
UNIVERSITY RESEARCH CO., LLC
NATIONAL IMMUNIZATION
PLAN OF IRAQ for 2015
DECEMBER 2014

1 |
P a g e
Table of Contents
I.
Preface…………………………………………………….……………………………………..2
II.
Acknowledgement ................................................................................................................. 2
III.
Acronyms ........................................................................................................................... 5
IV.
Introduction and Background .......................................................................................... 6
1.
Current situation ........................................................................................................................... 6
2.
Stakeholders functions in supporting Immunization in Iraq .................................................... 8
3.
Situational Analysis of Routine EPI by System based on Previous Years' Data (2008-2010) 9
4.
Immunization Schedules 2014 - 2015 ........................................................................................... 9
5.
Key Achievements in 2014 in collaboration with USAID, WHO and UNICEF ...................... 9
6.
Immunization Coverage (2011- 2014) ........................................................................................ 11
7.
Strengths, Issues of Concern and Challenges............................................................................ 15
V.
National Immunization Plan for 2015 ............................................................................... 16
1.
Vision of the National EPI Program .......................................................................................... 16
2.
Guiding Principles of the National EPI Program ..................................................................... 16
3.
Goals of the EPI program in Iraq .............................................................................................. 17
4.
Objectives and Planned Activities for 2015 ............................................................................... 17
VI.
Monitoring and Evaluation ............................................................................................. 20
1.
Strategic approaches to ensure an effective immunization program ...................................... 20
2.
Key Performance Indicators ....................................................................................................... 21
3.
Financing of immunization activities ......................................................................................... 22
VII.
Strategies towards program sustainability ...................................................................... 22
VIII.
References ........................................................................................................................ 25
2 |
P a g e
I.
Preface
Immunization is one of the most successful, safe and cost-effective public health interventions
for preventing deaths and disabilities from vaccine preventable diseases. Small pox has been
eradicated and the world is on the verge of eradicating polio. Significant reductions have been
achieved in reducing illness, disability and death from diphtheria, tetanus, whooping cough and
measles. In 2003 alone, it is estimated that immunization averted more than 2 million deaths.
Yet it is an unfinished agenda. Immunization program needs to be sustained year after year since
new children are born an every year, new vaccines are being introduced and a high level of
population immunity has to be maintained to prevent reintroduction of any illness or outbreaks.
Immunization will help to achieve the Millennium Development Goals (MDGs) on reducing child
mortality, improving maternal health and combating diseases.
Immunization has a promising future. We are entering a new era in which it is expected that the
number of available vaccines will double. Immunization services are increasingly used to deliver
other important health interventions, making them a strong pillar of health systems.
There are still millions of people who do not benefit from the protection that vaccination provides.
They are at risk of life-threatening illness every day. In Iraq there are still thousands of children
who do not complete all their doses and hence not fully protected. Hence there is always the risk
of outbreaks and reintroduction of diseases.
This document presents Iraq’s National Immunization Plan for 2015. It has been prepared by the
Ministry of Health with technical support from partners including the United States Agency for
International Development’s (USAID’s) Primary Health Care Project in Iraq (PHCPI).
PHCPI has assisted the Iraqi Ministry of Health (MOH) to achieve its strategic goal of quality
primary health care (PHC) services in the country. PHCPI supports the MOH in three key
components: 1) strengthening health management systems, 2) improving the quality of clinical
services, and 3) encouraging community involvement to increase the demand for and use of PHC
services. In October 2013, a modification to PHCPI’s technical scope of work had the project re-
focus its efforts to further help the MOH accelerate the achievement of MDGs 4 and 5, reduce
child mortality and improve maternal health.
For PHCPI, awareness and improvement of vaccination coverage has been a key element in
addressing MDG 4 and PHCPI specifically addresses this goal with activities providing training
to health care providers, traditional birth attendants, and community partners on the importance
of proper nutrition and vaccinations in the healthy development of infants and young children.
Additionally, PHCPI has trained a core of immunization Master Trainers as well as vaccinators
and supervisors for Iraq’s Expanded Program on Immunization (EPI).
Further support for Iraq’s immunization efforts has included the development of a tablet program
used by field vaccinators to track child immunizations and the creation of an acute flaccid
paralysis (AFP) field manual for the detection of poliomyelitis.
II.
Acknowledgement

3 |
P a g e
The University Research Co., LLC wishes to thank all the people who have collaborated on the
design, implementation, and analysis and reporting of this study. They have given generously of
their time and their experience. Significant contributions to the development of this plan were
made by USAID/Primary Health Care Project in Iraq (PHCPI) team in the field, Dr. Hala Jassim
AlMossawi, Chief of Party, Dr. Ahlam Kadhum and HQ team, Dr. Neeraj Kak, and Taylor Price
and to Dr. Omer Mekki from the World Health Organization and Dr. Ali Al-Taei from UNICEF
who provided significant technical assistance in the review of the plan. Special thanks are due to
Ministry of Health Public Health Directorate headed by Dr. Ziad Tariq and the technical working
group who contributed time and experience to develop this study.
Ministry of Health Technical Working Group:
1. Dr. Nabeel Abrahim Abass - Director of the Immunization Section
2. Dr. Thaear Saleem Salman - Immunization Section
3. Dr. Yousra Khalaf - Immunization Section
4. Dr. Sundus Jamal Putrus - Immunization section
4 |
P a g e

5 |
P a g e
III.
Acronyms
BCG Bacillus
Calmette-Guerin
DOH Directorate
of
Health
DQA Data
Quality
Assessment
PHC
Primary Health Care Centers
DPT Diphtheria,
Tetanus,
Pertussis
EPI
Expanded Program on Immunization
HipB
Haemophillus influenza type B
HEXA
HEXAVALENT Vaccine: (Diphtheria, Tetanus, Pertussis +Hepatitis B +
Haemophillus influenza type B) + injectable Polio Vaccine.
IDP
Internally Displaced Persons
KIMADIA General Company for Drug Marketing and Medical Appliances
MDGs Millennium
Development
Goals
MICS4
Multiple Indicators Cluster Survey Round 4-2011
MMR
Measles, Mumps, Rubella
NID National
Immunization
Days
OPV Oral
Polio
Vaccine
Penta
Diphtheria, Tetanus, Pertussis +Hepatitis B + Haemophillus influenza type B
DTP
+
IPV
RED Reach
Every
District
SIA Supplementary
Immunization
Activities
SNIDs
Sub National Immunization Days
Tetra
Tetravalent Vaccine: DPT (Diphtheria, Tetanus, and Pertussis) + Haemophillus
influenza type B
VPDs
Vaccine Preventable Diseases
PAB Protection of infant at Birth

6 |
P a g e
IV.
Introduction and Background
Preventing disease through immunization benefits all people, resulting in positive health,
economic and social yield at global, national and community levels. Immunization is a cost
effective and life-saving intervention, preventing needless diseases, disabilities and deaths.
Immunization and other linked interventions will provide an important contribution to achieving
the Millennium Development Goals (MDGs) either directly by contributing to the reduction of
childhood deaths or indirectly in reducing the incidence of other infectious diseases, and
ultimately , by improving the health of the population and thus contributing to poverty reduction.
In 1985, the Expanded Program of Immunization (EPI) was well established in Iraq delivering
immunization services to targeted groups, implementing national and global strategies to achieve
main objectives. Until two decades ago health status indicators were improving, especially in
controlling EPI targeted diseases reflecting high standards of EPI achievements.
From 1980 to 2003, Iraq faced the tragedy of three wars with economic sanctions during which
there was neglect of all aspects of life including the health sector that witnessed progressive
deterioration of the quality and accessibility of health services resulting in health indicators
December lining to the levels of the least developed countries. EPI was one of the major victims
of this December line.
This National Immunization Plan gives a brief analysis of the current situation and the goals,
objectives and activities planned for 2015.
1. Current situation
For eleven years following the war, health system staff has tried their best to overcome and
minimize the consequences and negative effects through reviving many of the primary health care
facilities. Through EPI, the MOH is now trying to achieve its goals of reducing Iraq’s maternal
and child mortality rates by two thirds. Yet, now more than before, the Iraqi EPI is confronted
with many challenges and obstacles hindering progress. These include:
Security complications;
Military operations;
Power supply shortages (electricity & fuel);
Political difficulties affecting the major political and strategic decisions and short- or long-
term plans of the Ministry of Health;
Inadequate communication and coordination between the MOH and other directorates. This
is affecting performance; and
Financial barriers.
In 2014, in addition to a polio outbreak, wild measles virus was imported to Iraq via Syrian
refugees. The abrupt down trend in June 2014 is most probably due to seasonality and to
disruption of surveillance following the chaos created by the sudden takeover of the government
in these provinces.
The current conflict has severely and adversely affected the health care delivery system in Salah
Al-Din, Anbar, Ninewa and Diyala Governorates, significantly affecting availability and access
to both preventive and curative health services.
7 |
P a g e
The Anbar conflict on January 9, 2014 and the Mosul crisis on June 9, 2014 not only damaged
the physical infrastructure of health facilities (hospitals, public health clinics, etc.), but displaced
health workers (doctors, nurses, displaced health workers, nurses, paramedics, etc.) and caused
myriad other issues.
The influx of over 1,500,000 internally displaced persons (IDPs) in the Kurdistan Region
Government has further overwhelmed the fragile health system in the three Governorates (Erbil,
Duhuk and Sulymania). The region was already burdened with over 200,000 Syrian refugees and
facing tremendous financial challenges due to political disputes with the Central Government.
Prior to the current crisis, Anbar, Ninewa, Diyala, Salah Al-Din and Kirkuk already had some of
the lowest health and nutrition indicators in the country.
In the MICS4-UNICEF (2012), over a third of children are reported as stunted (33%) in Anbar.
With the recent outbreak of the wild-polio virus in Deir Ez-Zor in Syria (bordering Anbar), the
likelihood of virus importation to Anbar, Ninewa, Diyala, Salah Al-Din and Kirkuk is very high
due to population movement. The ongoing conflict has adversely affected the immunization
campaigns jointly implemented by MOH/WHO/UNICEF decreasing coverage levels.
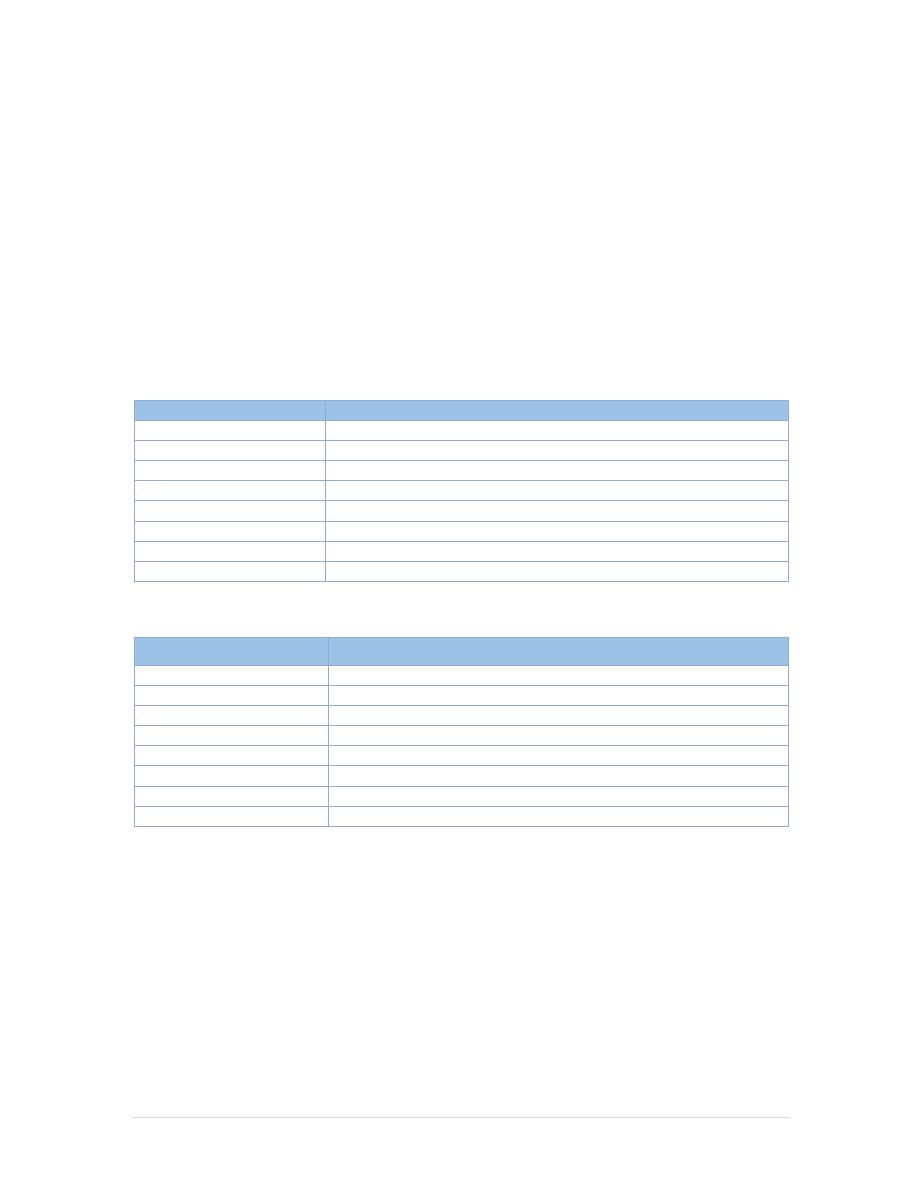
Tables 1 through 4 provide information about basic population and EPI data, national coverage
rates as well as districts coverage.
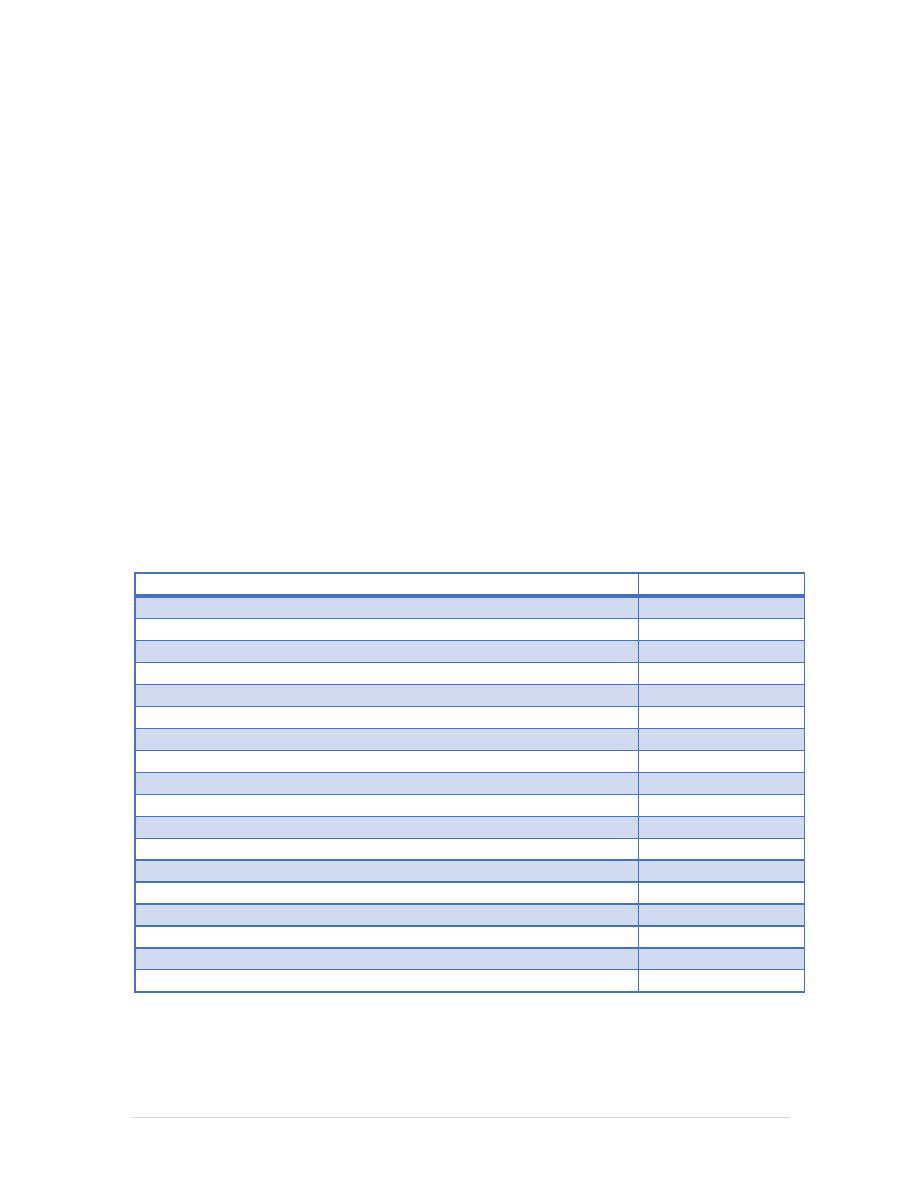
Table 1: Basic Population and EPI Data
Items Numbers
Births
1,318,392,(2014)
Area of Iraq covers
435,052 sq. Km.
Total population
36000000
Surviving infants
1,166253 (2014)
Infant mortality rate (per 1,000 live births)
32.7 (2011, MICS)
Under-five mortality rate (per 1,000 live births)
37.9 (2011, MICS)
Gross national income per capita (PPP, US$)
6,710
Percentage of routine EPI vaccines financed by government
100
Home-based vaccination records (percent)
70 (2011, MICS)
Male constitute
0.502
Under 5 year of age
5,871,642
Adolescents (age 10-19 years)
about 23%
Children in general
about 54.3%
Women of child
bearing 22 %
Directorates of Health (DOH)
19
Districts
132
PHCCs
2,638
Number of PHCCs offering routine immunization
1,532
8 |
P a g e
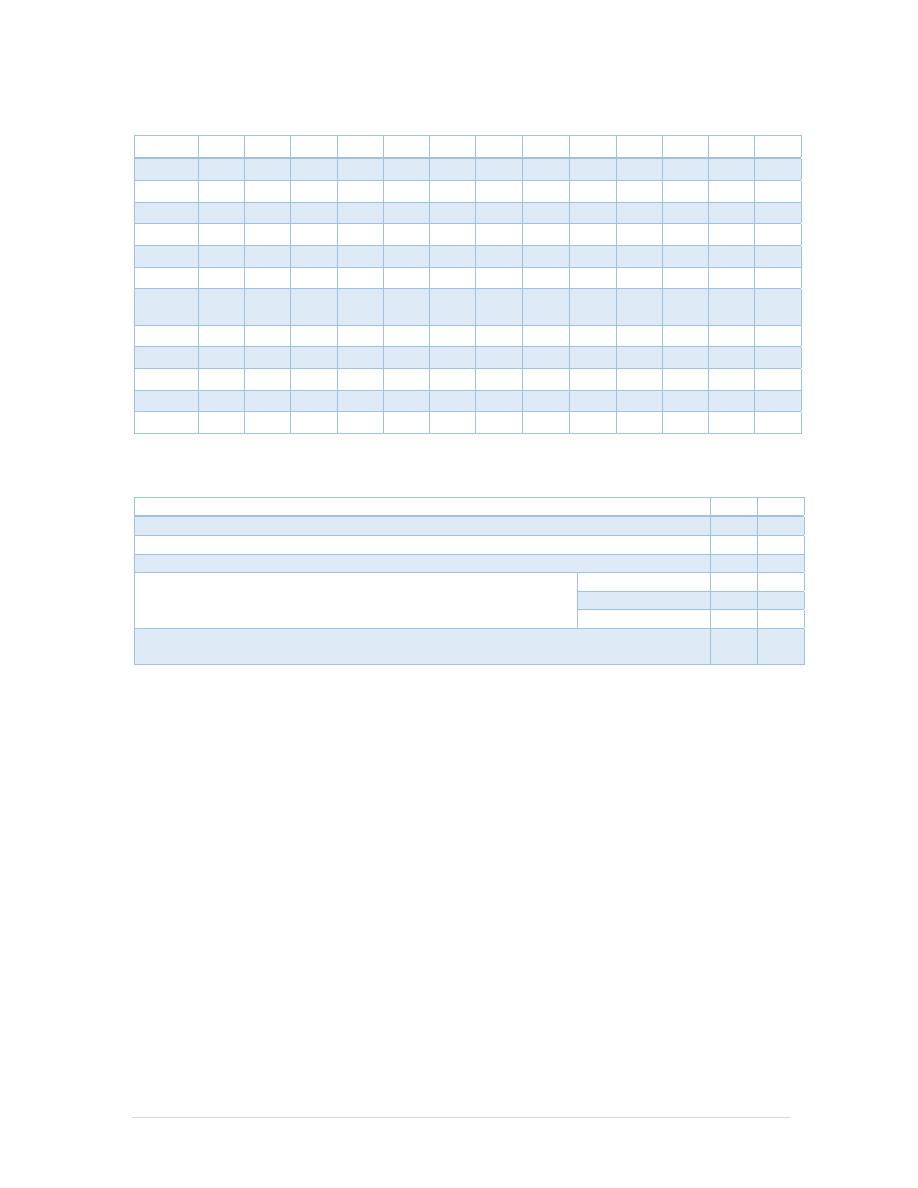
Table 2: National coverage rates (%) (WHO/UNICEF estimates, 2013)
2013 2012 2011 2010
2009
2008
2007
2006
2005
2000 1995 1990
1980
BCG
90
90
90
90
92
87
92
89
92
93
97
96
76
DTP1 82 87 90 86 88 81 68 76 84 92 86 93 36
DTP3
68
69
79
74
78
69
59
59
65
80
74
83
36
HepB3 43 37 32 27 60 92 90 88 93 0 … … 14
HepB3
66
61
77
72
75
66
56
59
65
67
57
0
…
Hib3
68
36 0 0 0 0 0 0 0 0 0 0 …
rota
(last)
52
31
0
0
0
0
0
0
…
…
…
…
…
PcV3 0 0 0 0 0 0 …
…
…
…
…
…
…
Pol3
70
70
80
74
78
71
74
63
69
83
73
83
16
MCV1 63 69 77 75 81 76 64 62 69 86 80 75 9
MCV2
57
68
77
77
87
76
64
52
58
0
…
…
…
PAB 72 85 85 80 69 69 69 70 71 75 81 70 4
Table 3: District coverage (as reported)
2012
2013
Number of districts in country
130
133
Percentage of districts reporting
100
99
DPT3: proportion of districts with coverage (%)
3
2
MCV1: proportion of districts with coverage at 95% or above
(%)
Below 50%
47
47
Between 50-79%
51
50
At 80% or above
11
18
DTP1-DTP3 drop-out rate: proportion of districts that have achieved a rate of less
than 10% (%)
23
48
2. Stakeholders functions in supporting Immunization in Iraq
There are three main stakeholders in the immunization program: the government, non-
governmental organizations (NGOs) and international partners, and the community. The
Government of Iraq (GOI) provides overall leadership and stewardship to the program through
policy and program development as well as infrastructure for program delivery, both physical and
human resources. Main actors are comprised of UNICEF, WHO, UNFPA, World Bank and
USAID. National NGOs and professional associations assist in advocacy and social mobilization
activities specifically during large-scale vaccination campaigns and other special vaccination
activities. The community, or beneficiary, facilitates the immunization program by providing
necessary support through local structures, such as local health committees, to the health
providers in terms of space and community mobilization.
9 |
P a g e
3. Situational Analysis of Routine EPI by System based on Previous Years'
Data (2008-2010)
A tabular analysis of various components of routine EPI is presented in Annex 1 which indicates
that an effective functioning system of routine EPI services is in place in Iraq in spite of wars,
conflicts and other issues that may have adversely affected program performance. This system
will be further strengthened and serve as the foundation for activities during 2015 as presented in
Section 3.
4. Immunization Schedules 2014 - 2015
In 2015, Iraq’s National Immunization Schedule will be updated. Table 5, below, gives the current
schedule and Table 6 gives the schedule effective 2015. The TT schedule for pregnant women
and women of child bearing age will remain the same.
Table 5: Vaccination Schedule for Infants and Children 2012
Age
Type of vaccine
0-1 Week
OPV0 dose , HepB1 , BCG
2 Months
OPV1 , PENTA1,ROTA1
4 Months
OPV2 , TETRA1,ROTA2
6 Months
OPV3 , PENTA2,ROTA3
9 Months
Measles + VIT A
15 Months
MMR (Measles , Mumps , Rubella)
18 Months
TETRA2, OPV First Booster dose + VIT A
4-6 Years
DPT , OPV Second Booster dose + MMR2
Table 6: National Immunization Schedule for Infants and Children 2015
Age
Type of vaccine
0-1 Week
HepB1 , BCG + OPV0dose
2 Months
HEXA 1,ROTA1 ,PREV13-1+OPV1
4 Months
HEXA2,ROTA2,PREV13-2 + OPV2
6 Months
HEXA3,ROTA3,PREV13-3 + OPV3
9 Months
Measles + VIT A
15 Months
MMR(Measles , Mumps , Rubella)
18 Months
PENTA (DTP+IPV+Hib ) OPV + VIT A
4-6 Years
TETRA (DTaP +IVP ) + OPV + MMR
5. Key Achievements in 2014 in collaboration with USAID, WHO and
UNICEF
5 Polio NIDs and 7 SNIDs were conducted with more than 90% coverage by administrative
report. The following NIDS were conducted
- Spring - first round in March 2014
- Spring second round) in April 2014
- Spring third round) in May 2014
- Autumn - first round in September 2014
- Autumn - second round in October 2014

10 |
P a g e
Polio and measles campaigns for IDPs;
Influenza campaigns for high-risk people;
Completed RED Approach strategy;
Developed four guidelines for health workers (National guideline on EPI, National guideline
on SIAs, National guideline on AEFI and National guideline on vaccine and cold chain
management);
Achieved OPV3 coverage of 77%.
Achieved measles coverage of 72%.
Conducted five central training courses on cold chain management;
Conducted one central training course for workers on immunization guidelines;
Conducted three training courses for workers in PHC districts and PHC Centers on
immunization management.
Conducted three meetings for EPI managers at the DOH.
Conducted five training courses for AFP Surveillance officers on Acute Flaccid Paralysis
(AFP) surveillance.
Conducted five peripheral training courses to improve performance of health workers in
immunization units in DOH.
Conducted five advocacy meetings for workers in Surveillance units for activation of
surveillance of AFP;
Conducted a campaign for seasonal Influenza for high risk populations and areas in November
2014.
Conducted a polio and measles vaccination campaign for IDP′s in August 2014;
Conducted a comprehensive sub- national measles campaign December 2014;
Conducted two master training of trainers (TOT) in immunization management and
surveillance for 47 Master Trainers in Amman and Erbil in November – December 2014;
Training of vaccinators and supervisors on immunization by PHCPI/USAID (1661
vaccinators and 425 supervisors till end December 2014).
11 |
P a g e
6. Immunization Coverage (2011- 2014)
Immunization coverage - a key measure of immunization performance.
The following are methods, materials and tools used to measure or estimate immunization
coverage, and on immunization coverage at the country level based on data reported by provinces.
Methods:
The administrative method – collected from reported routine immunization data, i.e.
registry system of doses administered;
The following is a link to immunization coverage (up to 2013) by the WHO and UNICEF for all
countries, including Iraq.
http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tscoveragebcg.html
Access to Immunization
Population access to routine immunization is estimated based on the proportion of children under
the age of one year that have received the first dose of pentavalent vaccine. An acceptable level
of access would be over 90%. The lower coverage rates in the subsequent routine doses attributed
to irregular and shortage of vaccines supplies.
The routine immunization coverage monitored by the achieved coverage of the following vaccine
doses, OPV3, Penta2, Rota (last dose) and Measles.
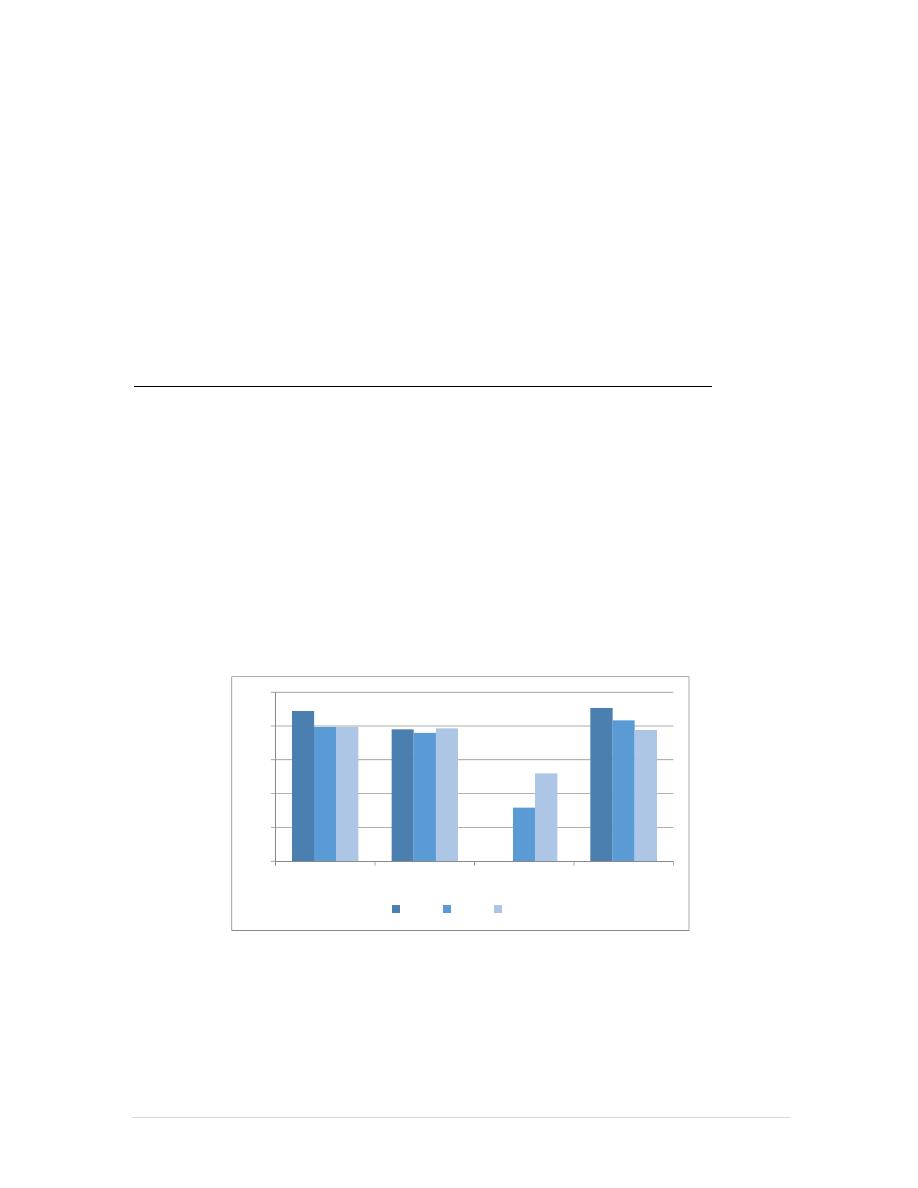
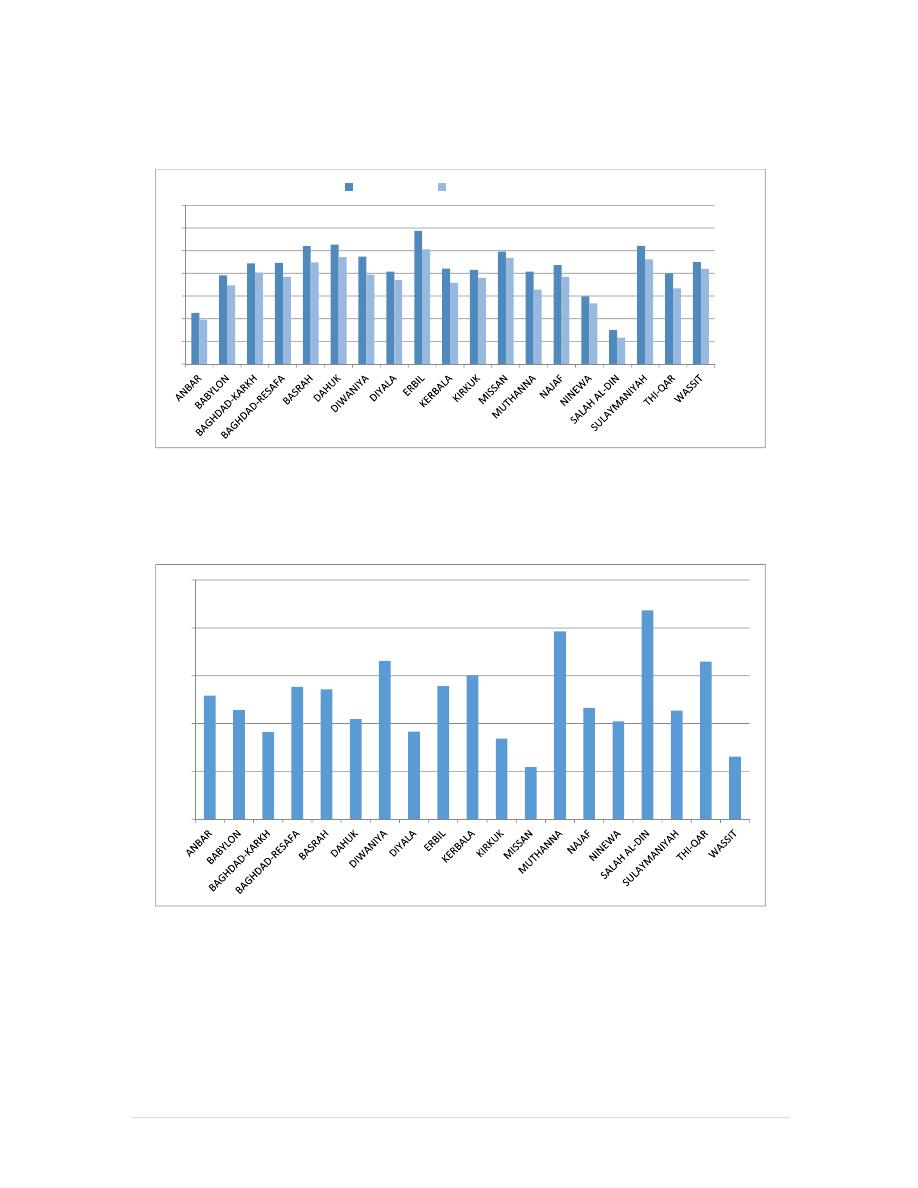
Figure 1 shows progressive decline in the achieve coverage of the most EPI antigens since 2011
Figure 1: Immunization Coverage OPV3, Penta2, Rota3 and measles 2011-2013
The 2013 national coverage levels for each vaccine, presented in Figure 2, indicate that, except
for BCG, coverage of all vaccines is significantly below the national goal of 95% with
measles/MMR and TT coverage levels below 80%. Increasing routine immunization coverage to
95% at national and provincial levels and 90% at district level is of top priority in 2015.
89
78
0
91
79
76
32
83
79
79
52
78
0
20
40
60
80
100
OPV3 cov
Penta2
Rota3
Measles
2011
2012
2013
12 |
P a g e
Figure 2: National Coverage of all vaccines – 2014
Immunization Drop-out Rate
The capacity of the health system to complete the immunization course for a child or woman is
estimated based on the drop-out rate indicator between the first dose and the third dose of the
pentavalent vaccine. This indicator shows the percentage of children under the age of one year
that initiate immunization but do not complete three doses within the first year of life. The
maximum acceptable drop-out rate is 10%; higher rates indicate inefficiency of the health service,
service discontinuity at fixed posts, lack of information to mothers about returning for the follow-
up doses, and a lack of subsequent visits by outreach or mobile teams.
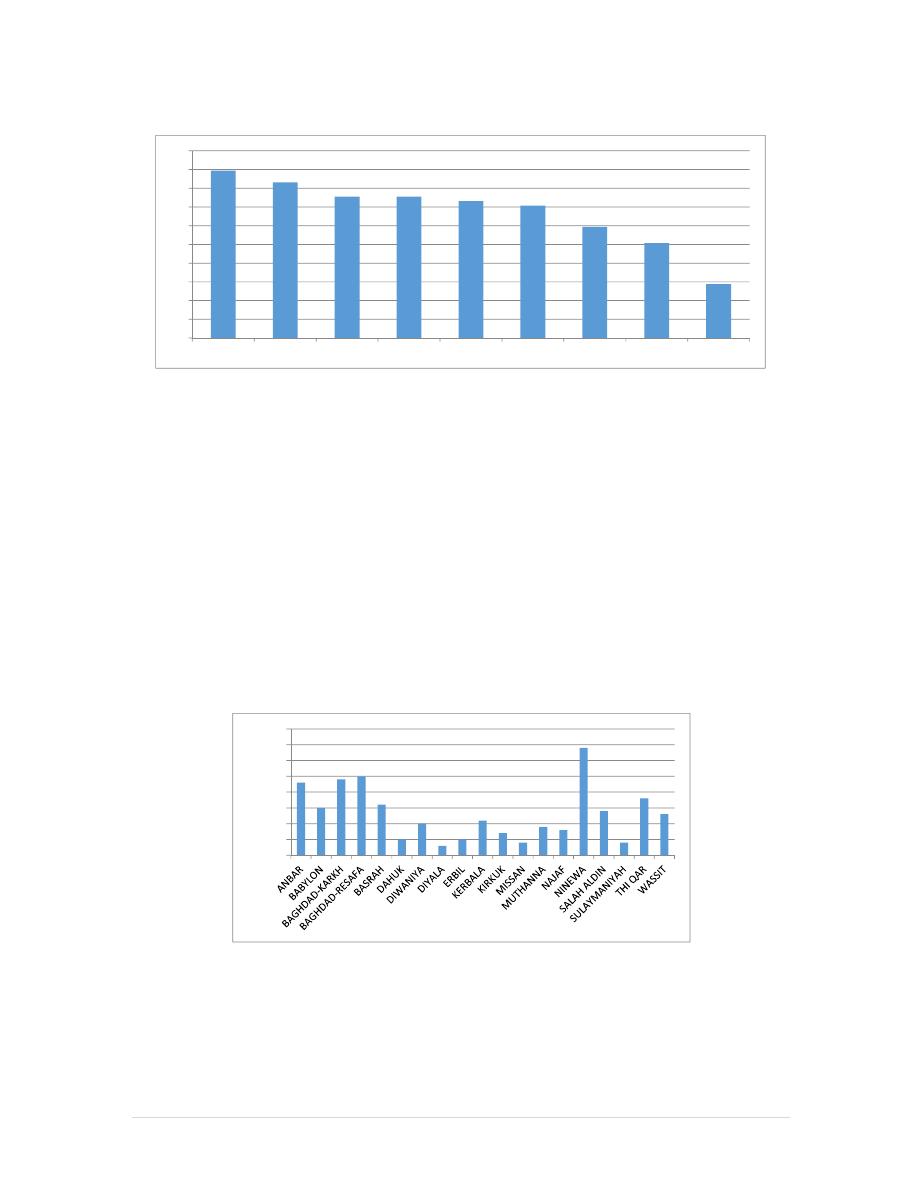
As shown in Figure 3 below, a large number of children did not receive the required three doses
of OPV in 2013. Many Governorates including Ninewa, Baghdad, Thi-Qar, Babylon and Wassit
have a large number of under immunized children indicating low levels of population immunity.
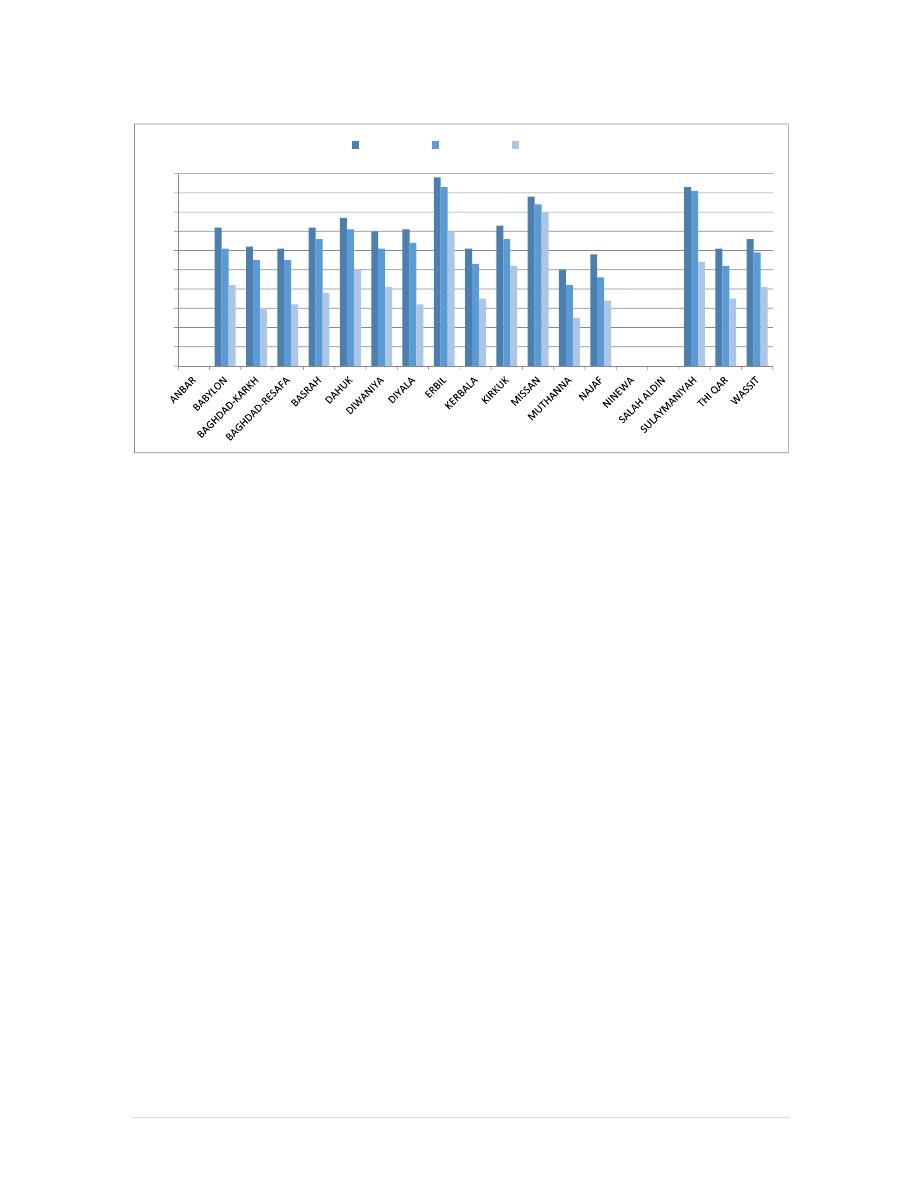
Figure 3: Number of Unvaccinated Children <1 Year with OPV3 by Governorate, 2013 Iraq
Figure 4 and Figure 5 (missing data from three provinces due to security unrest) further
substantiate the varying coverage levels of OPV3 by Governorates, however in 2014, coverage
levels decreased in many Governorates.
89
83
76
76
73
71
59
51
29
0
10
20
30
40
50
60
70
80
90
100
BCG Cov
PEN1 Cov
OPV3 Cov
MMR Cov
PEN2 Cov
MEA Cov
ROT1 Cov
ROT2 Cov
ROT3 Cov
0
5000
10000
15000
20000
25000
30000
35000
40000
13 |
P a g e
Figure 4: OPV3 Coverage by Governorate, 2013
Figure 5: OPV3 Coverage by Governorate, 2014
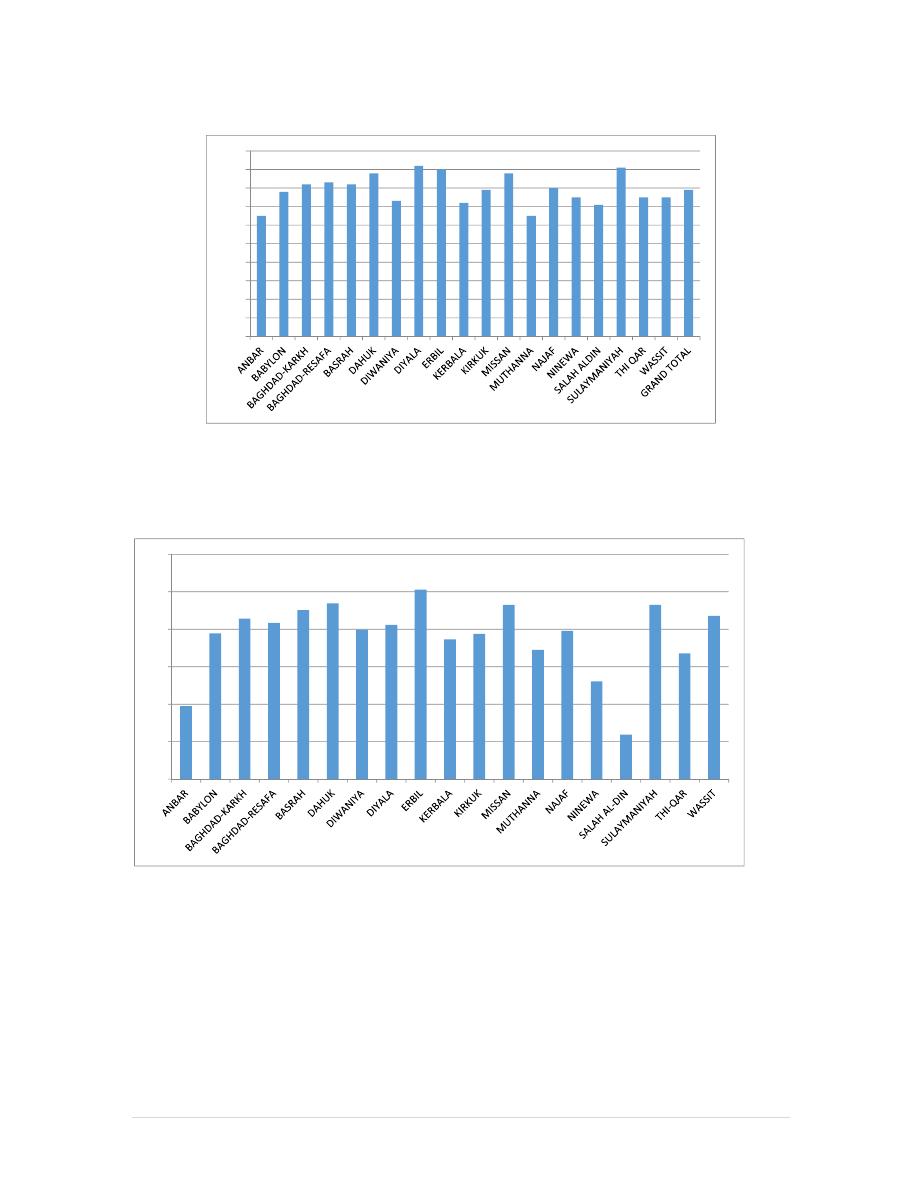
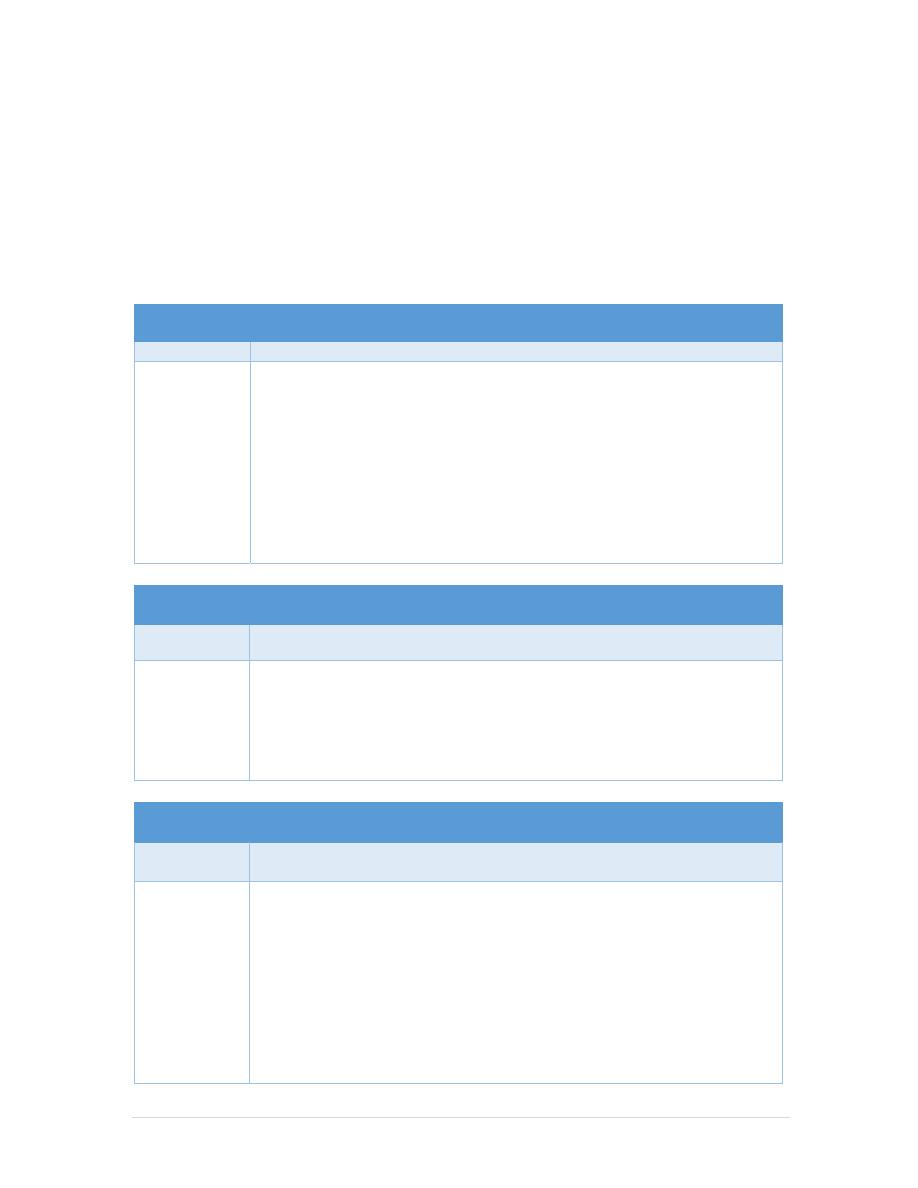
The next two Figures indicate levels of dropout between Penta1 and Penta2 (Figure 6) and
PENTA 1-measles (Figure 7). In general, Penta1 coverage is fairly high in most provinces, but
there is a 7-10% drop from Penta1 to Penta2.
The dropout rate between DTP1 and measles is much higher (Figure 7) ranging from 9% in
Kirkuk to 34% in Baghdad- Rusafa. Ten of the 15 Governorates had a dropout rate of over 15%.
Reducing dropout rates should be of priority in 2015.
65
78
82 83 82
88
73
92 90
72
79
88
65
80
75
71
91
75 75
79
0
10
20
30
40
50
60
70
80
90
100
39
78
86
83
90
94
80
82
101
75
78
93
69
79
52
24
93
67
87
0
20
40
60
80
100
120
14 |
P a g e
Figure 6: Comparison between Penta 1 and Penta 2, 2014
Figure 7:
Sum of Dropout DTP1 and DTP3
, 2014
45
78
89
89
104
105
95
81
118
84
83
99
82
87
60
30
104
80
90
39
69
81
77
90
94
79
74
101
72
76
94
66
77
54
23
92
67
84
0
20
40
60
80
100
120
140
PEN1 Cov
PEN2 Cov
12.9
11.4
9.1
13.9
13.6
10.5
16.6
9.2
13.9
15.0
8.4
5.5
19.6
11.6
10.2
21.8
11.3
16.5
6.6
0.0
5.0
10.0
15.0
20.0
25.0
15 |
P a g e
Figure 8: Comparison of Rotavirus Vaccine Coverage, 2014*
The low achieved coverage with rota3 dose is attributed partially to introduction of two types of Rota vaccines,
ROTATEQ with a recommended three doses and ROTARIX with two doses only
7. Strengths, Issues of Concern and Challenges
Points of strength
Good systematic documentation and analysis of EPI data through VACC-IFA database;
Partial implementation of DQS;
Good surveillance system for VPDs (attention to hot zones still needed) and more than 95%
of the reporting sites reporting timely and regularly;
Satisfactory integration between EPI, CDC and CPHL with a feedback from center to the
governorates (almost 100%);
Sustained funding of EPI activities by the Government and USAID, UNICEF and WHO.
Adequate coordination and collaboration between National EPI Team and concerned partners
(USAID, UNICEF and WHO).
Conducting a substantial numbers of POLIO SIAs that stopped WPV transmission.
Presence of an efficient and adequate vaccine cold chain system with significant expansion
of its capacity in 2014.
Issues of concern
Lack of accurate demographic data (as the last census was conducted in 1987);
Over reporting of the achieved coverage of targeted age groups.
Low routine immunization coverage levels (OPV3, Penta2, Hep B3 and measles).
High level dropout rates, especially between Penta1 and measles;
Rapid turnover of trained EPI staff;
Bureaucratic financial regulations and instructions.
Complicated vaccines procurements procedure;
Security issues.
72
62
61
72
77
70
71
98
61
73
88
50
58
93
61
66
61
55
55
66
71
61
64
93
53
66
84
42
46
91
52
59
42
30
32
38
50
41
32
70
35
52
80
25
34
54
35
41
0
10
20
30
40
50
60
70
80
90
100
ROT1 cov
ROT2 cov
ROT3 cov

16 |
P a g e
Inadequate AEFI reporting system;
Private sector involvement is inadequate
Key challenges
The main challenges facing EPI.
A deteriorating security situation;
competing health priorities;
poor management of health systems;
inadequate monitoring and supervision;
vaccine transportation in/out of national vaccines store;
a rapidly depleting capital of human resources for health;
difficulty in reaching vulnerable children/women in high risk areas as well as an
increasing number of IDPs;
Ineffective monitoring and supervision activities; and lack of sustained operational
resources.
V.
National Immunization Plan for 2015
1. Vision of the National EPI Program
The long term vision of the National EPI program for Iraq are as follows:
1. Every child born and present in Iraq should receive complete, safe and high quality EPI
services;
2. All people at-risk should be protected from vaccine preventable diseases.
2. Guiding Principles of the National EPI Program
1. Maximize access to EPI services by expanding provision of vaccination in hospitals and
reestablishment of outreach immunization sessions
2. Improve EPI services to decrease the dropout rate and control EPI targeted diseases
3. Introduction of pneumococcal conjugated vaccine and IPV in 2015.
4. Special budget for EPI allocated from the Ministry of Finance to cover all routine and
supplementary immunization activities.
5. Ensuring wide range community participation in the planning and implementation of EPI
activities.
6. Full range of coordination and cooperation with WHO –USAID- UNICEF for
implementation of national and global strategies to achieve planned goals.
7. Establishing work plans, products and services sufficient to achieve expected results.
8. Establishing an emergency preparedness plan in the event of a pandemic.
9. Raise the protection of all populations against VPDs and ensuring equity.
10. Increase vaccine storage capacity and improve distribution system.
11. Improve quality of cold chain system.
17 |
P a g e
3.
Goals of the EPI program in Iraq
1. Reduction of morbidity and mortality from EPI targeted diseases.
2. Stop transmission of poliomyelitis by 2015.
3. Control measles outbreaks and eliminate rubella and CRS (congenital rubella syndrome).
4. Maintaining MNT elimination.
4. Objectives and Planned Activities for 2015
Objective 1
Stop transmission of poliomyelitis virus
Milestone
Zero laboratory confirmed Polio case under high quality of surveillance.
Activities
Improve routine coverage of OPV3 to 95% at national level and 90%
at district level/ along all the year
Implement four NIDs and emergency SNIDs campaigns with OPV/
along all the year
Mop-up campaigns according to the epidemiological situation/ along
all the year
Executing the comprehensive national plan for combating imported
poliomyelitis cases/ first quarter of the year
Sustain an effective surveillance system for timely detection of AFP
cases/ along all the year
Objective 2
Maintain the current status of MNT (Maternal & Neonatal Tetanus)
elimination
Milestone
Maintain less than 1 case per 1000 live births
Activities
Achieve routine immunization coverage for pregnant women and
women of child bearing age of 85% at national level and 80% at
district level
Improve coordination and communication through quarterly meetings
with concerned personnel centrally and peripherally (MCH, CPHL,
CDC)
Objective 3
Prevent measles outbreaks and eliminate rubella and CRS (congenital
rubella syndrome)
Milestone
Reduction in the number of measles outbreaks
Zero cases of rubella
Activities
Raise routine immunization coverage to 95% at national level and
90% at district level (measles).
complete Phase 1 national measles campaign for children aged 9
months to 5 years/ on arrival of required vaccine.
National campaign using MR vaccine for age group (14-22 years) / on
arrival of required vaccine.
Maintain surveillance system for detection of all cases of (fever and
rash) and suspected CRS through an explicit and delineated work plan
using all prerequisite preventive resources
Maintain national measles laboratory activities
18 |
P a g e
Objective 4
Control all types of viral hepatitis
Milestone
Reduction in the number and frequency of cases compared to 2014
Activities
Increase routine immunization coverage to 95% with Pent2/ along all
the year
Increase coverage with birth dose within the first 24 hours of birth to
60%/ along all the year
Vaccination of high-risk groups with HepB for adults, specifically
students of medical colleges, health institutes and institutes of
mentally disabled in cooperation with the Ministry of Labor and
Social Affairs/ along all the year
Vaccinating immune-compromised patients, thalassemia patients,
those with hemophilia and those who need continuous blood
transfusions with viral hepatitis type A and type B/ along all the year
Objective 5
Control of other EPI targeted diseases through reducing number and
frequency of cases in comparison to 2014
Milestone
Reduction in the number of reported cases of diphtheria, pertussis
(whooping cough), Hib, Mumps, rota, TB and tetanus.
Activities
Improve routine coverage to 95% for EPI targeted diseases. / along
all the year
Objective 6
Improve the quality of immunization activities in PHCCs and districts
through application of service indicators and standards
Milestone
Improvement in service indicators and standards
Activities
Improve data quality through continues and regular data monitoring.
/ along all the year
Training of vaccinators and supervisors on DQS (data quality self-
assessment).
Strengthen electronic management of logistics distribution.
Ensure adequate stocks and cold chain equipment.
19 |
P a g e
Objective 7
Achieve 95% routine immunization coverage of all EPI vaccines at
national and provincial levels and at least 90% at district level
Milestone
Coverage levels as measured through MOH routine reports and periodic
surveys if and where possible
Activities
Expanding routine immunization network through additional fixed
and mobile sites for remote regions and IDP zones/ first quarter of
the year
Improve utilization through improving service delivery at vaccination
sites. / along all the year
Minimize missed opportunities/ along all the year
Adopt proper precautions and contraindications/ along all the year
Strengthen community involvement/ along all the year
Objective 8
Ensure uninterrupted vaccine supply
Milestone
No periods of vaccine shortage
Activities
Ensure political and financial commitment to provide the required
vaccines and other logistics. / first quarter of the year
Regular meetings with KEMADIA to ensure vaccines availability
around the year
Facilitating procurement of vaccines by WHO and UNICEFt/first
half of the year
Continues monitoring of vaccines stocks at all levels (Central,
DOHs, districts and PHCC). / along all the year
Objective 9
Capacity building of immunization personnel
Milestone
Number of personnel trained at various levels on various topics
Activities
Training of vaccinators by DOH (2-4 participants from each PHC
Center (twice yearly)
Training of supervisors (District and DOH) /first half of the year
Training of EPI Managers at DOHs and districts levels through
conducting 5 training courses. /first half of the year
Developing/editing training guidelines according to need
20 |
P a g e
Objective 10
Strengthen supervision
Milestone
Number of effective supervisory visits
Activities
Supervision and monitoring of high risk areas (monthly at district
level)
Monitoring and evaluation of data quality at DOH level (quarterly)
Monitoring and evaluation of data quality at district level (quarterly)
Monitoring and evaluation of data quality at PHCC (every two
months)
Supervision of EPI activities at PHCC (every two months)
Ensuring safety practices at all level with especial emphasis at PHCC
level./ monthly
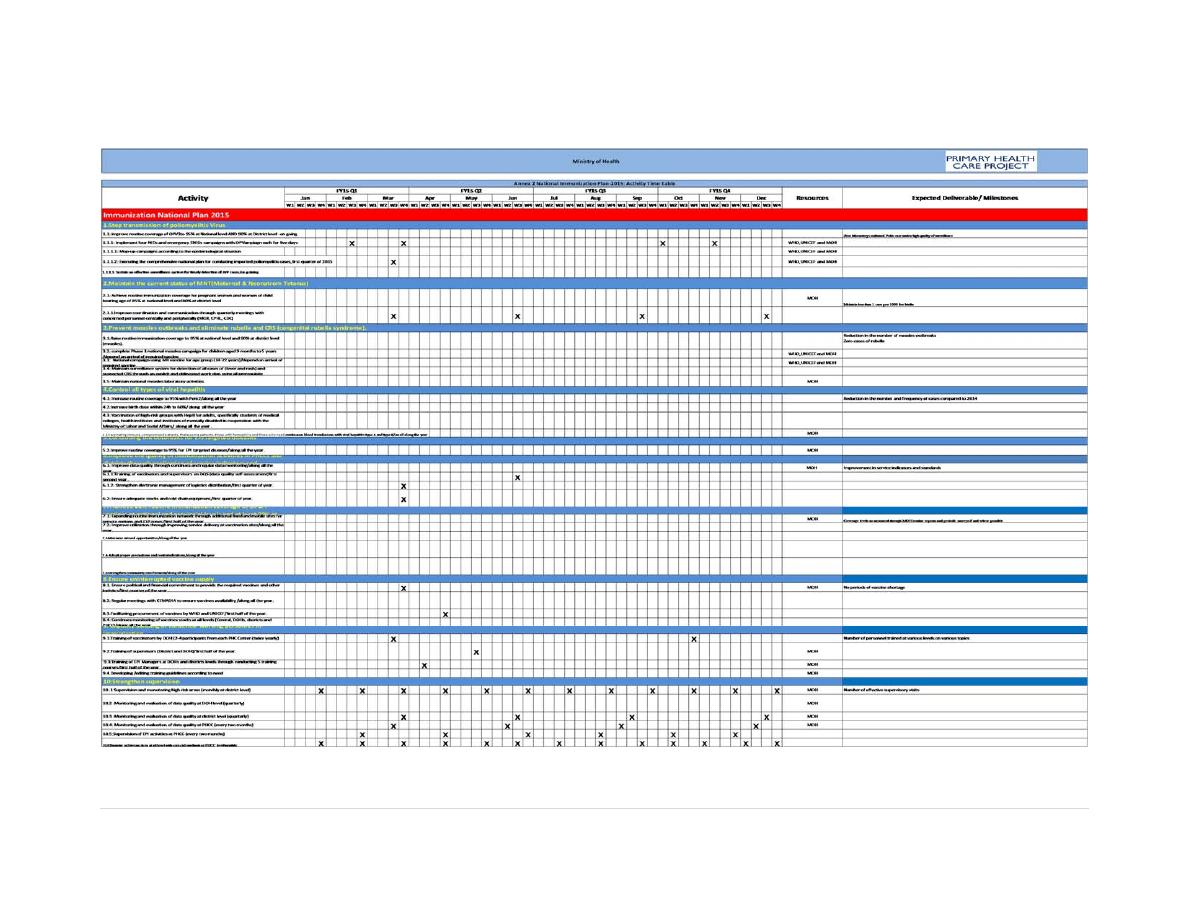
These objectives and activities are presented in a Gantt chart in Annex 2.
VI.
Monitoring and Evaluation
1. Strategic approaches to ensure an effective immunization program
The national strategies should be geared towards increasing routine immunization in an integrated
and
sustainable manner in order to increase access to and use of services.
Advocacy and broad-based partnerships with provincial government agencies, technical and
financial support organizations (WHO, UNICEF and USAID), civil society entities such as
provincial authorities, religious leaders, community health agents, NGOs, private health
services, and so on.
Information, education and communication to strengthen the capacity of families and
communities to actively seek vaccinations in order to complete children's courses of
immunization before they reach one year of age. For this purpose, educational messages will
be disseminated through - mainly local - mass media (radio and television) and local activists
such as traditional leaders, religious leaders and community agents will be mobilized (talks,
theatre, community debates, house-to-house visits).
Integration of routine immunization activities with other health interventions with the aim of
reducing costs and optimizing benefits for the health of the population.
The objectives of this plan will be met through effective implementation of all the activities listed
under each objective. To ensure success, following program aspects will be strengthened:
1. Ensure uninterrupted vaccine supply through full coordination with KEMADIA (General
Company for drug marketing and Medical Appliances), political commitment, financial
commitment and improved DG leadership.
2. Capacity building of EPI staff at various levels through refresher trainings, periodic meetings
and supportive supervision.
21 |
P a g e
3. Continuous and regular monitoring of EPI targeted diseases incidence in coordination with
the CPHL and Center for Control of Communicable Diseases (CDC).
4. Taking timely preventive and outbreak response measures in coordination with the CDC.
5. Use the reaching every child (REC) approach for increasing immunization coverage for all
EPI vaccines and reaching planned objectives at each PHC sector level.
6. Effective planning and timely implementation of all NIDs and other SIAs depending on the
epidemiological situation.
7. Upgraded quality of immunization activities in PHC centers and districts through regular
monitoring of performance indicators regarding vaccination activities.
8. Coordinating with other supporting governmental institutions and civil society institutions
and the municipality council for insuring effective community participation in planning and
execution of campaigns.
9. Achieve Immunization coverage will be further expanded and intensified through PHCCs,
sub-centers, outreach sites and other sectors as follows:
2. Key Performance Indicators
At the input level:
Timely release of funds (no shortages or delays);
Timely availability of vaccines and other supplies (shortages, if any); and
Availability of immunization staff at all levels (staff shortages, especially vaccinators and
supervisors).
At the Immunization site level:
Implementation of fixed and outreach immunization sessions at each level as per the
micro-plans (through monitoring of district level monthly reports);
Implementation of SIAs and other campaigns as per the plan (coverage levels by district
and high-risk areas);
Governorate and district level inter-sectorial coordination meetings (through monthly
reports); and
Monthly review of coverage and implementation issues (through local area monitoring by
supervisors).
At the performance/output level:
Immunization coverage levels of each EPI vaccine;
Occurrence of vaccine preventable diseases as per the surveillance reports;
Stopping of wild polio virus transmission;
Control of measles outbreaks and reduction of cases to < 1 / 1000000 total population.
Other indicators as per the milestones indicated under each objective.
Monitoring will be through routine DOH reports and periodic supervisory visits assessments.

22 |
P a g e
Recording and flow of information about routine immunization activities
The forms for recording the outreach immunization activities will be the same as for fixed
immunization activities and the results of the two types of activities will be integrated.
At the district level, the reports of all the PHCCs will be integrated in the monthly routine
immunization report.
The monthly reports of all the districts send to the DOH by the 7
th
of each month, as an
original or scanned copy.
The monthly reports of all the DOHs send to MOH/EPI by the 15
th
of each month, as an
electronic and original copy.
Implementation of high-quality NIDs against vaccine-preventable diseases
Improve the micro-planning and micro-mapping at district and PHCC levels
Enhancing the technical capacity of vaccinators and supervisors.
Recruitment, training, redeployment of special teams to support campaigns in areas of
high risk and difficult access.
Proper monitoring by recruiting and training of independent monitors.
Provision of adequate operational costs.
3. Financing of immunization activities
The immunization program is led and run by the MOH with the support of international agencies.
The Government of Iraq funding to the program is in terms of human resources, salaries, facilities
and establishment and operational costs. UNICEF, USAID and WHO support the EPI of Iraq
with technical, logistics and operational costs.
VII.
Strategies towards program sustainability
To ensure sustainability of the program, the GOI will ensure effective mechanisms for sustainable
financing and vaccine supplies. Mobilizing of the fund for the country program in the next year
plan period should be considered especially with the emergence of new outbreaks and evolving
situation of IDPs in Iraq. All efforts will be made to leverage resources to facilitate introduction
of new vaccines like (IPV, conjugated pneumococcal) in the country program. The program, as
part of its regular monitoring process, will monitor the trends in financing to ensure it is moving
towards improved financial sustainability by reducing its financing gaps. Indicators for financial
sustainability that the program will use include:
%
of funding gaps to total program needs for the period of 2015-2016;
% of total program costs financed by government;
% of total program costs financed by non-government sources;
What percentage of total routine vaccine spending was financed using government funds.
This is a one year work plan and these activities need to be sustained year after year with further
improvement and modifications as needed. Strategies for sustaining these activities will depend
on:

23 |
P a g e
Adequate and timely funding by the GOI and donor partners;
Political and programmatic commitment;
Effective program management – planning, implementation, supervision, monitoring
and timely corrective action; and
Community mobilization.
Long term strategies should be articulated upon the following:
Strategies to ensure effectiveness/efficiency of the immunization program;
Strategies to increase resource allocations
Strategies to increase resource reliability.
At the World Health Assembly in 2014, Member States addressed the following:
“Sustainable access to vaccines—especially newer vaccines—at affordable prices for all
countries;
technology transfer to facilitate local manufacture of vaccines as a means of ensuring
vaccine security;
improved data quality including through the use of new technologies like electronic
registries;
risk communication and management to address misinformation on immunization and
its impact on vaccination coverage; and
Evidence reviews and economic analysis for informed decision-making based on local
priorities and needs”.
24 |
P a g e

25 |
P a g e
VIII.
References
1. WHO/Department of Immunization, Vaccines and Biologicals (Training for mid-level
managers) (MLM) Module 6: Making a comprehensive annual national immunization
plan and budget, 2008.
2. Michel Zaffran (Coordinator, WHO/EPI): Global Progress, Challenges, Opportunity
and Looking Forward, 28th Intercountry Meeting of National EPI Managers, Amman-
Jordan, November, 2014.
3. Republic of Iraq ,Ministry of Health ,Directorate of Planning and resources
Development
4. Annual Statistical Report 2013.
5. G IVS Global Immunization Vision and Strategy 2006-2015.
6. MICS4: Multiple Indicators Cluster Survey Round 4, UNICEF, 2011.
7. MOH, cMYP and routine MOH EPI coverage and surveillance data, 2010.
