Routine supportive care includes maintaining adequate hydration and antipyretics.
The WHO recommends routine administration of vitamin A for 2 days to all children
with acute measles.
7
Prevention :
1. Exposure of susceptible individuals to patients with measles should be avoided
during this period.
2. In hospitals, standard and airborne precautions should be observed for this period.
3. Live measles vaccine prevents infection and is recommended as measles, mumps,
and rubella (MMR) for children at 12 to 15 months and 4 to 6 years of age.
4. Susceptible household contacts with a chronic disease or who are
immunocompromised should receive postexposure prophylaxis with measles vaccine
within 72 hours of measles exposure or immunoglobulin within 6 days of exposure.
Rubella
Rubella, also known as German measles or 3-day measles.
It is caused by a single-stranded RNA virus.
Rubella virus is most contagious through direct or droplet contact with
nasopharyngeal secretions from 2 days before until 5 to 7 days after rash onset.
Rubella usually occurs in the spring.
Transplacental antibody is protective during the first 6 months of life.
Clinical Manifestations :
1. The incubation period for postnatal rubella is typically 16 to 18 days (range, 14 to 21
days).
2. The mild catarrhal symptoms of the prodromal phase of rubella may go unnoticed.
3. The characteristic signs of rubella are retroauricular, posterior cervical, and posterior
occipital LAP accompanied by an erythematous, maculopapular, discrete rash. The
rash begins on the face and spreads to the body, lasting for 3 days and less
prominent than that of measles, usually resolves without desquamation. Rose-
colored spots on the soft palate, known as Forchheimer spots, develop in 20% of
patients and may appear before the rash.
4. Other manifestations of rubella include mild pharyngitis, conjunctivitis, anorexia,
headache, malaise, and low-grade fever. Polyarthritis, usually of the hands, may
occur, especially among adult females, but usually resolves without sequelae.
Paresthesias and tendinitis may occur.
8
Laboratory Studies :
Diagnosis is confirmed by serologic testing:
IgM antibodies (typically positive 5 days after symptom onset)
Fourfold increase in specific IgG antibodies in paired acute and convalescent sera.
Treatment :
There is no specific therapy for rubella.
Routine supportive care includes maintaining adequate hydration and antipyretics.
Prevention :
Live rubella vaccine prevents infection and is recommended as MMR for children at
12 to 15 months and at 4 to 6 years of age.
