
Pathology dr.rasha(lecture4)
1
The heart:-
Most common diseases of heart are:-
(I) Ischemic heart disease:-
It's a group of closely related syndromes cause by an imbalance between the
myocardial oxygen demand and blood supply.
The most common cause of ischemic heart disease is a reduction in coronary
arterial blood supply due to
I- atherosclerosis
of coronary arteries. Ischemic
heart disease is responsible for about one third of all deaths.
Depending on the rate and severity of coronary artery narrowing and the
myocardial response. One of the 4 syndromes may develop:-
1- Various forms of angina pectoris (chest pain).
2- Acute M.I.
3- Sudden cardiac death.
4- Chronic ischemic heart disease with congestive heart failure.
These syndromes are late manifestations of coronary atherosclerosis that
probably begins during childhood.
Pathogenesis:-
Symptomatic ischemic heart disease is associated with reduction reached 75%
or more of one or more coronary arteries by atherosclerotic plaque. In
addition to chronic fixed atherosclerotic plaques various superimposed lesions
also play an important role in the development of myocardial ischemia, these
include:
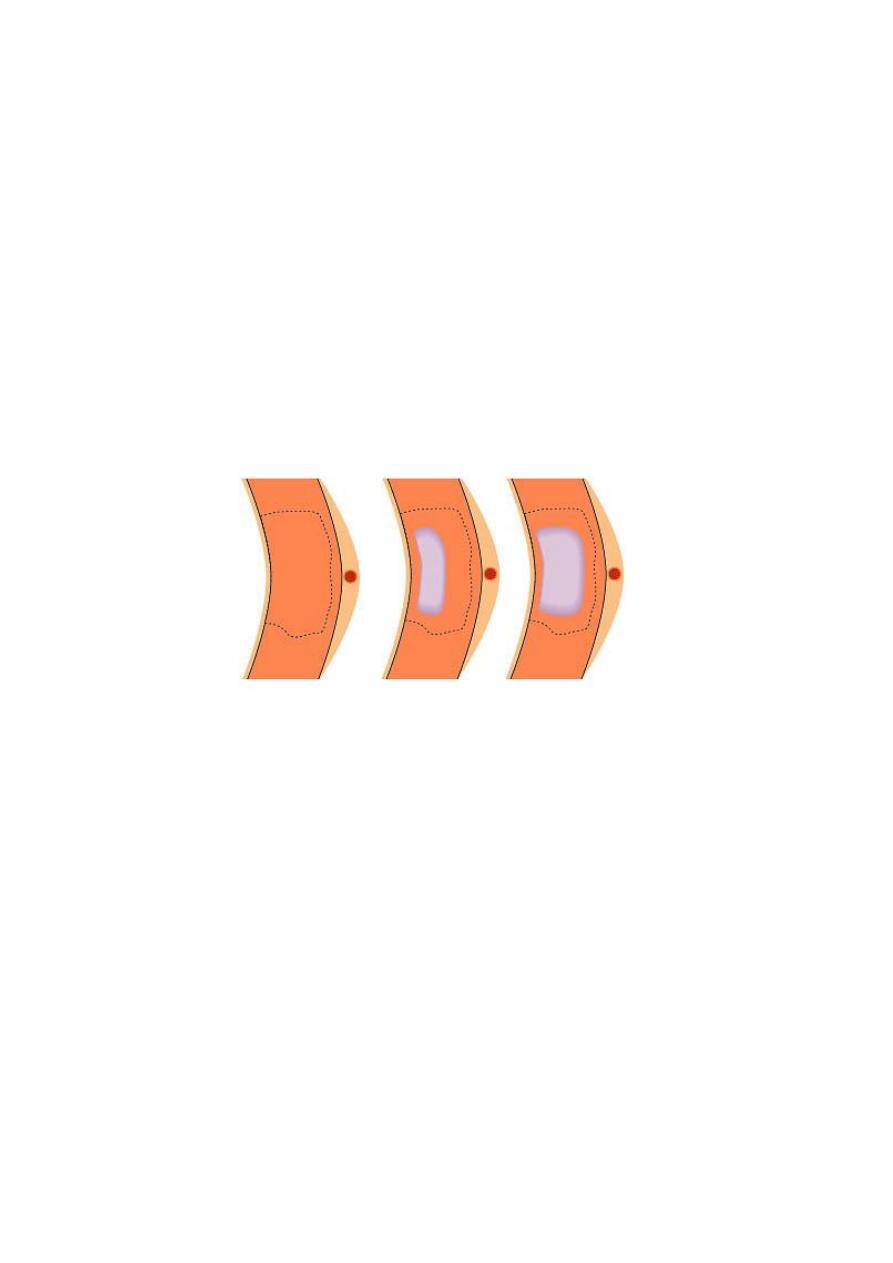
1- Acute changes in plaque morphology.
2- Platelets aggregation.
3- Coronary artery thrombosis.
4- Coronary artery vasospasm.
Pathology dr.rasha(lecture4)
2
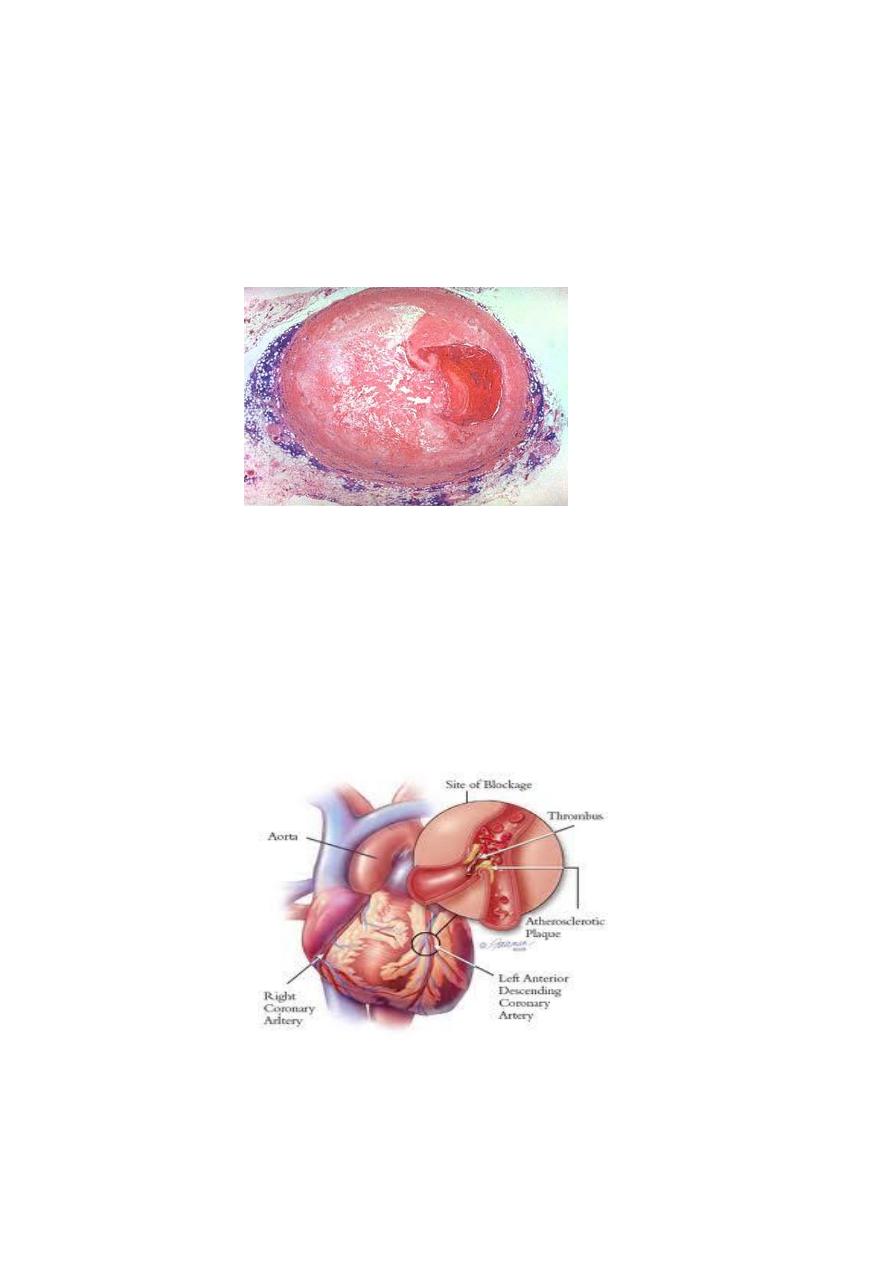
1-The acute morphological changes
of chronic atherosclerotic
plaques include fissuring, hemorrhage into the plaque and plaques
rupture with embolization of atheromatous debris into distal
coronary vessels, it will cause enlargement of the plaque also local
disruption of plaque increase the risk of platelets aggregation and
thrombosis at that site.
2- Local platelets aggregation
seen in unstable angina pectoris and
sudden cardiac death, these platelets cause mechanical obstruction and
releasing of mediators causing coronary vasospasm, so cause myocardial
ischemia.
3- Coronary artery thrombosis
is
almost always associated with severe
atherosclerotic plaques. Local disruption of atheromatous plaques plays an
important role in the development of thrombi by exposing thrombogenic,
lipid-rich plaque debris to the blood.
4- Coronary artery spasm:
This occur in particular type of angina pectoris,
this occur at site of plaque disruption, it's supposed to be induced by the
, from platelets,
2
release of vasospastic mediators such as thromboxane A
Pathology dr.rasha(lecture4)
3
also endothelial dysfunction also precipitate vasospsm by reduced
elaboration of endothelial cell-derived relaxing factors, also ά-adrenergic
activity and smoking have also implicated.
(II) There are other minor causes
decrease blood flow through coronary arteries as:
1- Emboli
originating from vegetation on aortic or mitral valves.
2- Coronary vasculitis.
3- Severe systemic hypotension.
(III) There are factors increased myocardial oxygen demand
also cause
myocardial ischemia, as in:
1- Left myocardial hypertrophy.
2- Hypertension.
3- Disaeases of heart valves.
:
Angina pectoris
The term angina pectoris refers to presence of intermittent chest pain
caused by reversible myocardial ischemia.
Myocardial infarction:
It's a single most common cause of death which's consisting of
Definition:
development of a defined area of myocardial necrosis caused by local
ischemia.
Risk factor of M.I are the same of atherosclerosis.
Pathogenesis:
Most acute M.I are caused by preexisting atherosclerosis with thrombosis.
This thrombosis occur usually on nidus of fissure formation on the plaque,
however vasospasm and platelets aggregation may contribute to coronary
artery occlusion.
Pathology dr.rasha(lecture4)
4
Myocardial necrosis begins within 20 to 30 minutes of time of coronary
artery occlusion. The myocardial infarcts typically begin with
subendocardial region, because: a-it's the last area to receive blood from
branches of the epicardial coronary arteries.
b- the relatively high intramural pressures that exist in this area.
The zone of necrosis extends externally over the nest several hours to
involve mid and subepicardial areas of myocardium.
The infarct usually reach the full size within 3 to 6 hours, so that during this
period lysis of thrombus by administration of thrombolytic agents as tissue
plasminogen activator may limit the size of infarct.
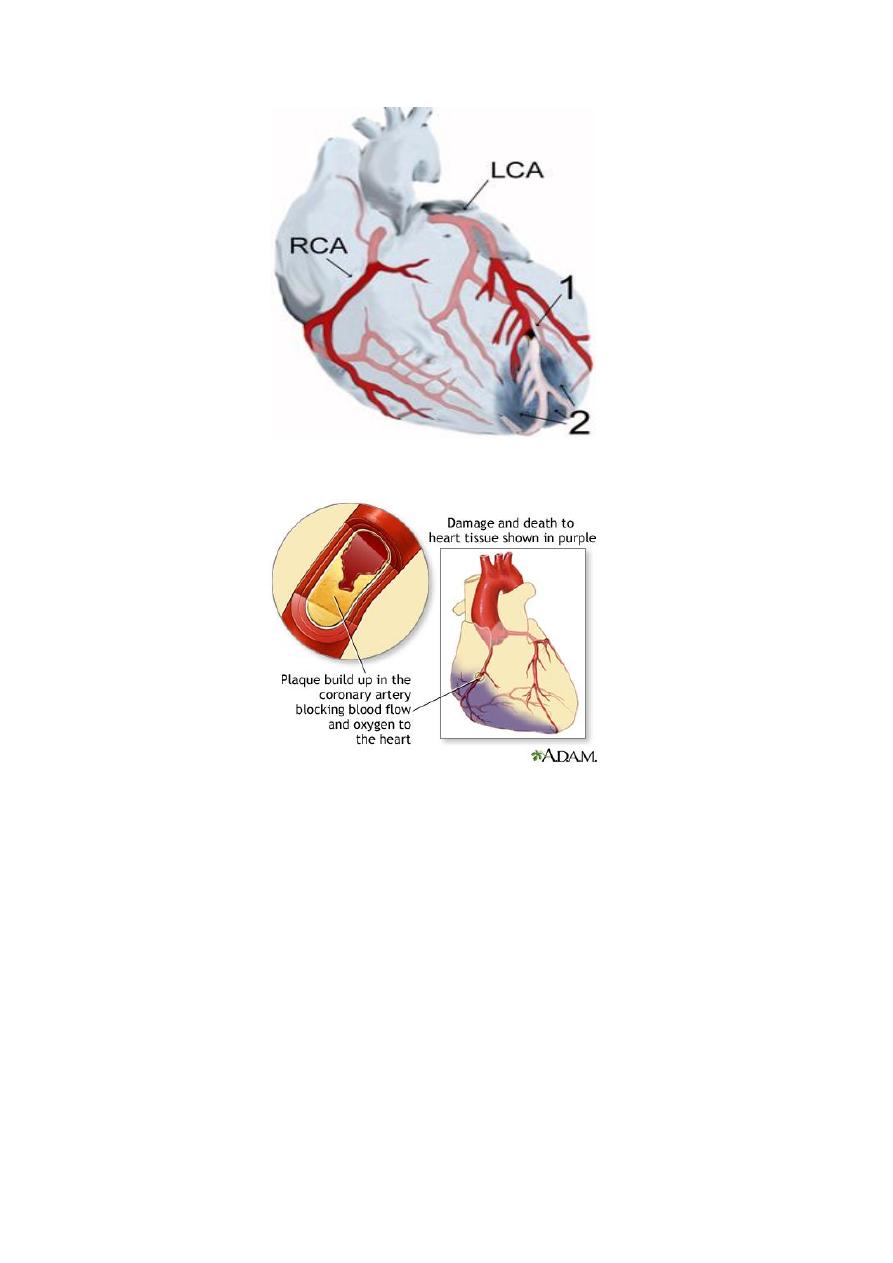
The location of M.I is determined by the site of the occlusion and by the
anatomy of coronary circulation .e.g. occlusion of left anterior descending
coronary artery cause infarction of anterior and apical areas of left
ventricle, occlusion of the right coronary artery is responsible for most
infarcts involving the posterior and basal portions of left ventricle.
Pathology dr.rasha(lecture4)
5
The size of infarct is influenced by several factors e.g. occlusion of more
proximal segments of the coronary arteries products larger infarcts
involving the full thickness of myocardium, while occlusion of more distal
arterial branches cause smaller infarcts, also in long standing coronary
atherosclerosis, collateral circulation may develop over time in response to
chronic ischemia, this collateral limit the size of infarct.
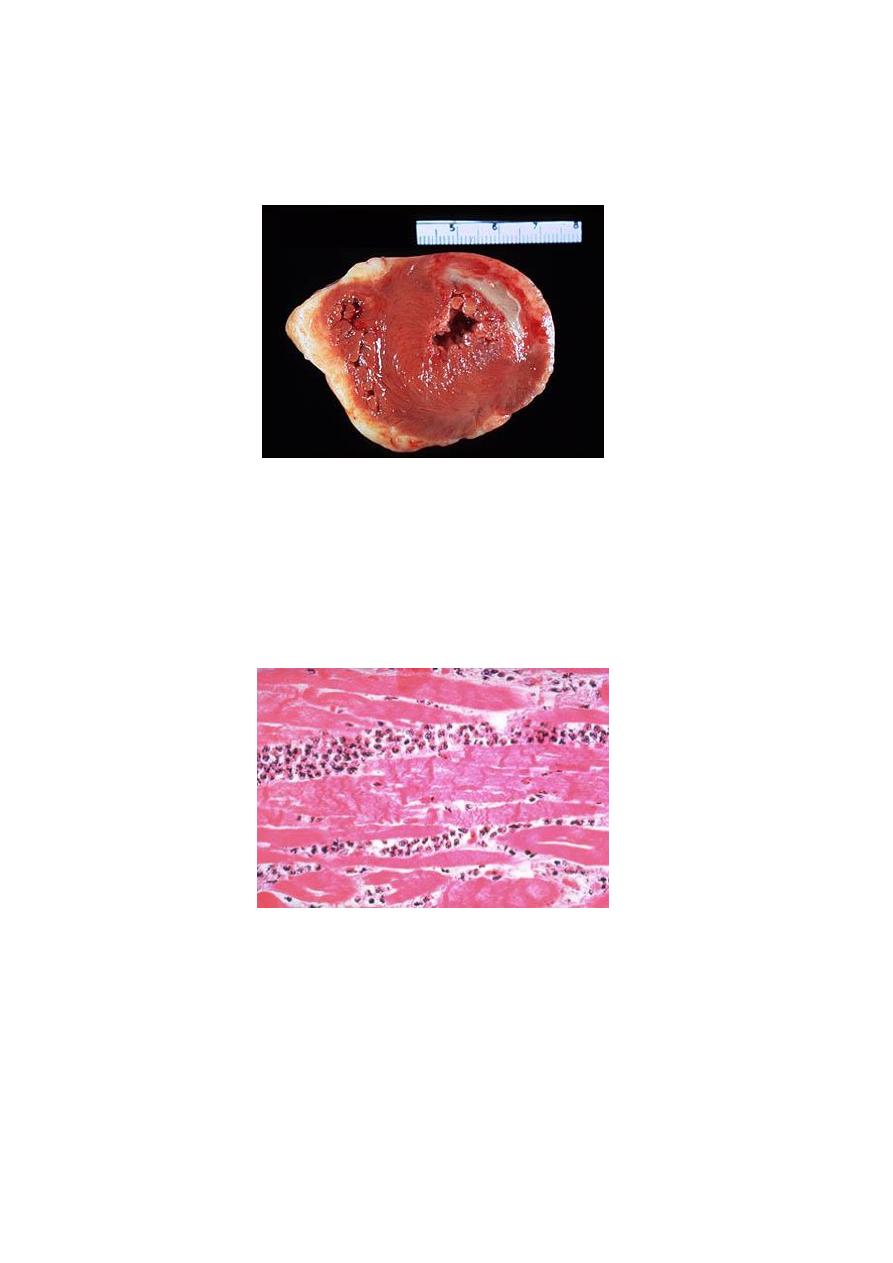
Morphology:-
The changes occur is that of coagulative necrosis and inflammation
followed the formation of granulation tissue, resorption of the necrotic
myocardium and finally organization of the granulation tissue to form a
fibrous scar.
Pathology dr.rasha(lecture4)
6
The morphological changes associated with M.I for the first 12 hours no
changes are evident on gross examination , between 18-24 hours a slight
pallor may be noted .
Microscopically:
Coagulative necrosis become apparent by about 12 to 18
hours so the myocytes become necrotic and having eosnophilic cytoplasm
with loss of cross striation , the nuclei begin to undergo fragmentation
(karyorrhexis) or pyknosis, neutrophils are attracted by the necrotic
myocardium.
Chronic ischemic heart disease (ischemic cardiomyopathy)
It is a progressive congestive heart failure as a consequence of long term
ischemic myocardial injury, it is associated with a history of angina pectoris
and may be preceded by recognized infarct

Pathology dr.rasha(lecture4)
7
Morphology:
The coronary arteries contain areas of moderate to severe
atherosclerosis, the heart is enlarged due to dilation of all cardiac chambers ,
multiple areas of myocardial fibrosis with transmural scarring .
Microscopically:
Reveals extensive myocardial fibrosis due to chronic ischemia.
