NMJ DISORDERS
Myasthenia Gravis:Autoimmune, fluctuating (diurnal rhythm & relapse & remission), fatigueable & painless weakness disorder affecting particularly, ocular, masticator, facial, neck, deglutition, lingual muscles & extremity & respiratory muscles.
Epidemiology:
Is of clinical interest, annual incidence rate: 1/300,000. The disease has two peaks 1st peak: 20-30 yr & female: male ratio = 2:1 to 3:1, the 2nd peak: 50-60 yr & male to female ratio 3:2, onset younger than 10 yr is rare <10%. The second peak associated with thymoma especially in males.
Pathologically:
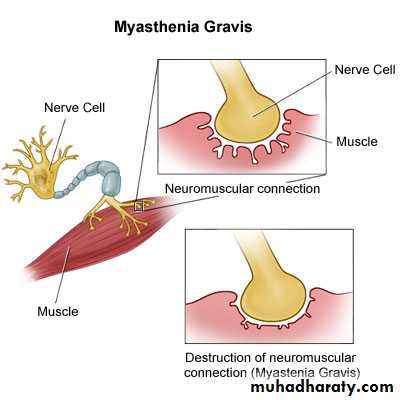
Autoimmune disease, in which autoantibodies (AchR Ab) attack the Ach R in the muscle post-junctional membrane; blocking neuromuscular transmission & inducing complement, mediated inflammatory response which decreases Ach R & damages muscle end plate.
>75% +ve Ach R Ab, about 40% of seronegative patients have +ve AntiMusk Ab.
Thymus gland abnormalities as thymic gland follicular hyperplasia & Lymphorrhages lymphocyte infiltration into muscle is found in majority of cases; while Thymoma found in 15% mainly in the 2nd peak & mainly in males.
There is association with certain HLA types & other Autoimmune diseases ex. Thyroid diseases, SLE, RH Arthritis.
Certain Factors trigger exacerbation of the disease:
Infection - Pregnancy - Menses
Drugs: AB: -Tetracycline - Quinolones - Aminoglycosides
-Beta Blockers - Na channel blocker (phenytoin)
-Lithium - Procainamide & quinine
FIG.1 Simplification of Motor End Plate FIG.2 Epressionless (Sagging) Face
Clinical Presentation:
Insidious onset,painless, diurnally fatigueable weakness, characteristic worsening with exercise & improvement with rest:
Occular : variable unexplained diplopia, ptosis, lid twitching (Cogan Sign).
Face: weak facial muscles may give expressionless face & tenting of the lips, weakness of speaking & nasal quality, chewing & swallowing (support chin with hands).
Respiratory: weakness of diaphragmatic muscle may necessate ICU admission.
Extremties: mainly proximal limb girdle muscles mostly shoulder girdle.
NO ( SENSORY, MUSCLE ATROPHY or REFLEX LOSS)
INVESTIGATIONS:
Clinically (Provocative Tests):Eye: sustained up gaze (Curtain sign)
Limbs: sustained elevation (dropping)
Oropharyngeal: Counting Loud.
Tensilon Test: By IV injection of Edrophonium Bromide initially 2mg, later 8m half minute later if no side effects, improvement after 30 seconds & may persist for 3 minutes.
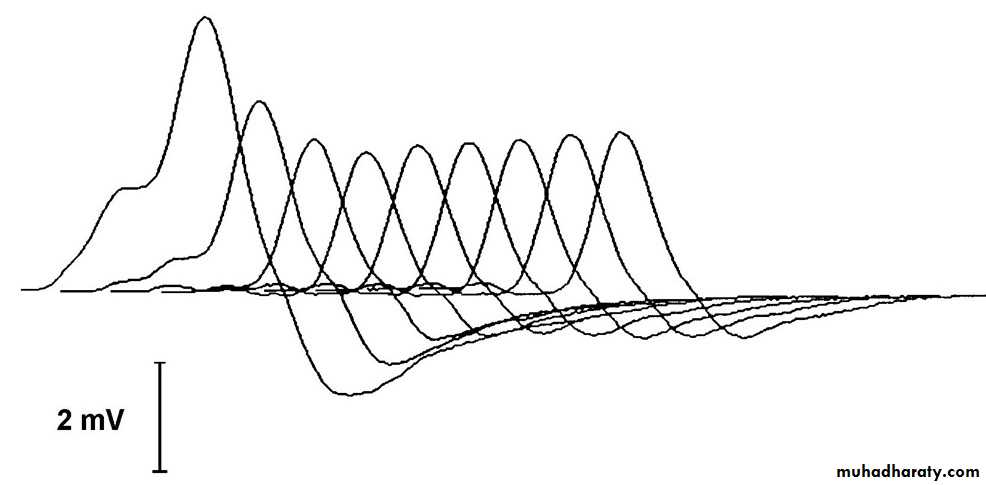
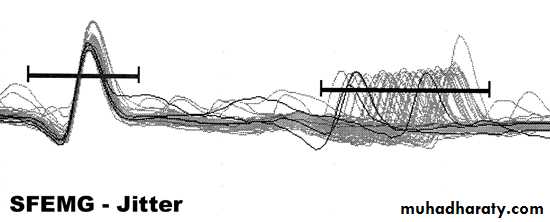
EMG: Repetitive nerve stimulation RNS show decremental response & Single Fibre EMG is diagnostic in most cases.
AchR Ab 80%&if negative AntiMusk Ab 40% & Anti skeletal muscle Ab in Suspected thymoma.
CXR & Contrast chest CT should be done for all patients.
Exclusion of overlap syndrome: Thyroid function test & Antinuclear Ab.s connective Tissue Diseases.
For Diagnosed cases Serial follow up for: Immune Status, TB, Hepatitis, and HIV.
EMG-RNS Decremental Respense 2-SFEMG-Jitterness
TREATMENT:Aim: 1- To maximize the activity of Ach at the receptor sites at NMJ.
2- To limit or abolish the immunological attack on motor end plates.
AntiCholinestrase Drugs: Pyridostigmine Bromide 60mg tab. & up to 480 mg sometimes given.
Immune Modulators:
Corticosteroids: for patients not responding optimally to Pyridostigmine, should be initiated in the hospital & for long courses (months to years). Not indicated for pure ocular myasthenia.
AZATHIOPRIME ( Immuran) tab, 2-3mg/kg, could be steroid sparing agent, but delayed onset of action..
Mycophenolate Mofetil
Cholinergic Crisis TreatmentsEMERGENCY TREATMENTS
Plasmapharesis PE: in Myasthenic Crisis & Preoperative preparation.
Immunoglobulin IgG: as alternative to PE in crisis patient.
Thymectomy: should be offered in any:
Seropositive - <45yr old - not confined to ocular
Disease duration not more than 7 years.
CRISES IN MYASTHENIA GRAVIS
I-Myasthenic Crisis: Profound weakness in affected muscles in myasthenic patient, often precipitated by: 1- withdrawal of anticholinestrase drugs.
2- Withdrawal or decreasing dose or acute administration of high dose of steroid.
3- Infection. 4- Bad choice of contraindicated drugs.
Patient should be managed in ICU with IV IgG or PE, AB, Correction of the cause.
II-Cholinergic Crisis:
Occurs in patient with AchE I drug OD overdose characterised by weakness in unaffected
muscles enhanced by iv edrophonium, pallor, sweating, salivation, nausea, vomiting, colicky abdominal pain & meiosis. Reversed by anti cholinergic drugs.
Course & prognosis:
Course is extremely variable but tend to stabilize after 7 years from disease onset. Fatality mostly from respiratory failure about 5% with appropriate management in the first years of illness.Lambert Eaton Myasthenic Syndrome LEMS:
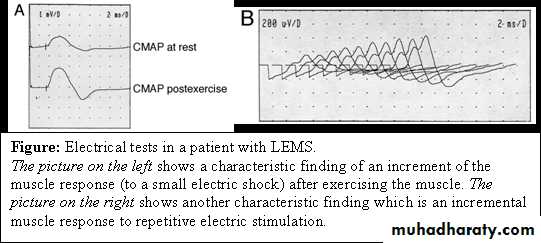
Autoimmune NMJ Disorder, VGCC Ab inhibiting synaptic release, High probability to be Paraneoplastic Disease; hence screening for primary cancer especially in elderly.Clinically: characteristically spare eye muscles, Lower limb weakness proximally with areflexia & tendency to improve after exercise (vs MG), erectile & sphincteric dysfunction, dry mouth & postural hypotension (autonomic) are characteristic.
Investigations:
EMG shows POSTTETANIC POTENTIATION
CT scan to look for malignancy.
Treatment:
Treatment of associated cancer
Symptomatic:
3,4 Diaminopyridine DAP or
Guanidine
Infective NMJ Disorder:
Botulism:Caused by the neurotoxin of Clostridium botulinum, which is extremely potent & cause disease after ingestion of even picogram amounts.
PERIODIC PARALYSIS SYNDROMES
Disorders characterised by Recurrent, Episodic, Generalised, Painless, of fairly Rapid onset of muscle weakness associated with coincidental changes in serum electrolyte level, and reversal to norm in between attacks.
Hypokalaemic Periodic Paralysis:
The best well known form of Periodic Paralysis, Calcium Chanelopathy, AD pattern of inheritance with reduced penetration in females, ratio 3 to 4:1.
Association with THYROTOXICOSIS might be & attacks might be provoked by Exercise or Diet rich in (CHO & Na).
TYPICAL ATTACK: usually after second half of the night or early morning, evolves over minutes to several hours, proximal more than distal muscles of the limbs in Ascending pattern, more than trunk muscles, lasting less than 72hr.
The muscles more likely to escape weakness: eyes, face, tongue, pharynx, larynx, diaphragm & sphincters.
Investigations:
Ictal Serum Potassium levels below 3.5mEq/L.
ECG: prolong PR, QRS, QT & flattening of T wave.
Thyroid Function Tests.
Muscle Bx: multiple centrally placed vacuoles & PAS granules.
EMG: show electrical silence in severly weakened muscle.
Treatment:
1-Acute Attack: - Orally (if possible) KCl tab.
-IV KCl: 0.2-0.4 mmol/Kg/day in Mannitol as Vehicle
2- Prophylaxis: -Avoid (intense exercise, Na & CHO rich diet), but mild regular exercise advised to keep fitness
3- Acetazolamide 250-1000/day in divided daily doses.
4- Dichlorphenamide if Acetazolamide fails. Or.
5-Spironolactone 25-100 mg/day
Thyrotoxicosis should be treated.
Course & Prognosis:
In acute attack recovery of the lastly affected muscle till reaches first affected (Descending). Attacks tend to occur every few weeks& tend to lessen with advancing age. Rarely death may occur from respiratory failure or fatal cardiac arrhythmias.
Hyperkalaemic Periodic Paralysdisis (HyperKPP)
AD, Na Chanelopathy, with peak incidence in the first decade.
TYPICAL ATTACK: often preceded by Potassium Rich Diet, or Rest, 7especially rest following strenuous exercise, the attacks are brief 30min.-4 hours, associated with serum potassium levels often but not always 5-6mmol/L, with pattern similar to HypoKPP & only in severest attack head & neck muscles involved while respiratory muscles spared, recovery might be hastened with mild exercise.
MYOTONIA if coexist usually detected EMG wise, but occasionally could be seen clinically & its effect is difficult to separate from attack, indeed, when attack of paresis prevented by mild continuous movement, firm, painful lumps may form in calf muscles.
Investgations:
1-K Level: during attack, while it is usually normal in between.
2-ECG.
Treatment:
Acute Attack:
1-IV Ca Gluconate Slowly. If after minutes this unsuccessful then:
2-IV Glucose or Glucose & Insulin. 3-Diuretics: as IV Frusemide.
Prophylaxis
1-Acetazolamide (Diamox): tab 250mg 2-3/day. Or Dichlorphenamide.
2-Chlorthiazide. 0.5 mg/day. 3-Mexiletine tab. 200mg, 3/day.
4- Treatment for myotonia if significant.
NormoKalemic Periodic Paralysis (NormoKPP)
This condition is similar to HyperKPP in all aspects except that their serum potassium levels during the attack are within normal & they are sensitive for potassium loading.
+