1
Local anesthetics
Local Anesthetics
DEFINITION
Drugs which
produce a REVERSIBLE loss of sensation …
In a localized part of the body….. interfering with nerve conduction
without loss of consciousness
when applied directly onto nerve tissues or mucous membranes
Local anesthetics are ‘local’ ONLY because of how they are administered!
(Selectivity)
The first clinically used Local Anesthetic
Cocaine
A natural alkaloid from Erythroxylon coca.
Prototype Drug Lignocaine (Synthetic)
MECHANISM OF ACTION
Diffusion into the nerve fiber
Blockade of sodium channels
Mechanism of action:
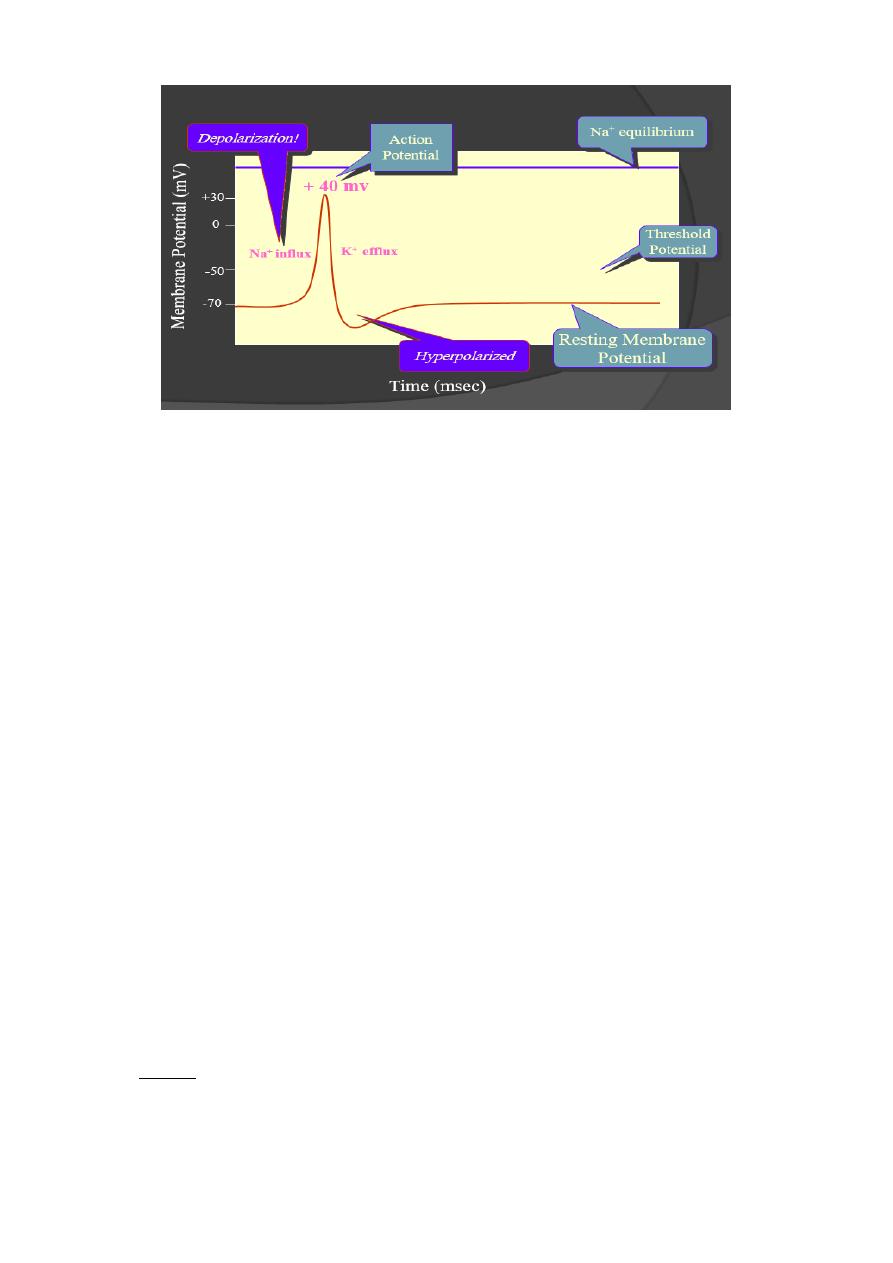
Blocking of Na –channels which are responsible for depolarization so no depolarization
and no action potential ( i.e rising threshold of action potential and slowing impulse
conduction ).
2
Progressively increasing conc. of a LA applied to a nerve fiber produce blockade of more &
more Na+ channels :
The threshold for excitation increases
Impulse conduction slows
The rate of rise of AP declines
Finally the ability to generate an AP is abolished
Properties Desirable in a Local Anesthetic
Non-irritating
Do not cause permanent damage to nerve structure
Systemic toxicity should be low
Effective
Injected
Applied locally
Onset of action as short as possible
The effect of local anesthetic on nerve depend on:
1. Diameter of the nerve: the smaller, the rapid onset of action.
2. State of myelination: mylinated n.f are more rapidly anesthetized.
3. position of fibers ( cord, root , plexus)
4. Frequency of conduction: the faster the frequency, the more rapid onset of
anesthesia.
CLASSIFICATION ACCORDING TO CHEMISTRY
ESTERS
Cocaine
Procaine
Tetracaine
3
Benzocaine
AMIDES
Lignocaine/Lidocaine
Bupivacaine
o Mepivacaine
Prilocaine
o Ropivacaine
CLASSIFICATION ACCORDING TO CLINCIAL USES
SURFACE ANESTHESIA
Tetracaine
Lignocaine
Cocaine
Benzocaine
INFILTRATION ANESTHESIA & FIELD BLOCK ANESTHESIA
Lignocaine
Procaine
Bupivacaine
NERVE BLOCK ANESTHESIA
Procaine
Lignocaine
Bupivacaine
Tetracaine
SPINAL ANESTHESIA
Lignocaine
Tetracaine
Bupivacaine
EPIDURAL ANESTHESIA
Lignocaine
Bupivacaine
ANESTHETIC USED IN OPHTHALMOLOGY
Proparacaine
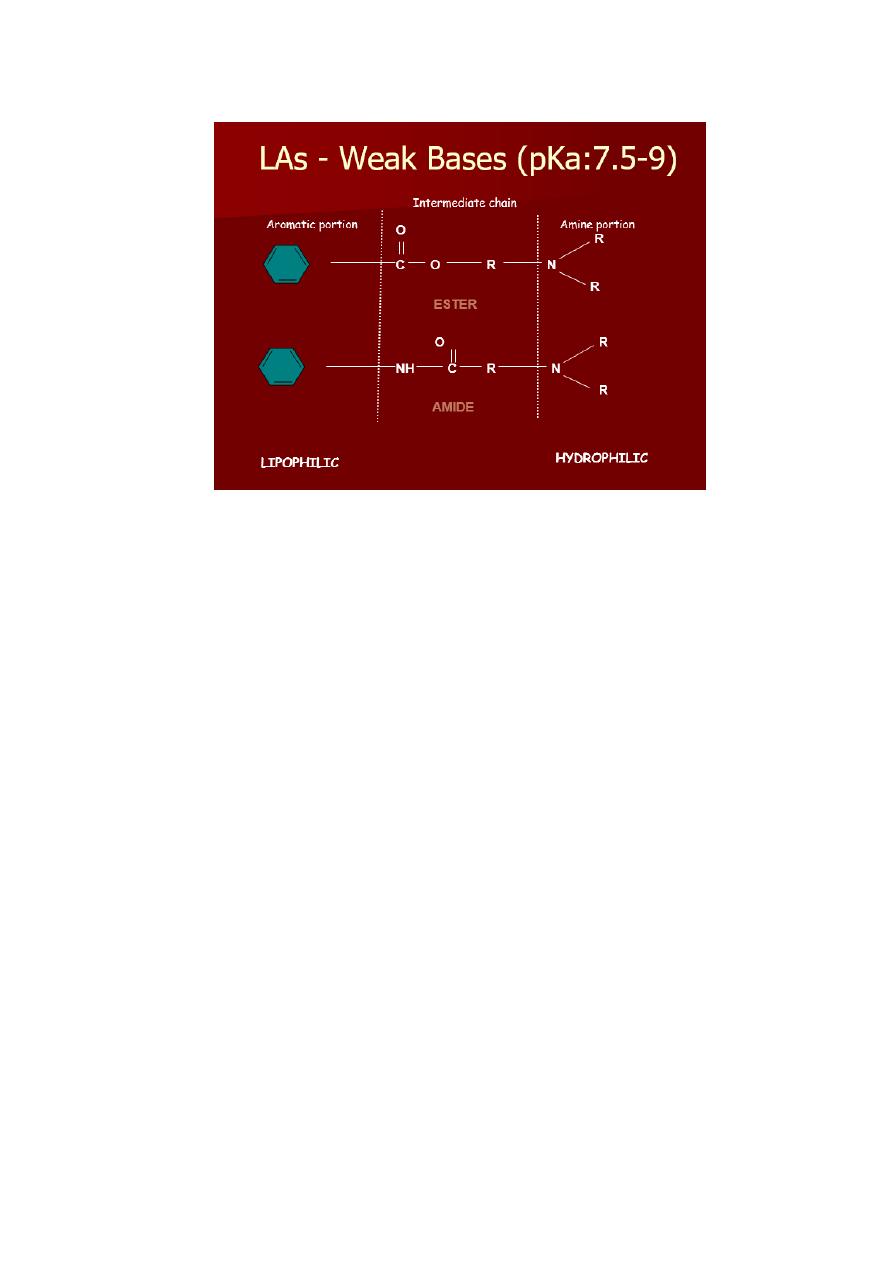
Chemistry
Most local anesthetics consist of 3 parts
1. Lipophilic Aromatic group
2. Intermediate chain
3. Hydrophilic Amino group
4
ORDER OF BLOCKADE
AUTONOMIC
PAIN
TEMPERATURE
TOUCH
MOTOR
Cocaine
Medical use limited to surface or topical anesthesia
Avoid epinephrine because cocaine already has vasoconstrictor properties.
(EXCEPTION!!!)
A toxic action on heart may induce rapid and lethal cardiac failure.
A marked pyrexia is associated with cocaine overdose.
SELECTIVE PHARMACOLOGICAL
Benzocaine
Available for relief of pain and irritation
for surface anesthesia (topical) only ... ointments, sprays, etc.
Used to produce anesthesia of
mucous membranes
LIDOCAINE (Xylocaine) Most widely used LA
Effective by all routes.
Faster onset, more intense, longer lasting, than procaine.
Good alternative for those allergic to ester type
5
More potent than procaine but about equal toxicity
More sedative than others
Bupivacaine (Marcaine)
o No topical effectiveness
o Slower onset and one of the longer duration agents
o Unique property of sensory and motor dissociation can provide sensory
analgesia with minimal motor block
has been popular drug for analgesia during labor
o More cardiotoxic than other LA
Clinical aspects
Applications of local anesthesia:
nerve block: injected locally to produce (e.g., dental and other minor surgical
procedures)
topical application: to skin for analgesia (e.g., benzocaine) or mucous
membranes (for diagnostic procedures)
spinal anesthesia: injection into CSF to produce anesthesia for major surgery
(e.g., abdomen) or childbirth
local injection: at end of surgery to produce long-lasting post-surgical analgesia
(reduces need for narcotics)

6
i.v. infusion: for control of cardiac arrhythmias (e.g., lidocaine for ventricular
arrhythmias)
Notes:
1. L.A are not effective in case of abscess because inflammation lead to acidosis
that prevent ionization of the cationic amine group so prevent binding to
receptor.
2. To prolong the duration of action of L.A vasoconstrictor agents are added like
adrenaline. To terminate the action of NA α-blockers are used as phentolamine.
3. To avoid systemic side effects of NA in patients with CVS diseases , felyspressin
another vasoconstrictor agent is used.
4. In case of impaired liver function , large repeated doses of amide compounds
may predispose to toxicity.
5. Lignocain is one of antiarrhythmic drugs ( class1b)
Adverse effects of L.A:
in case of systemic absorption:
1. CNS: parasthesia, visual disturbances, convulsions.
2. CVS: hypotension , brady cardia.
3. Respiratory: hyperventilation, alkalosis and resp. failure.
Procedure:
1- 2 volunteers
2- 1
st
: received 3 I.D injections of normal saline, lignocaine 2%, lignocaine2%+
adrenaline1: 100000 in the flexor aspect of the forearm. Then blebs and
surrounding areas are pricked with sterile needle and the volunteer indicate if he
feel the pricks, and no. of pricks felt is recorded. the procedure repeated after 5, 10
,15 minutes. Comparision between the onset and duration of anesthesia is done.
3- 2
nd
: apply topical lignocaine on lips and lignocain spray on tongue. After 5,10,15
minutes the volunteer describe sensation for light touch , deep touch,pain and taste
( sweet, salt,sour,bitter)
