Acute peritonitis and intra-abdominal abscesses
Lec:11Dr. Basim Rassam
Al-Madena copy1
INTRA-ABDOMINAL infections result in two major manifestations..
1-early or diffuse infection result in localized or generalized peritonitis.2-late and localized infection produces.. intra-abdominal and pelvic abscesses.
Learning Objectives
To recognize and understand:
* The clinical features of localized and generalized peritonitis.
* The common causes and complications of peritonitis.
* The principles of surgical management in patients with peritonitis.
* The clinical presentations and treatment of abdominal/pelvic abscesses.
* The clinical presentations of tuberculosis peritonitis.
ACUTE PERITONITIS AND INTRA-ABDOMINAL AND PELVIC ABSCESSES.
Al-Madena copy
2
The Peritoneum:
The peritoneal membrane is conveniently divided into two parts – the visceral peritoneum surrounding the viscera and the parietal peritoneum lining the other surfaces of the cavity. The peritoneum had a number of functions.Summary box .
Functions of the peritoneum• Pain perception (parietal peritoneum).
• Visceral lubrication.• Fluid and particulate absorption.
• Inflammatory and immune responses.
• Fibrinolytic activity.
Al-Madena copy
3
The parietal portion is richly supplied with nerves and, when irritated, causes severe pain accurately localized to the affected area. The visceral peritoneum, in contrast, is poorly supplied with nerves and its irritation causes vague pain that is usually located to the midline.
The peritoneal cavity is the largest cavity in the body, the surface area of its lining membrane (2m2 in an adult) being nearly equal to that of the skin. The peritoneal membrane is composed of flattened polyhedral cells (mesothelium), one layer thick, resting upon a thin layer of fibroblastic tissue. Beneath the peritoneum, supported by a small amount of areola tissue, lies a network of lymphatic vessels and rich plexuses of capillary blood vessels from which all absorption and exudation must occur. In health, only a few milliliters of peritoneal fluid is found in the peritoneal cavity. The fluid is pale yellow, somewhat viscid and contains lymphocytes and other leucocytes; it lubricates the viscera, allowing easy movement and peristalsis.
Al-Madena copy
4
In the peritonea space, mobile gas-filled structures float upwards, as does free air(‘gas’). In the erect position, when free fluid is present in the peritoneal cavity, pressure is reduced in the upper abdomen compared with the lower abdomen. When air is introduced, it rises, allowing all of the abdominal contents to sink.
During expiration, intra-abdominal pressure is reduced and peritoneal fluid, aided by capillary attraction, travels in an upward direction towards the diaphragm. Experimental evidence shows that particulate matter and bacteria are absorbed within a few minutes into the lymphatic network through a number of ‘pores’ within the diaphragmatic peritoneum. This upward movement of peritoneal fluids is responsible for the occurrence of many subphrenic abscesses.
The peritoneum has the capacity to absorb large volumes of fluid: this ability is used during peritoneal dialysis in the treatment of renal failure. But the peritoneum can also produce an inflammatory exudates when injured.
Al-Madena copy
5
Summary box .
CAUSES OF PERITONIAL INFLAMMATORY EXUDATE..• Bacterial infection, e.g. appendicitis, tuberculosis.
• Chemical injury, e.g. bile peritonitis.• Ischemic injury, e.g. strangulated bowel, vascular occlusion.
• Direct trauma, e.g. operation.
• Allergic reaction, e.g. starch peritonitis.
Al-Madena copy
6
When a visceral perforation occurs, the free fluid that spills into the peritoneal cavity runs downwards, largely directed by the normal peritoneal attachments. For example, spillage from a perforated duodenal ulcer may run down the right parabolic gutter.
When parietal peritoneal defects are created, healing occurs not from the edges but by the development of new mesothelial cells throughout the surface of the defect. In this way, large defects heal as rapidly as small defects.
Al-Madena copy
7
Acute Peritonitis
Most cases of peritonitis are caused by an invasion of the peritoneal cavity by bacteria, so that when the term “peritonitis” is used without qualification, bacterial peritonitis is implied. Bacterial peritonitis is usually polymicrobial, both aerobic and anaerobic organisms being present. The exception is primary peritonitis (“spontaneous” peritonitis), in which a pure infection with streptococcal, pneumococcal or Haemophilus bacteria occurs.
Al-Madena copy
8
Bacteriology
Bacteria from the gastrointestinal tractThe number of bacteria within the lumen of the gastrointestinal tract is normally low until the distal small bowel is reached, whereas high concentrations are found in the colon. However, disease (e.g. obstruction, achlorhydria, diverticulitis) may increase proximal colonization. The biliary and pancreatic tracts are normally free from bacteria, although they may be infected in disease, e.g. gallstones. Peritoneal infection is usually caused by two or more bacterial strains. Gram-negative bacteria contain end toxins (lip polysaccharides) in their cell walls that have multiple toxic effects on the host, primarily by causing the release of tumor necrosis factor (TNF) from host leucocytes. Systemic absorption of end toxin may produce end toxic shock with hypotension and impaired tissue perfusion. Other bacteria such as Clostridium wheelchair produce harmful serotoxins.
Bactericides are commonly found in peritonitis. These Gram-negative, non-sporing organisms, although predominant in the lower intestine, often escape detection because they are strictly anaerobic and slow to growth on culture media unless there is an adequate carbon dioxide tension in the anaerobic apparatus (Gillespie). In many laboratories, the culture is discarded if there is no growth in 48 hours. These organisms are resistant to penicillin and streptomycin but sensitive to metronidazole, clindamycin, lincomycin and cephalosporin compounds. Since the widespread use of metronidazole (Flagyl), Bacteroides infections have greatly diminished.
Al-Madena copy
9
Non- gastrointestinal caused of peritonitis
Pelvic infection via the fallopian tubes is responsible for a high proportion of “non- gastrointestinal” infections.Immunodeficient patients, for example those with human immunodeficiency virus (HIV) infection or those on immunosuppressive treatment, may present with opportunistic peritoneal infection, e.g. Mycobacterium avium – intracellulare (MAI).
Al-Madena copy
10
Mycobacterium avium – intracellulare (MAI)
(Summary box 58.3).Summary box .
Bacteria in peritonitis
1-Gastrointestinal source
• Escherichia coli• Streptococci (aerobic and anaerobic)
• Bacteroides
• Clostridium
• Klebsiella pneumonia
• Staphylococcus
2-Other sources
• Chlamydia• Gonococcus
• β-Haemolytic streptococci
• Pneumococcus
• Mycobacterium tuberculosis
Al-Madena copy
11
Route of infection
Infecting organisms may reach the peritoneal cavity via a number of routes
Summary Box.
Paths to peritoneal infection• Gastrointestinal perforation, e.g. perforated ulcer, diverticular perforation.
• Exogenous contamination, e.g. drains, open surgery, trauma.
• Transmural bacterial translocation (no perforation), e.g. inflammatory bowel disease, appendicitis, ischaemic bowel.
• Female genital tract infection, e.g. pelvic inflammatory disease.
• Haematogenous spread (rare), e.g. septicaemia.
Al-Madena copy
12
Even in patients with non-bacterial peritonitis (e.g. acute pancreatitis, intrapertioneal rupture of the bladder or haemoperitoneum), the peritoneum ofter becomes infected by transmural spread of organisms from the bowel, and it is not long (often a matter of hours) before a bacterial peritonitis develops. Most and many gastric perforations are also sterile at first; intestinal perforations are usually infected from the beginning. The proportion of anaerobic to aerobic organisms increase with passage of time. Mortality reflects:
•the degree and duration of peritoneal contamination;
• the age of the patient• the general health of the patient;
• the nature of the underlying cause.
Al-Madena copy
13
Localised peritonitis
Anatomical, pathological and surgical factors may favour the localization of peritonitis.
Al-Madena copy14
Anatomical
The greater sac of the peritoneum is divided into (1) the subphrenic, spaces (2) the pelvis and (3) the peritoneal cavity proper. The last is divided into a supracolic and an infrasonic compartment by the transverse colon and transverse mescaline, which deters the spread of infection from one to the other. When the supracolic compartment overflows, as is often the case when a peptic ulcer perforates, it does so over the colon into the infrasonic compartment or by way of the right parabolic gutter to the right iliac fosse and hence to the pelvis.Al-Madena copy
15
Pathological
The clinical course is determined in part by the manner in which adhesions form around the affected organ. Inflamed peritoneum loses its glistening appearance and becomes reddened and velvety. Flakes of fibrin appear and cause loops of intestine to become adherent to one another and to the parietals. There is an outpouring of serous inflammatory exudates rich in leucocytes and plasma proteins that soon becomes turbid; if localization occurs, the turbid fluid becomes frank pus. Peristalsis is retarded in affected bowel and this helps to prevent distribution of the infection. The greater momentum, by enveloping and becoming adherent to inflamed structures, often forms a substantial barrier to the spread of infection.Al-Madena copy
16
Surgical
Drains are frequently placed during operation to assist localization (and exit) of intra-abdominal collections: their value is disputed. They may act as conduits for exogenous infection.Al-Madena copy
17
Diffuse peritonitis
A number of factors may favour the development of diffuce peritonitis:
• Speed of peritoneal contamination is a prime factor. If an inflamed appendix . or other hollow viscus perforates before localization has taken place, there is a gush of contents into the peritoneal cavity, which may spread over a large area almost instantaneously. Perforation proximal to an obstruction or from sudden anastomotic separation is associated with severe generalised peritonitis and a high mortality rate.• Stimulation of peristalsis by the ingestion of food or even water hinders localisation. Violent peristalsis occasioned by the administration of a purgative or an enema may cause the widespread distribution of an infection that would otherwise have remained localised.
• The virulence of the infecting organism may be so great as to render the localisation of infection difficult or impossible.
• Young children have a small omentum, which is less effective in localizing infection.
• Disruption of localised collections may occur with injudicious handling, e.g. appendix mass or pericolic abscess.
• Deficient natural resistance (“immune deficiency “) may result from use of drugs (e.g. steroids), disease { e.g. acquired immune deficiency syndrome(ADIS)} or old age.
Al-Madena copy
18
Clinical features
Localised peritonitisLocalised peritonitis is bound up intimately with the causative condition, and the initial symptoms and signs are those of that condition. When the peritoneum becomes inflamed, the temperature, and especially the pulse rate, rise. Abdominal pain increase and usually there is associated vomiting. The most important sign is guarding and rigidity of the abdominal wall over the area of the abdomen that is involved, with a positive ”release” sign (rebound tenderness). If inflammation arises under the diaphragm, shoulder tip (“phernic”) pain may be felt. In cases of pelvic peritonitis arising from an inflamed appendix in the pelvic position or from salpingitis, the abdominal signs are often slight; there may be deep tenderness of one or both lower quadrants alone, but a rectal or vaginal examination reveals marked tenderness of the pelvic peritoneum. With appropriate treatment, localised peritonitis usually resolves; in about 20% of cases, an abscess follows. Infrequently, localised peritonitis becomes diffuse. Conversely, in favourable circumstances, diffuse peritonitis can become localised, most frequently in the pelvis or at multiple sites within the abdominal cavity.
Al-Madena copy
19
Diffuse (generalised) peritonitis
Diffuse (generalised) peritonitis may present in differing ways dependent on the duration of infection.Early
Abdominal pain is severe and made worse by moving or breathing. It is first experienced at the site of the original lesion and spreads outwards from this point. Vomiting may occur. The patient usually lies still. Tenderness and rigidity on palpation are found typically when the peritonitis affects the anterior abdominal wall. Abdominal tenderness and rigidity are diminished or absent if the anterior wall is unaffected, as in pelvic peritonitis or, rarely, peritonitis in the lesser sac. Patients with pelvic peritonitis may complain of urinary symptoms; they are tender on rectal or vaginal examination. Infrequent bowel sounds may still be heard for a few hours but they cease with the onset of paralytic ileus. The pluse rises progressively but, if the peritoneum is deluged with irritant fluid, there is a sudden rise. The temperature changes are variable and can be subnormal.
Al-Madena copy
20
Late
If resolution or localisation of generalised peritonitis does not occur, the abdomen remains silent and increasingly distends.Circulatory failure ensues, with cold, clammy extremities, sunken eyes, dry tongue, thread (irregular) pulse and drawn and anxious face (Hippocratic fancies; The patient finally lapses into unconsciousness. With early diagnosis and adequate treatment, this condition is rarely seen in modern surgical practice.
Al-Madena copy
21Summary box .
Clinical features in peritonitis• Abdominal pain, worse on movement.
• Guarding/rigidity of abdominal wall.
•Pain/tenderness on rectal/ vaginal examination (pelvic peritonitis).
• Pyrexia (may be absent).
• Raised pulse rate.
• Absent or reduced bowel sounds.
• “Septic shock” {systemic inflammatory response syndrome (SIRS) in later stages.
Al-Madena copy
22
Diagnostic aids
Investigations may elucidate a doubtful diagnosis, but the importance of a careful history and repeated examination must not be forgotten.
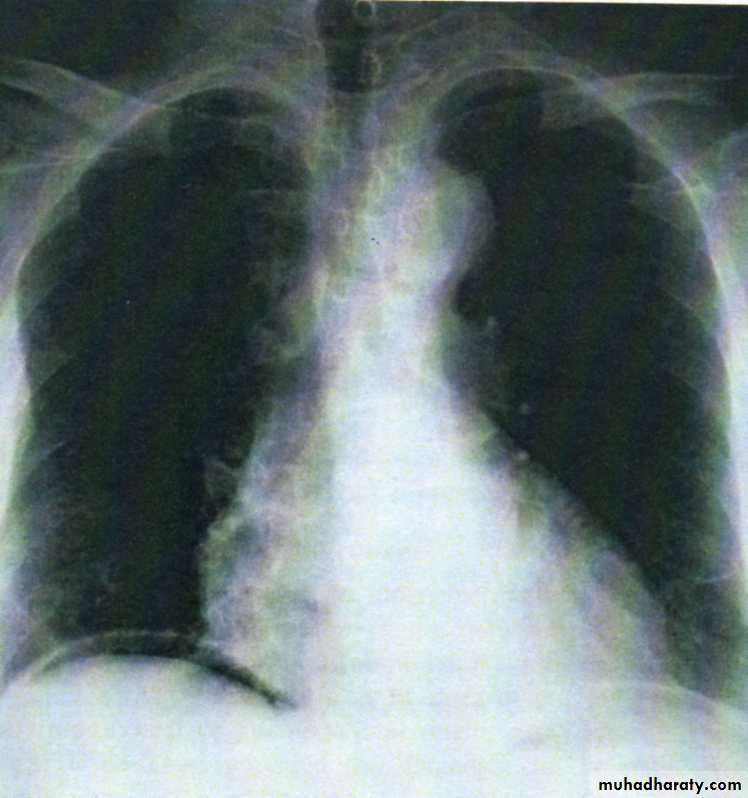
• A radiograph of the abdomen may confirm the presence of dilated gas-filled loops of bowel ( consistent with a paralytic ileus) or show free gas, although the latter is best shown on an erect chest radiograph . If the patient is too ill for an “erect” film to demonstrate free air under the diaphragm, a lateral decubitus film is just as useful, showing gas beneath the abdominal wall.
Al-Madena copy
23• Serum amylase estimation may establish the diagnosis of acute pancreatitis provided that it is remembered that moderately raised values are frequently found following other abdominal catastrophes and operations, e.g. perforated duodenal ulcer.
• Ultrasound and computerized tomography (CT) scanning are increasingly used to identify the cause of peritonitis Such knowledge may influence management decisions
• Peritoneal diagnostic aspiration may be helpful but is usually unnecessary. Bile-stained fluid indicates a perforated peptic ulcer or gall bladder; the presence of pus indicates bacterial peritonitis. Blood is aspirated in a high proportion of patients with intraperitoneal bleeding.
Al-Madena copy
24Summary box.
Investigations in peritonitis• Raised white cell count and C-reactive protein are usual.
• Serum amylase >4x normal indicates acute pancreatitis.
• Abdominal radiographs are occasionally helpful.
• Erect chest radiographs may show free peritoneal gas (perforated viscus).
• Ultrasound/CT scanning often diagnostic.
• Peritoneal fluid aspiration (with or without ultrasound guidance) may be helpful.
Al-Madena copy
25
Treatment
In case of doubt, early surgical intervention is to be preferred to a “wait and see” policy. This rule is particularly true for previously healthy patients and those with postoperative peritonitis. Caution is required in patients at high operative risk because of co morbidity or advanced age.
Treatment consists of:
A- general care of the patient;
B- specific treatment of the cause;
C- peritoneal lavage when appropriate.
Al-Madena copy
26
A-General care of the patient
1-Correction of circulating volume and electrolyte imbalance.Patients are frequently hypovolaemic with electrolyte disturbances. The plasma volume must be restored and electrolyte concentrations corrected. Central venous catheterization and pressure monitoring may be helpful, particularly in patients with concurrent disease. Plasma protein depletion may also need correction as the inflamed peritoneum leaks large amounts of protein. If the patient’s recovery is delayed for more than 7-10 days, intravenous nutrition is required.
2-Gastrointestinal decompression
A nasogastric tube is passed into the stomach and aspirated. Intermittent aspiration is maintained until the parplytic ileus has resolved. Measured volumes of water are allowed by mouth when only small amounts are being aspirated. If the abdomen is soft and not tender, and bowel sounds return, oral feeding may be progressively introduced. It is important not to prolong the ileus by missing this stage.Al-Madena copy
27
3-Antibiotic therapy
Administration of antibiotics prevents the multiplication of bacteria and the release of endotoxins. As the infection is usually a mixed one, initial treatment with parenteral broad-spectrum antibiotics active against aerobic and anaerobic bacteria should be given.
4-Correction of fluid loss
A fluid balance chart must be started so that daily output by gastric aspiration and urine is known. Additional losses from the lungs, skin and in faces are estimated, so that the intake requirements can be calculated and seen to have been administered. Throughout recovery, the haematocrit and serum electrolytes and urea must be checked regularly.
5-Analgesia
The patient should be nursed in the sitting-up position and must be relieved of pain before and after operation. If appropriate expertise is available, epidural infusion may provide excellent analgesia. Freedom from pain allows early mobilization and adequate physiotherapy in the postoperative period, which help to prevent basal pulmonary collapse, deep vein thrombosis and pulmonary embolism.
Al-Madena copy
28
6-Vital system support
Special measures may be needed for cardiac, pulmonary and renal support, especially if septic shock is present.B-Specific treatment of the cause
If the cause of peritonitis is amenable to surgery, operation must be carried out as soon as the patient is fit for anaesthesia. This is usually within a few hours. In peritonitis caused by pancreatitis or salpingitis, or in cases of primary peritonitis of streptococcal or pneumococcal origin, non-operative treatment is preferred provided the diagnosis can be made with confidence.
Al-Madena copy
29
C-Peritoneal lavage
In operations for general peritonitis it is essential that, after the cause has been dealt with, the whole peritoneal cavity is explored with the sucker and, if necessary, mopped dry until all seropurulent exudates is removed. The use of a large volume of saline (1-2 litters) containing dissolved antibiotic (e.g. tetracycline) has been shown to be effective (Matheson) .Summary box.
Management of peritonitis
General care of patient:
• Correction of fluid and electrolyte imbalance.
• Insertion of nasogastric drainage tube.
• Broad – spectrum antibiotic therapy.
• Analgesia.
• Vital system support.
Operative treatment of cause when appropriate with peritoneal debridement/lavage.
Al-Madena copy
30
Prognosis and complications
With modern treatment, diffuse peritonitis carries a mortality rate of about 10%. The systemic and local complications are shown in Summary boxes.Summary boxes .
Systemic complications of peritonitis• Bacteraemic/endotoxic shock.
• Bronchopneumonia/ respiratory failure.• Renal failure.
• Bone marrow suppression .
• Multisystem failure.
Al-Madena copy
31
Summary boxes .
Abdominal complications of peritonitis
• Adhesional small bowel obstruction.
• Paralytic ileus.
• Residual or recurrent abscess.
• Portal pyaemia/liver abscess.
Acute intestinal abstruction due to peritoneal adhesions
The usually gives central colicky abdominal pain with evidence of small bowel gas and fluid levels sometimes confined to the proximal intestine on radiography. Bowel sounds are increased. It is more common with localised peritonitis. It is essential to distinguish this from paralytic ileus.Al-Madena copy
32
Paralytic ileus
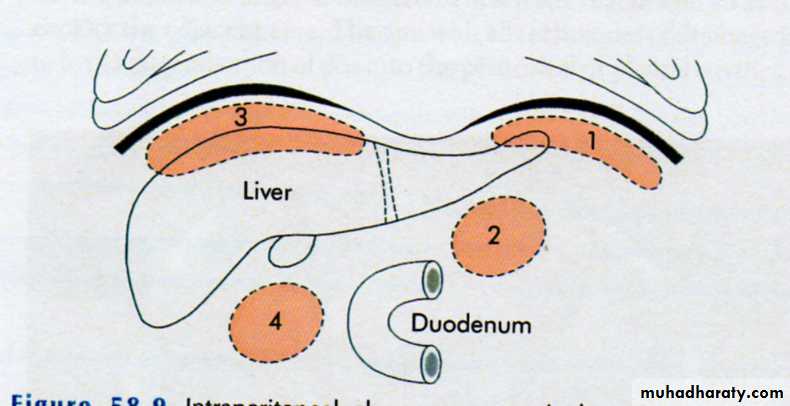
There is usually little pain, and gas-filled loops with fluid levels are seen distributed throughout the small and large intestine on abdominal imaging. In paralytic ileus, bowel sounds are reduced or absent.Abdominal and pelvic abscesses
Abscess formation following local or diffuse peritonitis usually accupies one of the situations shown in The symptoms and signs of a purulent collection may be vague and consist of nothing more than lassitude, anorexia and malaise; pyrexia (often low – grade), tachycardia, leucocytosis, raised C-reactive protein and localised tenderness are also commonAl-Madena copy
33
Summary box .
Clinical features of an abdominal/pelvic abscess• Malaise
• Sweats with or without rigors.• Abdominal/pelvic (with or without shoulders tip) pain.
• Anorexia and weight loss.
• Symptoms from local irritation, e.g. hiccoughs (subphrenic), diarrhea and mucus (pelvic).
• Swinging pyrexia.
• Localised abdominal tenderness/mass.
Later, a palpable mass may develop that should be monitored by marking out its limits on the abdominal wall and meticulous daily examination. More commonly, its course is monitored by repeat ultrasound or CT scanning. In most cases, with the aid of antibiotic treatment, the abscess or mass gradually reduces in size until, finally, it is undetectable. In others, the abscess fails to resolve or becomes larger, in which event it must be drained. In many situations, by waiting for a few days the abscess becomes adherent to the abdominal wall, so that it can be drained without opening the general peritoneal cavity. If facilities are available, ultrasound or CT guided drainage may avoid further operation. Open drainage of an intraperitoneal collection should be carried out by cautious blunt finger exploration to minimize the risk of an intestinal fistula.
Al-Madena copy
34
Pelvic abscess
The pelvis is the commonest site of an intraperitoneal abscess because the vermiform appendix is often pelvic in position and the fallopian tubes are frequent sites of infection. A pelvic abscess can also occur as a sequel to any case of diffuse peritonitis and is common after anastomostic leakage following colorectal surgery. The most characteristic symptoms are diarrhea and the passage of mucus in the stools. Rectal examination reveals a bulging of the anterior rectal wall, which, when the abscess is ripe, becomes softly cystic. Left to nature, a proportion of these abscesses burst into the rectum, after which the patient nearly always recovers rapidly. If this does not occur, the abscess is definitely pointing into the rectum, rectal drainage (Fig. 58.6) is employed. If any uncertainty exists, the presence of pus should be confirmed by ultrasound or CT scanning with needle aspiration if indicated. Laparotomy is almost never necessary. Rectal drainage of a pelvic abscess is far preferable to suprapubic drainage, which risks exposing the general peritoneal cavity to infection. Drainage tubes can also be inserted percutaneously or via the vagina or rectum under ultrasound or CT guidance .Al-Madena copy
35Intraperitoneal abscess
AnatomyThe complicated arrangement of the peritoneum results in the formation of four intraperitoneal spaces in which pus may collect
Left subphrenic space
This is bound above by the diaphragm and behind by the left triangular ligament and the left lobe of the liver, the gastrohepatic omentum and the anterior surface of the stomach. To the right is the falciform ligament and to the left the spleen, gastosplenic omentum and diaphragm. The common cause of an abscess here is an operation on the stomach, the tail of the pancreas, the spleen or the splenic flexure of the colon.Al-Madena copy
36Left subhepatic space/lesser sac
The commonest cause of infection here is complicated acute pancreatitis. In practice, a perforated gastric ulcer rarely causes a collection here because the potential space is obliterated by adhesions.Right subphrenic space
This space lies between the right lobe of the liver and the diaphragm. It is limited posteriorly by the anterior layer of the coronary and the right triangular ligaments and to the left by the falciform ligament. Common causes of abscess here are perforating cholecystitis, a perforated duodenal ulcer, a duodenal cap “blow-out” following gastrectomy and appendicitis.
Right subhepatic space
This lies transversely beneath the right lobe of the liver in Rutherford Morison’s pouch. It is bounded on the right by the right lobe of the liver and the diaphragm. To the left is situated the foramen of Winslow and below this lies the duodenum. In front are the liver and the gall bladder and behind are the upper part of the right kidney and the diaphragm. The space is bounded above by the liver and below by the transverse colon and hepatic flexure. It is the deepest space of the four and the commonest site of a subphrenic abscess, which usually arises from appendicitis, cholecystitis, a perforated duodenal ulcer or following upper abdominal surgery.
Al-Madena copy
37
Clinical features
The symptoms and signs of subphrenic infection are frequently non-specific and it is well to remember the aphorism, “pus somewhere, pus nowhere else, under the diaphragm”.
Symptoms
A common history is that, when some infective focus in the abdominal cavity has been dealt with, the condition of the patient improves temporarily but, after an interval of a few days or weeks, symptoms of toxaemia reappear. The condition of the patient steadily, and often rapidly, deteriorates. Sweating, wasting and anorexia are present. There is sometimes epigastric fullness and pain, or pain in the shoulder on the affected side, because of irritation of sensory fibres in the phrenic nerve, referred along the descending branches of the cervical plexus. Persistent hiccoughs may be a presenting symptom.Al-Madena copy
38
Signs
A swinging pyrexia is usually present. If the abscess is anterior, abdominal examination will reveal some tenderness, rigidity or even a palpable swelling. Sometimes the liver is displaced downwards but more often it is fixed by adhesions. Examination of the chest is important and, in the majority of cases, collapse of the lung or evidence of basal effusion or even an empyema is found.Investigations
A number of the following investigations may be helpful:• Blood tests usually show a leucocytosis and raised C-reactive protein.
• A plain radiograph sometimes demonstrates the presence of gas or a pleural effusion. On screening, the diaphragm is often seen to be elevated (so called “tented” diaphragm) and its movements impaired.
• Ultrasound or CT scanning is the investingation of choice and permits early detection of subphrenic collections
• Radiolabelled white cell scanning may occasionally prove helpful when other imaging techniques have failed.
Al-Madena copy
39Differential diagnosis
Pyelonephritis, amoebic abscess, pulmonary collapse and pleural empyema may give rise to diagnostic difficulty.
Treatment
The clinical course of suspected case is monitored, and blood tests and imaging investigations are carried out at suitable intervals. If suppuration seems probable, intervention is indicated. If skilled help is available it is usually possible to insert a percutaneous drainage tube under ultrasound or CT control. The same tube can be used to instill antibiotic solutions or irrigate the abscess cavity. To pass an aspirating needle at the bedside through the pleura and diaphragm invites potentially catastrophic spread of the infection into the pleural cavity.If an operative approach is necessary and a swelling can be detected in the subcostal region or in the loin, an incision is made over the site of masimum tenderness or over any area where oedema or reness is discovered. The parietes usually form part of the abscess wall so that contamination of the general peritoneal cavity is unlikely.
If no swelling is apparent, the subphrenic spaces should be explored by either an anterior subcostal approach or from behind after removal of the outer part of the 12th rib according to the position of the abscess on imaging. When the posterior approach, the pleura must not be opened and, after the fibers of the diaphragm have been separated, a finger is inserted beneath the diaphragm so as to explore the adjacent area. The aim with all techniques of drainage is to avoid dissemination of pus into the peritoneal or pleural cavities.
When the cavity is reached, all of the fibrinous loculi must be broken down with the finger and one or two drainage tubes must be fully inserted. These drains are withdrawn gradually during the next 10 days and the closure of the cavity is checked by sonograms or scanning. Appropriate antibiotics are also given.
Al-Madena copy
40
Special forms of peritonitis
PostoperativeThe patient is ill with raised pulse and peripheral circulatory failure. Following an anastigmatic dehiscence, the general condition of a patient is usually more serious than if the patient had suffered leakage from a perforated peptic ulcer with no preceding operation. Local symptoms and signs are less definite. Abdominal pain may not be prominent and is often difficult to assess because of normal wound pain and postoperative analgesia. The patient’s deterioration may be attributed wrongly to cardiopulmonary collapse, which is usually concomitant.
Peritonitis follows abdominal operations more frequently than is realized. The principles of treatment do not differ from those of peritonitis of other origin. Antibiotic therapy alone is inadequate; no antibiotic can stay the onslaught of bacterial peritonitis caused by leakage from a suture line, which must be dealt with by operation.
In patients on treatment with steroids
Pain is frequently slight or absent. Physical signs similarly vague and misleading.Al-Madena copy
41
In children
The diagnosis can be more diffuclt, particularly in the preschool child. Physical signs should be elicited by a gentle, patient and sympathetic approach.
In patients with dementia
Such patients can be fractious and unable to give a reliable history. Abdominal tenderness is usually well localised, but guarding and rigidity are less marked because the abdominal muscles are often thin and weak.
Bile peritonitis
Unless there is reason to suspect that the biliary tract was damaged during operation, it is improbable that bile as a cause of peritonitis will be thought of until the abdomen has been opened. The common causes of bile peritonitis are shown in Summary box.Al-Madena copy
42
Summary box .
Causes of bile peritonitis• Perforated cholecysitits.
• Post cholecystectomy:Cystic duct stump leakage
Leakage from an accessory duct in the gall bladder bed Bile duct injury
T-tube drain dislodgement (or tract rupture on removal)
• Following other operations/ procedures:
Leaking duodenal stump post gastrectomy
Leaking biliary – enteric anastomosis
Leakage around percutaneous placed biliary drains
• Following liver trauma
Al-Madena copy
43
Unless the bile has extravasated slowly and the collection becomes shut off from the general peritoneal cavity, there are signs of diffuse peritonitis. After a few hours a tinge of jaundice is not unusual. Laparotomy (or laparoscopy) should be undertaken with evacuation of the bile and peritoneal lavage. The source of bile leakage should be identified. A leaking gall bladder is excised or a cystic duct ligated. An injury to the bile duct may simply be drained or alternatively intubated; later, reconstructive operation is often required. Infected bile is more lethal than sterile bile. A “blown” duodenal stump should be drained as it is too oedematous to repair, but sometimes it can be covered by a jejunal patch. The patient is often jaundiced from absorption of peritoneal bile, but the surgeon must ensure that the abdomen is not closed until any obstruction to a major bile duct has been either excluded or relieved. Bile leaks after cholecystectomy or liver trauma may be dealt with by percutaneous (ultrasound – guided) drainage and endoscopic biliary stenting to reduce bile duct pressure. The drain is removed when dry and the stent at 4-6 weeks.
Al-Madena copy
44
Meconium peritonitis
Pneumococcal peritonitisPrimary pneumococcal peritonitis may complicate nephritic syndrome or cirrhosis in children. Otherwise healthy children, particularly girls between 3 and 9 years of age, may also be affected, and it is likely that the route of infection is sometimes via the vagina and fallopian tubes. At other times, and always in males, the infection is blood-borne and secondary to respiratory tract or middle ear disease. The prevalence of pneumococcal peritonitis has declined greatly and the condition is now rare.
Clinical features
The onset is sudden and the earliest symptom is pain localised to the lower half of the abdomen. The temperature is raised to 39 0 C or more and there is usually frequent vomiting. After 24-48 hours, profuse diarrhoea is characteristic. There is usually increased frequency of micturition. The last two symptoms are caused by severe pelvic peritonitis. On examination, abdominal rigidity is usually bilateral but is less than in most cases of acute appendicitis with peritonitis.
Al-Madena copy
45
Differential diagnosis
A leucocytosis of 30 000µ 1-1 (30 X 109 1-1) or more with approximately 90% polymorphs suggests pneumococcal peritonitis rather than appendicitis. Even so, it is often impossible to exclude perforated appendicitis. The other condition that can be difficult to differentiate from primary pneumococcal peritonitis in its early stage is basal pneumonia. An unduly high respiratory rate and the absence of abdominal rigidity are the most important signs supporting the diagnosis of pneumonia, which is usually confirmed by a chest radiograph.Al-Madena copy
46
Treatment
After starting antibiotic therapy and correcting dehydration and electrolyte imbalance, early surgery is required unless spontaneous infection of pre-existing ascites is strongly suspected, in which case a diagnostic peritoneal tap is useful. Laparotomy or laparoscopy may be used. Should the exudates be odourless and sticky, the diagnosis of pneumococcal peritonitis practically certain, but it is essential to careful exploration to exclude other pathology. Assuming that no other cause for the peritonitis is discovered, some of the exudates is aspirated and sent to the laboratory for microscopy, culture and sensitivity tests. Thorough peritoneal lavage is carried out and the incision closed. Antibiotic and fluid replacement therapy are continued. Nasogastric suction drainage is essential. Recovery is usual.Other organisms are known to cause some cases of primary pneumococcal peritonitis, the peritoneal in children, including Haemophilus, other streptococci and a few Gram – negative bacteria. Underlying pathology ( including an intravaginal foreign body in girls) must always be excluded before primary peritonitis can be diagnosed with certainty.
Al-Madena copy
47
Idiopathic streptococcal and staphylococcal peritonitis in adults
Idiopathic streptococcal and staphylococcal peritonitis in adults is fortunately rare. In streptococcal peritonitis, the peritoneal exudates is odourless and thin, contains some flecks of fibrin and may be blood- stained. In these circumstances pus is removed by suction, the abdomen closed with drainage and non-operative treatment of peritonitis performed. The use of intravaginal tampons has led to an increased incidence of Staphylococcus aureus infections: these can be associated with “toxic shock syndrome” and disseminated intravascular coagulopathy.
Al-Madena copy
48
Familial Mediterranean Fever (periodic peritonitis)
Familial Mediterranean fever (periodic peritonitis) is characterized by abdominal pain and tenderness, mild pyrexia, polymorphonuclear leucocytosis and, occasionally, pain in the thorax and joints. The duration of an attack is 24-72 hours, when it is followed by complete remission, but exacerbations recur at regular intervals. Most of the patients have undergone appendicectomy in childhood. This disease, often familial, is limited principally to Arab. Armenian and Jewish populations; other races are occasionally affected. Mutations in the MEFV (Mediterranean fever) gene appear to cause the disease. This gene produces a protein called pyrin, which is expressed mostly in neutrophils but whose exact function is not known.Usually, children are affected but it is not rare for the disease to make its first appearance in early adult life, with cases in women outnumbering those in men by two one. Exceptionally the disease becomes manifest in patients over 40 years of age. At operation, which may be necessary to exclude other cases but should be avoided if possible, the peritoneum – particularly in the vicinity of the spleen the gall bladder- is inflamed. There is no evidence that the interior of these organs is abnormal. Colchincine therapy is used during attacks and to prevent recurrent attacks.
Al-Madena copy
49
Starch peritonitis
Like talc, starch powder has found disfavor as a surgical glove lubricant. In a few starch-sensitiveAl-Madena copy
50
Tuberculous Peritonitis
Acute tuberculous peritonitisTuberculous peritonitis sometimes has an onset that so closely resembles acute peritonitis that the abdomen is opened. Straw-coloured fluid escapes and tubercles are seen scattered over the peritoneum and greater omentum. Early tubercles are grayish and translucent. They soon undergo caseation and appear white or yellow and are then less difficult to distinguish from carcinoma. Occasionally, they appear like patchy fat necrosis. On opening the abdomen and finding tuberculous peritonitis, the fluid is evacuated, some being retained for bacteriological studies. A portion of the diseased omentum is removed for histological confirmation of the diagnosis and the wound closed without drainage.
Chronic tuberculous peritonitis
The condition presents with abdominal pain (90% of cases), fever (60%), loss of weight (60%), ascites (60%), night sweats (37%) and abdominal mass (26%) (Summary box).
Al-Madena copy
51
Summary box .
Tuberculous peritonitis
• Acute and chronic forms.• Abdominal pain, sweats, malaise and weight loss are frequent.
• Caseating peritoneal nodules are common – distinguish from metastatic carcinoma and fat necrosis of pancreatitis.
• Ascites common, may be loculated.
• Intestinal obstruction may respond to anti-tuberculous treatment without surgery.
Al-Madena copy
52
Origin of the infection
Infection originates from:• tuberculous mesenteric lymph nodes;
• tuberculosis of the ileocaecal region;• a tuberculous pyosalpinx;
•blood-borne infection from pulmonary tuberculosis, usually the “military” but occasionally the “cavitating” form.
Al-Madena copy
53
Al-Madena copy
54Al-Madena copy
55Al-Madena copy
56Al-Madena copy
57