1
Fifth stage
vM
Pediatrics
mv
Lec 2
Dr.Athal
23/11/2016
ROSEOLA INFANTUM
- EXANTHEM SUBITUM -
Sixth disease
Epidemiology
Transplacental antibody protects most infants until 6 months of age. The incidence of
infection increases as maternally derived antibody levels decline. By 2 to 3 years of
age, approximately all children are seropositive for viral antibody.
Virus is likely acquired from asymptomatic adults who periodically shed these viruses.
It is caused primarily by human herpes virus type 6 (HHV-6), and by HHV-7 in 10%
to 30% of cases. HHV-6 and HHV-7 are DNA viruses, which are of the herpesvirus
family.
HHV-6 is a major cause of acute febrile illnesses in infants and may be responsible for
20% of visits to the emergency department for children 6 to 18 months old.
Clinical Manifestations
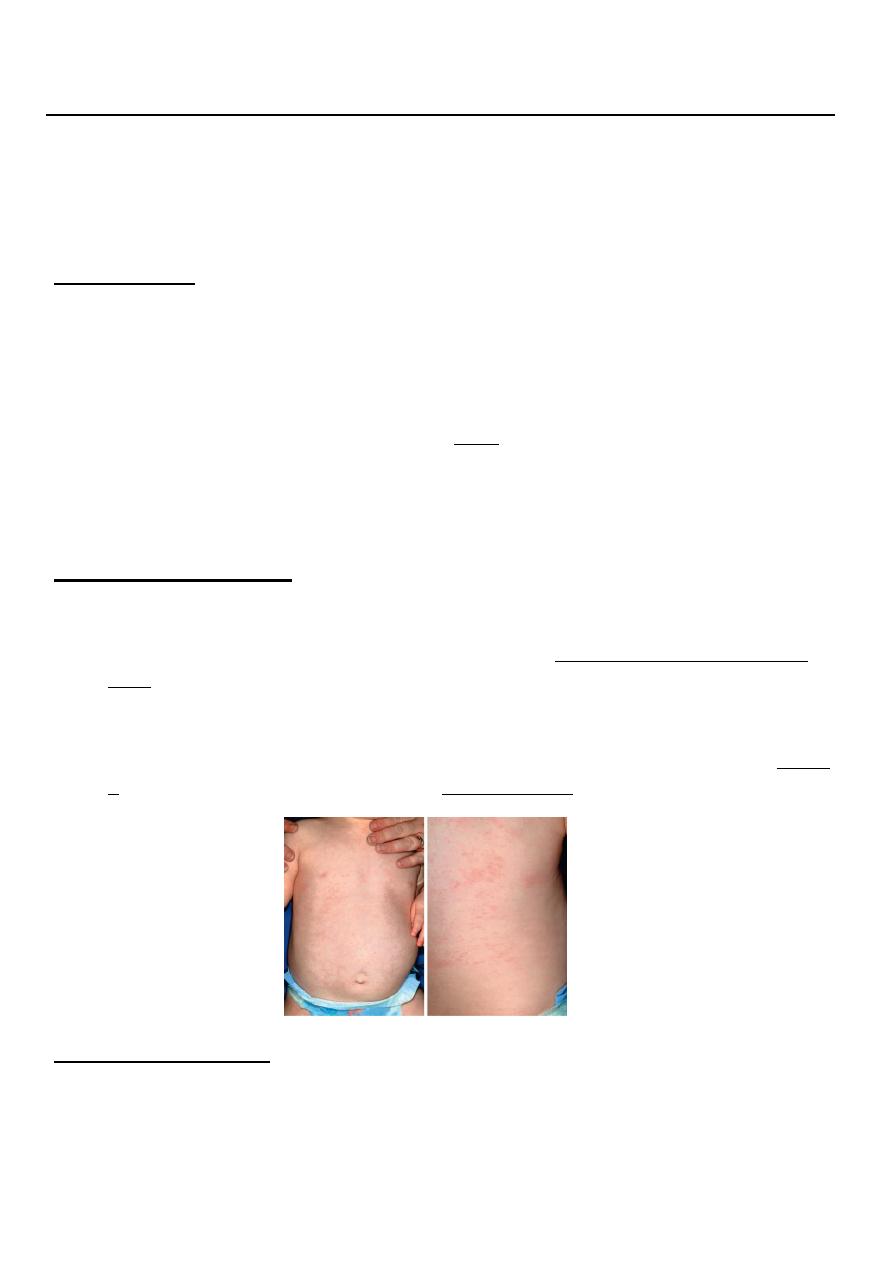
Roseola is characterized by high fever (often ≥40°C which may be accompanied by
fussiness) lasting 3 to 5 days.
Followed by maculopapular, rose-colored rash that appears with the remission of
fever, although it may present earlier. The rash usually lasts 1 to 3 days but may fade
rapidly & is not present in all infant.
Roseola is associated with approximately one third of febrile seizures.
Roseola caused by HHV-6 and HHV-7 is clinically indistinguishable, although HHV-
6 associated roseola typically occurs in younger infants.
Labrotory Findings :
The most characteristic laboratory findings noted are lower mean numbers of total
WBC, lymphocytes, and neutrophils counts.
Encephalitis with roseola is characterized by:
Minimal CSF pleocytosis with mild elevations of protein and normal glucose
concentration.
2
Serologic testing showing a fourfold rise in acute and convalescent sera.
Documentation of HHV-6 DNA by PCR in the CSF is diagnostic.
Treatment
There is no specific therapy for roseola. Routine supportive care includes maintaining
adequate hydration and antipyretics.
In immunocompromised hosts, use of ganciclovir or foscarnet can be considered.
___________________________________
ERYTHEMA INFECTIOSUM
FIFTH DISEASE
Epidemiology
caused by the human parvovirus B19
Single stranded DNA virus.
Benign self-limited illness affecting any age mostly 5-15 yrs old and even adults .
Seasonal peaks occur in the late winter and spring, with sporadic infections throughout
the year.
Incubation period average 15-17 days .It is transmitted by respiratory secretions
airborne route & also transmissible in blood and blood products
it an important cause of aplastic crisis in patients with hemolytic anemias like
thalassemia, sickle anemia & spherocytosis. Parvovirus B19 also causes severe fetal
anemia and even hydrops fetalis after primary infection during pregnancy
Clinical Manifestations
1. Parvovirus B19 infections usually begin with a mild prodromal nonspecific illness
characterized by low grade fever, malaise, myalgias, and headache.
2. This illness is followed by the characteristic rash within few days (Erythema
Infectiosum) , which occurs in 3 stages that are not always distinguishable.
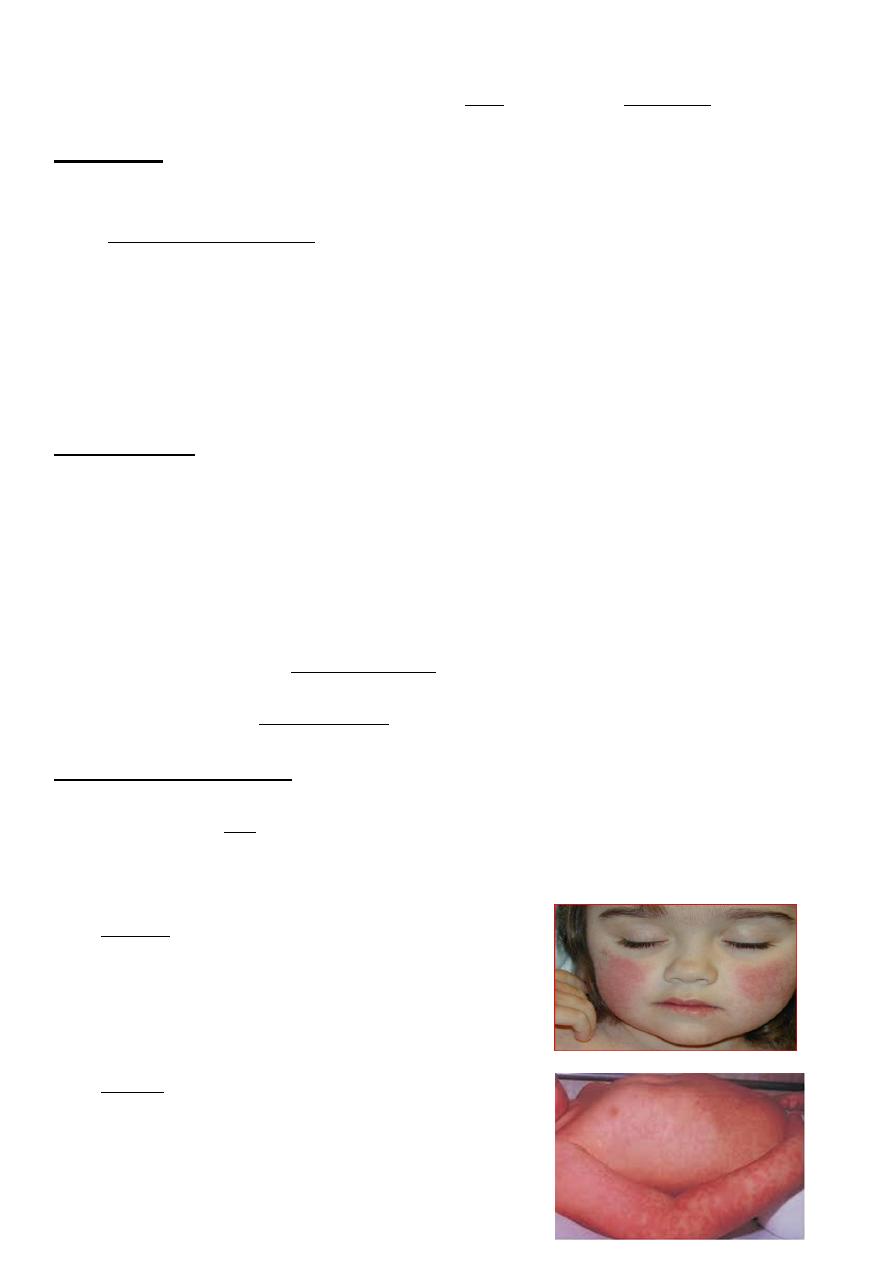
Stage 1: erythematous cheeks, appearing as a
"slapped cheek" rash with circumoral pallor. The
exanthem may appear like a sunburn, occasionally
is
edematous.
Stage 2: an erythematous symmetric,
maculopapular rash appears 1 to 4 days later,
spreading on trunk & proximal extremities (rash
tends to be more prominent on extensor surfaces,
sparing the palms and soles) then fades as central
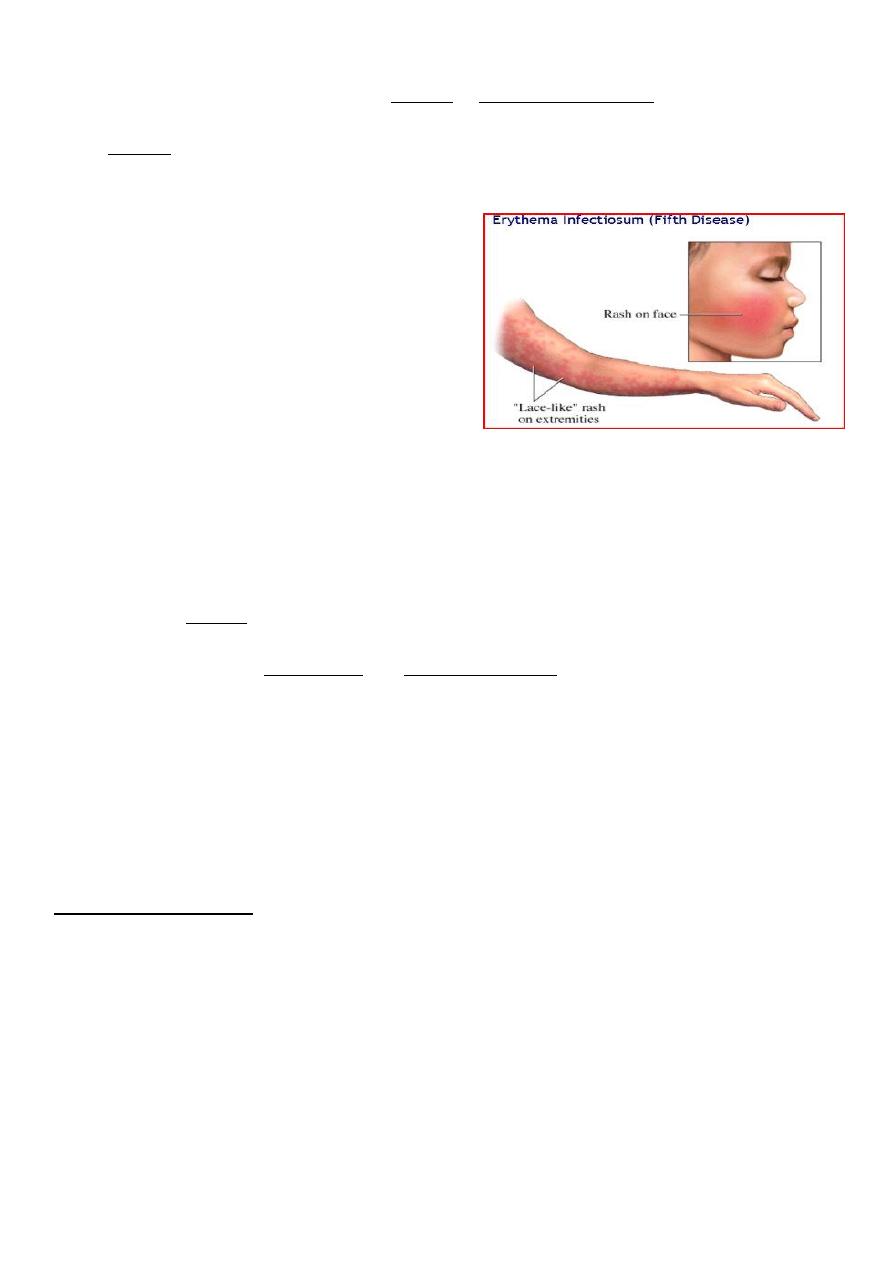
3
clearing takes place, giving a distinctive lacy reticulated rash that lasts 2 to 40 days
(mean 11 days). This rash may be pruritic & does not desquamate.
Stage 3: the rash wax and wane over 1-3 wk on exposure to sunlight, heat, exercise,
bathing, rubbing and stress.
Other features of the rash are as follows:
The rash is often pruritic, especially in adults.
Enanthems are virtually never observed.
The patient is no longer infectious when the
rash appears
3. Arthropathy: joint symptoms are much more common among adults and older
adolescents with B19 infection.
4. Transient Aplastic Crisis: occurs in patients with all types of chronic hemolysis
characterized by ineffective erythroid production typically lasting 7 to 10 days. patients
with aplastic crisis are ill with fever, malaise, and lethargy and have signs and symptoms
of profound anemia, including pallor, tachycardia, and tachypnea. Rash is rarely present.
The reticulocyte count is extremely low, and the hemoglobin level is lower than usual for
the patient. Transient neutropenia and thrombocytopenia also commonly occur.
5. Immunocompromised Persons: chronic anemia is the most common manifestation,
sometimes accompanied by neutropenia, thrombocytopenia, or complete marrow
suppression.
6. Fetal Infection: primary maternal infection is associated with nonimmune fetal hydrops
and intrauterine fetal demise.
Laboratory Studies
Hematologic abnormalities occur with parvovirus infection, including reticulocytopenia
lasting 7 to 10 days, mild anemia, thrombocytopenia, lymphopenia, and neutropenia.
Detection of Parvovirus B19 by
PCR
Electron microscopy of erythroid precursors in the bone marrow.
Serologic tests showing specific IgM antibody to parvovirus are diagnostic,
demonstrating infection that probably occurred in the prior 2 to 4 months.
4
Treatment
There is no specific therapy. Routine supportive care includes maintaining adequate
hydration and antipyretics.
Transfusions may be required for transient aplastic crisis.
Intrauterine transfusion has been performed for hydrops fetalis associated with fetal
parvovirus B19 infection.
IVIG may be used for immunocompromised persons with severe anemia or chronic
infection.
___________________________________
VARICELLA-ZOSTER VIRUS INFECTION
Chickenpox (varicella)
DNA virus that is a member of the herpesvirus family
Humans are the only natural host.
VZV (chickenpox) is highly communicable among susceptible individuals.
It is mild disease in young children but may be severe in adult and in
immunocompromised children.
The period of infectivity to others; ranges from 2 days before to 7 days after the onset
of the rash till when all lesions are crusted and dried.
Epidemiology
In the prevaccine era, the peak age of occurrence was 5 to 10 years.
In the postvaccine era, the incidence of varicella has declined in all age groups, with
the peak incidence now in 10 to 14 year olds.
Peak seasonal infection in late winter and spring.
Transmission is by direct contact, droplet, and air.
Clinical Manifestations
The incubation period of varicella is generally 14 to 16 days.
Prodromal symptoms of fever, malaise, and anorexia, running nose may precede the
rash by 1 day.
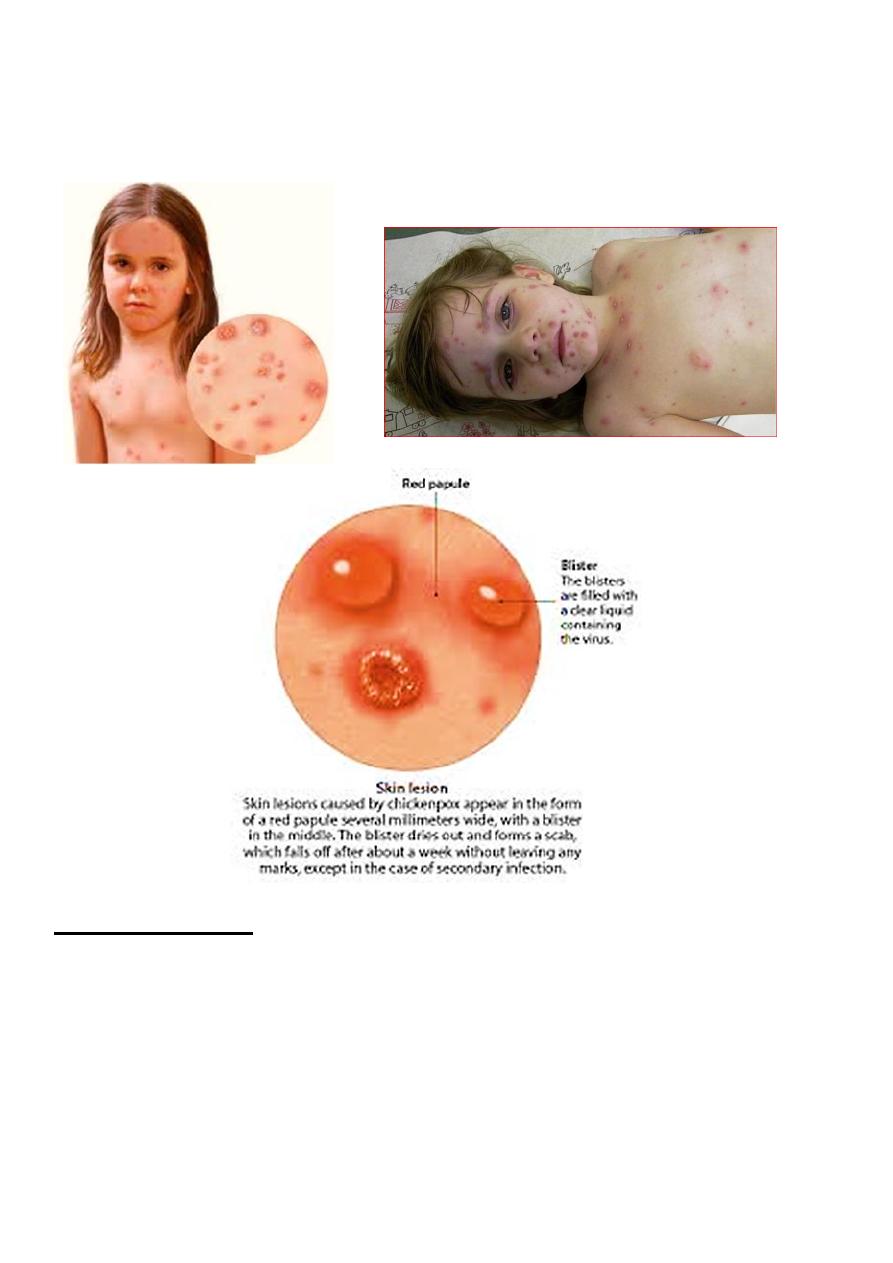
The characteristic rash appears initially as small red papules that rapidly progress to
oval, "teardrop" vesicles on an erythematous base. The fluid progresses from clear to
cloudy, and the vesicles ulcerate, crusted, and dried and heal. New crops appear in 3 to
4 days, usually beginning on the trunk followed by the head, the face, and, less
commonly the extremities, with all stages of lesions being present at the same
time(crop). Pruritus is universal.
Lesions may be present on mucous membranes.
5
Lymphadenopathy may be generalized.
The severity of the rash varies, as do systemic signs and fever, which generally abate
after 3 to 4 days.
Laboratory Studies
Laboratory testing confirmation for diagnosis is usually unnecessary.
PCR is the current diagnostic method of choice, and genotyping to distinguish vaccine
and wild-type strains is available through the CDC.
Detection of varicella-specific antigen in vesicular fluid by immunofluorescence using
monoclonal antibodies or demonstration of a fourfold antibody increase of acute and
convalescent sera is also diagnostic but not as sensitive as PCR.
6
Treatment
Symptomatic therapy of varicella includes nonaspirin antipyretics, cool baths, and
careful hygiene.
Routine oral administration of acyclovir is not recommended in otherwise healthy
children with varicella.
Indication of antiviral (acyclovir) therapy:
1. Early therapy with antivirals (especially within 24 hours of rash onset) in
immunocompromised persons is effective in preventing severe complications,
including pneumonia, encephalitis, and death from varicella.
2. Acyclovir or valacyclovir may be considered in those at risk of severe varicella,
such as:
unvaccinated persons older than 12 years.
those with chronic cutaneous or pulmonary disease.
receiving short course, intermittent, or aerosolized corticosteroids.
receiving long-term salicylate therapy.
Complications
1. Varicella is a more severe disease for neonates, adults, and immunocompromised
persons.
2. Secondary infection of skin lesions by streptococci or staphylococci is the most
common complication. Hemorrhagic lesions may occur, known as varicella
gangrenosa .
3. Pneumonia is uncommon in healthy children but occurs more in healthy adults and
immunocompromised persons.
4. Myocarditis, pericarditis, orchitis, hepatitis, ulcerative gastritis,
glomerulonephritis, and arthritis may complicate varicella.
5. Reye syndrome may follow varicella; thus, salicylate use is contraindicated during
varicella infection.
6. Neurologic complications frequently include postinfectious encephalitis, cerebellar
ataxia & Guillain-Barre syndrome.
Prevention
Children with chickenpox should not return to school until all vesicles have crusted.
A hospitalized child with chickenpox should be isolated to prevent transmission.
A live attenuated varicella vaccine—two doses for all children— is recommended.
The first dose should be administered at age 12 to 15 months and the second dose at 4
to 6 years.
Varicella vaccine is 85% effective in preventing any disease and 97% effective in
preventing moderately severe and severe disease.
Passive immunity can be provided by VZIG, which is indicated within 4 days of
exposure for susceptible individuals at increased risk for severe illness. It is
recommended for:
7
1. immunocompromised children
2. pregnant women
3. newborns exposed to varicella.
4. Hospitalized premature infants born at ≥28 weeks of gestation whose mothers
do not have evidence of immunity to varicella.
5. Hospitalized premature infants born at <28 weeks of gestation or who weigh
≤1,000 g at birth, regardless of their mothers' evidence of immunity to varicella.
6. ≥15 yr and older, who are exposed to infection.
Zoster (shingles)
It is the manifestation of reactivated latent infection of endogenous VZV.
Zoster is transmitted by direct contact.
Only 5% of cases of zoster occur in children younger than 15 years of age, with 75%
of cases occurring after 45 years of age. The incidence of zoster is increased in
immunocompromised persons.
Clinical Manifestations
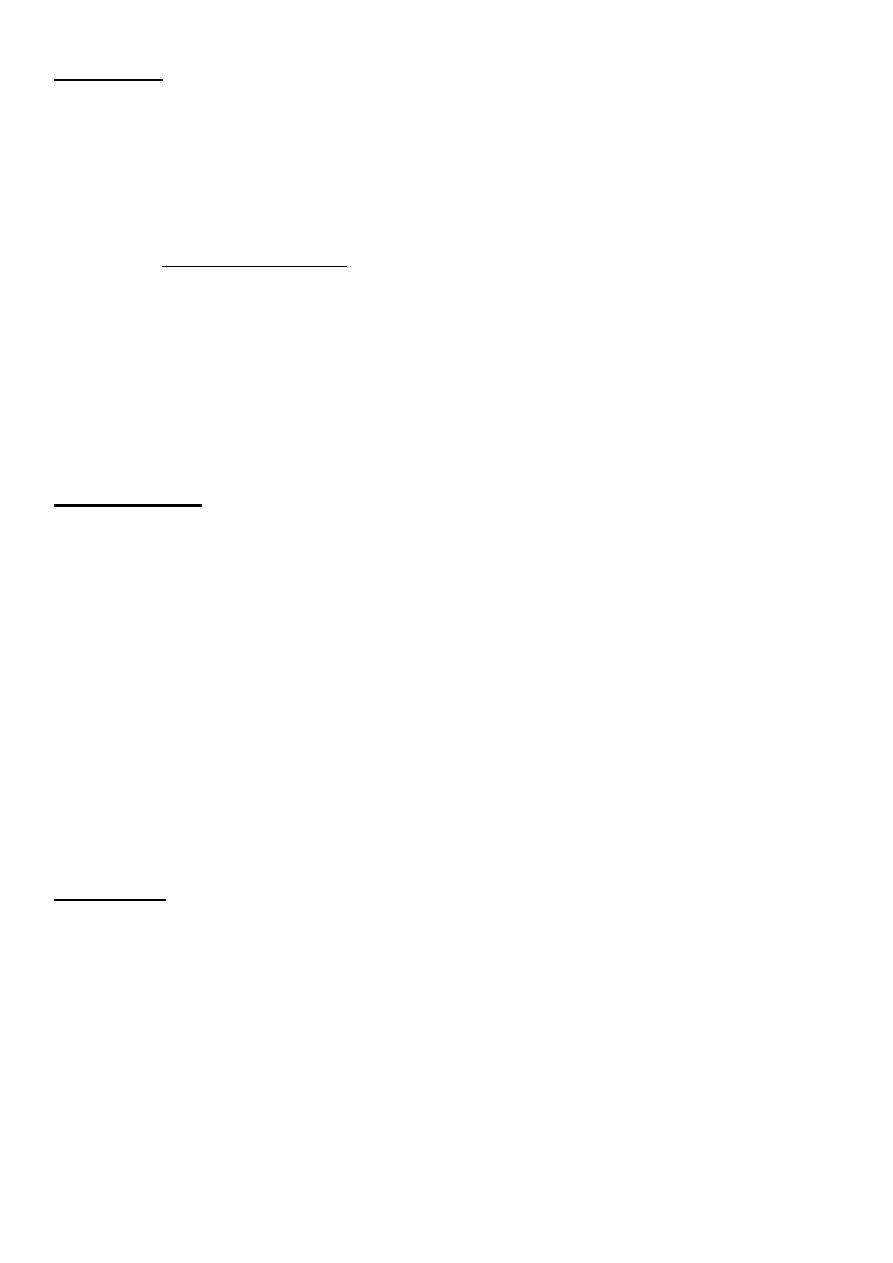
The preeruption phase of zoster includes intense localized and constant pain and
tenderness (acute neuritis) along a dermatome, accompanied by malaise and fever.
In several days, the eruption of papules, which quickly vesiculate, occurs in the
dermatome or in two adjacent dermatomes. Groups of lesions occur for 1 to 7 days
and then progress to crusting and healing.
Thoracic and lumbar regions are typically involved.
Lesions generally are unilateral and are accompanied by regional lymphadenopathy.
Any branch of cranial nerve V may be involved, which also may cause corneal and
intraoral lesions. Involvement of cranial nerve VII may result in facial paralysis and
ear canal vesicles (Ramsay Hunt syndrome). Ophthalmic zoster may be associated
with ipsilateral cerebral angiitis and stroke.
Immunocompromised persons may have unusually severe, painful herpes zoster that
involves cutaneous and, rarely, visceral dissemination (to liver, lungs, and central
nervous system).
Postherpetic neuralgia, defined as pain persisting longer than 1 month, is uncommon
in children.
8
Treatment
Antiviral treatment of zoster accelerates cutaneous healing, hastens the resolution of
acute neuritis, and reduces the risk of postherpetic neuralgia.
Acyclovir is recommended for children.
congenital varicella
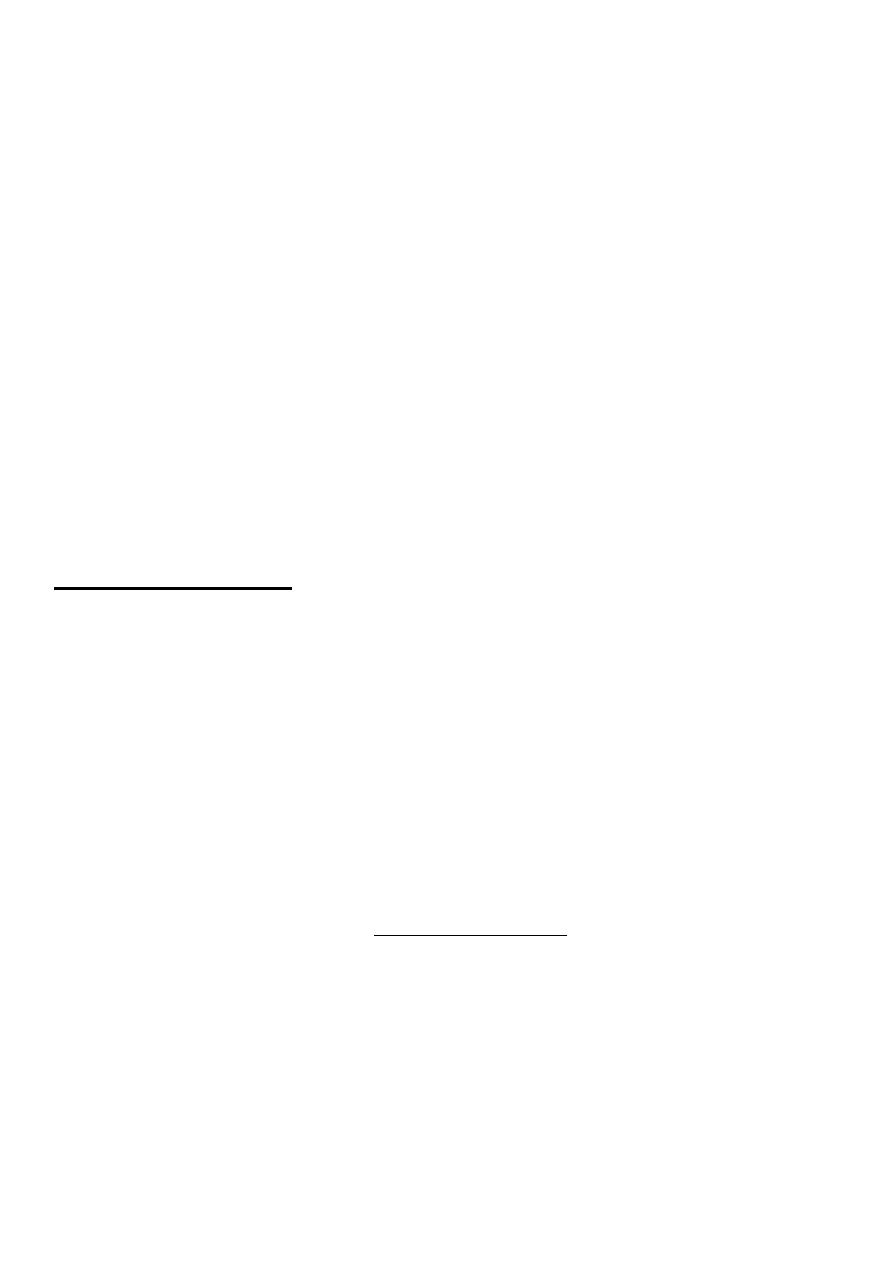
Fetal varicella during first 6 months of pregnancy includes followings pathological
effects: low birth wt, cortical brain atrophy, mental retardation, cataract,
microcephaly, cicatrical scarring of body and limbs with aplasia of fingers and toes
.
