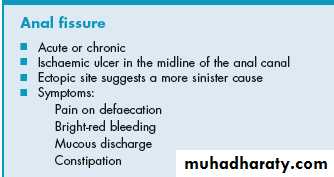
ANAL FISSURE
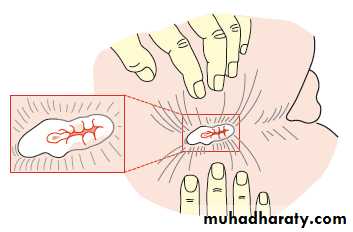
DefinitionAn anal fissure (synonym: fissure-in-ano) is a longitudinal split in the anoderm of the distal anal canal which extends from the anal verge proximally towards, but not beyond, the dentate line.
90% located in
Midline posterior
Aetiology
Classically, acute anal fissures arise from the trauma caused by the strained evacuation of a hard stoolor, less commonly, from the repeated passage of diarrhoea.
The location in the posterior midline perhaps relates to the exaggerated shearing forces acting at that site at defaecation,combined with a less elastic anoderm.
Anterior anal fissure is much more common in women and may arise following vaginal delivery.
Clinical features
Men and women are affected equally.Anterior fissures account for about 10 per cent of those encountered in women, but only 1 per cent in men.
acute anal fissures are characterised by severe anal pain associated with defaecation.
as well as the passage of fresh blood, normally noticed on the tissue after wiping.
When chronic, patients may also complain of itching secondary to irritation from the sentinel tag, discharge from the ulcer
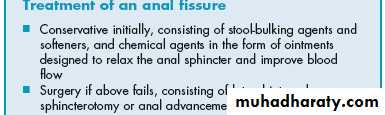
Treatment
Emphasis must be placed on normalisation of bowel habitsThe addition of fibre to the diet to bulk up the stool, stool softeners and adequate water intake are simple and helpful measures.
Warm baths and topical local anaesthetic agents relieve pain;
topical application of pharmacological agents that relax the internal sphincter,
most commonly nitric oxide donors (by reducing spasm, pain is relieved, and increased vascular perfusion promotes healing).Such agents include glyceryl trinitrate (GTN) 0.2 %applied four times per day to the anal margin (although this may cause headaches) and
diltiazem cream 2 % applied twice daily.
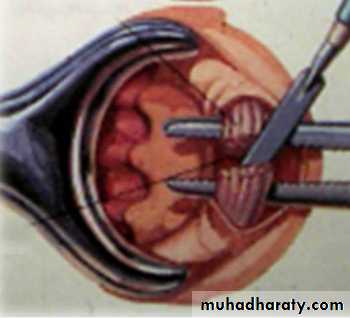
Operative measures
Lateral anal sphincterotomythe internal sphincter is divided away from the fissure itself – usually either in the right or the left lateral positions
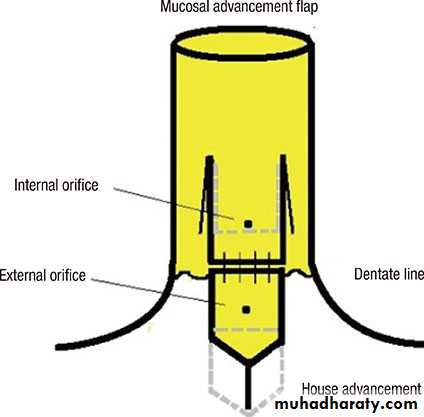
Anal advancement flap
After excision of the edges of the fissure , an inverted house-shaped flap of perianal skin is carefully mobilised on its blood supply and advanced without tension to cover the fissure, and then sutured
HAEMORRHOIDS
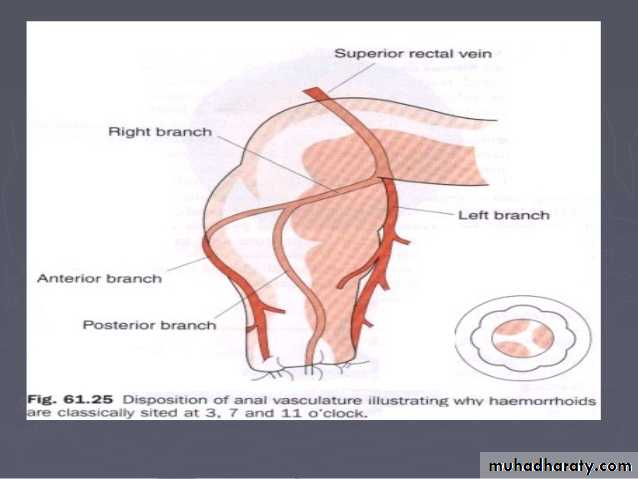
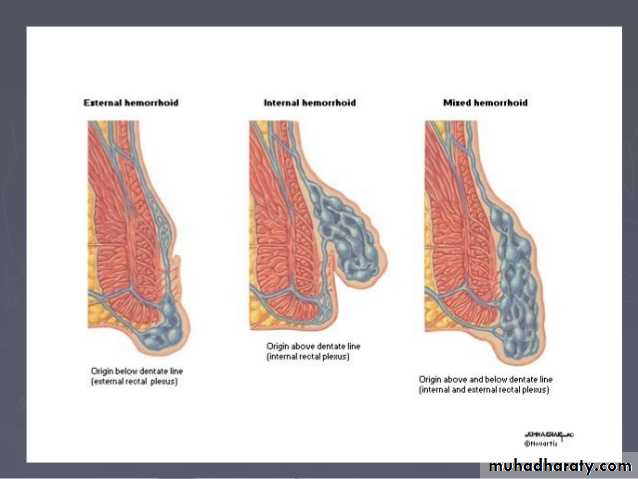
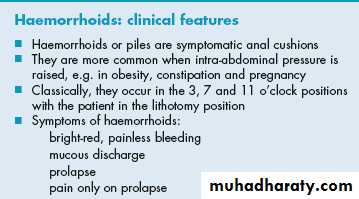
Internal haemorrhoids (Greek: haima, blood; rhoos, flowing; synonym: piles, Latin: pila, a ball) are symptomatic anal cushions and characteristically lie in the 3, 7 and 11 o’clock positions (with the patient in the lithotomy position).External haemorrhoids relate to venous channels of the inferior haemorrhoidal plexus deep in the skin surrounding the anal verge
Theories of development
Portal hypertension and varicose veinsInfection
Diet and stool consistency
Anal hypertonia
Ageing
Current view : Shearing forces acting on the anus (for a variety of reasons) lead to caudal displacement of the anal cushions and mucosal trauma. With time, fragmentation of the supporting structures (a normal consequence of ageing, but perhaps accelerated in those with haemorrhoids) leads to loss of elasticity of the cushions such that they no longer retract following defaecation
Clinical features
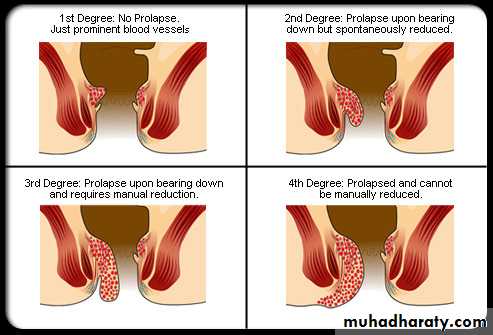
Bleeding, {usually painless} is the principal and earliest symptom. The nature of the bleeding is characteristically separate from the motion and is seen either on the paper on wiping or as a fresh splash in the pan. Sometimes , the bleeding may be sufficient to cause anaemia.Piles associated with bleeding alone are called first-degree haemorrhoids
Patients may complain of true ‘piles’, lumps that appear at the anal orifice during defaecation and which return spontaneously afterwards (second-degree haemorrhoids),
piles that have to be replaced manually (third-degree haemorrhoids)
or piles that lie permanently outside (fourth-degree haemorrhoids).
Management
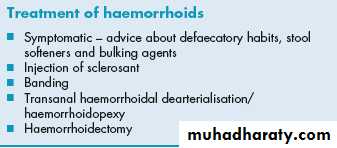
Exclusion of other causes of rectal bleeding, especially colorectal malignancy, is the first priority.normalising bowel and defaecatory habits:
stool softeners and bulking agents.
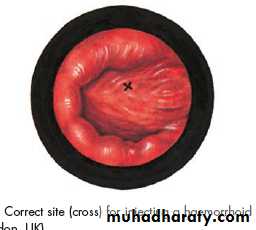
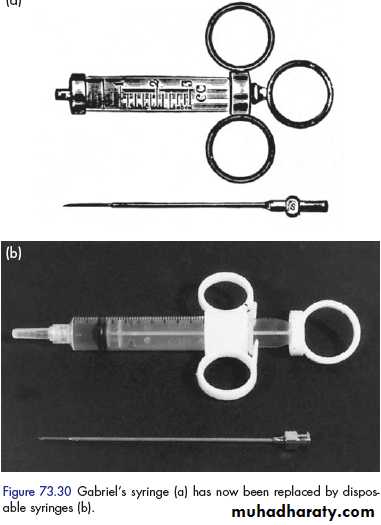
In those with first- or second-degree piles whose symptoms are not improved by conservative measures, injection sclerotherapy the submucosal injection of 5 % phenol in arachis oil or almond oil, may be advised.
injection sclerotherapy
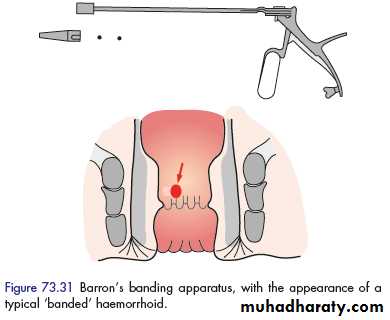
The Barron’ bander is a commonly available device used to slip tight elastic bands onto the base of the pedicle of each hemorrhoid The bands cause ischaemic necrosis of the piles{ 2nd degree hemorrhoid } .
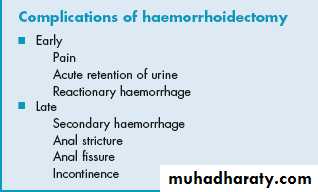
Operation
IndicationsThe indications for haemorrhoidectomy include:
• third- and fourth-degree haemorrhoids;
• second-degree haemorrhoids that have not been cured by non-operative treatments;
• fibrosed haemorrhoids;
• interoexternal haemorrhoids when the external haemorrhoid is well defined.
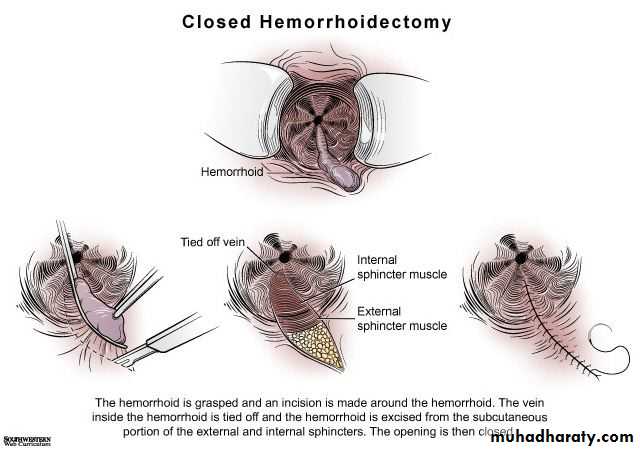
Open and closed hemorroidectomy
Closedopen
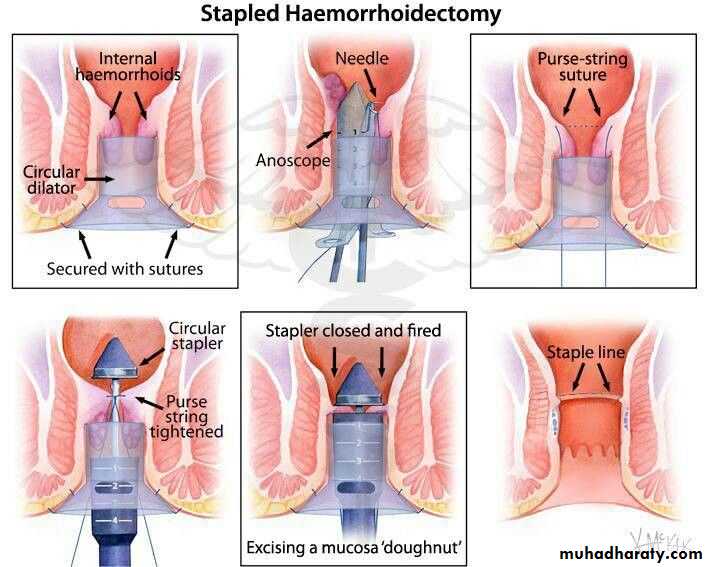
stapled haemorrhoidopexy
utilises a purpose-designed stapling gunThis procedure excises a strip of mucosa and submucosa (together with the vessels travelling within them) circumferentially, well above the dentate line
Transanal haemorrhoidal dearterialisation
is used for the treatment of second- and third-degree haemorrhoids. Some have recently advocated transanal Doppler-guided ligation of those vessels feeding the haemorrhoidal masses, to which others have added suture ‘mucopexy’ to deal with any prolapseExternal haemorrhoids
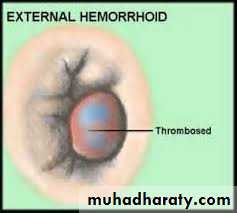
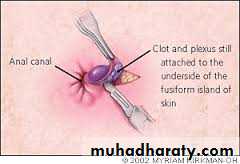
A thrombosed external haemorrhoid relates anatomically to the veins of the superficial or external haemorrhoidal plexus and is commonly termed a ‘perianal haematoma’.It presents as a
sudden onset, olive-shaped, painful blue subcutaneous swelling at the anal margin and is usually consequent upon straining at stool, coughing or lifting a heavy weight
If the patient presents within the first 48 hours, the clot may be evacuated under local anaesthesia.
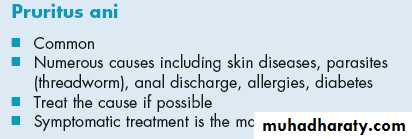
PRURITUS ANI
This is intractable itching around the anus, a common and embarrassing condition. Usually, the skin is reddened and hyperkeratotic and it may become cracked and moist.Causes
Lack of cleanliness,anal or perianal discharge
Vaginal discharge
Parasitic causes. Threadworms should be excluded,
Epidermophytosis
Allergy
Skin diseases
psychoneurosis. And Diabetes
Treatment
The cause is treated. Symptomatic treatment includes the following:• Hygiene measures.
Hydrocortisone. In patients with dermatitis
Strapping the buttocks keeps moist opposing surfaces apart,
Operative treatment :This may be necessary for a concomitant lesion of the anorectum