ANOMALIES AND INJURIES
OF THE BLADDER
Dr. Ali Wafaa Al-Wefy

Congenital anomalies of the bladder
• Agenesis:
both ureters are obstructed and the condition is not
compatible with life.
• Duplication:
very rarely the bladder is divided by a septum either in
the midline or lying transversely.
• Patent urachus:
the urachus may remain patent and leak urine at the
umbilicus with the risk of infection and metaplasia of the bowel
epithelium that lines the urachus.
• Exstrophy:
also known as ectopia vesicae, is a congenital anomaly
that exists along the spectrum of the exstrophy –epispadias complex
and most notably involves protrusion of the urinary bladder through a
defect in the abdominal wall.

Historical Aspects
• In older texts, the first account of bladder
exstrophy was ascribed to Assyrian-Babylonian
sources dating from the first and second
millennia BCE. At that time, birth anomalies in
both humans and animals were carefully recorded
on tablets for their importance as omens, based
on their interpretation by divination experts.

Bladder exstrophy-epispadias complex
Three main presentations of the bladder exstrophy-
epispadias complex:
1. Classic bladder exstrophy
2. cloacal exstrophy
3. epispadias

• Exstrophy of the bladder is part of a spectrum of
anomalies involving the
urinary tract
, the
genital tract
,
the
musculoskeletal
system, and sometimes the
intestinal tract
.
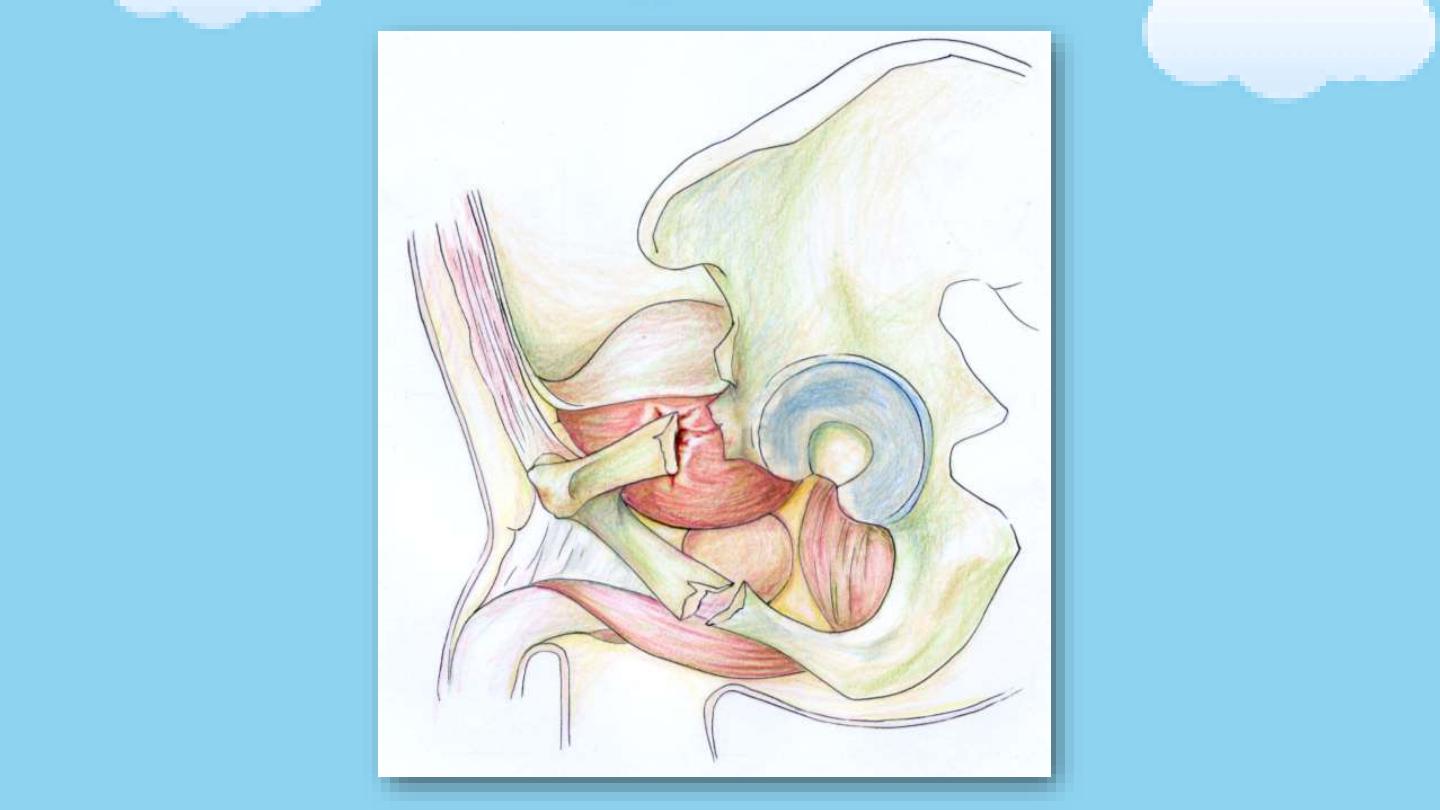
CLASSIC BLADDER EXSTROPHY
• In classic bladder exstrophy (CBE), most anomalies are related to
defects of the:
• Abdominal wall: indirect inguinal hernia
• Bladder: bladder open anteriorly and the mucosa is fused with the
skin.
• Genitalia: short vagina, bifid clitoris, separation of crura, epispadias
• Pelvic bones: separation of symphysis pubis, external rotation of iliac
wings
• Anorectal: anus displaced anteriorly.

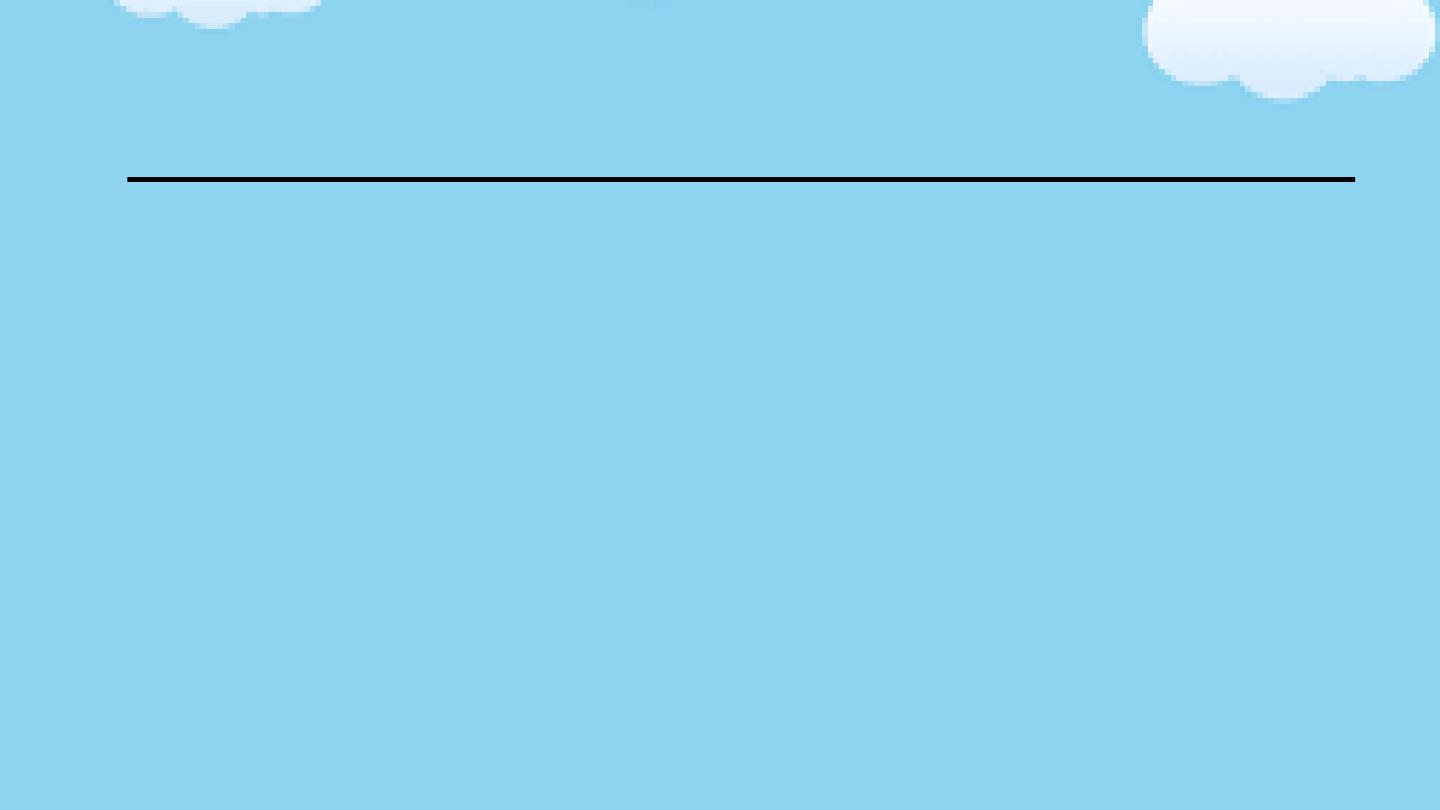
Surgery
• Functional bladder closure immediately after birth
• Bladder neck reconstruction for continence
• Genitoplasty: repair of epispadias, vaginal reconstruction
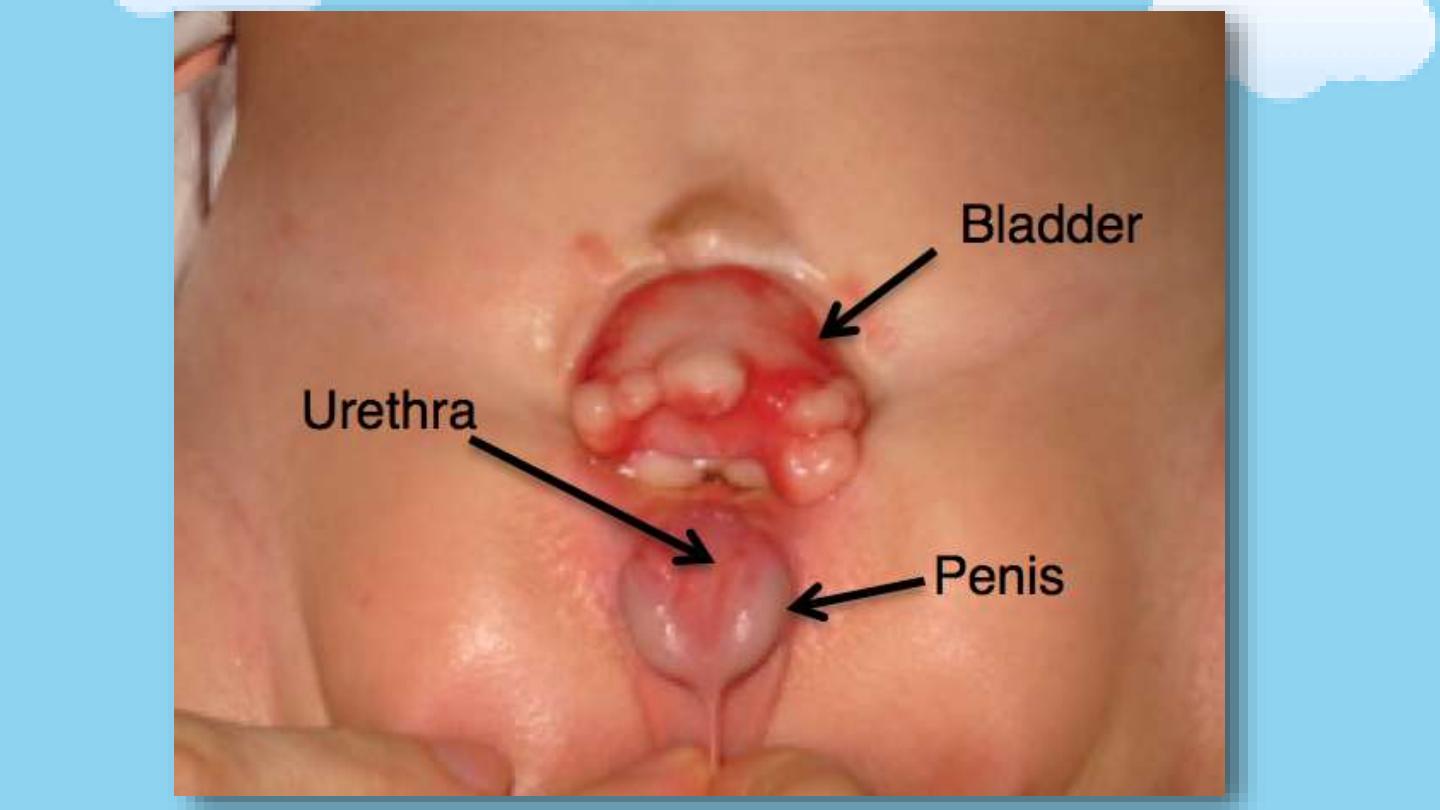

Exstrophy in a male patient

Exstrophy in a female patient

External rotation of the iliac bones
Bladder injury

Bladder injury
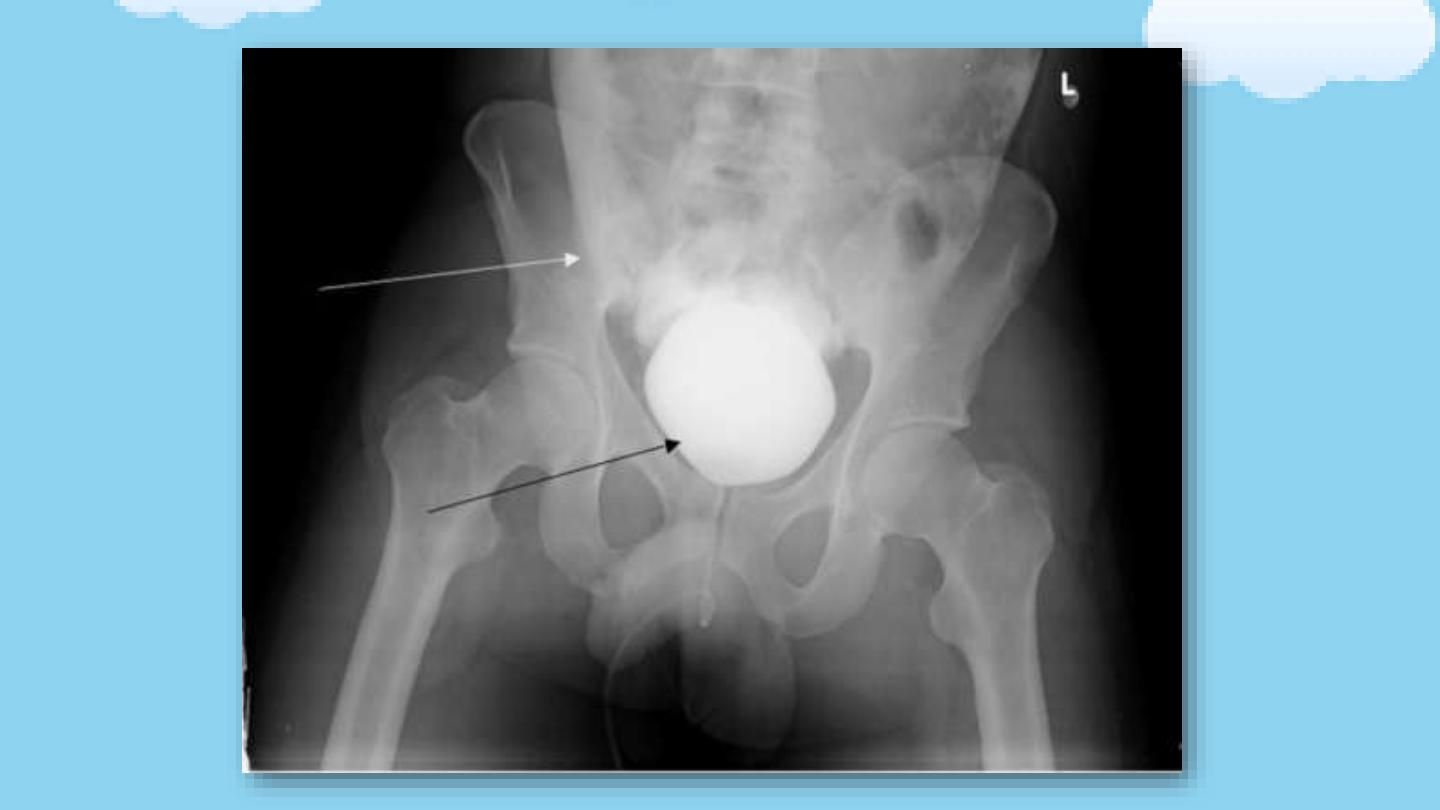
Bladder injury is often associated with blunt trauma and
particularly with
pelvic fracture
. Some series report up to
90%
of bladder ruptures occurring with associated pelvic fracture.
Severe
associated injuries
are often seen when both
pelvic fracture and bladder rupture are present, and mortality
may occur in 12–22% of cases

Causes
1. Blunt:
• Motor vehicle accident: 70-97% have associated pelvic
fracture
• 10-15% of all pelvic fractures have bladder injury with or
without urethral injury.
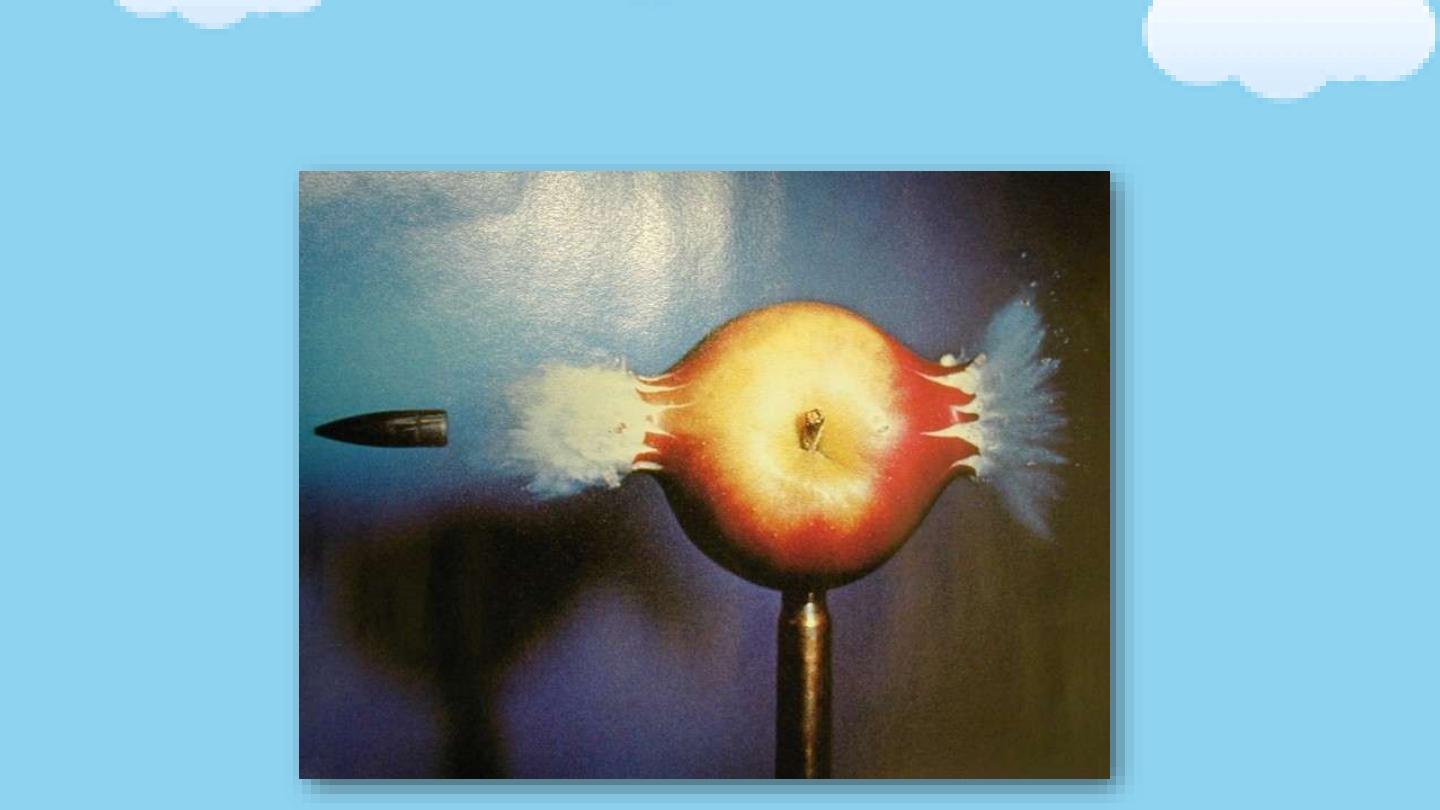
2. Penetrating injury:
bullet, knife, foreign body.
3. Iatrogenic during surgery:
obstetric, gynecologic, general
surgical and urologic interventions.
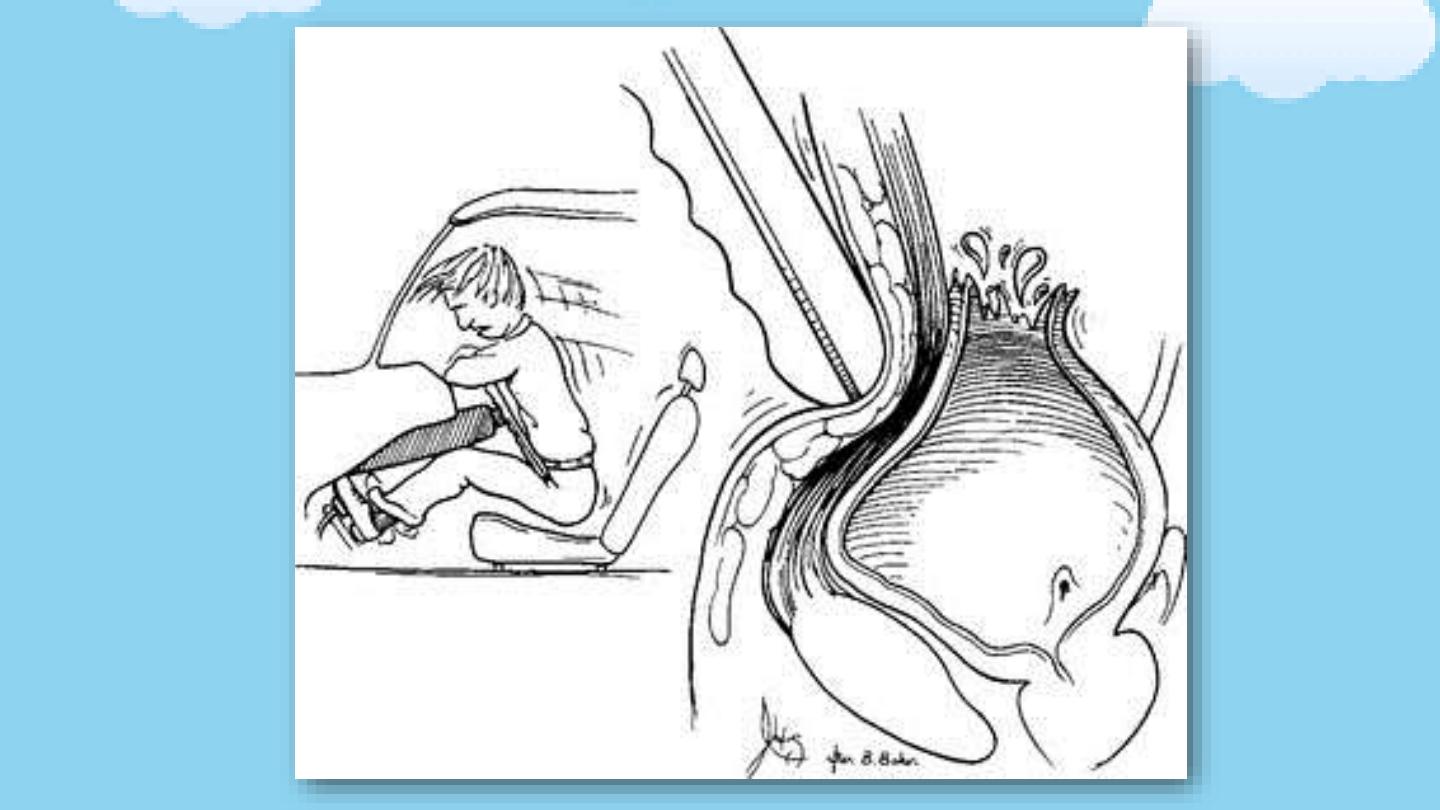

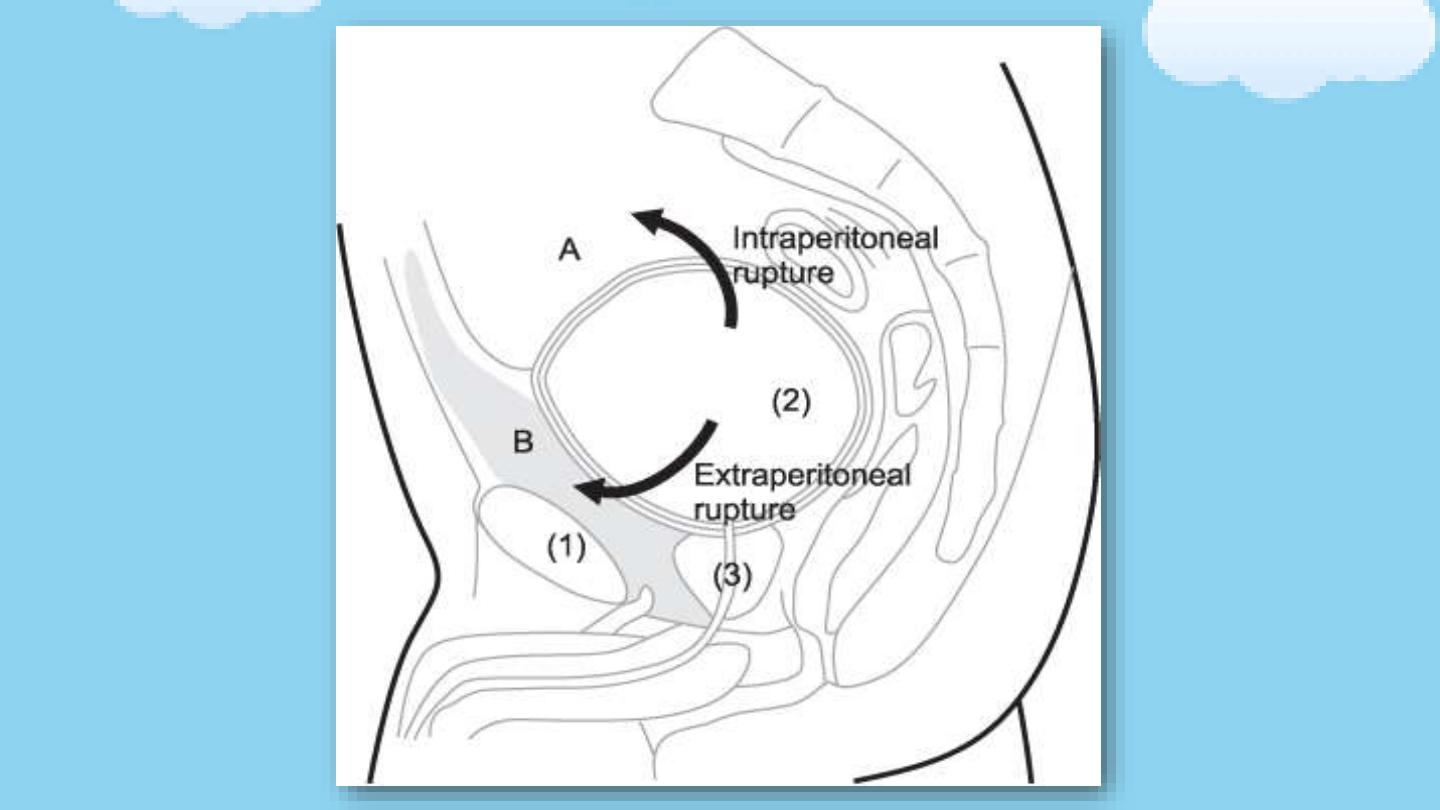
Types of bladder injury
• 1. Contusion:
Trauma with hematuria with no evidence of bladder
leak ( no extravasation of urine)
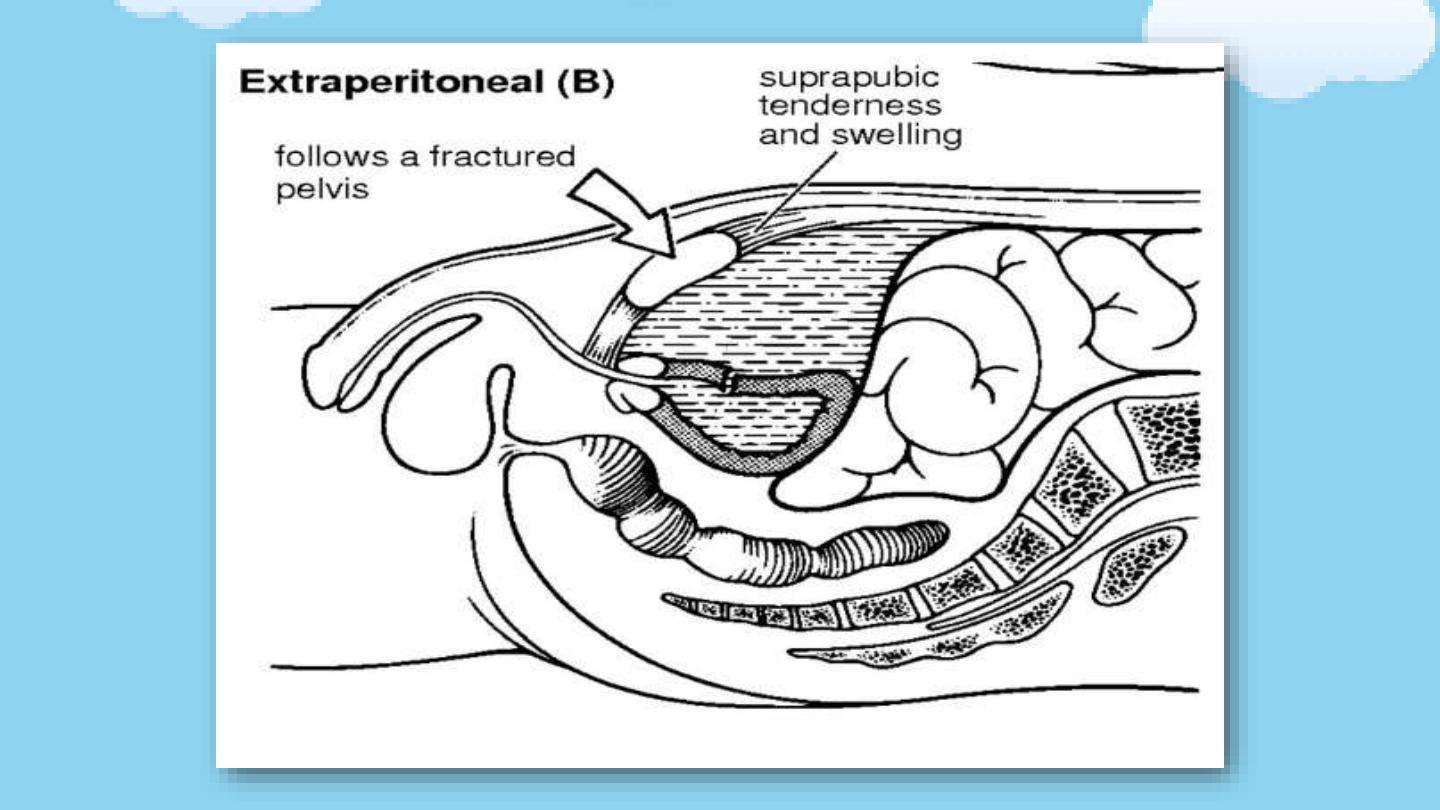
• 2. Extraperitoneal rupture
(65%): the peritoneum is intact and urine
escapes into the space around the bladder, but not into the
peritoneal cavity.
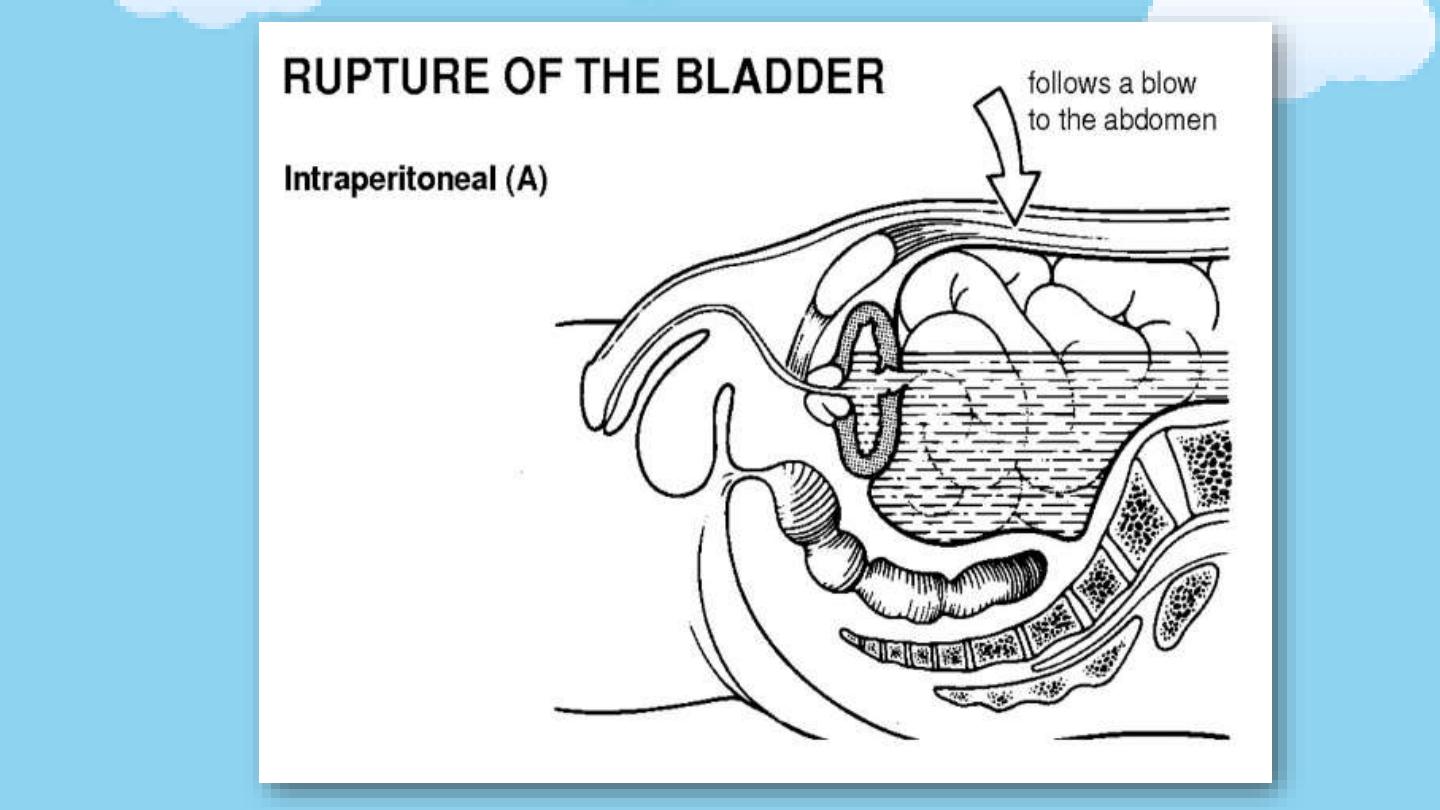
• 3. Intraperitoneal rupture
(25%): the peritoneum overlying the
bladder is breached allowing urine to escape into the peritoneal
cavity.
• 4. Combined:
intra and extraperitoneal (10%)

Clinical features
The classic triad of symptoms and signs suggesting a bladder
rupture are:
1. Gross hematuria.
2. Suprapubic pain and tenderness with sometimes bruising.
3. Difficulty or inability in passing urine.

Additional signs are as follows:
1. Abdominal distension
2. Absent bowel sounds (indicating an ileus from urine in the peritoneal
cavity)
3. Fever in peritonitis
4. Urine ascites
5. Increased BUN/Cr
6. Free fluid on abdominal CT or ultrasound
7. Enlarged scrotum

Diagnosis
1. Retrograde cystography
a Foleys catheter is inserted and 350ml of diluted contrast in
an adult and
{(age + 2) x 30}
mL in children is injected to the
bladder then x-ray image is taken.
In extraperitoneal perforations, extravasation of contrast is
limited to the immediate area surrounding the bladder (a
dense “
flame-shaped” collection
of contrast).
In intraperitoneal perforations, loops of bowel or the lower
lateral portion of the peritoneal cavity may be outlined by the
contrast.
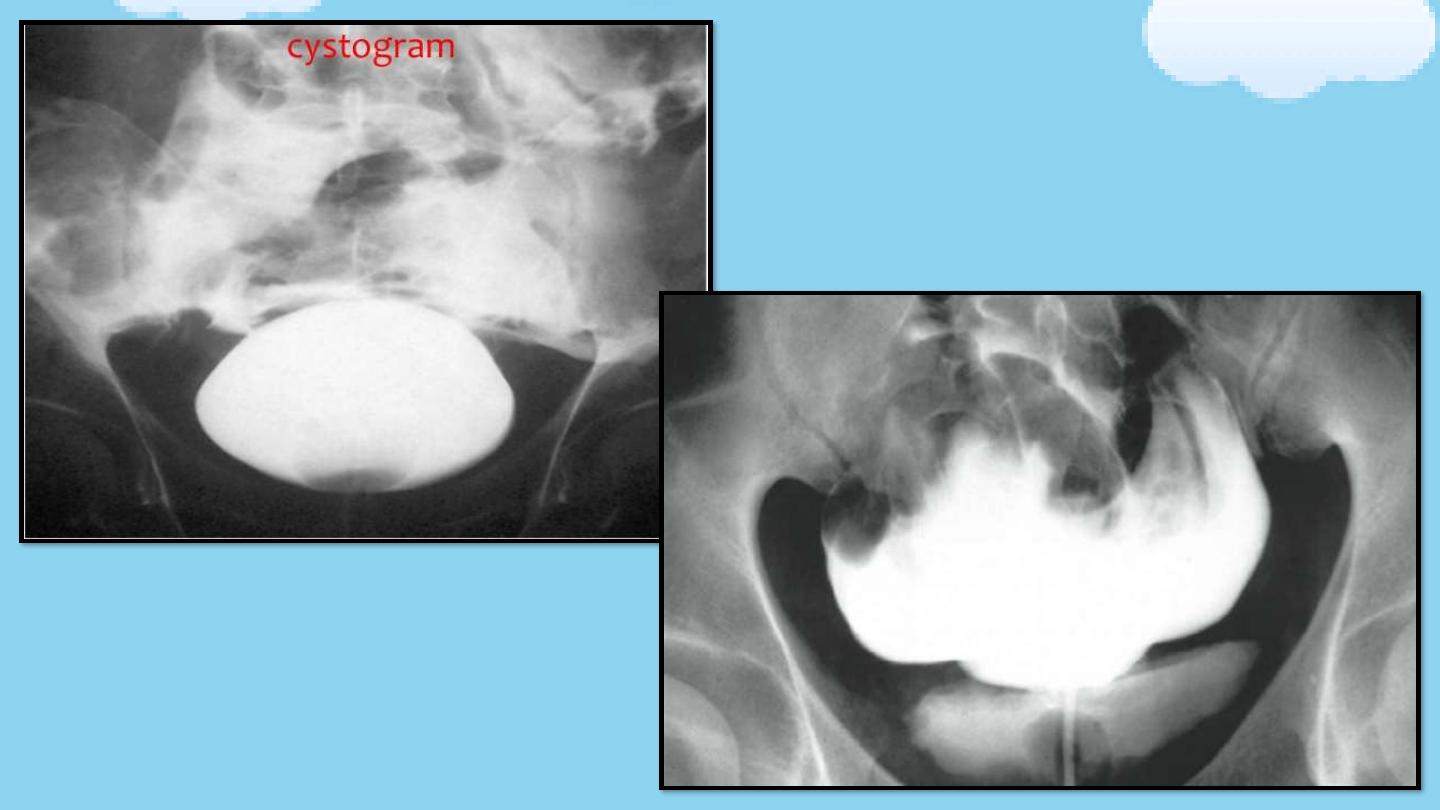
Extraperitoneal bladder rupture
Intraperitoneal bladder rupture

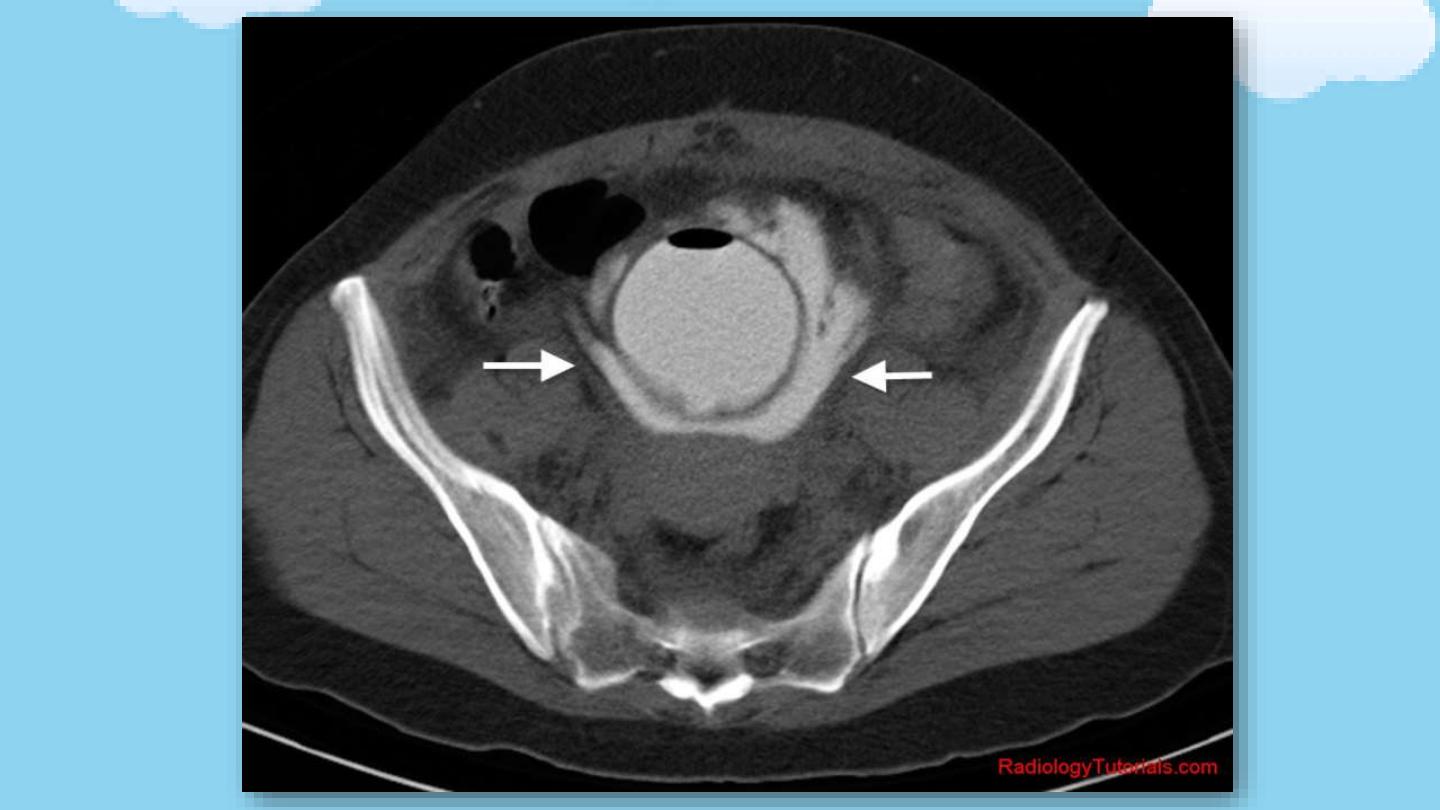
2. CT cystography:
a “
full-bladder
” phase is required. CT cystography is
usually more appropriate, since many trauma patients
are already undergoing CT for other abdominal, chest,
head, or pelvic injuries.
3. Methods to diagnose bladder rupture intraoperatively:
a. Direct inspection of the bladder
b. b. Fill the bladder with colored dye (e.g. indigo carmine
or methylene blue)
c. Cystoscopy
d. Intentional cystotomy for direct internal inspection of the
bladder.

Management
1. Bladder contusion
• Adequate drainage of the bladder should result in
resolution within a few days.
• Follow-up cystography is recommended to assess integrity
of the bladder wall.

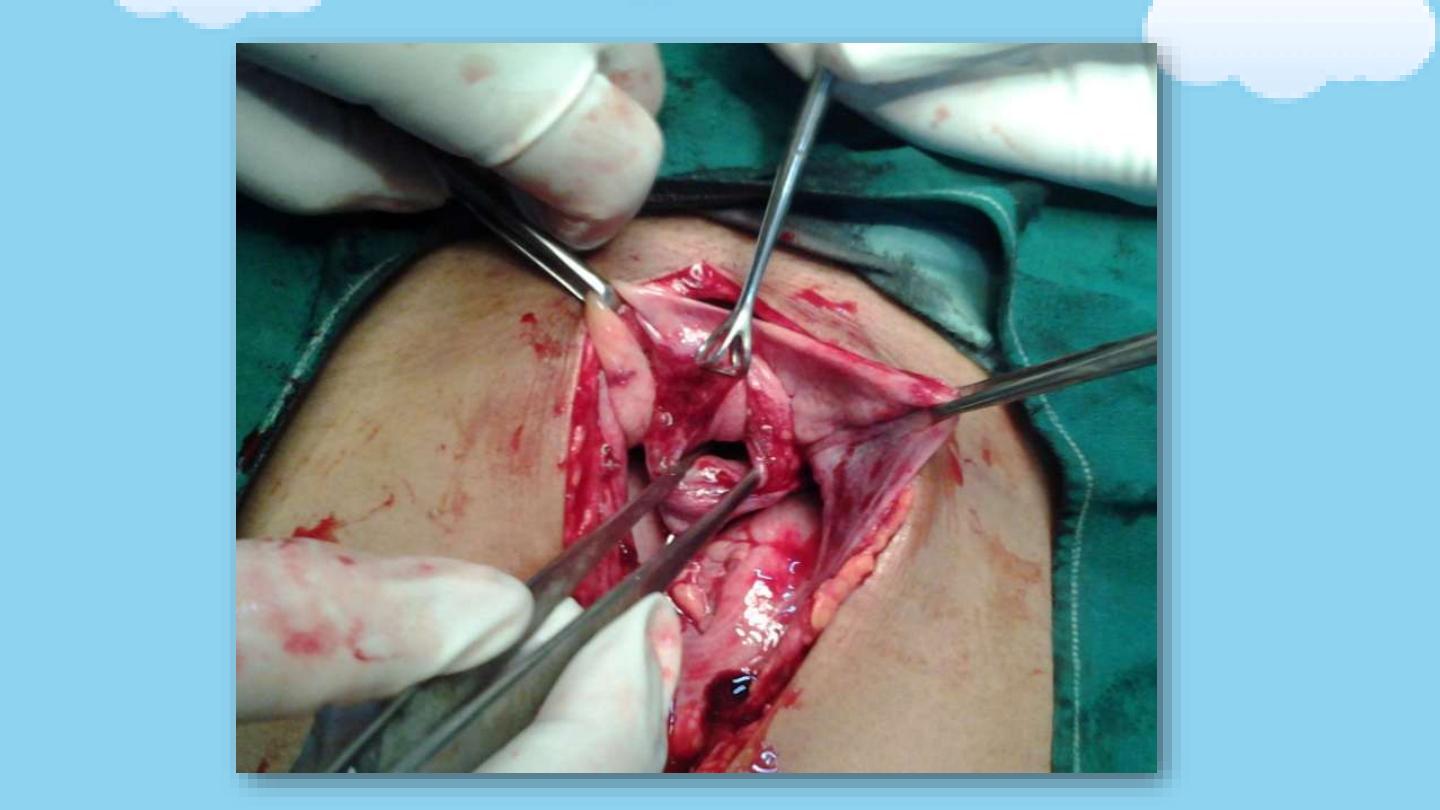
2. Intraperitoneal rupture
• usually requires exploratory
laparotomy
, cystotomy
and
suturing of the bladder wall defect
, urethral
catheter placement, and water-tight bladder closure
in
2 or 3 layers
with absorbable suture.
• suprapubic tube
may be considered for a complex
bladder repair, significant ongoing gross hematuria, or
patients that will require long term catheterization.
• Antibiotics

3. Extraperitoneal rupture
• A. Extraperitoneal When conditions are ideal, use bladder drainage with
a
urethral catheter
for about 2 weeks followed by a cystogram to confirm
the perforation has healed.
• If extravasation is noted, replace the catheter for 2 more weeks and
repeat imaging; some injuries may take up to 6 weeks to heal.
• If no urinary extravasation exists, the catheter can be removed.
• Antibiotics on day of injury until 3d after Foley removed

• B. Open surgical repair (as described for intraperitoneal
bladder rupture) is recommended for any of the following
scenarios.
a) If the bladder was opened to place a suprapubic catheter
for a
urethral injury
or
Bone spike
protruding into the
bladder on CT.
b) Injuries to the bladder discovered intraoperatively during
nonurological surgery
c) Injuries occurring as a result
of penetrating trauma
d) Poor urinary drainage
due to clot obstruction.
e) Associated
rectal or vaginal perforation
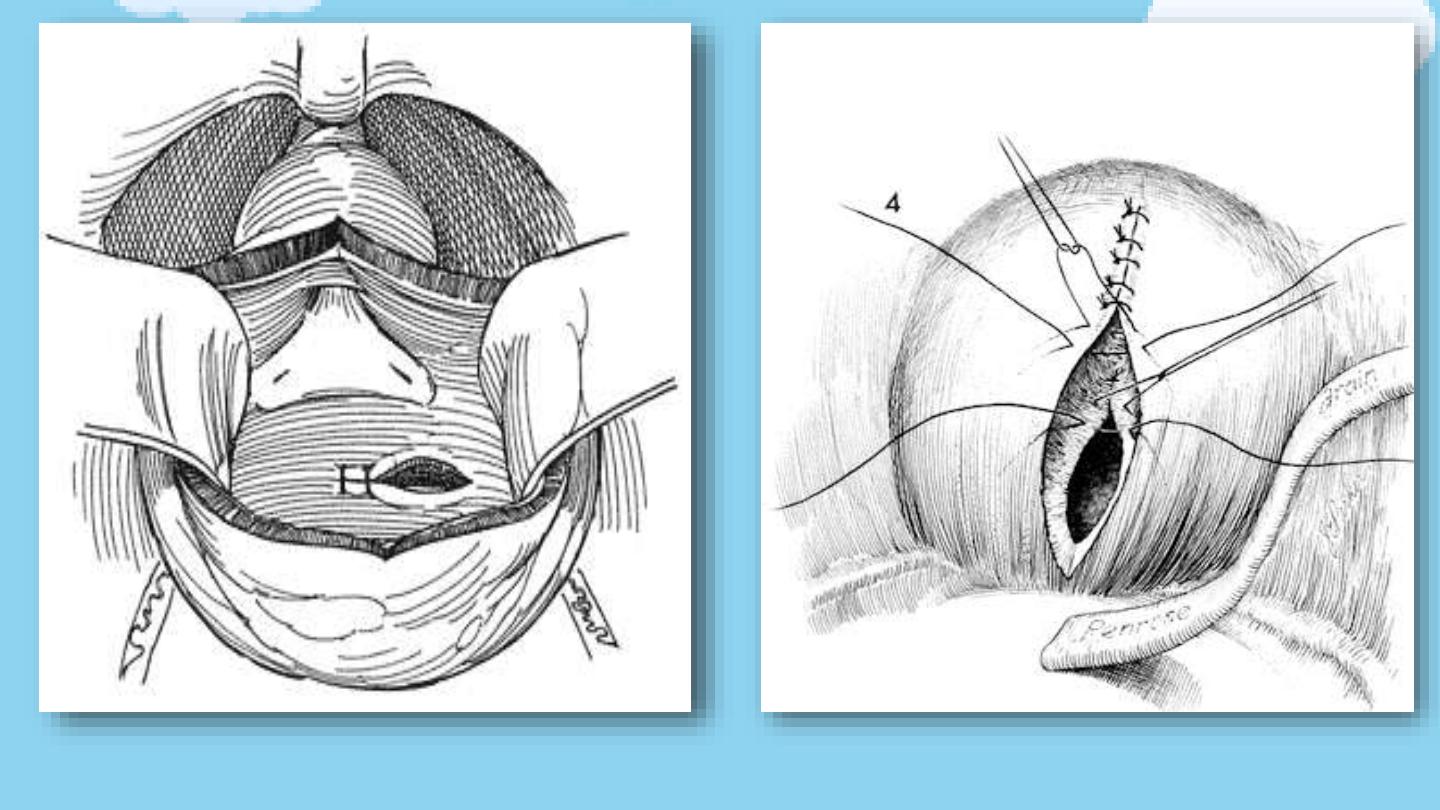
The rupture is being sutured
The cystotomy is being sutured

complications
• Complications of bladder injury are primarily due to a delay
in diagnosis leading to
azotemia, ascites, and sepsis
.
• Vesical fistula
when other organ injuries are present
(Vesicovaginal fistula, ureterovesical fistula, rectovesical
fistulae).
• Bladder neck injury
, if not identified and repaired, may result
in incontinence.
• Persistent extravasation
suggests catheter obstruction, bony
fragments, or ischemic complications of injury.

