Normal physiology and microecology of the vagina:
The vagina is lined by nonkeratinized squamous epithelium which is powerfully
influenced by oestrogen and progesterone.
The vagina of the new born is colonized by aerobic and anaerobic bacteria acquired
while passing through the birth canal. The newborn’s vaginal epithelium is strongly
estrogenized and rich in glycogen,which supports the growth lactic acid producing
lactobacilli,this result in low PH<4.5,further support the growth of acidophilic
protective microflora. Within days of delivery,oestrogen decreases ,the epithelium
become thin ,atrophic and devoid of glycogen.the vaginal PH rises,and the
predominant vaginal flora becomes diverse gram positive cocci and bacilli .
With the onset of puberty and steroidogenesis, the vagina become estroginized,and
the glycogen content increases,lactobacilli become predominant with self sustained
vaginal PH(3.5-4.5) providing some protection from STIs including HIV ,even
though a wide variety of aerobic and anaerobic bacteria can be cultured from the
normal vagina and at any time a women can harbor at least 3 -8 type of bacteria.
Gynecology Zakho hospital
Dr.Asmaa December 5, 2016
Reproductive Tract infection

2
Multiple factors alter this protective microflora, as:
1. .antibiotics suppress the growth of commonsal organisms allowing pathogenic strains
to be predominant(yeast).
2. .douching with water or non buffered solutions may transiently alter the PH or
selectively suppress the endogenous bacteria.
3. .Sexual intercoarse with introduction of semen raises PH to 7.2 to 6-8 hours ,also the
vaginal transudate during coitus as
4. Lubricant increase vaginal PH (7.4) which also favor abnormal flora.
5. The presence of foreign body in the vagina in children and the presence of forgotten
tampon and diaphragm in adult disturbs normal vaginal cleansing mechanisms and
may lead to secondary infection.
Physiologic vaginal fluid:
is mainly composed of proteins ,polysaccharides, aminoacids, enzymes, and
immunoglobulines.
Vaginal fluid is a mixture of (source):
Cervical fluid secretion(major component).
Endometrial fluid.
Oviductal fluid.
Excudate from the bartholine’s gland and skene’s.
Transudate from vaginal squamous epithelium, squamous cell it self,and
metabolic product of the microflora.
3
Physiologically the vaginal and endocervical fluid increases during:
Pregnancy.
Mid cycle
Intercoarse.
The vaginal fluid become markedly reduced in post-menopausal women.
Etiology of vaginal discharge:
1. Up to 90% of cases are caused by 3 conditions:
2. bacterial vaginosis(40%-50%)
3. -vulvovaginal candidiasis(20%-25%)
4. -trichomoniasis(15%)
Others :
mucopurulant
cervicitis
caused
by
chlamydia,neisseria
gonorrhoea,mycoplasma or BV associated bacteria
Atrophic
vaginitis(over
growth
with
aerobic
anaerobic
bacteria)less common.
Foreign body vaginitis.
Genital ulcer disease as herpes and syphilis.
Desquamative vaginitis.
Lichen planus.
Irritation from sexual activity.
Irritation from allergen containing substanses.
Fistula(urinary or faecal )
4
Bacterial vaginosis:
Is the most common cause of vaginal discharge and in many case is the only
symptoms.
It’s mainly caused by disruption of normal healthy vaginal lactobacillus
(hydrogen peroxide producing)flora(lactobacillus jensenii and lactobacillus
crispatus) and an overgrowth of predominantly anaerobic bacteria. Anaerobic
bacteria can be found in less than 1% of the flora of normal women. In women
with BV, the concentration of anaerobes, and G. vaginalis and Mycoplasma
hominis, is 100 to 1000 times higher than in normal women ..
most common organisms involved in BV:
Garderella vaginalis,
genital mycoplasmas(mycoplasma hominis,mycoplasma urealyticum)
Vaginal anaerobic bacteria as:prevotella, bacteroids, mobiluncus species
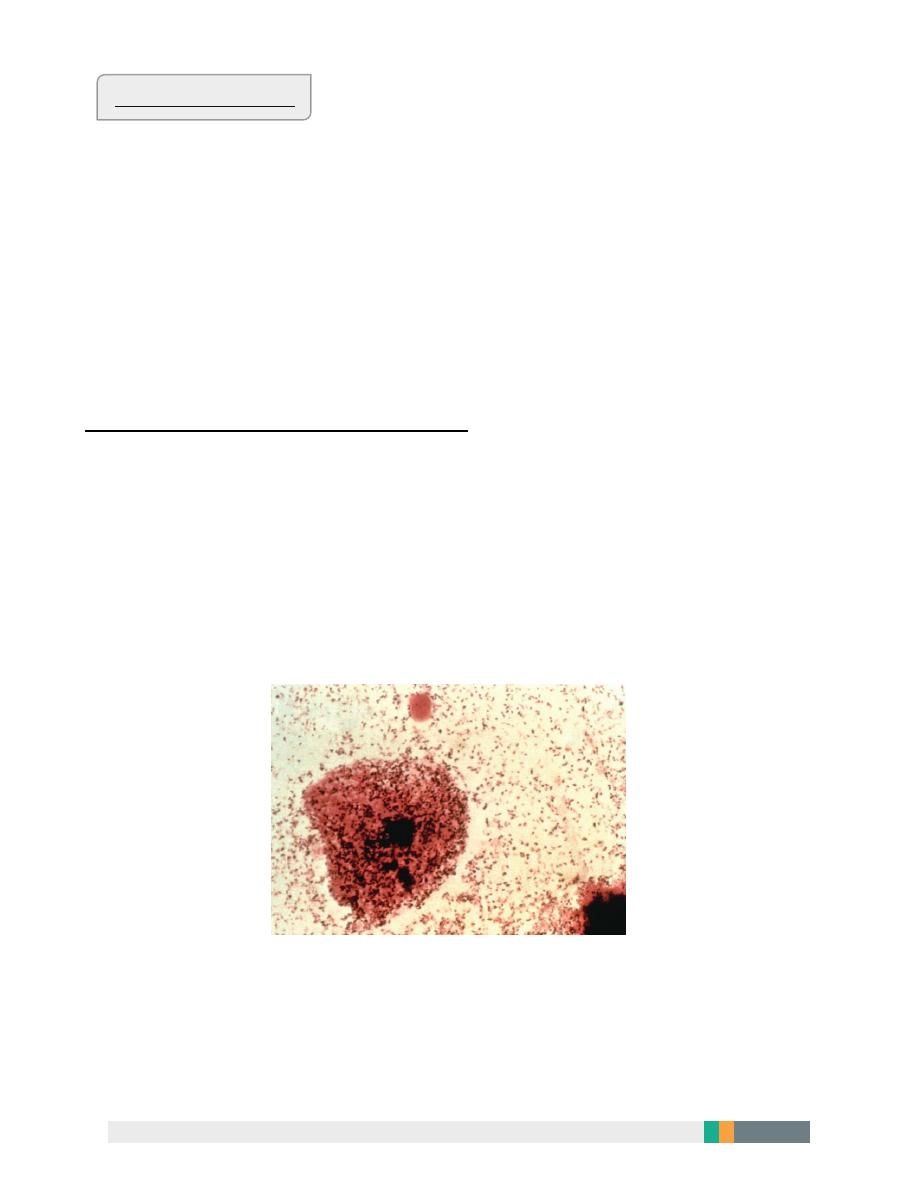
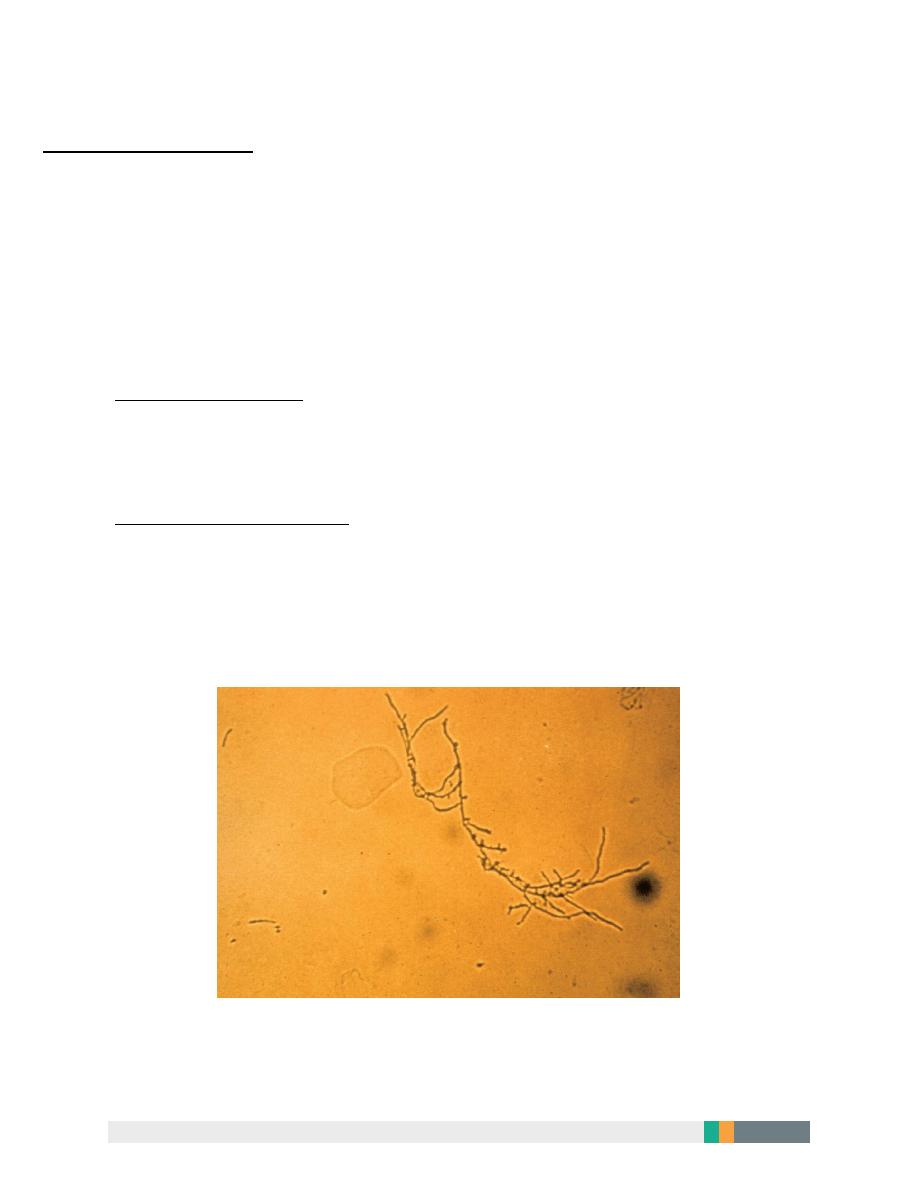
a clue cell, which is an epithelial cell with “serrated” edges caused by bacteria (arrows).
5
Risk factors of bacterial vaginosis:
New sexual partner.
Smoking.
Intrauterine device use.
Frequent douching
Clinical features of bacterial vaginosis:
A profuse , milky, non adherent discharge that demonstrate an amine or fishy
odour after alkalization with a drop of KOH(positive whiff test).
Risk from having bacterial vaginosis:
pelvic inflammatory disease (PID),
-postabortal PID,
-postoperative cuff infections after hysterectomy,
-abnormal cervical cytology.
-Pregnant women with BV are at risk for premature rupture of
the membranes, preterm labor and delivery, chorioamnionitis,
post cesarean endometritis.
Partner treatment is generally not Recommended.
6
Office-based testing is required to diagnose BV.
a microscopy of a clue cell.
The addition of potassium hydroxide to the vaginal secretions (the “whiff” test)
releases a fishy, amine-like odor.
Clinicians who are unable to perform microscopy can use alternative
diagnostic tests such as a pH and amines test card,
detection of G. vaginalis ribosomal RNA,
Gram stain. Culture of G. vaginalis is not recommended as a diagnostic tool
because of its lack of specificity.
Treatment of bacterial vaginosis
Metronidazole 500 mg orally twice a day for 7 days.
OR Metronidazole gel 0.75%, one full applicator (5 g) intravaginally , once a day
for 5 days
OR Clindamycin cream 2%, one full applicator (5 g) intravaginally at bedtime for
7 days

7
Vulvovaginal candidiasis:
It’s the second most common cause of vulvovaginal related symptoms.
Candida albicans cause more than 90% of cases formerly ,
Now less azole susceptible species such as candid glabrata recognized as
causative agent in 15% of cases..those less susceptible yeast require prolonged or
alternative treatments.
Candida’s require oestrogenated tissues so VVC becomes more common after
menarche and less common after menopause.
An estimated 75% of women acquire Vulvo-
vaginal candidiasis sometimes in their life .
5% suffer frequent symptomatic recurrence (more than 5 attacks/year)
Risk factors for recurrent VVC include :
High oral contraceptive pills.
Diaphragm use with spermicide.
Diabetes mellitus.
Antibiotic use .
Pregnancy.
Immunosuppression from any cause (HIV,Aids,/ transplantation ,steroid use)
Tight occlusive clothing.
8
Clinical presentations
Vaginal itching.
Burning sensation.
Irritation.
Post voiding dysuria.
The discharge is odorless ,PH less than 4.7,thick or crudy with the appearance
of cottage cheese.
Examination shows vulvovaginal erythema with evidence of acute or chronic
excoriation.
Microscopic examination of a wet –mount preperation is positive for budding
yeast cells,pseudohyphae or myceleal tangles in 50%-70% of cases..women with
clinical suggestion with absent wet preparation evidence may benefit from
,,fungal culture.
9
Treatment of vulvovaginal candidiasis
Treatment of the underlying cause
Over the counter antifungal treatment:
Clotrimazole 1% cream 5 g intravaginally for 7-14 days OR
Clotrimazole 2% cream 5 g intravaginally for 3 days OR
Miconazole 2% cream 5 g intravaginally for 7 days OR
Miconazole 4% cream 5 g intravaginally for 3 days OR
Miconazole 100 mg vaginal suppository, one suppository for 7 days OR
Miconazole 200 mg vaginal suppository, one suppository for 3 days OR
Miconazole 1200 mg vaginal suppository, one suppository for 1 day OR
Tioconazole 6.5% ointment 5 g intravaginally in a single application
Prescription Intravaginal Agents Butoconazole 2% cream (single dose
bioadhesive product), 5 g intravaginally for 1 day
OR Terconazole 0.4% cream 5 g intravaginally for 7 days
OR Terconazole 0.8% cream 5 g intravaginally for 3 days
OR Terconazole 80 mg vaginal suppository, one suppository for 3 days
Oral Agent:
Fluconazole 150 mg oral tablet, one tablet in single dose .
10
Treatment of recurrent V VC
First line treatment is or oral antifungal regimen consists of inducing a
remission of chronic symptoms with fluconazole (150 mg every 3 days for
three doses), then maintaining a suppressive dose of this agent (fluconazole,
150 mg weekly) for 6 months. On this regimen, 90% of women with RVVC will
remain in remission
In recurrent cases may be treated after confirming the diagnosis with weekly
suppressive doses of topical imidazoles.
Boric acid (600mg vaginal gelatin capsules)3 times daily for 1 week is an effective
treatment for imidazole resistant species.
VVC is not sexually transmitted in most cases male partners sometimes reinfect
their partners and may be required to be treated.
Trichomoniasis :
It’s caused by protozoan trichomonas vaginalis.
Trichomoniasis is a cause of cervicitis vaginitis ,and urethritis.and upper
reproductive tract symptoms,
increased risk of adverse pregnancy outcome (prematurity,low birth weight)
increased transmission of HIV infection.
About 50% of cases in women and men are asymptomatic.
Symptomatic infection is classically manifested
by a green-yellow ,frothy vaginal discharge with a musty odor.
dyspareunia ,vulvovaginal irritation and occasionally dysuria may be present.

11
In patients with high concentrations of organisms, a patchy vaginal erythema
and colpitis macularis (“strawberry” cervix) may be observed. Microscopy of
the secretions may reveal motile trichomonads and increased numbers of
leukocytes.
Male partners are often asymptomatic even though they demonstrate non gonococcal
urethritisp on direct examination.
Couples with trichomoniasis should be screened for other STIs and empiric treatment
of partners.
Diagnosis :clinical features
Saline wet mount to see the characteristic motility of the trichomonas.
Culture is more sensitive.
Polymerase chain reaction .
Antigen testing.

12
Treatment:
Metronidazole 2 gm single oral treatment is a recommended.(not take alcohol 2
days sfter treatment)
Multidose treatment 500mg twice daily for 7 days,,,bothe single and multiple
therapy is effective in 95% of cases.
Metronidazole resistance should be treated by tinidazole,or higher doses of
metronidazole 2 gm daily for 7 days.
A.L.Y

13
