TUBERCULOSIS
Dr.Redha 2013Epidemiology
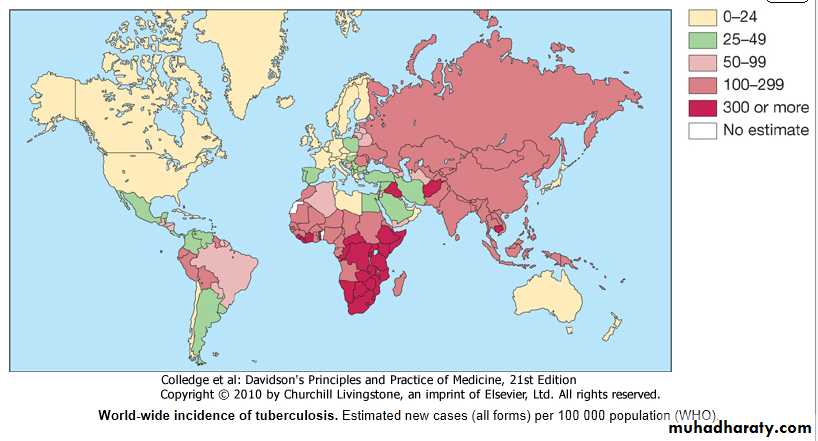
• Tuberculosis (TB) is caused by infection with Mycobacterium tuberculosis (MTB), which is part of a complex of organisms including M. bovis (reservoir cattle) and M. africanum (reservoir human).• The impact of TB on world health is significant; in 2006, there were an estimated 9.2 million new cases, 14.4 million prevalent cases and 1.5 million deaths attributable to TB.
• It is estimated that around one-third of the world's population has latent TB.
• The majority of cases occur in the world's poorest nations, who struggle to cover the costs associated with management and control programmes (Fig. next).
• The resurgence نهوضof TB has been largely driven in Africa by HIV disease, and in the former Soviet Union and Baltic states by lack of appropriate health care exacerbated by social and political upheavalثورات.
Pathology and pathogenesis
• M. bovis infection arises from drinking non- sterilized milk from infected cows.• M. tuberculosis is spread by the inhalation of aerosolized droplet nuclei from other infected patients.
• Once inhaled, the organisms lodge in the alveoli and initiate the recruitment of macrophages and lymphocytes.
• Macrophages undergo transformation into epithelioid and Langhans cells which aggregate with the lymphocytes to form the classical tuberculous granuloma (Fig.).
• Numerous granulomas aggregate to form a primary lesion or 'Ghon focus' (a pale yellow, caseous nodule, usually a few mm to 1-2 cm in diameter), which is characteristically situated in the periphery of the lung.
• Spread of organisms to the hilar lymph nodes is followed by a similar pathological reaction; the combination of a primary lesion and regional lymph nodes is referred to as the 'primary complex of Ranke'.
• Reparative processes encase the primary complex in a fibrous capsule limiting the spread of bacilli: so-called latent TB. If no further complications ensue, this lesion eventually calcifies and is clearly seen on a chest X-ray.
• However, lymphatic or haematogenous spread may occur before immunity is established, seeding secondary foci in other organs including lymph nodes, serous membranes, meninges, bones, liver, kidneys and lungs, which may lie dormant for years.
• The only clue that infection has occurred may be the appearance of a cell-mediated, delayed-type hypersensitivity reaction to tuberculin, demonstrated by tuberculin skin testing.
• If these reparative processes fail, primary progressive disease ensues .
• The estimated lifetime risk of developing disease after primary infection is 10%, with roughly half of this risk occurring in the first 2 years after infection.
Factors increasing the risk of TB
i-Patient-related• Age (children > young adults < elderly)
• First-generation immigrants from high-prevalence
• countries
• Close contacts of patients with smear-positive pulmonary TB
• Overcrowding (prisons, collective dormitories); homelessness (doss houses and hostels)
• Chest radiographic evidence of self-healed TB
• Primary infection < 1 year previously
• Smoking
.
ii- Associated diseases
• Immunosuppression: HIV, anti-TNF therapy, high-dose
corticosteroids, cytotoxic agents
• Malignancy (especially lymphoma and leukemia)
• Type 1 diabetes mellitus
• Chronic renal failure
• Silicosis
• Gastrointestinal disease associated with malnutrition .
• Deficiency of vitamin D or A
• Recent measles: increases risk of child contracting TB
Timetable of TB
Time from infectionManifestations
3-8 weeks
Primary complex, positive tuberculin skin test
3-6 months
Meningeal, miliary and pleural disease
Up to 3 years
Gastrointestinal, bone and joint, and lymph node disease
Around 8 years
Renal tract disease
From 3 years onwards
Post-primary disease due to reactivation or reinfection
Clinical features: pulmonary disease
Primary pulmonary TB
• Primary TB refers to the infection of a previously uninfected (tuberculin-negative) individual.
• A few patients develop a self-limiting febrile illness but clinical disease only occurs if there is a hypersensitivity reaction or progressive infection.
• Progressive primary disease may appear during the course of the initial illness or after a latent period of weeks or months.
Features of primary TB
Infection (4-8 weeks)• Influenza-like illness
• Skin test conversion
• Primary complex
Disease
• Lymphadenopathy: hilar (often unilateral), paratracheal or mediastinal
• Collapse (especially right middle lobe)
• Consolidation (especially right middle lobe)
• Obstructive emphysema
• Cavitation (rare)
• Pleural effusion
• Endobronchial
• Miliary
• Meningitis
• Pericarditis
Hypersensitivity
• Erythema nodosum
• Phlyctenular conjunctivitis
• Dactylitis
Miliary TB
• Blood-borne dissemination.
• May present acutely .
• More frequently is characterized by 2-3 weeks of fever, night sweats, anorexia, weight loss and a dry cough.
• Hepatosplenomegaly may develop and the presence of a headache may indicate coexistent tuberculous meningitis.
• Auscultation of the chest is frequently normal, although with more advanced disease widespread crackles are evident.
…. Miliary TB
• Fundoscopy may show choroidal tubercles.• The classical appearances on chest X-ray are of fine 1-2 mm lesions ('millet seed') distributed throughout the lung fields, although occasionally the appearances are coarser.
• Anaemia and leucopenia reflect bone marrow involvement.
• 'Cryptic' miliary TB is an unusual presentation sometimes seen in old age (Box next).
Cryptic TB
• Age over 60 years• Intermittent low-grade pyrexia of unknown origin
• Unexplained weight loss, general debility (hepatosplenomegaly
in 25-50%)
• Normal chest X-ray
• Blood dyscrasias; leukaemoid reaction, pancytopenia
• Negative tuberculin skin test
• Confirmation by biopsy (granulomas and/or acid-fast bacilli
demonstrated) of liver or bone marrow
Post-primary pulmonary TB
• Post-primary disease refers to exogenous ('new' infection) or endogenous (reactivation of a dormant primary lesion) infection in a person who has been sensitized by earlier exposure.
• It is most frequently pulmonary and characteristically occurs in the apex of an upper lobe ?? where the oxygen tension favours survival of the strictly aerobic organism.
• The onset is usually insidious, developing slowly over several weeks.
• Systemic symptoms include fever, night sweats, malaise, and loss of appetite and weight, and are accompanied by progressive pulmonary symptoms (Box next).
Clinical presentations of postprimary pulmonary TB
• Chronic cough, often with hemoptysis• Pyrexia of unknown origin
• Unresolved pneumonia
• Exudative pleural effusion
• Asymptomatic (diagnosis on chest X-ray)
• Weight loss, general debility
• Spontaneous pneumothorax.
• Very occasionally, this form of TB may present with one of the complications listed next.
• \
Chronic complications of pulmonary TB
i - Pulmonary
• Massive haemoptysis
• Cor pulmonale
• Fibrosis/emphysema
• Atypical mycobacterial infection
• Aspergilloma
• Lung/pleural calcification
• Obstructive airways disease
• Bronchiectasis
• Bronchopleural fistula
• \
Chronic complications of pulmonary TB
ii - Non-pulmonary
• Empyema necessitans
• Laryngitis
• Enteritis*
• Anorectal disease*
• Amyloidosis
• Poncet's polyarthritis
• Radiological changes include ill-defined opacification in one or both of the upper lobes, and as progression occurs, consolidation, collapse and cavitation develop to varying degrees (Fig).
• It is often difficult to distinguish active from quiescent disease on radiological criteria alone, but the presence of a miliary pattern or cavitation favours active disease.
• In extensive disease, collapse may be marked and result in significant displacement of the trachea and mediastinum.
• Occasionally, a caseous lymph node may drain into an adjoining bronchus resulting in tuberculous pneumonia.
Clinical features: extrapulmonary disease
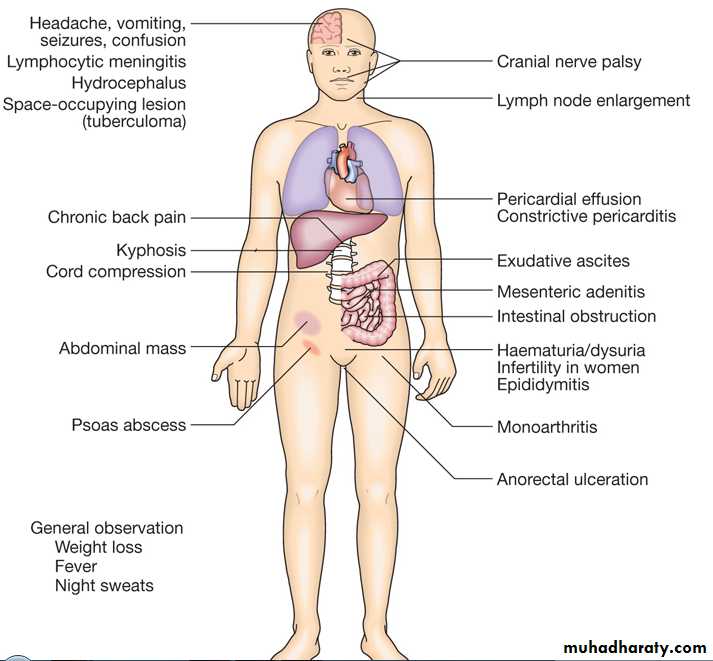
• Extrapulmonary tuberculosis (Fig. next) accounts for about 20% of cases in those who are HIV-negative but is more prevalent in HIV-positive individuals.
Lymphadenitis
• Lymph nodes are the most common extrapulmonary site of disease.
• Cervical and mediastinal glands are affected most frequently, followed by axillary and inguinal; more than one region may be involved.
• Disease may represent primary infection, spread from contiguous sites or reactivation.
• Supraclavicular lymphadenopathy is often the result of spread from mediastinal disease.
…..Lymphadenitis
• The nodes are usually painless and initially mobile but become matted together with time.• When caseation and liquefaction occur, the swelling becomes fluctuant and may discharge through the skin with the formation of a 'collar-stud' abscess and sinus formation.
• Approximately half of cases fail to show any constitutional features such as fevers or night sweats. The tuberculin test is usually strongly positive.
• During or after treatment, paradoxical enlargement, development of new nodes and suppuration may all occur but without evidence of continued infection; rarely, surgical excision is necessary.
Gastrointestinal disease
• TB can affect any part of the bowel and patients may present with a wide range of symptoms and signs (see Fig. above).• Upper gastrointestinal tract involvement is rare and is usually an unexpected histological finding in an endoscopic or laparotomy specimen.
• Ileocaecal disease accounts for approximately half of abdominal TB cases.
• Fever, night sweats, anorexia and weight loss are usually prominent and a right iliac fossa mass may be palpable.
• Up to 30% of cases present with an acute abdomen.
• Ultrasound or CT may reveal thickened bowel wall, abdominal lymphadenopathy, mesenteric thickening or ascites.
……Gastrointestinal disease
• Barium enema and small bowel enema reveal narrowing, shortening and distortion of the bowel with caecal involvement predominating.
• Diagnosis rests on obtaining histology by either colonoscopy or mini-laparotomy.
• The main differential diagnosis is Crohn's disease .
• Tuberculous peritonitis is characterised by abdominal distension, pain and constitutional symptoms.
• The ascitic fluid is exudative and cellular with a predominance of lymphocytes.
• Laparoscopy reveals multiple white 'tubercles' over the peritoneal and omental surfaces.
• Low-grade hepatic dysfunction is common in miliary disease when biopsy reveals granulomas.
• Occasionally, patients may be frankly icteric with a mixed hepatic/cholestatic picture.
Pericardial disease
• Disease occurs in two forms: pericardial effusion and constrictive pericarditis.• Fever and night sweats are rarely prominent and the presentation is usually insidious with breathlessness and abdominal swelling.
• Coexistent pulmonary disease is very rare, with the exception of pleural effusion.
• Pulsus paradoxus, a raised JVP, hepatomegaly, prominent ascites and peripheral oedema are common to both types.
• Pericardial effusion is associated with increased pericardial dullness and a globular enlarged heart on chest X-ray.
……Pericardial disease
• Constriction is associated with a raised JVP, an early third heart sound and, occasionally, atrial fibrillation; pericardial calcification occurs in around 25% of cases.• Diagnosis is on clinical, radiological and echocardiographic grounds .
• The effusion is frequently blood-stained.
• Open pericardial biopsy can be performed where there is diagnostic uncertainty.
• The addition of corticosteroids to antituberculosis treatment has been shown to be beneficial for both forms of pericardial disease.
Central nervous system disease
• Meningeal disease represents the most important form of central nervous system TB (see Fig. above).
• Unrecognized and untreated, it is rapidly fatal.
• Even when appropriate treatment is prescribed, mortality rates of 30% have been reported and survivors may be left with neurological sequelae.
Bone and joint disease
• The spine is the most common site for bony TB (Pott's disease), which usually presents with chronic back pain and typically involves the lower thoracic and lumbar spine (see Fig. above).
• The infection starts as a discitis and then spreads along the spinal ligaments to involve the adjacent anterior vertebral bodies, causing angulation of the vertebrae with subsequent kyphosis.
• Paravertebral and psoas abscess formation is common and the disease may present with a large (cold) abscess in the inguinal region.
• CT and/or MRI are valuable in gauging the extent of disease, the amount of cord compression, and the site for needle biopsy or open exploration if required.
• The major differential diagnosis is malignancy, which tends to affect the vertebral body and leave the disc intact. Important complications include spinal instability or cord compression.
• TB can affect any joint, but most frequently involves the hip or knee.
• Presentation is usually insidious with pain and swelling; fever and night sweats are uncommon.
• Radiological changes are often non-specific, but as disease progresses, reduction in joint space and erosions appear.
• Poncet's arthropathy refers to an immunologically mediated polyarthritis that usually resolves within 2 months of starting treatment.
Genitourinary disease
• Fever and night sweats are rare with renal tract TB and patients are often only mildly symptomatic for many years.• Haematuria, frequency and dysuria are often present, with sterile pyuria found on urine microscopy and culture.
• In women, infertility from endometritis, or pelvic pain and swelling from salpingitis or a tubo-ovarian abscess occur occasionally.
• In men, genitourinary TB may present as epididymitis or prostatitis.