Motility disorders
Achalasia of the oesophagus
Pathophysiology
Achalasia is characterised by:
a hypertonic lower oesophageal sphincter, which fails to relax in response to the
swallowing wave
failure of propagated oesophageal contraction, leading to progressive dilatation of the
oesophagus.
The cause is unknown. Defective release of nitric oxide by inhibitory neurons in the lower
oesophageal sphincter has been reported, and there is degeneration of ganglion cells within the
sphincter and the body of the oesophagus.
Loss of the dorsal vagal nuclei within the brainstem can be demonstrated in later stages.
Infection with Trypanosoma cruzi in Chagas’ disease causes a syndrome that is clinically
indistinguishable from achalasia.
Clinical features
The presentation is with dysphagia. This develops slowly, is initially intermittent, and is worse
for solids and eased by drinking liquids, and by standing and moving around after eating.
Heartburn does not occur because the closed oesophageal sphincter prevents gastro-
oesophageal reflux. Some patients experience episodes of chest pain due to oesophageal
spasm. As the disease progresses, dysphagia worsens, the oesophagus empties poorly and
nocturnal pulmonary aspiration develops. Achalasia predisposes to squamous carcinoma of the
oesophagus.
Investigations
Endoscopy should always be carried out because carcinoma of the cardia can mimic the
presentation and radiological and manometric features of achalasia (‘pseudo-achalasia’).
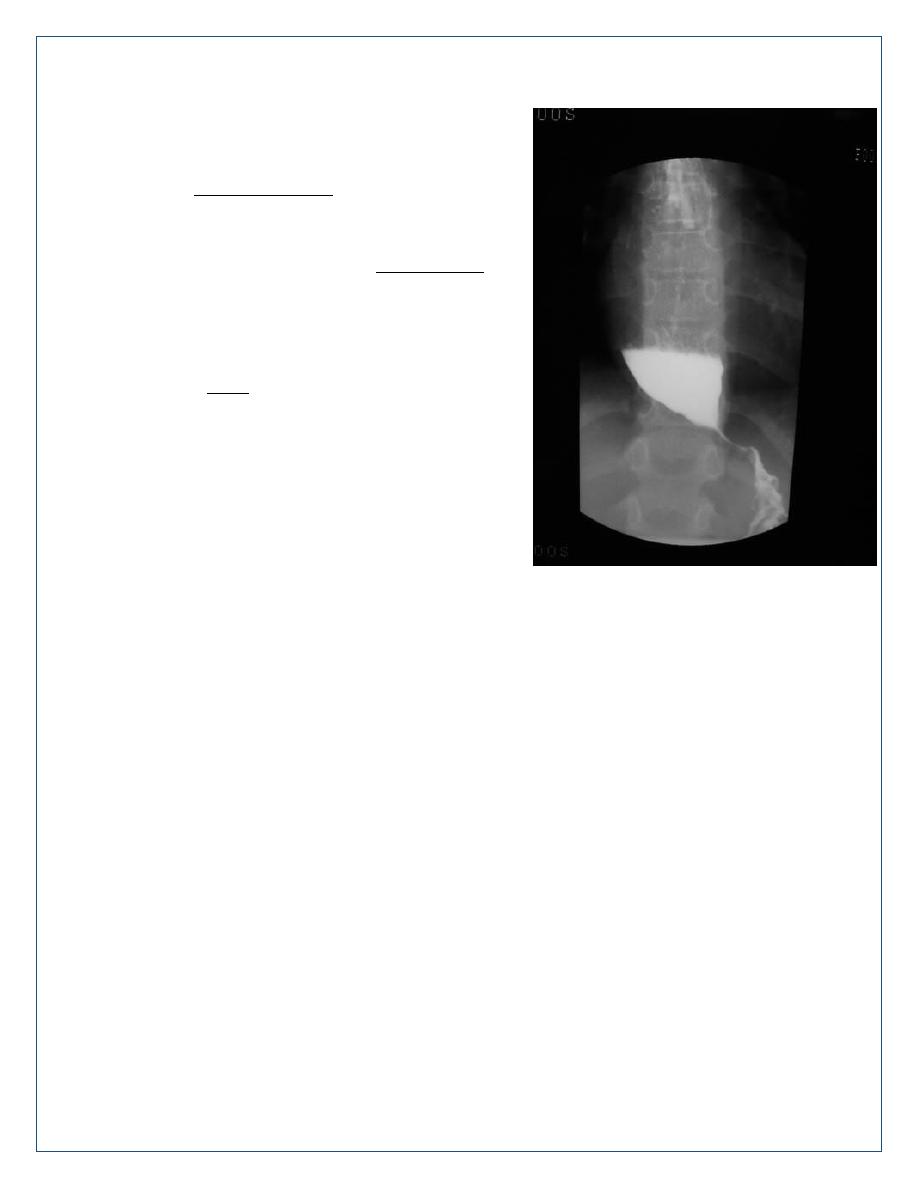
A barium swallow shows tapered narrowing of the lower oesophagus and, in late disease, the
oesophageal body is dilated, aperistaltic and foodfilled.
Manometry confirms the highpressure, non-relaxing lower oesophageal sphincter with poor
contractility of the oesophageal body.
Management
Endoscopic
Forceful pneumatic dilatation fluoroscopically positioned
balloon disrupts the oesophageal sphincter and improves
symptoms in 80% of patients.
Endoscopically directed injection of botulinum toxin into
the lower oesophageal sphincter induces clinical
remission but relapse is common.
Recently, a complex endoscopic technique has been
developed in specialist centres (peroral endoscopic
myotomy, POEM).
Surgical
Surgical myotomy (Heller’s operation), performed either
laparoscopically or as an open operation, is effective but
is more invasive than endoscopic dilatation.
Both pneumatic dilatation and myotomy may be
complicated by gastro-oesophageal reflux, and this can
lead to severe oesophagitis because oesophageal
clearance is so poor. For this reason, Heller’s myotomy is accompanied by a partial
fundoplication anti-reflux procedure. PPI therapy is often necessary after surgery.
