Gall bladder and biliary disease lecture no. 4
Dr .Muayad Abass Fadhelalmadena copy
1
In 15% of patients, cholecystectomy fails to relieve the symptoms for which the operation was performed. ‘post-cholecystectomy’ syndrome.
problems are usually related to the preoperative symptoms and are continuation of those symptoms. Full investigation should be undertaken to confirm the diagnosis
presence of a stone in the common bile duct,
a stone in the cystic duct stump
or operative damage to the biliary tree.
Late symptoms after cholecystectomy
Al-Madena copy
2
best DIAGNOSED by
MRCP or ERCP.The latter has the added advantage that, if a stone is found in the common bile duct, it can be removed.
Al-Madena copy
3
Patients with symptoms developing either immediately or delayed after a cholecystectomy, particularly jaundice ,need
urgent investigation.
Management of bile duct obstruction following cholecystectomy
Al-Madena copy
4
immediate ultrasound scan. whether there is intra- or extrahepatic ductal dilatation.
The anatomy defined by MRCP.ERCP therapeutic manoeuvres :
removal of an obstructing stone
insertion of a stent across a biliary leak.
If a fluid collection is present in the subhepatic space, drainage catheters may be required. These can be inserted under radiological control or, if this expertise is not available, at open operation.
Al-Madena copy
5Small biliary leaks will usually resolve spontaneously, especially if there is no distal obstruction.
Should the common bile duct be damaged, the patient should be referred to an appropriate expert for reconstruction of the duct.
Al-Madena copy
6
About 15% of injuries recognised at the time of operation.
In 85% of cases, the injury declares itself postoperatively by:(1) a profuse and persistent leakage of bile if drainage has been provided, or bile peritonitis if such drainage has not been provided;
(2) deepening obstructive jaundice.
Al-Madena copy
7When the obstruction is incomplete, jaundice is delayed until subsequent fibrosis renders the lumen of the duct inadequate.
The surgical repair and subsequent outcome is related to the level of injury, which is determined using the Bismuth classification
Al-Madena copy
8Bismuth classification
Type I Low common bile duct; stump > 2 cmType II Middle common hepatic duct; stump < 2 cm
Type III Hilar – confluence of right and left ducts intact
Type IV Right and left ducts separated
Type V Involvement of the intrahepatic ducts
Al-Madena copy
9
In the debilitated patient,
temporary external biliary drainage by passing a catheter percutaneously into an intrahepatic duct.stents may be passed through strictures at the time of ERCP and left to drain into the duodenum.
When the general condition improved,
Definitive surgery can be undertaken.
The principles of surgical repair are
maintenance of duct length and restoration of biliary drainage.
Treatment
Al-Madena copy
10
For benign stricture or duct transection, the preferred treatment is immediate Roux-en-Y choledochojejunostomy by an experienced surgeon.
For a stricture of recent onset through which a guidewire can be passed, balloon dilatation with insertion of a stent.
The outcome of such surgery is good, with 90% of patients having no further cholangitis or stricture formation.
Al-Madena copy
11PRIMARY STONES:occure years after a cholecystectomy or development of new pathology, such as infection of the biliary tree or infestation by Ascaris lumbricoides or Clonorchis sinensis.
Secondary stone (missed stone )from gall bladder
Any obstruction to the flow of bile can give rise to stasis with the formation of stones within the duct.
The consequence of duct stones is either obstruction to bile flow or infection.
Stones in the bile duct
Al-Madena copy
12
Stones in the bile ducts are more often associated with infected bile (80%) than are stones in the gall bladder
Al-Madena copy
13Symptoms
The patient may be asymptomaticMay has bouts of pain,
jaundice and fever. The patient is often ill and feels unwell. The
term ‘cholangitis’ is given to the triad of pain, jaundice and fevers,
sometimes known as ‘Charcot’s triad’.
Signs
Tenderness may be elicited in the epigastrium and the right hypochondrium.
In the jaundiced patient, it is useful to remember
Courvoisier’s law – in obstruction of the common bile duct
due to a stone, distension of the gall bladder seldom occurs; the
organ is usually already shrivelled. In obstruction from other
causes, distension of the gall bladder is common by comparison.
Al-Madena copy
14
Management
Full supportive measures are required with rehydration, correction of clotting abnormalities and treatment with appropriate broad-spectrum antibiotics.Al-Madena copy
15Once the patient has been resuscitated, relief of the obstruction is essential.
Endoscopic papillotomy is the preferred first techniquewith a sphincterotomy, removal of the stones using a
Dormia basket or the placement of a stent if stone removal is not possible.
If this technique fails, percutaneous transhepatic
cholangiography can be performed to provide drainage and subsequent percutaneous choledochoscopy.
Surgery, in the form of choledochotomy, is now rarely used for this situation, as most patients can be managed by minimally invasive techniques
Al-Madena copy
16The aim of this surgery is to drain the common bile duct and remove the stones by a longitudinal incision in the duct.
When the duct is clear of stones, a T-tube is inserted and the duct closed around it;
the long limb of the T-tube is brought out on the right side, and the bile is allowed to drain externally.
When the bile has become clear and the patient has recovered, a cholangiogram is performed, usually 7–10 days following operation.
If residual stones are found, the T-tube is left in place for 6 weeks so that the track is ‘mature’. The retained stones can be removed percutaneously by an interventional radiologist (Burhenne technique)
Choledochotomy
Al-Madena copy
17
Causes of benign biliary stricture
Congenital
■ Biliary atresia
Bile duct injury at surgery
■ Cholecystectomy
■ Choledochotomy
■ Gastrectomy
■ Hepatic resection
■ Transplantation
Inflammatory
■ Stones
■ Cholangitis
■ Parasitic
■ Pancreatitis
■ Sclerosing cholangitis
■ Radiotherapy
Trauma
Idiopathic
Stricture of the bile duct
Al-Madena copy18
■ Ultrasonography
■ Cholangiography via T-tube, if present
■ ERCP
■ MRCP
■ PTC
■ Multidetector row CT
Radiological investigation of biliary strictures
Al-Madena copy19
Benign tumours of the bile duct
uncommonless than 0.1% of biliary tract operations.
clinical presentation may mimic the more common conditions such as cholecystitis, choledocholithiasis,cancer of the bile duct and pancreatic cancer.
TUMOURS OF THE BILE DUCT
Al-Madena copy20
Benign neoplasms classificationas follows:
• papilloma and adenoma;• multiple biliary papillomatosis;
• granular cell myoblastoma;
• neural tumours;
• leiomyoma;
• endocrine tumours.
Al-Madena copy
21
Carcinoma may arise at any point in the biliary tree, from the common bile duct to the small intrahepatic ducts
Malignant tumours of the bile duct
Al-Madena copy
22
Incidence
rare malignancy accounting for 1–2% of new cancers in a western practice.two-thirds of patients being older than 65 years.
the tumour is usually an adenocarcinoma
(cholangiocarcinoma), predominantly in the extrahepatic biliary system.
Al-Madena copy
23Patients with a history of followings are at increased risk of developing the disease.
ulcerative colitis,hepatolithiasis,
Choledochal cyst or
sclerosing cholangitis
Al-Madena copy
24
longstanding history of sclerosing cholangitis increases the risk of developing biliary tract cancer by 20-fold compared with the normal population.
Al-Madena copy
25liver fluke infestations in the Far East are also associated with cholangiocarcinoma. Opisthorchis viverrini infestation is important in Thailand, Laos and western Malaysia.
These parasites induce DNA changes and mutations through production of
carcinogens and free radicals, which stimulate cellular proliferation in the intrahepatic bile ducts and can ultimately lead to invasive cancer.
Al-Madena copy
26slow-growing tumours that invade locally and metastasise to local lymph nodes.
Distant metastases to the peritoneal cavity, liver and lung may occur.Jaundice is the most common presenting feature.
Abdominal pain, early satiety and weight loss are also commonly seen.
Clinical features
Al-Madena copy27
On examination,
Jaundice is evident,
cachexia often noticeable
a palpable gall bladder is present if the obstruction is in the distal common bileduct (Courvoisier’s sign).
Al-Madena copy
28Investigations
Biochemical investigations will confirm the presence of obstructive jaundice (elevated bilirubin, alkaline phosphatase and gamma-glutamyl transferase).The tumour marker CA19-9 may also be elevated.
Non-invasive studies such as ultrasound and CT
scanning define the level of biliary obstruction, the locoregional extent of disease and the presence of metastase
Al-Madena copy
29For proximal tumours, percutaneous transhepatic cholangiography is the most useful modality.
PTC
outlines the anatomy of the tumour and the intrahepatic biliary system.
it allows percutaneous biliary drainage,
samples can be obtained for cytology
to confirm the diagnosis.
Al-Madena copy
30
. For distal tumours, an ERCP is preferred
as an endobiliary stent can be placed across the obstructing lesion.Again, cytology or biopsies can be taken for diagnosis.
Al-Madena copy
31Treatment
depends on the site and extent of disease.ONLY 10–15% are suitable for surgical resection.
. Most patients are inoperable,
Al-Madena copy
32Depending on the site of disease,
resection may involve partial hepatectomy and reconstruction of the biliary tree.Distal common duct tumours may require a pancreaticoduodenectomy.
The perioperative mortality rate is now less than 5%.
The median survival is 18 months, with 20% of patients surviving 5 years post resection.
Al-Madena copy
33
Survival appears to be better for distal tumours compared with those involving the upper third of the biliary tree.
Adjuvant chemotherapy or radiotherapy has a
limited role and is not considered standard therapy.
Al-Madena copy
34Bile duct cancer
■ Rare, but incidence increasing■ Presents with jaundice and weight loss
■ Diagnosis by ultrasound and CT scanning
■ Jaundice relieved by stenting
■ Surgical excision possible in 5%
■ Prognosis poor – 90% mortality in 1 year
Al-Madena copy
35Incidence
This is a rare disease
variable by geographical region and racial/ethnic groups.
The highest incidence is in Chileans,
American Indians and in parts of northern India, where it accounts for as much as 9.1% of all biliary tract disease.
Carcinoma of the gall bladder
Al-Madena copy
36
. In western practice, gall bladder cancer accounts for less than 1% of new cancer diagnoses.
The patients are usually older, in their sixties or seventies.
Al-Madena copy
37The aetiology is unclear, association with
preexisting gallstone disease.Calcification of the gall bladder is associated
with cancer in 10–25% cases.
Infection may promote the development of cancer as the risk of carcinoma in typhoid carriers is significantly increased .
Al-Madena copy
38
Pathology
The majority of cases are adenocarcinoma (90%).; the tumour is most commonly nodular and infiltrative, with thickening of the gall bladder wall, often extending to the whole gall bladder.
Al-Madena copy
39The tumour spreads by direct extension into the liver, seeding of the peritoneal cavity and involvement of the perihilar lymphatics and neural plexuses.
At the time of presentation, the majority of tumours are advanced.
Al-Madena copy
40Clinical features
Patients may be asymptomatic at the time of diagnosis.. If symptoms are present, they are usually indistinguishable from benign gall bladder disease such as biliary colic or cholecystitis, particularly in the older patient.
Jaundice and anorexia are late feature.
A palpable mass is a late sign
Al-Madena copy
41
Investigation
Laboratory findingsmay be consistent with biliary obstruction
or non-specific findings such as anaemia, leucocytosis, mild elevation in transaminases and increased erythrocyte sedimentation
rate (ESR) or C-reactive protein (CRP).
Al-Madena copy
42The level of serum CA19-9 is elevated in 80% of patients.
The diagnosis is made on ultrasonographydefined by a multidetector row CT scan,
percutaneous biopsy confirming the histological diagnosis.
laparoscopy is useful in staging the disease, as it can detect peritoneal or liver metastases that would preclude further surgical resection.
Al-Madena copy
43Treatment and prognosis
Occasionally, the diagnosis is made by histological examination of a gall bladder removed for ‘benign’ gallstone disease.
For early stage disease confined to the mucosa or muscle of the gall bladder, no further treatment is indicated.
However, for transmural disease, a radical en bloc resection of the gall bladder fossa and surrounding liver along with the regional lymph nodes should be performed.
Al-Madena copy
44The disease has a very poor prognosis with the median survival less than 6 months and a 5-year survival of 5%.
The value of adjuvant therapy is unproven.
Al-Madena copy
45Gall bladder cancer
■ Rare■ Presents as for benign biliary disease (gallstones)
■ Diagnosis by ultrasound and CT scanning
■ Excision in less than 10% – remainder palliative treatment
■ Prognosis poor – 95% mortality in 1 year
Al-Madena copy
46
Preperation of a Patient with Obstructive Jaundice for Surgery
• Correct Anaemia if Present• Good Hydration with i.v. fluids to prevent dehydration & maintain the Renal Function
• Mannitol i.v. infusion to maintain osmotic diuresis and prevent Bilirubin from precipitating in the tubules.
• Vitamine K injectable to activate important clotting factors (fat soluble vitamines are not absorbed)
• Add 5% Glucose Water to help build up Liver glycogen
• Antibiotics Broad Spectrum
Al-Madena copy
47
TRAUMA of biliary tree
blunt or penetrating abdominal trauma.Operative trauma is perhaps more frequent than external trauma.
physical signs are those of an acute abdomen.
Management depends on the location and extent of the biliary and associated injury.
In the stable patient, a transected bile duct is best repaired by a Roux-en-Y choledochojejunostomy.
Injuries to the gall bladder can be dealt with by cholecystectomy.
Al-Madena copy
48
Al-Madena copy
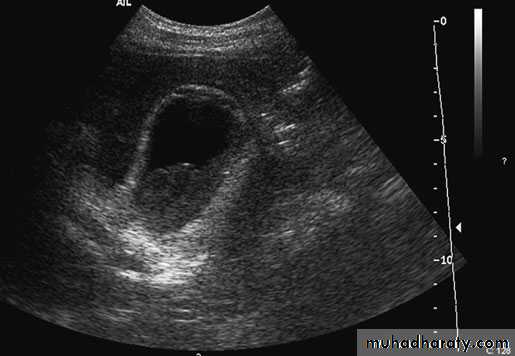
49Cholecystitis. Ultrasound demonstrates pericholecysticfluid (thin arrow), gall bladder wall (thick arrow) and biliary sludge
Al-Madena copy
50Al-Madena copy
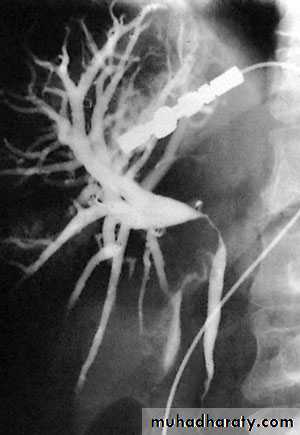
51NORMAL ERCP
Al-Madena copy
52
Endoscopic retrograde cholangiopancreatographydemonstrating stone obstructing the common bile duct (arrow
Al-Madena copy
53Transhepatic cholangiogram showing a stricture of thecommon hepatic duct
Al-Madena copy
54Gas in the gall bladder and gall bladder wall(Clostridium perfringens). Emergency surgery is indicated.
Al-Madena copy
55Endoscopic retrograde cholangiopancreatography: thepatient presented with jaundice 4 days after laparoscopic cholecystectomy.The bile duct contained multiple stones
Al-Madena copy
56Extraction of a stone from the common bile duct by theBurhenne technique. (a) A T-tube in situ with a stone in the duct. (b) Asteerable catheter has been manipulated into the duct and a basketplaced around the stone. (c) The stone being extracted from the bile ductalong the T-tube track.