AHMED JASIM GYNE 19/12/2016
Dysmenorrhoea
Is defined as painful menstruation and it is very common complaint.
Dysmenorrhoea can be classified as:
1. primary Dysmenorrhoea (primary spasmodic)(is the commoner
type).
2. Secondary Dysmenorrhoea (congestive, acquired).
Primary dysmenorrhea :-
Presence of painful menstruation where there is no underlying
pathology.
The prevalence of dysmenorrhoea is high. 72% of women reported
dysmenorrhoea in their life.
Etiology :-
There are a number of factors that may have an aetiological role.
1. Endocrine: Ovulatory cycle are necessary for development of
primary dysmenorrhoea.
2. Abnormal uterine activity : Primary dysmenorrhoea is
associated with uterine hypercontractility and a high resting tone
between contractions which may be mediated by increased
Prostaglandin levels or vasopressin.
3. Psychological : It is unlikely but it may influence individual
perception to painful stimuli.
Diagnosis :-
Diagnosis is usually based on history and normal findings on clinical
examination.

History :-
It is usually occurs in girls or young women.
It appears 6–12 months after the menarche when ovulatory cycles begin to
become established (The early cycles after the menarche are usually
anovular and tend to be painless).
The pain usually begins just prior to, or on the first day of the period. It lasts
for several hours or continuo throughout the first and second day.
It is usually described as a colicky (spasmodic, crampy) lower abdominal
pain and intense in suprapubic region associated with backache radiated to
lower limb and there may be associated gastrointestinal disturbances such as
diarrhoea and vomiting and other symptoms such as nausea, fatigue, and
headache. Severe pain occur in small number of women and leads to absence
from work or education.
If symptoms are typical of primary dysmenorrhoea, a therapeutic trial may
be embarked on before considering any examination and investigation
especially in adolescents.
Examination :-
General examination : no abnormal finding.
Abdominal examination: no abnormal finding
pelvic examination in married patient : no abnormal finding.
Investigations :-
Investigations requested in these condition:
1. When clinical evaluation raises strong suspicion of underlying pathology.
2. When symptoms of primary dysmenorrhoea are not alleviated by combined
oral contraceptive pills and / or NSAID therapy.
Investigation by ultrasound examination or magnetic resonance imaging (MRI)
or laparoscopy or hysteroscopy according to history and differential diagnosis as
no need to do all investigation in most of cases.
Treatment :-
A. Reassurance and explanation.
B. Using heating pads or taking a warm bath may help to decrease pain.
C. Medical treatment:
1. Ant prostaglandins (NSAIDs): non-steroidal anti-inflammatory drugs
Acts via their suppression of menstrual fluid prostaglandins.
NSAIDs drugs such as ibuprofen (400mg every 6hours), mefenamic acid (500 mg
every 8 hours), naproxen 250mg every 6 hours), and aspirin are all effective.
Ibuprofen is the preferred analgesic because of its favorable efficacy and safety
profiles. They are usually taken during the first few days of menstruation. The
advantage of starting treatment at the onset of menstruation is that it prevents the
patient treating herself when she is unknowingly pregnant which would only
become apparent when a period is missed.
2. THE COMBINED ORAL CONTRACEPTIVE PILL
It is given especially when fertility control (contraception) is required.
They are thought to act by inhibiting ovulation and decreasing endometrial
production of prostaglandins and leukotrienes by inducing endometrial atrophy and
therefore reducing the amount of endometrial tissue available to produce these
mediators. Extended cycle use minimize the number of withdrawal bleeding
episodes.
Extended cycle oral contraceptive (Seasonale) is a 91-day oral contraceptive.
Tablets containing the active hormones are taken for 12 weeks (84 days), followed
by 1 week (7 days) of placebo tablets. it is particularly useful for women who
experience symptoms associated with the withdrawal bleed such as severe
dysmenorrhoea.
3. Combination of both NSAIDs and Combined oral contraceptive pill.
Combination of both NSAIDs and Combined oral contraceptive pill
4. Progestins :-
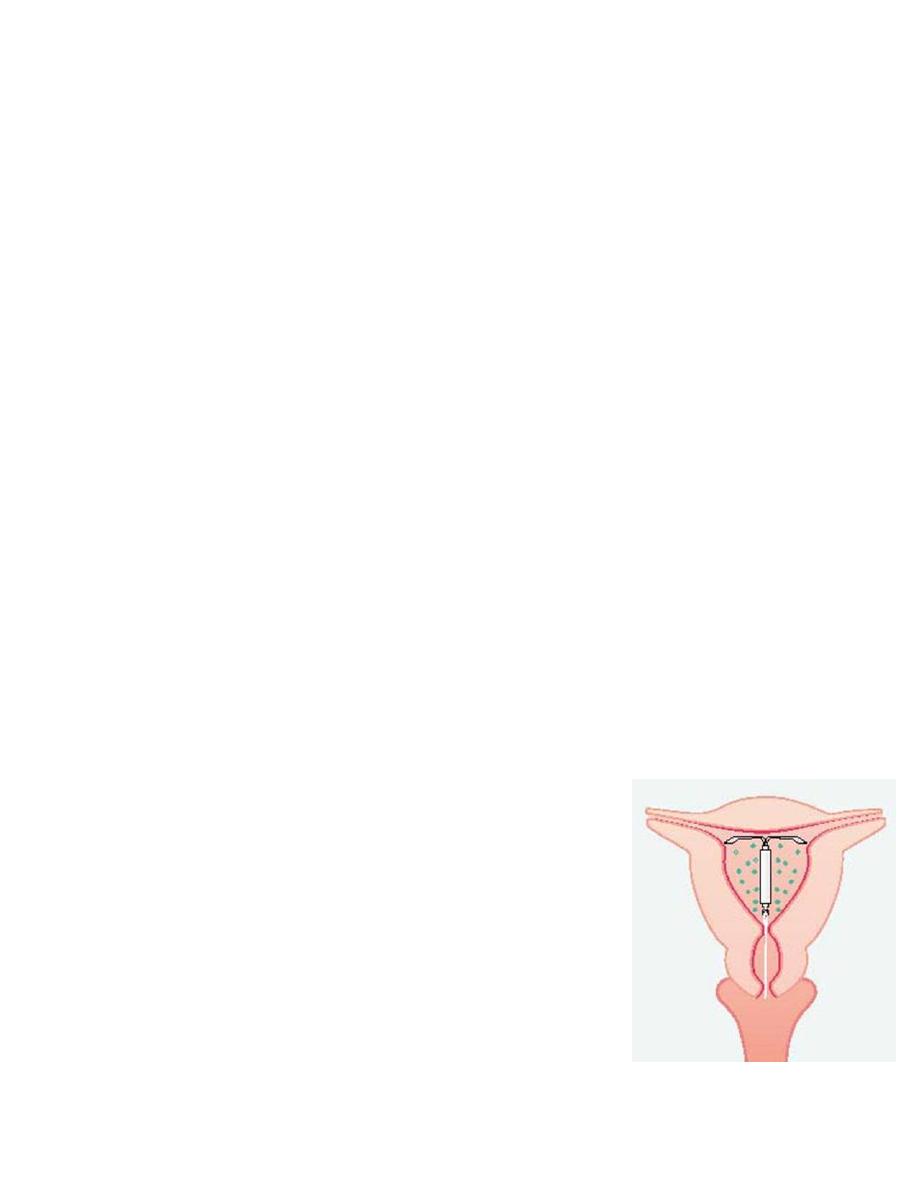
A. Medicated intrauterine device (levonorgestrel
intrauterine system (LNG-IUS) (Mirena)):
effective treatment for women who have a
contraindication to either NSAIDs or the combined
oral contraceptive.
B. medroxy progesterone acetate Depot (Depo-
Provera) 150 mg Intra-Muscular (I.m.) every 12
weeks.
Clinically they are effective since they render most
women amenorrhoeic.
Desogestrel : new progestogen only contraceptive pills. It effectively
inhibit ovulation and relieve symptoms of dysmenorrhoea.
5. other drugs under evaluation or clinical trial studies used are:
a. vasopressin receptor antagonist:
b. Tocolytics agent: can reduce uterine contractility and thus are
potentially effective. These are:
Beta-adrenergic agonists
calcium channel blockers
Transdermal glyceryl trinitrate has also been evaluated
vitamin E
omega-3 polyunsaturated fatty acids beneficial in the management
of dysmenorrhoea in adolescents.
6. Other measures:
Psychotherapy.
Hypnotherapy.
Transcutanous nerve stimulation (acupuncture).
7. Surgery: It may provide long term relief and used rarely in patients resistant
to drug therapy.
ablation of uterine nerve.
presacral neurectomy
Secondary amenorrhea :
Presence of painful menstruation in the presence of an identifiable pathologic
cause .
It is usually due to one of following:
Endometriosis.
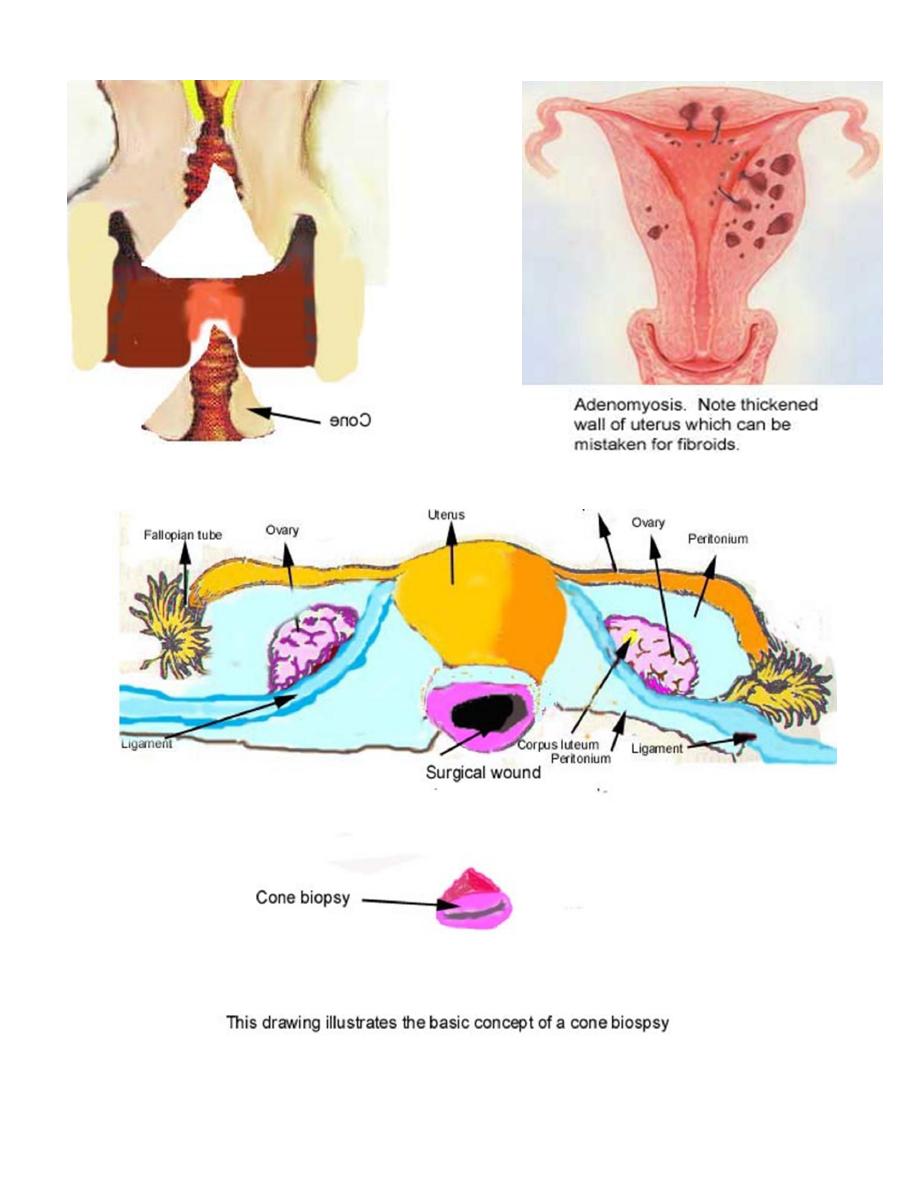
Adenomyosis.
Pelvic inflammatory disease (PID).
Asherman's syndrome (intrauterine adhesions).
Cervical stenosis (may result from conization).
Acquired fixed retroversion of uterus.
Uterine fibroids.

Management :-
It is easily diagnosed from history
History :-
Secondary dysmenorrhoea is easily diagnosed from history.
It develops in older women (in their 30s or 40s). it may appear after some
years of painless menstruation.
The pain is often more severe prior to menstruation. The pain begins a few
days prior to menstruation and continuo throughout the period and even after
the menses. It is less related to the first day of flow. The pain is often a dull
ache felt in lower abdomen and back and sometimes extending to the thighs.
It is usually associated with dysparunia, infertility, abnormal uterine
bleeding.
Clinical examination may not determine cause.
Investigations :-
May help to identify cause and choosing it according to case:
*Pelvic ultrasound show ovarian endometriosis and fixity of ovaries in PID.
*Hysterosalpingogram useful to identify intrauterine adhesion.
*Microbilogical cultures: From endocervix, peritoneal fluid if PID is
suspected.
*Laproscop
Treatment :-
*Treatment of underlying cause (discussed in other lectures).
*Treatment used of primary dysmenorrhoea are often helpful.
*In patient with intractable dysmenorrhea , hysterectomy with bilateral
oopherectomy may be needed.
SH.J
