Diseases of Salivary Glands
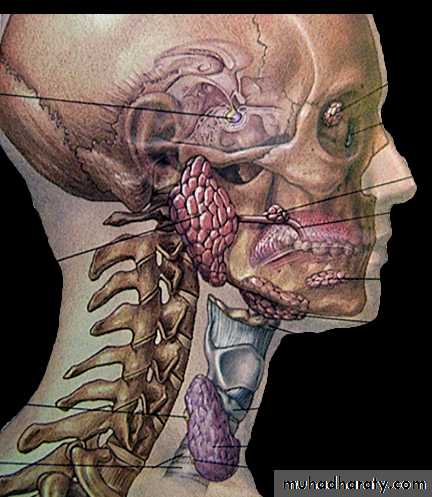
Dr Maitham H. KenberParotid
glandSubmandibular
glandSublingual
glandSalivary Glands Overview
• Major salivary glands
• a. Parotid gland• b. Submandibular gland
• c. Sublingual gland
• 2. Minor salivary glands
• 600 – 1,000 minor salivary gland distributed throughout the mucosa of the upper aerodigestive tract (more common in the soft and hard palate).
•
Salivary glands
Minor glands
Minor salivary glands are not found within gingiva and anterior part of the hard palate
Major salivary glands
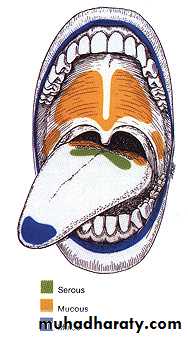
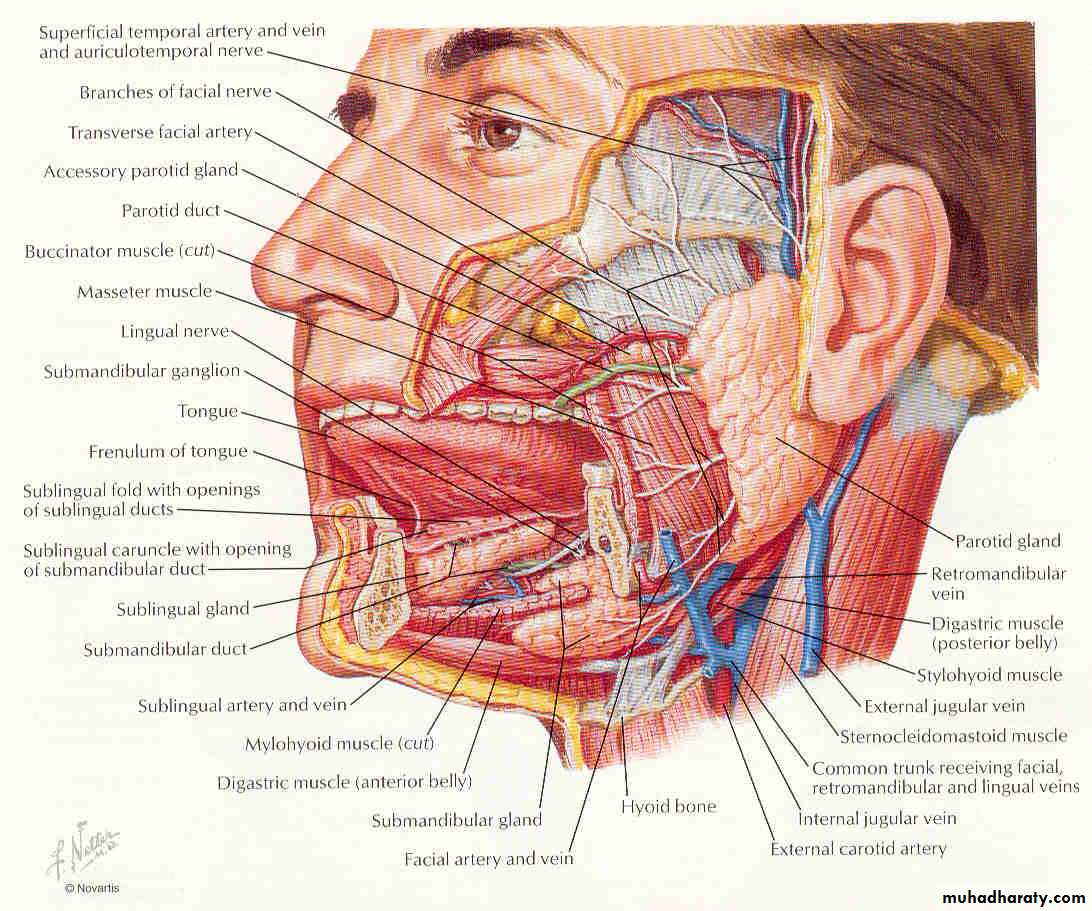
Parotid: watery serous saliva rich in amylase, proline-rich proteinsStenson’s duct
Submandibular gland: more mucinous
Wharton’s duct
Sublingual: viscous saliva
ducts of Rivinus;
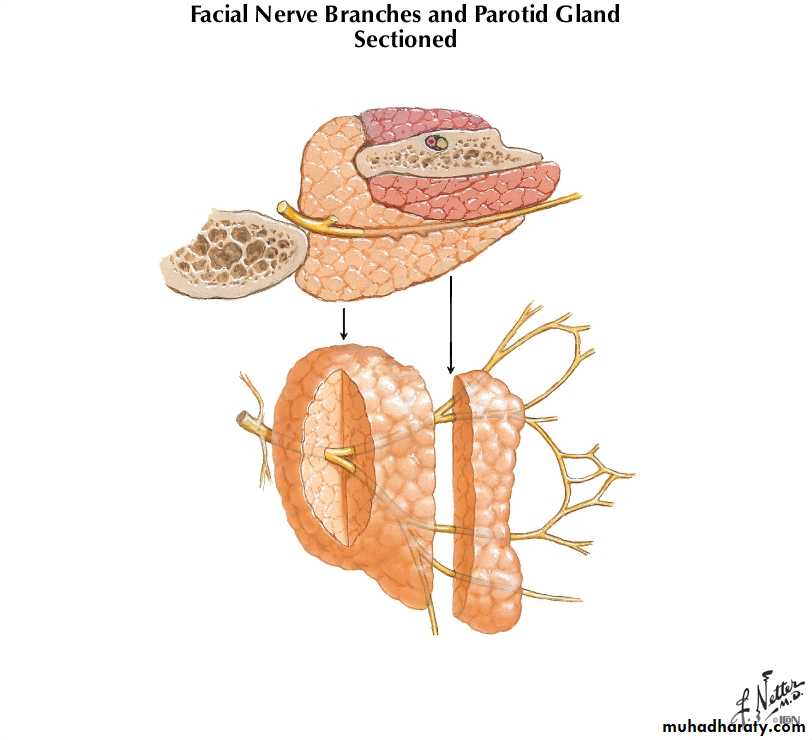
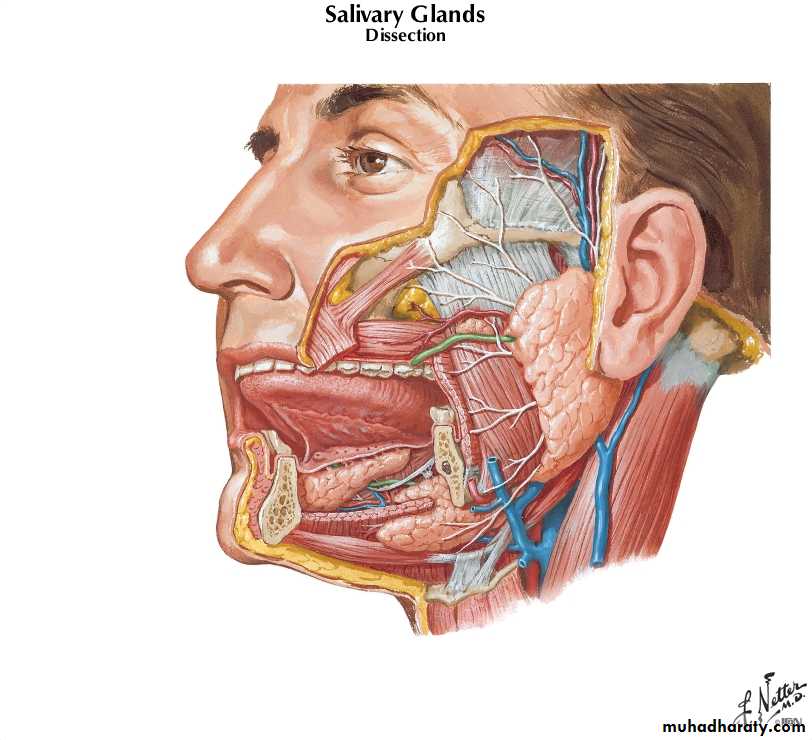
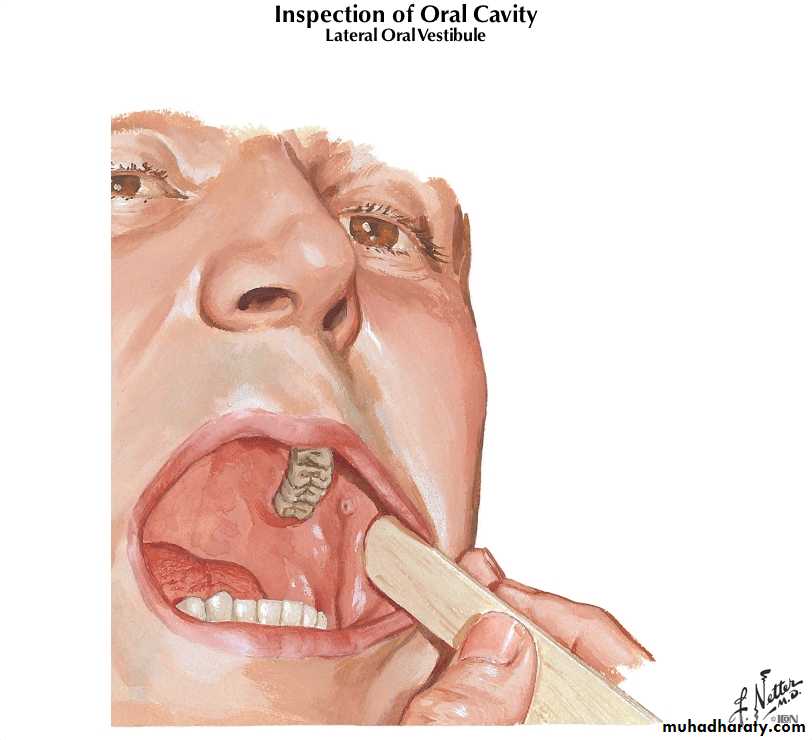
Parotid gland
Located in the preauricular region and along the posterior surface of the mandible .Parotid gland is divided by the facial nerve into :
* superficial lobe overlying the lateral surface of the masseter
* deep lobe between the mastoid process of the temporal bone and the ramus of the mandible
Parotid duct
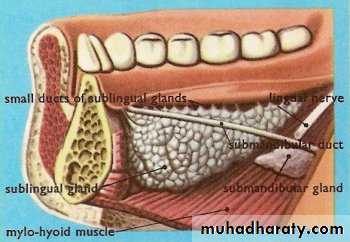
Submandibular gland
Lies in digastric (submandibular) triangleDevided by mylohyoid muscle into
1.superficial lobe
2.deep lobe
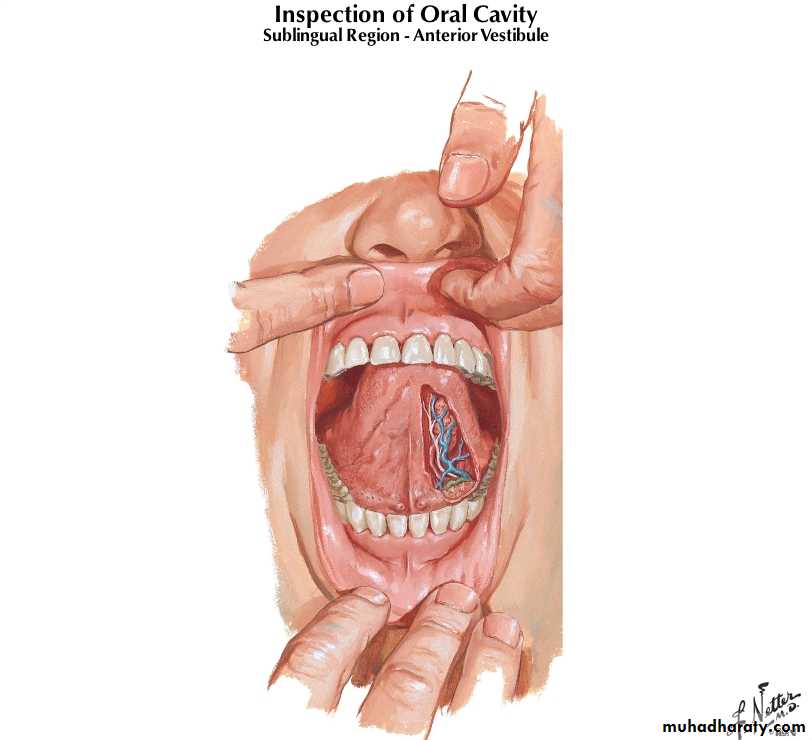
Duct of submandibular (Wharton’s duct) from deep lobe pass between hyoglossus and mylohyoid m. to open at sublingual caruncle in the floor of the mouth lateral frenulum of the tongue
Sublingual gland
Sublingual caruncle
Sublingual Salivary glands
Smallest of the major salivary glands.Almond shape
Deep to the floor
of mouth mucosa.
It is drained by approximately
10 small ducts (Ducts of Rivinus)
Functions
Protectionlubricant (glycoprotein)
barrier against noxious stimuli; microbial toxins and minor traumas
washing non-adherent and acellular debris
formation of salivary pellicle
calcium-binding proteins: tooth protection; plaque
Functions cont’d
Buffering (phosphate ions and bicarbonate)
bacteria require specific pH conditions
plaque microorganisms produce acids from sugars
Functions cont’d
Digestionneutralizes esophageal contents
dilutes gastric chyme
forms food bolus
brakes starch
Functions cont’d
Antimicrobiallysozyme hydrolyzes cell walls of some bacteria
lactoferrin binds free iron and deprives bacteria of this essential element
IgA agglutinates microorganisms
Functions cont’d
Maintenance of tooth integritycalcium and phosphate ions
ionic exchange with tooth surface
Functions cont’d
Tissue repair
bleeding time of oral tissues shorter than other tissues
resulting clot less solid than normal
remineralization
Functions cont’d
Tastesolubilizing of food substances that can be sensed by receptors
trophic effect on receptors
Salivary Gland Diseases
Functional disordersObstructive disorders
Infectious disordersNeoplastic disorders
Functional Disorders of the Salivary Glands
Functional Disorders of the Salivary Glands cont’dSialorrhea (Increased flow of saliva)
(i) Psychosis
(ii) mental retardation(iii) certain neurological diseases
(iv) rabies
( v) mercery poisoning
Functional Disorders of the Salivary Glands cont’d
• Xerostomia (Dry mouth)• ↓ flow of saliva
• Mumps,
• Sarcoidosis
• Sjoegrens syndrome
• Lupus
• post-irradiation treatment
Functional Disorders of the Salivary cont’d Glands (Sjogren’s Syndrome)
Triad of dry eyes, dry mouth, dry joints
Autoimmune disorderLymphocytic infiltration of the salivary glands.
Functional Disorders of the Salivary Glands cont’dMucocele
Secondary to trauma
70% occur in lower lip
Excisional biopsy usually curative
Functional Disorders of the Salivary Glands cont’d
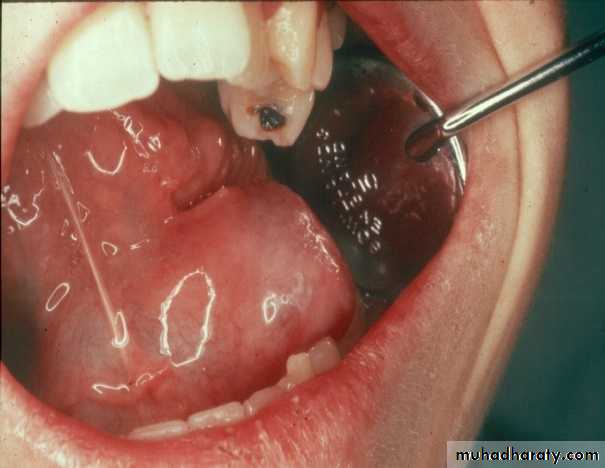
RanulaSublingual salivary gland mucocele
Treatment should include removal of Sublingual gland
Obstructive Disorders of the Salivary Glands
Obstructive Disorders of the Salivary GlandsObstruction to the flow of saliva via the salivary duct can occur due to the presence of salivary gland stone (Sialolith).
Obstruction can also secondary to the stricture (Narrowing) of the salivary gland duct.
Obstructive Disorders of the Salivary Glands cont’d
Sialolithiasis (Salivary gland stone)93% occur in submandibular gland
7% in parotid gland
Multiple occurrence in same gland is common
Sialolithiasis (calculi) cont’d
Associated with Chronic sialoadenitis
Male > female , 50-80 years of age
submandibular gland affected far more common than parotid gland
Composed of Calcium , phosphate and carbonate , combined with other salts (Mg,Zn,NH3) and organic material
Factor predisposing to calculi in SMSG
Submandibular saliva1.high mucin content
2.alkaline pH
3.high phosphate & calcium
Sialolithiasis (calculi) cont’d
Sialolithiasis (calculi) cont’d
Factor predisposing to calculi in SMSG cont’dAnatomy
1.length and irregular course of Wharton’s duct
2.position of ductal orifice
3.size of orifice smaller than duct lumen
• Symptoms
• colicky postprandial pain and swelling• Local swelling & tenderness at ductal opening if the stone is superficial
• Secondary infection – predispose to duct stricture
Sialolithiasis (calculi) cont’d
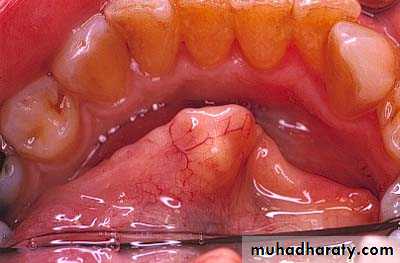
Submandibular Gland - Sialolithiasis
Diagnosis
Pain and sudden enlargement of gland while eating
Palpation of stone in the submandibular duct
Occlusal radiograph (80%)
Sialogram
Submandibular Gland - Sialolithiasis
Submandibular Gland – Sialolithiasis cont’dTreatment
Stone can be removed transorally if in the duct and easily palpable
Submandibular Gland – Sialolithiasis cont’d
TreatmentIf the stone is inside the gland and therefore damaging the gland, then the whole gland should be removed under G.A.
Parotid Gland - Sialolithiasis
DiagnosisBased on history
Swelling during meals
Bimanual palpation of painful gland
40% non-radiopaque
Most parotid stones are multiple
Sialogram
Parotid Gland - Sialolithiasis
Treatment
Stones in extraglandular portion of duct can be removed transorally
Intraglandular stones removed from extraoral
approach by Superficial Parotidectomy.
Sialogram
A sialogram is a dye investigation of a salivary gland. It is carried out to look in detail at the larger salivary glands, namely the parotid or submandibular glands.
Infectious Disorders of the Salivary Glands
Acute Sialadenitis - InfectiousEtiology
Viral - ( Mumps)
Bacterial
Viral- Acute Sialadenitis (Mumps)
Acute painful parotitisViral in etiology
Self limitingMumps
ComplicationsOrchitis/oophritis
Meningitis / encephalitis
Pancreatitis
Deafness
Arithritis
Bacterial - Acute Sialadenitis
Signs and symptomsSwelling, xerostomia, failure of secretion with ascending infection
(Staph aureus, Strep pyogenes, most common infective organism)
Painful swelling parotid gland, overlying skin red, shiny & tense, pus from parotid duct
(if involving the parotid gland)
Bacterial - Acute Sialadenitis
TreatmentCulture pus for Sensitivity
Prescribe appropriate antibioticSupportive therapy
FluidsHot pads
Salivary stimulants
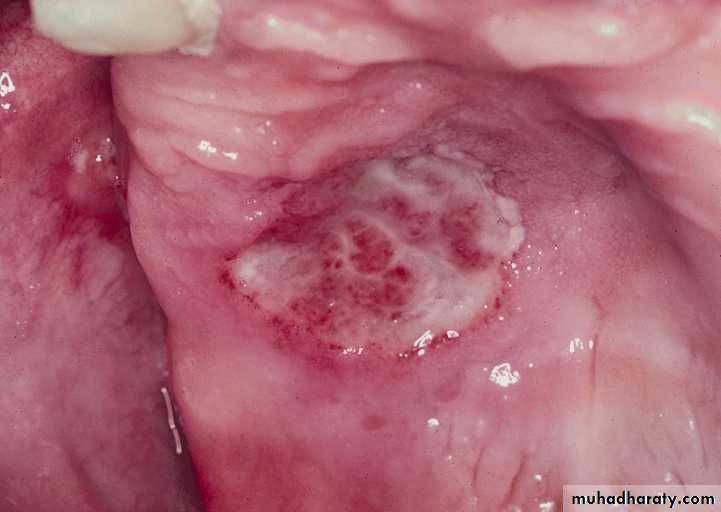
Necrotizing Sialometaplasia
Benign inflammatory conditionUsually involves the minor salivary gland of hard palate
Will often simulate a malignant condition
No definite etiology
1-3 cm ulcer heals spontaneously
Bilateral
Midline
in locationNeoplastic Disorders of the Salivary Glands
80% of salivary gland tumor occur in the parotid.5 – 10% in the submandibular gland.
10 – 15% in the minor salivary gland.
80% of the parotid tumor are benign.
The most common is pleomorphic adenoma.50% of the submandibular gland tumor are benign.
30% of the minor salivary gland are benign.
Salivary Gland Tumors
Benign Salivary Gland Tumors
Adenomas (Epithelial)
Pleomorphic adenoma
Monomorphic adenomaAdenolymphoma
Oxyphilic adenomaOther types
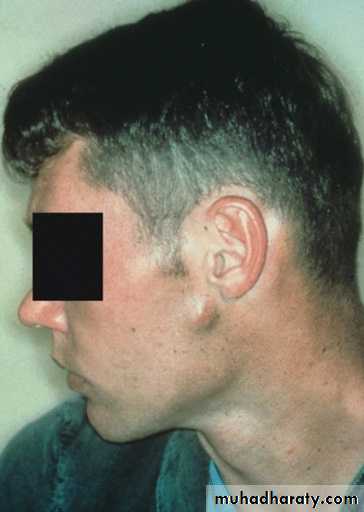
Pleomorphic Adenoma (Mixed Tumor)
Commonest tumour ( 53% - 71% ) of the salivary glandsTumor is slow growing, painless, solitary, firm, smooth, moveable without nerve involvement
Both mesenchymal / epithelial elements
Investigations include FNA, CT, MRIPleomorphic adenoma cont’d
Epithelial ComponentsTubular and cord-like arrangements
Cells contain a moderate amount of cytoplasm
Mitoses are rare
Stromal or “mesenchymal” Components
Can be quite variable
Attributable to the myoepithelial cells
Most tumors show chondroid (cartilaginous) differentiation
Osseous metaplasia not uncommon
Relatively hypocellular and composed of pale blue to slightly eosinophilic tissue.
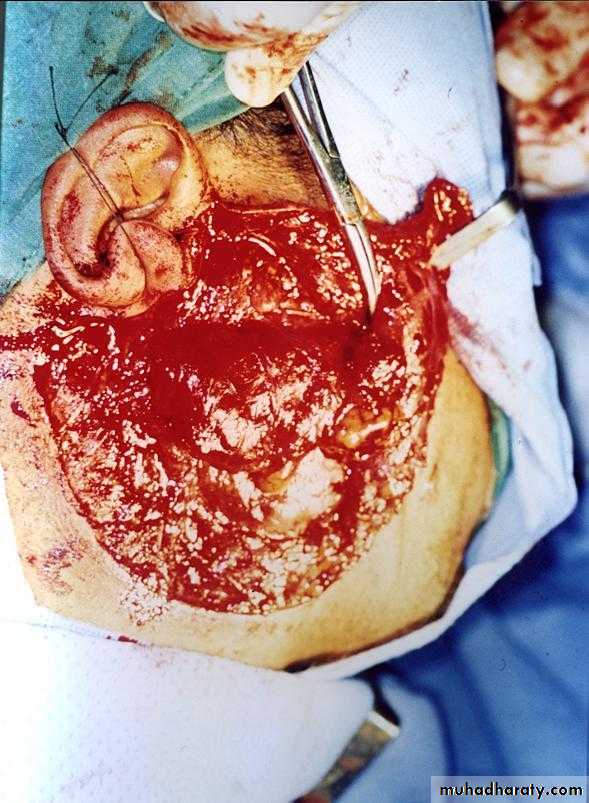
Management
Superficial parotidectomy
total parotidectomy if deep lobe involvement
Recurrent rate 5% with superficial parotidectomy
Chance of turn to malignancy 3-10%
Pleomorphic adenoma cont’d
Monomorphic Adenoma
Similar to Pleomorphic Adenoma except no mesenchymal stromal componentPredominantly an epithelial component
More common in minor salivary glands (upper lip)
Rare malignant potential
Types:
Basal Cell Adenoma
Canicular Adenoma
Myoepithelioma Adenoma
Clear Cell Adenoma
Membranous Adenoma
Glycogen-Rich Adenoma
Warthin’s Tumor
Warthin’s tumour is also called as papillary cystadenoma lymphomatosum6% - 10% of all parotid tumors
Benign , affects parotid gland only
bilateral ( 10% )
Older age group
Superficial location, therefore in most cases Superficial parotidectomy is performed.
Both lymphoid and oncocytic epithelial elements must be present to diagnose Warthin’s
Malignant potential not existed
Malignant Tumours of the Salivary Glands
Locally aggressive in natureSome grow along neural pathways, may access skull base and brain eventually
Also lymphatic and haematogenous spreadIncidence of Salivary Gland Malignancy According to Site
Sublingual 70%Submandibular 40%
Parotid 20 %
A useful rule of thumb is the 25/50/75 rule. That is, as the size of the gland decreases, the incidence of malignancy of a tumor in the gland increases in approximately these proportions.Salivary Gland Tumors
Features suggestive of malignancyInduration
Fixed overlying skin or mucosa
Ulceration of skin or mucosa
Rapid growth
Short duration
Pain often severe
Facial nerve palsy
Malignant neoplasm
Mucoepidermoid carcinomaAdenoid cystic carcinoma
Acinic cell carcinoma
adeno carcinoma
Carcinoma Ex. Pleomorphic adenoma or malignant mixed tumor
Squamous cell carcinoma
Undifferentiated carcinoma
miscellaneous
Mucoepidermoid Carcinoma
Mucoepidermoid carcinoma (MEC) is the most common malignant tumor of the parotid gland and the second-most common malignancy (adenoid cystic carcinoma is more common) of the submandibular and minor salivary glands.
MECs constitute approximately 35% of salivary gland malignancy, and 80% of MECs occur in the parotid gland.
Mucoepidermoid tumor
MECs contain two major elements:mucin-producing cells and epithelial cells of the epidermoid variety
75% are low grade & have good prognosis
5 year survival 85%
High grade mucoepidermoid carcinomas invade locally, spread regionally with distant metastasis.
5 year survival drops 30%
Carcinoma in pleomorphic adenoma
Mixed malignant tumourLong standing pleomorphic adenoma
Older age group
Worse prognosis
Lymph node metastases 15%
Distant metastases 30%
5 year survival 40% - 50%
15% year survival 20%
Adenoid cystic carcinoma (cylindroma)
2nd most common malignant
ACC is the most common malignant tumor found in the submandibular, sublingual, and minor salivary glands.
Age : 40-60 yrs
Peri-neural invasion
30% lymph node metastasis,
50% distant metastasis
- 5 year survival 75%
- 10 year survival 30%
- 20 year survival 13%
Adenoid cystic carcinoma
Acinic cell carcinoma2-4 % of all salivary gland tumors
Most common at parotid gland
Age 30-60 yrs
Characteristic
Bilateral ( 3%)
Well defined border
Hematogenous spreading to lung, spine
Gross : no capsule but clear border
Management
Surgical with facial nerve conservation
Low recurrent rate
Acinic cell carcinoma
Acinic cell carcinoma
adenocarcinoma
Minor salivary > parotid glandMen 30-60 yr
Most severe
High recurrence rate
Metastasis is common
Management
Total parotidectomy ( if in parotid) & resection some part of facial nerve & cervical lymph node dissection
Squamous cell carcinoma of Salivary glands
Infrequent occurrence 1% - 5%May have skin infiltration
Total radical parotidectomy
Evaluation & Diagnosis of Malignant Salivary gland TumorsHistory & clinical examination, use TNM Classification to stage the cancer
Sialography – of no value
CT scans and MRI
CT sialography for retromandibular / parapharayngeal lesions
Incisional biopsy is contraindicated
FNAC
74
Investigations
FNAC >90% specificity, sensitivity
MR =ideal for deep lobe
MR Angiography
CT-3D sialography
99 m Tc scan for Warthin’s
75
MR>CT
Tumor-salivary gland interface
Benign Vs malignant
7 n or Perineural evaluation
Intracranial extension of tumor
DD; Parapharyngeal tumors
DD; Neurogenic tumors
76
CT>MR for bone erosion
CE-CT is better than non CE
Base of skull involvement
Mandible erosion
77
T
T1 <2 cm
T2 >2-4 cm
T3 >4-6 cm
T4 >6 cm
78
N
No no lymph node metastasis
N1 <3 cm,ipsilateral single
N2 A >3-6 cm,ipsilateral single
B <6cm,ipsilateral multiple
C <6cm, bilateral
N3 >6 cm
79
M
Mo -ve distant mets
M1 +ve distant mets
80
M
Lung
40% Adenoid Cystic
30% Malignant Mixed
Also with Acinic cell
SM:P::2:1
81
Mode of Spread
Expansion
Local infiltration
Lymphatics
Perineural infiltration
Seedling locally and in the skin
Indication for postoperative radiation therapy salivary malignancy
High-grade tumors
Squamous cell carcinoma
Malignant mixed tumors
Adenocarcinoma
High-grade mucoepidermoid carcinoma
Close or positive margins
Facial nerve involvement
Indication for postoperative radiation therapy salivary malignanncy
Perineural spreadBone/connective tissue involvement
Lymph node metastasis
Extranodal extension
Recurrent diseases
True or false