Lecture 2
Dr. Basil M.N. SaeedProfessor of Otorhinolaryngology
Inflammation of the Larynx
Acute Laryngitis in Adults
An acute superficial inflammation of the laryngeal mucosa.Aetiology
Infection: Its most frequently caused by adeno or influenza viruses but secondary bacterial infection may supervene. Acute laryngitis occurs as part of respiratory tract infection or as an isolated disease.
Trauma: Vocal abuse or endoscopic manipulation.
Irritation: Inhaled fumes, smoking or alcohol abuse.
Clinical Picture
Hoarseness of voice or complete loss of voice.
Discomfort and pain in the throat (sore throat).
Dry and irritative cough.
Generalized symptoms: malaise and fever.
Examination
Indirect and fiberoptic laryngoscopy reveals:
Redness and oedema of the larynx.
The vocal cords is covered with mucous and pus.
Treatment
Bed rest and vocal rest, and Steam inhalation.
Avoidance of tobacco and irritating agents.
Systemic antibiotics if there is secondary bacterial infection.
Acute Laryngotracheobronchitis (croup)
It’s an inflammatory condition of the larynx, trachea and bronchi. Its more common than acute epiglottitis.Aetiology
It affects infants and young children. Causative organism is usually parainfluenza virus type I and II. Secondary bacterial infection is common and makes the condition worse.
Clinical Picture
It affects children 6 months to 3 years of age. There is frequently a preceding nasal or pharyngeal infection followed by:
Dry croupy or barking like cough with hoarseness.
Inspiratory stridor and dyspnea.
Constitutional symptoms: fever and tackycardia.
Examination
Oedema and redness of the larynx.
Tenacious exudation and crusting over the larynx.
Investigations
Anteroposterior X-ray of the neck shows subglottic narrowing (steeple sign).
Treatment
Reassurance and rest.
Oxygen.
Adequate hydration.
Humidification of the inspired air.
Systemic antibiotics to overcome the secondary bacterial infection.
Steroids: using hydrocortisone or dexamethasone to reduce the inflammatory oedema.
Nebulized ventolin or racemic adrenaline administrated via a respirator is a bronchodialator
If signs of respiratory obstruction develop then intubation or tracheostomy is indicated.
Acute Epiglottitis
Affects young children 2-7 years of age, but it is less common and more dangerous than croup.
Aetiology
Haemophilus influenzae type B infection.
Clinical Picture
The onset is sudden and lethal airway obstruction can develop within hours. Symptoms are triad of drooling, dysphagia, and distress.
Sore throat and upper respiratory tract infection.
Inspiratory stridor develops rapidly and may end in sudden death.
Painful and difficult swallowing, so the child leans forward and drools saliva.
Muffled voice and cry resembling a “plum” in the throat.
High fever with toxaemia.
Examination
Depressing the tongue may show swollen, red cherry epiglottis but no attempt should be made to examine the larynx as this may end in fatal total obstruction. It is better done in operation theature where facilities for intubation or tracheostomy are available.
Investigations
Lateral X-ray of the neck may show swollen epiglottis (thumb sign).
Treatment
Once the diagnosis is suspected the child must be admitted to the hospital and intubation or tracheostomy should be kept in mind.
As croup.
Antibiotics: I.V. amoxycilin is the drug of choice, but the emergence of penicillin resistant strains, third generation cephalosporines (Ceftriaxone) by paranteral route are best used.
Intubation and tracheostomy is required in 60% of cases.
Steeple sign (Croup) Thumb sign (Epiglottitis)
Chronic LaryngitisA chronic inflammatory reaction of the larynx in which the laryngeal mucosa undergoes irreversible inflammatory changes. It may be diffused or localized.
Aetiology
Infection: repeated attacks of acute laryngitis or focal sepsis in the teeth, tonsils and sinuses.
Faulty use of the voice.
Excessive smoking and alcoholism.
Pollution by dust and irritant fumes.
Gastroesophageal reflux.
Symptoms
Hoarseness and tiredness of voice.
Irritation and raw sensation in the throat. A frequent desire to clear the throat is common.
Dry and irritating cough.
Examination Indirect and fibroptic laryngoscopy: Hyperaemia and oedema of the vocal cords. Excessive viscid secretions may be seen which results from increased activity of the mucous glands.
Investigation
Laryngoscopy is indicated if hoarseness persists for more than 3 weeks to exclude malignancy.
Treatment
Treat the predisposing factors
a. Elimination of focal sepsis in the teeth, tonsils and sinuses.
b. Voice rest and speech therapy.
c. Elimination of irritant factors as tobacco, fumes and alcoholism.
Medical treatment
Steam inhalation and application of laryngeal sprays.
Mucolytics (solvodin) when the secretions are thick and tenacious.
Antibiotics if there is secondary bacterial infection .
Surgical treatment
Endoscopic stripping of the vocal cords in resistant cases.
Vocal Cord Nodules
They are bilateral, small, grayish, white, localized thickening of the vocal cords situated at the junction of the anterior third and posterior 2/3 of the vocal cord. In this area maximum vibration occurs followed by fibrosis and traumatic scarring.
Aetiology
Misuse of the voice or bad voice production with straining. It is commonly seen in singers, teachers and actors affecting women more than men.
Pathology
A preliminary phase of submucosal transudation followed by ingrowth of vessels and then fibrous organization.
Clinical Picture
Hoarseness of voice.
Voice fatigue.
Examination
The site of nodule is at the junction of the anterior third and posterior 2/3 of the vocal cord.
Treatment
Small voice rest and speech therapyElimination of focal sepsis in the teeth, tonsils and sinuses.
Large endoscopic excision followed by voice rest.
Chronic laryngitis Vocal cord nodule
Laryngeal PolypSmooth unilateral glistering mass attached to the vocal cord due to accumulation of fluid in the sub-epithelial space.
Aetiology
Vocal abuse.
Heavy smoking and allergy.
Pathology
Accumulation of fluid in the sub-epithelial layer followed by ingrowth of new connective tissue, so the polyp becomes firm, inconsistency.
Clinical Picture
Hoarseness of voice.
A large polyp may result in choking spills and stridor.
Examination
Indirect laryngoscopy and fibroptic endoscopy: sessile or pedunculated mass arising from the vocal cord near the anterior commissure, but it can be seen anywhere in the larynx.
Treatment
Endoscopic excision followed by voice rest and speech therapy. Histological examination is necessary to exclude malignancy.
Intubation granuloma
It results from injury to vocal process of arytenoids due to rough intubation, use of large tube or propounded intubation.
Pathology
Mucosal ulceration is followed by granuloma formation over the exposed cartilage.
Clinical Picture
Patients are referred few days or weeks after an operation with hoarseness of voice. Stridor is rare.
Examination
Endoscopy reveals a large fleshy granuloma arising from the vocal process of arytenoids.
Treatment
Voice rest and endoscopic removal preferably with LASER.
Tumours of the Larynx
Benign
Epithelial
Connective tissue
Papilloma
Angioma
Fibroma
Chondroma
Malignant
Epithelial
Connective tissue
Sq. cell. CA
Sarcoma
Lymphoma
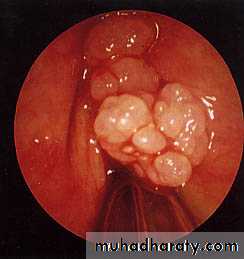
Papilloma
They can be divided into juvenile and adult onset types. They are known for recurrence after removal.Juvenile: They are multiple often involving infants and young children. They are not premalignant and tend to disappear after puperty.
Adult onset: Usually its single and arises from the free edge of the vocal cord in adults. It may undergo malignant changes.
Aetiology
Viral infection by human papilloma virus type 6 and 11. The virus is thought to be transmitted through the mother,s birth canal.
Clinical Picture
Hoarseness of the voice.
Stridor from interference with the laryngeal intet.
Examination
The papilloma commonly seen at the anterior aspect of the vocal cords.
Treatment
Endoscopic excision using LASER because of the precision in removal and less bleeding. Histological examination is necessary to exclude malignant changes.
Interferon therapy is being tried to prevent recurrence.
Tracheostomy in severe cases.