
1
OBSTETRICS
Lec: 10
Transverse lie-‐ oblique lie
Dr. Haider Al-‐Shamma'a
Objectives
•
Able to define transverse and oblique lie
•
The student should be able to diagnose transverse , oblique lie
•
Should be able to list the causes.
•
Able to outline the management and justify it
•
Able to define unstable lie
•
Able to list the causes
•
Able to outline the management and can justify it
•
Able to identify fetal causes of abnormal labor
•
Able to outline the management with justification
•
The student should be able to diagnose cord prolapse
•
Able to appreciate the risks of cord prolapse
•
Able to manage the patient with cord prolapse
-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐
•
Transverse
lie:
-‐
occurs
when
the
longitudinal
axis
of
the
fetus
is
perpendicular
to
the
longitudinal
axis
of
the
mother
the

2
presenting
part
is
the
shoulder
(
also
named
shoulder
presentation
).
•
Oblique
lie
:-‐
when
the
head
or
the
breech
is
slightly
higher
than
the
other
side
3
4
•
the denominator is the back ( dorsum )
•
Dorso-‐anterior is more common than dorso-‐posterior
•
Incidence :-‐ 1/250 – 1/500 deliveries
Causes of transverse lie
1. Multiparity is the most common cause
2. Prematurity
3. Polyhydramnious
4. Multiple pregnancy
5. Contracted pelvis
6. Placenta previa
7. Fibroids of the lower segment
8. Congenital abnormalities of the uterus as septate and arcuate
uterus
5
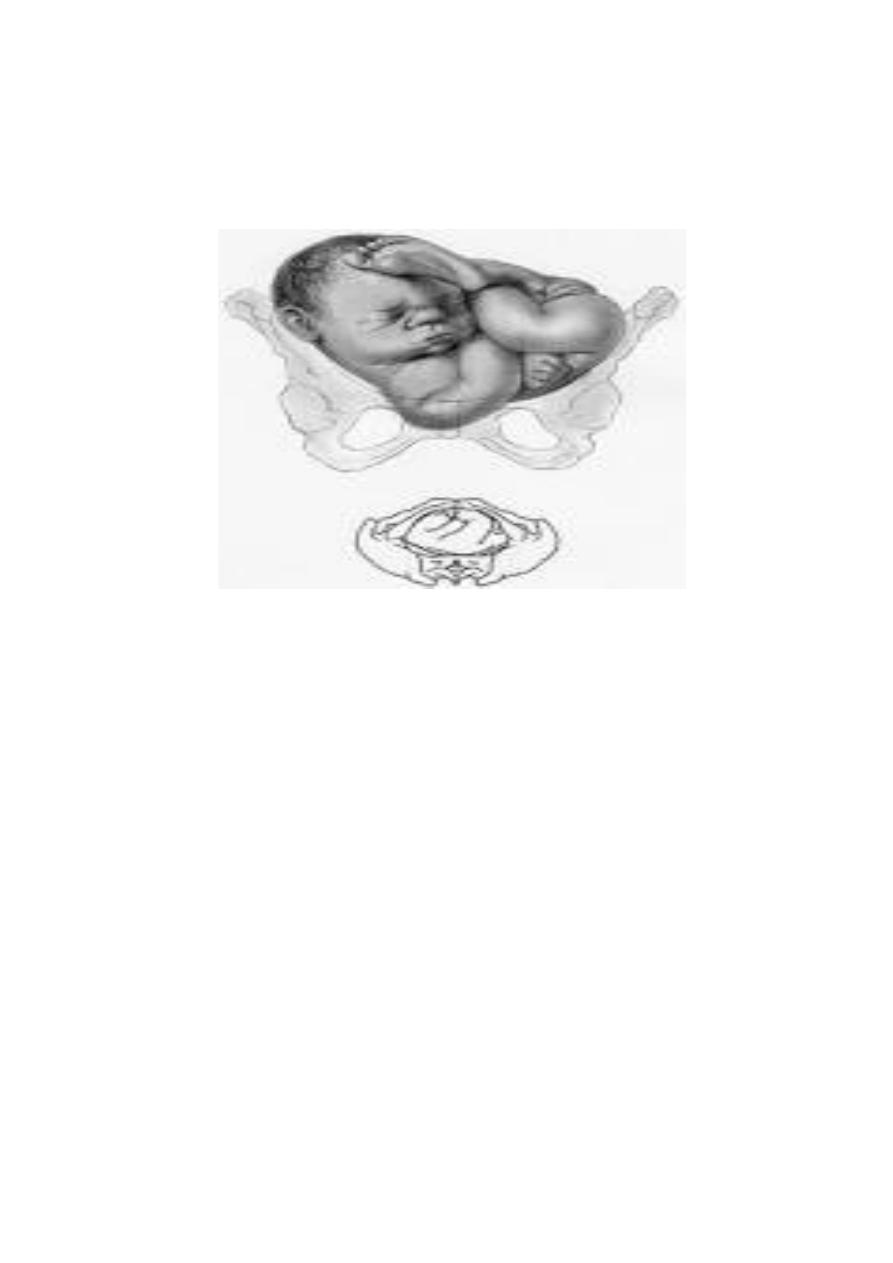
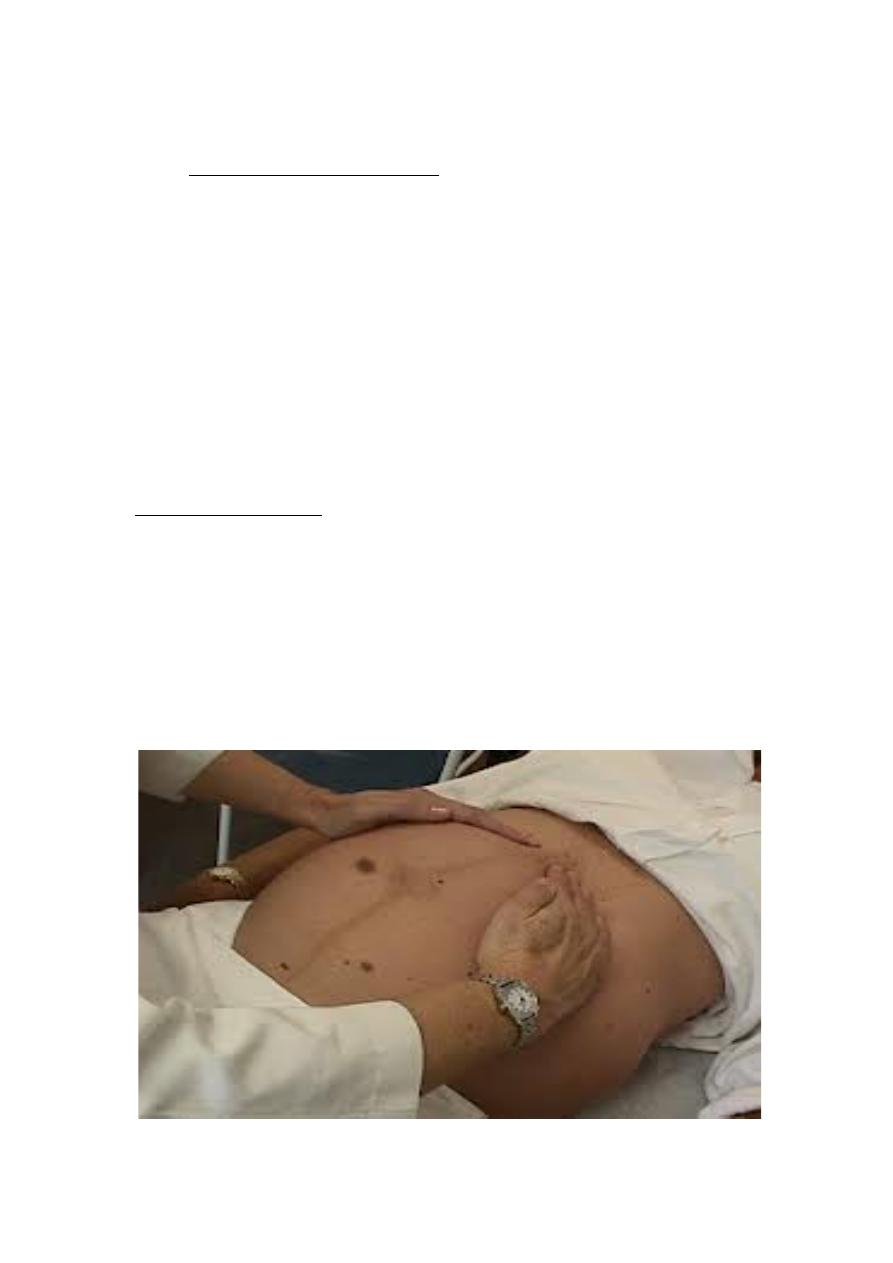
Diagnosis of transverse lie
•
On abdominal examination:-‐
1) The abdomen is asymmetrically distended
2) Width more than length
3) Fundal height less than expected
4) Round heard mass at one iliac fossa , softer breech at the other
fossa
5) Absent presenting part ( pelvic grip feel empty lower segment
On p/v examination:-‐
1) Cannot feel the presenting part (high)
2) Bulging membranes or rupture membranes
3) Fetal arm or umbilical cord may prolaps to the vagina
Abdominal Finding T. Lie
6
Hand prolapse
Mechanism of labor
•
No
mechanism
of
labor
due
to
very
large
dimensions
of
the
fetus
,
in
a
neglected
case
lead
to
fetal
death
and
rupture
of
the
uterus
and
maternal
death
•
Rarely
in
a
small
premature
dead
macerated
fetus
in
a
stout
mother
,
the
baby
may
fold
on
itself
and
deliver
vaginally
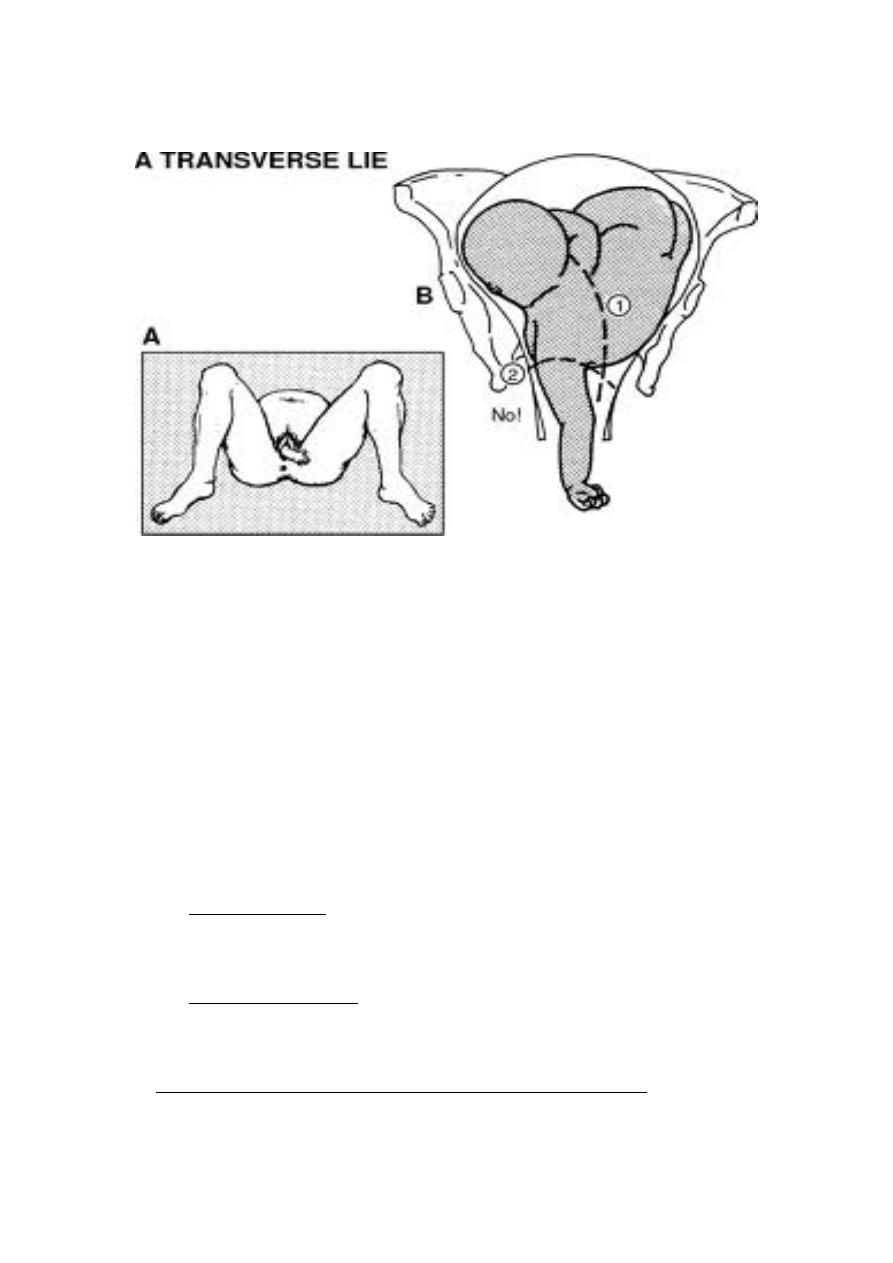
Management of transverse lie
1. Before labour :-‐
Manage as breech do ECV *
2. During early labor:-‐
Before rupture membrane can try ECV
3. Advanced labor , failure of ECV or contraindicated ECV :-‐

7
Cesarean
section
is
the
safest
method
even
incase
of
a
dead
fetus
(TLSCS
or
easier
LVCS)
•
Rarely in advanced neglected case with no facilities of CS
Decapitation
by
hook
or
saw
,
then
pull
the
hand
to
deliver
the
trunk
then
deliver
the
head
by
forceps
Cesarean section is safer
Unstable lie
•
When the fetus changes its axis every visit
•
Causes as t lie
•
Management :-‐ECV each visit after 36 weeks
•
((same contraindication as ECV of breech)
•
Admission to hospital at 36 weeks
•
ECV and induction of labor at 38 wks
•
Elective cs may be performed in selected cases
Fetal malformation causes difficult labor
•
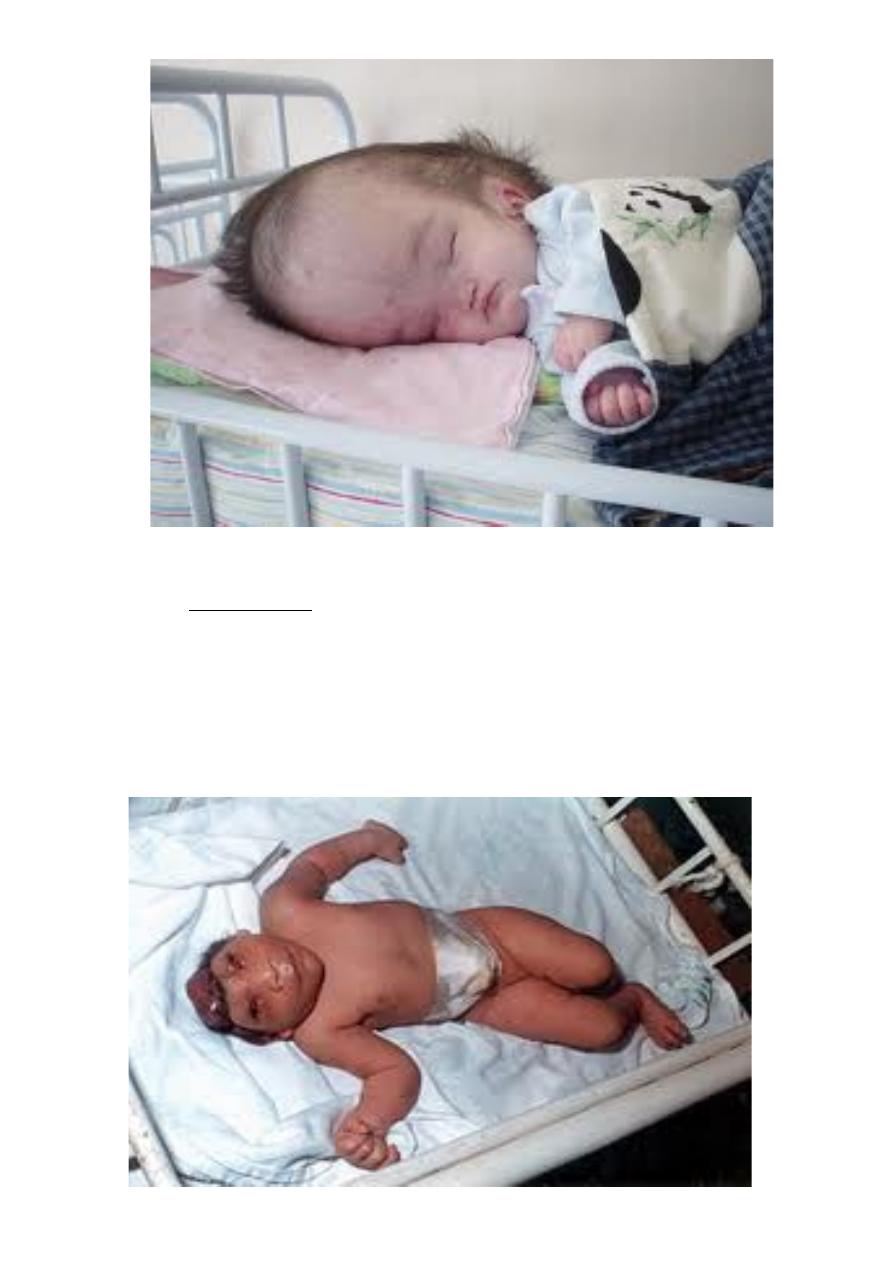
Hydrocehalus
•
Diagnosed by U/S
•
During labor feel widely separated sutures
•
Big head cause obstructed labor rare in modern practice
•
Management
:
terminate
pregnancy
when
the
head
reaching
9.5
cm
by
induction
of
labor
or
by
CS
(up
to
12cm)
•
Advanced
obstructed
labor
perforate
the
head
and
drain
the
CSF
and
deliver
vaginally
(
rare
)
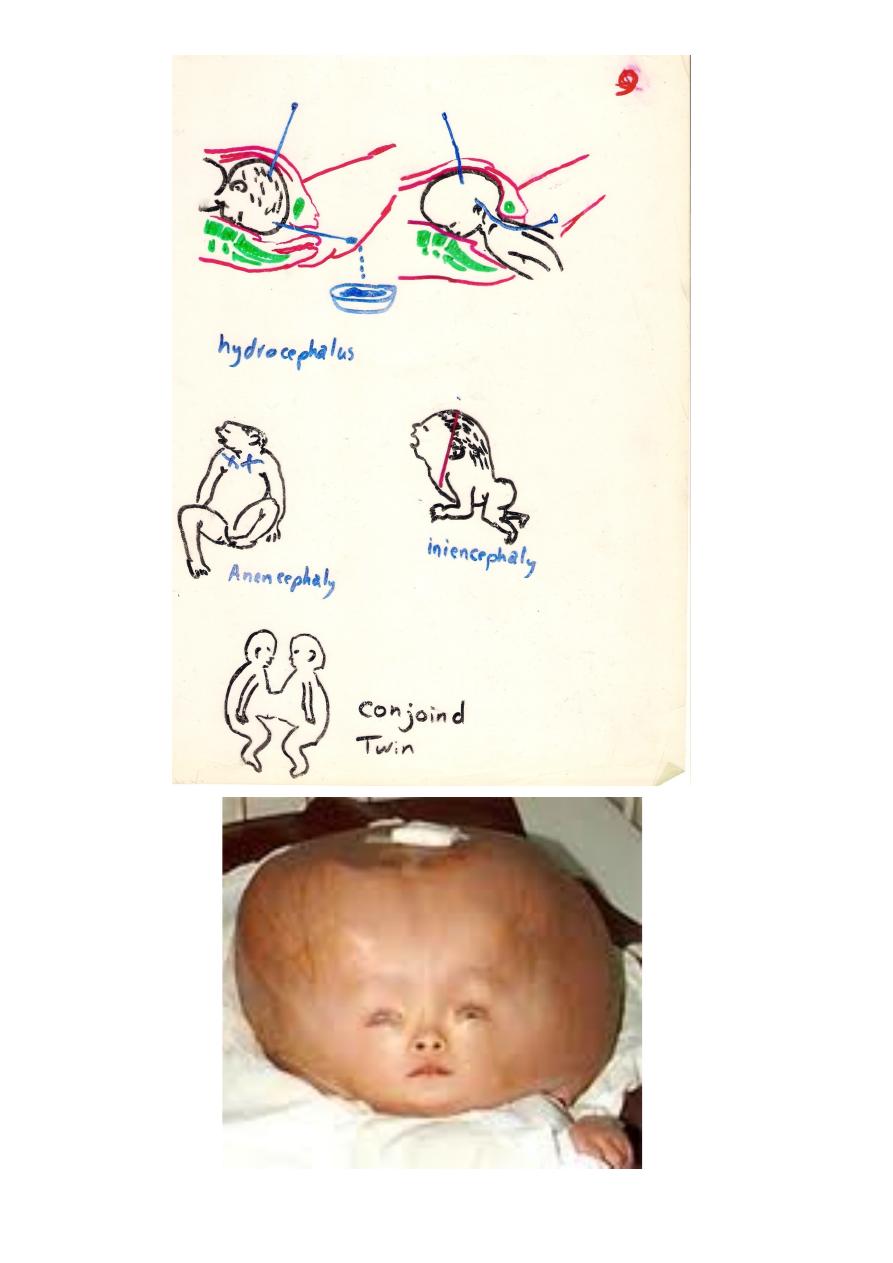
8
9
•
Anencephalus
•
Absent vault and brain , incompatible with life
•
May cause prolonged pregnancy(>42 wks)
•
due
to
irregular
shape
dilatation
is
difficult
,
may
need
cleidotomy
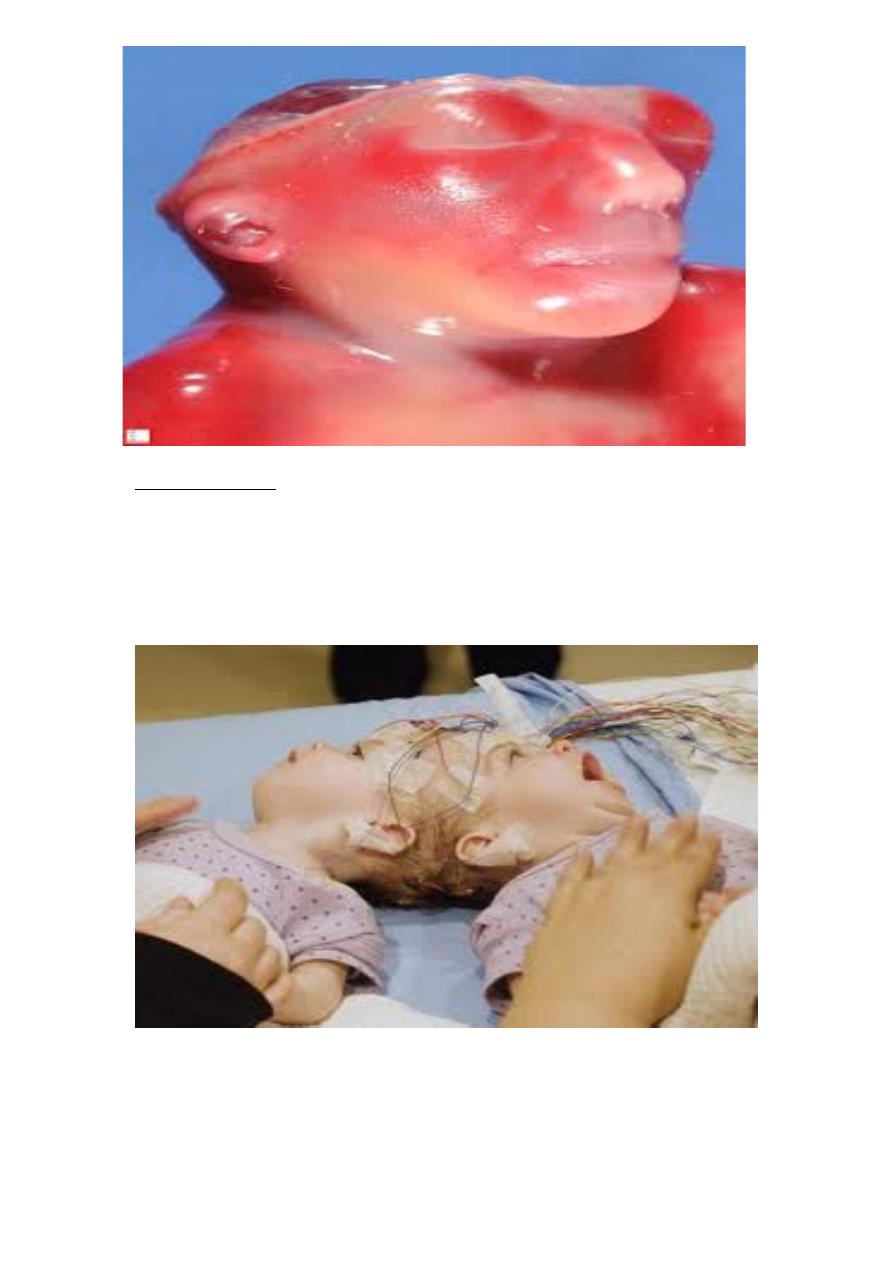
10
Conjoined twins
•
Suspected if the twins maintain the same relation to each other
•
U/S can diagnose the connection
•
Cause obstructed labor and need CS even that may be difficult!!
11
Thoracopagus
•
Compound presentation
•
Head +hand
•
Head + foot
•
Give large and irregular presenting part with risk of cord prolaps
•
Management:-‐
•
Usually corrected spontaneously with progress of head descent
•
If persistent try to push limb up
•
CS may be needed
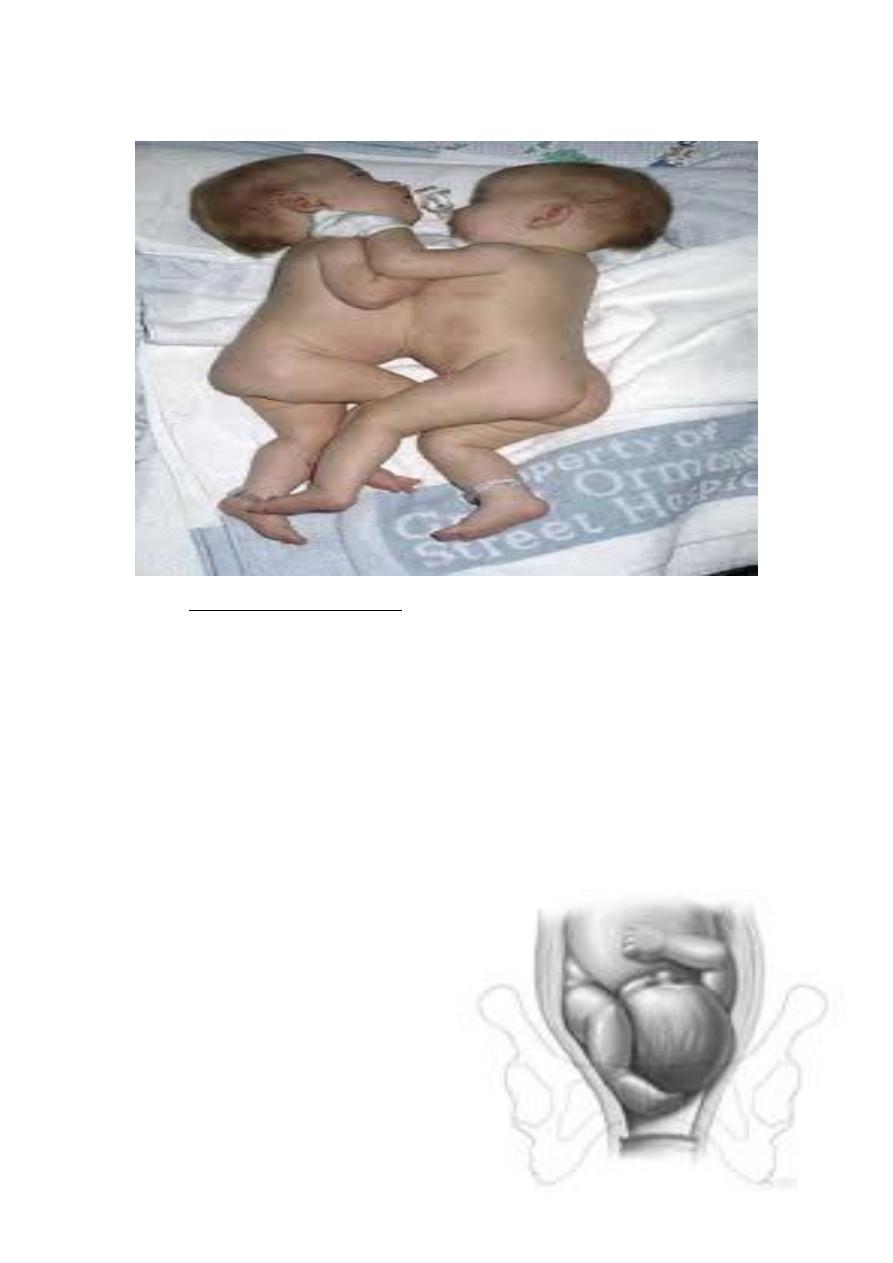
Cord prolapse
•
Descent
of
loop
of
cord
through
the
cervix
to
the
vagina
or
even
outside
the
12
vagina when the membranes ruptures
•
Causes
1) Malposition mal presentation
2) Rupture of the membranes when the head is high
•
Diagnosis of cord prolaps
•
Feel soft cord felt below the fetus
•
Pulsation can be felt and this mean the fetus is alive
•
If No pulsation either dead or spasm
Consequences of cord prolapse
•
Thermal
and
tactile
stimulation
cause
spasm
that
interfere
with
fetal
oxygenation
fetal
hypoxia
and
death
may
occur
in
less
than
30
min
•
Also
cord
compression
between
the
presenting
part
and
boney
pelvis
Treatment of cord prolapse
•
Steep
Trendlingburg
position
or
knee
chest
position
to
dis-‐impact
the
fetus
and
reduce
cord
compression
•
Vaginal pack
•
Terminate
pregnancy
by
the
most
rapid
method
before
fetal
death
(1
st
stage C/S) & ( 2
nd
stage : forceps , vacuum extractor or C/S which
ever can deliver first)
13
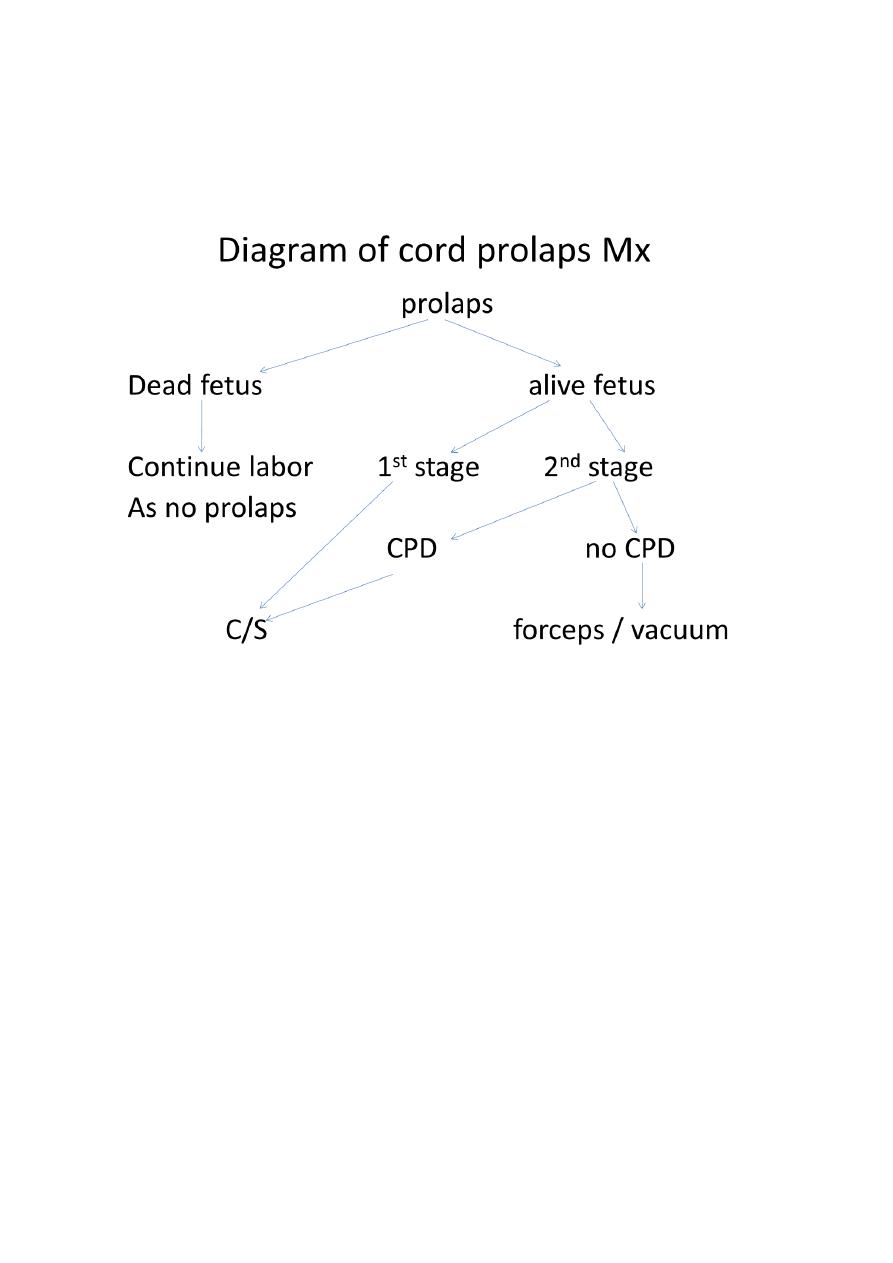
Diagram of cord prolaps Mx
