
1
Fifth stage
Gynecology
Part-2
Dr.Ahmed
/2016
Endometriosis II
Investigations:
• Making a diagnosis on the basis of symptoms alone is difficult as the presentation is so
variable and mimic other disease. Consequently, there is often a delay of several years
between symptom onset and a definitive diagnosis at laparoscopy.
Non invasive test:
None of these tests can definitively confirm or dismiss the presence of endometriosis
lesions. These are:
1. Ultrasound examination: trans-vaginal ultrasound is a useful tool to diagnose and
exclude ovarian endometriomas but it has no value for peritoneal disease.
2. Serum cancer antigen 125 test (CA-125):
• CA-125 measurement has no value as a diagnostic tool for minimal–mild
endometriosis.
• Serial measurements are useful as prognosticators of treatment outcome.
However, normal post-treatment values do not mean that endometriosis is absent.
3. MRI scans: Beneficial in imaging ovarian cyst or invasion of surrounding organ.
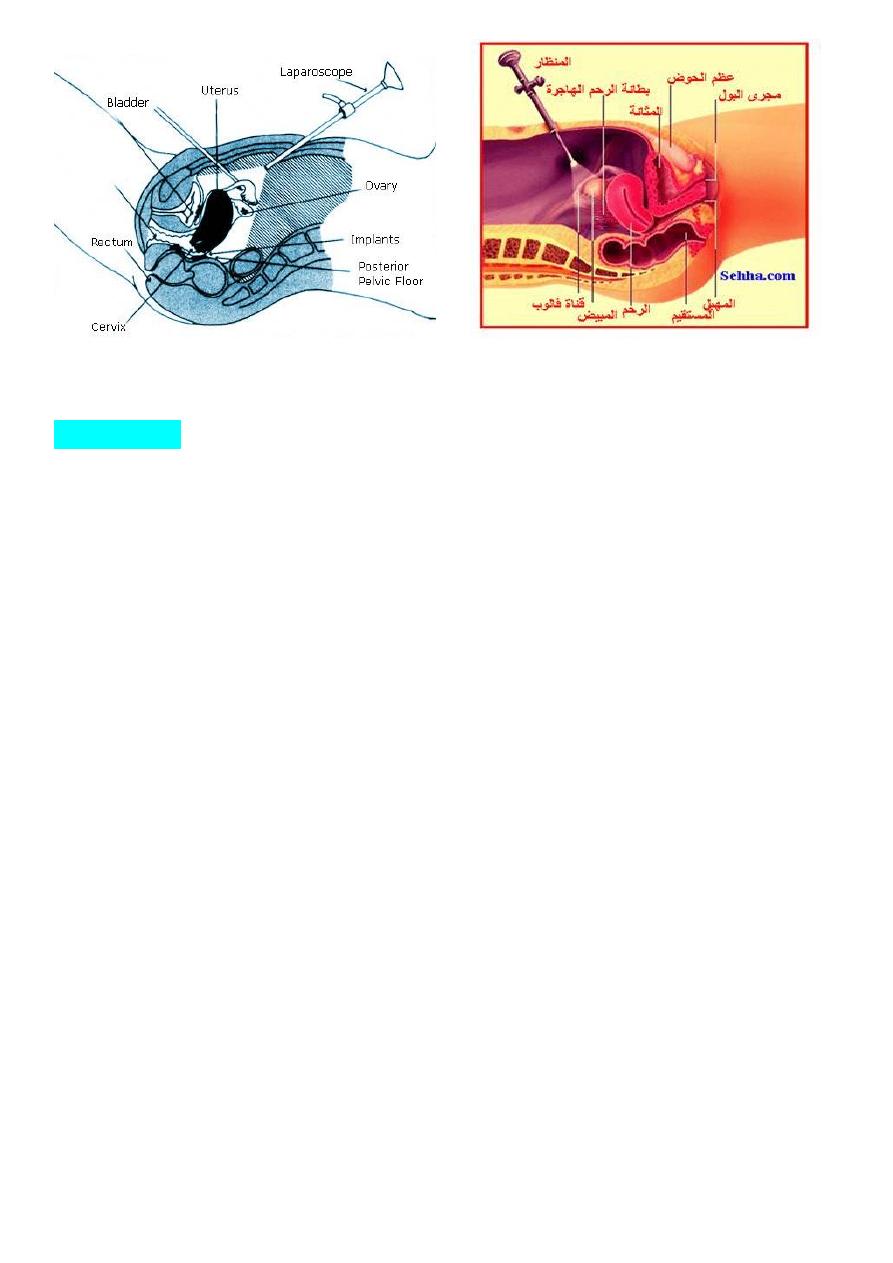
Invasive investigation: Laparoscopy
• Laparoscopy is the gold standard for diagnostic purposes, unless disease is visible in
the vagina or elsewhere. Laparoscopy is considered the primary diagnostic modality
for endometriosis. The classic lesions are blue-black or have a powder-burned
appearance or atypical lesion.
• Visual inspection is usually adequate but histological confirmation of at least one
lesion is ideal, and mandatory if disseminated peritoneal endometriosis (DIE) or a >3
cm diameter endometrioma is present.
• The entire pelvis should be inspected systematically, and good practice is to document
in detail.
2
Treatment:
Treatment must be individualized, taking into account these factors which influence choice
of treatment and these are :
• 1. Woman’s age.
• 2. Fertility status.
• 3. Nature of symptoms.
• 4. Severity of disease.
• 5. Previous treatments.
1.expectant management:
which is essentially a "wait-and-see" approach. It is recommended for:
1.asymptomatic women.
2. infertile patients with superficial disease and mild symptoms.
3. older women approaching menopause.
Expectant management consists of a period of observation with no treatment except the use
of antiprostaglandin medications to relieve pain.
2. medical treatment:
A. Non-steroidal anti inflammatory agents: Are potent analgesic and are helpful in
reducing severity of dysmenorrhoea and pelvic pain but have no specific impact on
disease and its progression.
3
B. hormonal therapies: Hormonal treatments have traditionally attempted to mimic
pregnancy or the menopause. It temporarily shrink endometrial lesions and relieve
symptoms. Peritoneal lesions decrease in size during therapy but reappear rapidly
following therapy; Endometriomas rarely decrease in size and adhesions will be
unaffected.
It may include:
1. combined oral contraceptive pill (COC): continuous use or extended cycle use (every
3 months).
2. Progestogens: It produce pseudo decidualization of endometrium. Oral treatment start
on the fifth day of menstruation and continuo for six months and may need to increase
dose. These are: Norethisterone (primolut-N), medroxy progesterone acetate (Provera),
dydrogestrone. Or can use Mirena (IUD).
3. GnRH-analogues (agonists and antagnosists) induce pseudo-menopause.
It used with Add-back therapy which involves taking one of the following medications at
the same time as a GnRH agonist: a low-dose oestrogen, a low-dose progestin, or
tibolone alone. Add-back therapy can reduce the menopausal-type side effects of GnRH
agonist therapy and preventing or minimizing the thinning of the bones associated with
treatment with a GnRH agonist alone.
4. Danazol 400-800 mg daily course 3-6 months. Androgenic side effect
5. Gestrinone 2.5mg twice weekly- course 3-6 months. Androgenic side effect
Hormonal treatment for subfertility caused by endometriosis:
• Hormonal treatment for subfertility associated with minimal–mild endometriosis does
not improve the chances of natural conception. Clearly treatment can do more harm
than good because of the lost opportunity to conceive.
• In more advanced disease, there is no evidence of an effect on natural conception, but
there may be a role for hormonal treatment as an adjunct to assisted conception.
4
3.surgery:
Conservative surgery
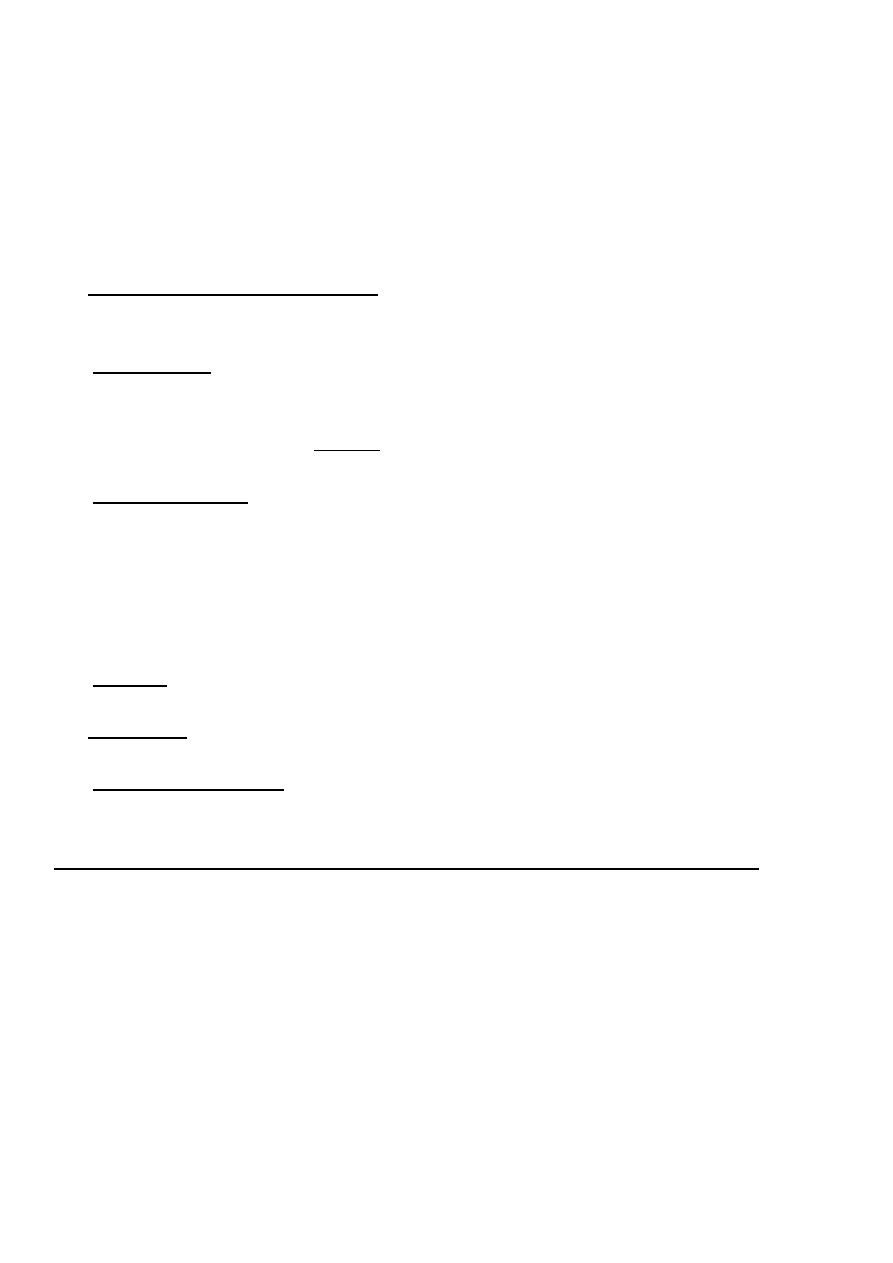
• The laparoscopic approach is the method of choice for treating endometriosis
conservatively. The aim is to destroy visible endometriotic implants, endometriomas,
and lyse peritubal and periovarian adhesions and to restore normal anatomy. excision
or coagulation is preferable for typical lesions. Excision is the preferred method for
endometriomas.
• oophorectomy if large one and patient not need fertillity.
• Fertility patients should be counseled about the risks of reduced ovarian function after
endometrioma excision and the loss of an ovary.
Laparoscopic excision of nodular endometrial lesions overlying the rectum
Definitive surgery:
• Endometriosis surgery can be complex and difficult, and surgeons often need
specialized skills and expertise to perform such surgery.
It is indicated when there is:
• Severe symptomatology.
• Progressive disease.
• Women complete their families.
• Treated by hysterectomy and bilateral salpingo-oopherectomy.
• Patients can receive HRT subsequent to surgery after 6 months or more from surgery.
5
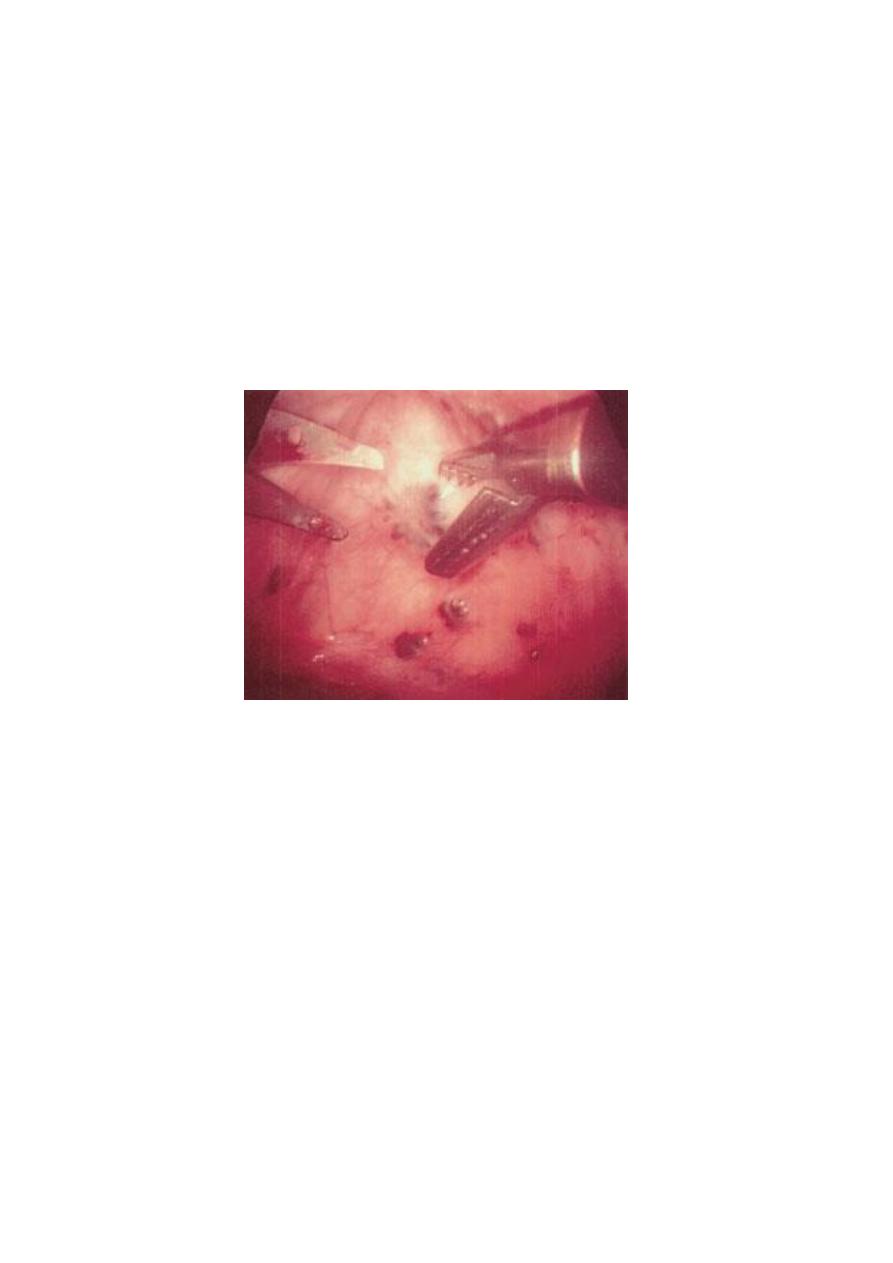
the gross appearance of "powder burns". Small foci are seen here just under the serosa of the
posterior uterus in the pouch of Douglas.
4. Combined Medical-Surgical Therapy
• Preoperative medical treatment by GnRH agonists or Danazol use in women with
advanced endometriosis as it can:
• decrease the extent of endometriosis, making it easier to achieve complete resection of
endometriotic implants by laparascopy is facilatated.
• decreases the size of endometriomas, which can facilitate surgery.
• Postoperative after conservative surgery giving GnRH agonists or Danazol to improve
patient outcomes.
Three outcomes are generally used to assess treatment efficacy:
1. the anatomic manifestation of the disease, can be assessed laparoscopically before
and after therapy to determine treatment efficacy.
2. pain symptomatology.
3. infertility status.
6
Endometriosis and pregnancy
• Pregnancy generally leads to an improvement in endometriosis symptoms, particularly
during the latter months of pregnancy (due to the high levels of progesterone and due
to lack of menstruation during pregnancy). However, some women experience a
worsening of symptoms, particularly during the first three months ( may be due to
rapid growth of the uterus lead to stretching and pulling of adhesions, may be due to
high levels of oestrogen).
• For most women, the beneficial effects of pregnancy are only temporary. Many
women will experience a recurrence of their disease and its symptoms within a few
years, and some will experience a recurrence soon after resuming their periods.
Endometriosis and breastfeeding
• Regular breastfeeding inhibits the release of oestrogen by the ovaries, which
suppresses ovulation and the growth and development of the endometriosis and lead to
remission of symptoms
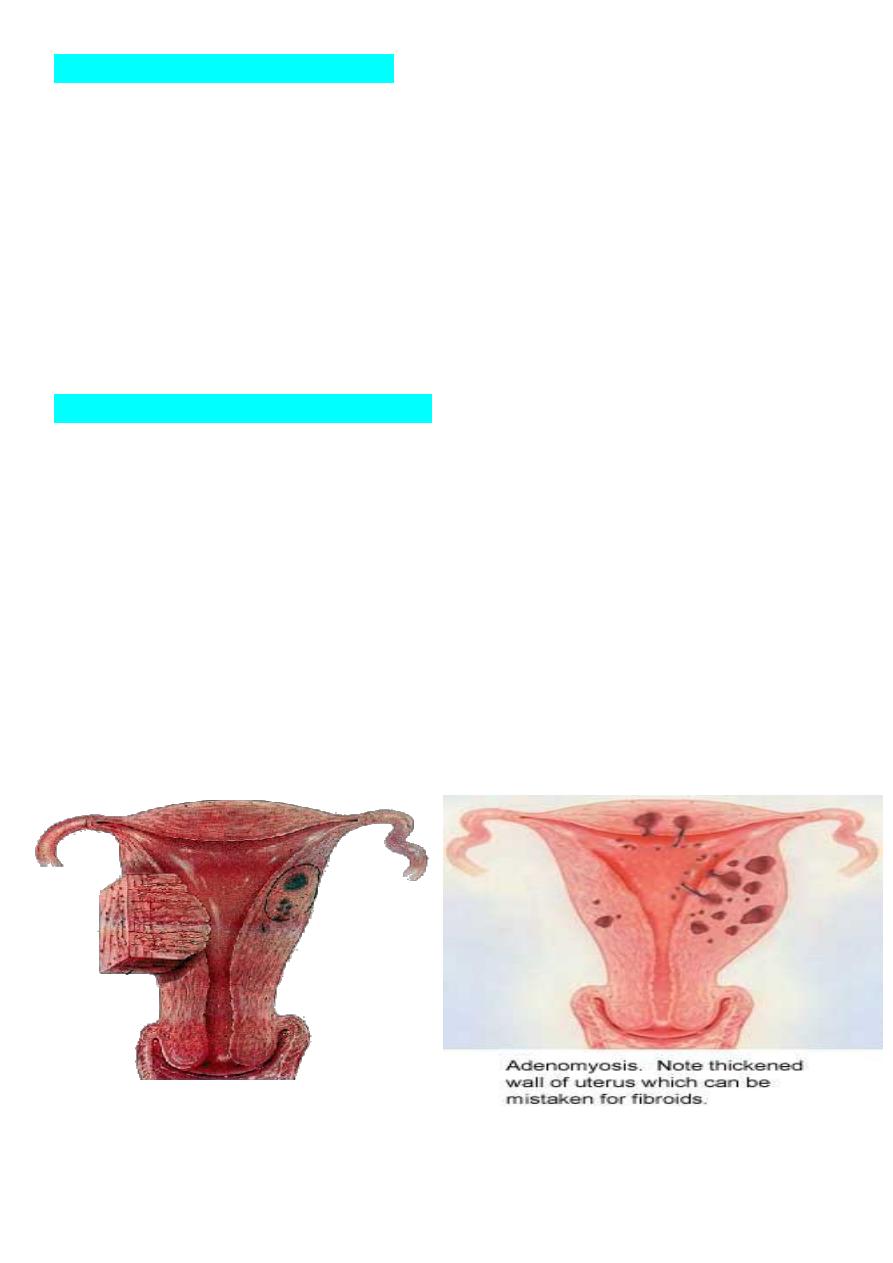
Adenomyosis
It is disorder in which benign invasion of endometrium into the myometrium. These
endometrium is responsive to steroid hormones and bleeding will occur each month.
7
Aetiolgy:
• Its cause is not known.
• It may be triggered by weakness in smooth muscle of myometrium by increased
intrauterine pressure or by surgical trauma as in repeated pregnancies, history of
miscarriage, induced abortion and caesarean section.
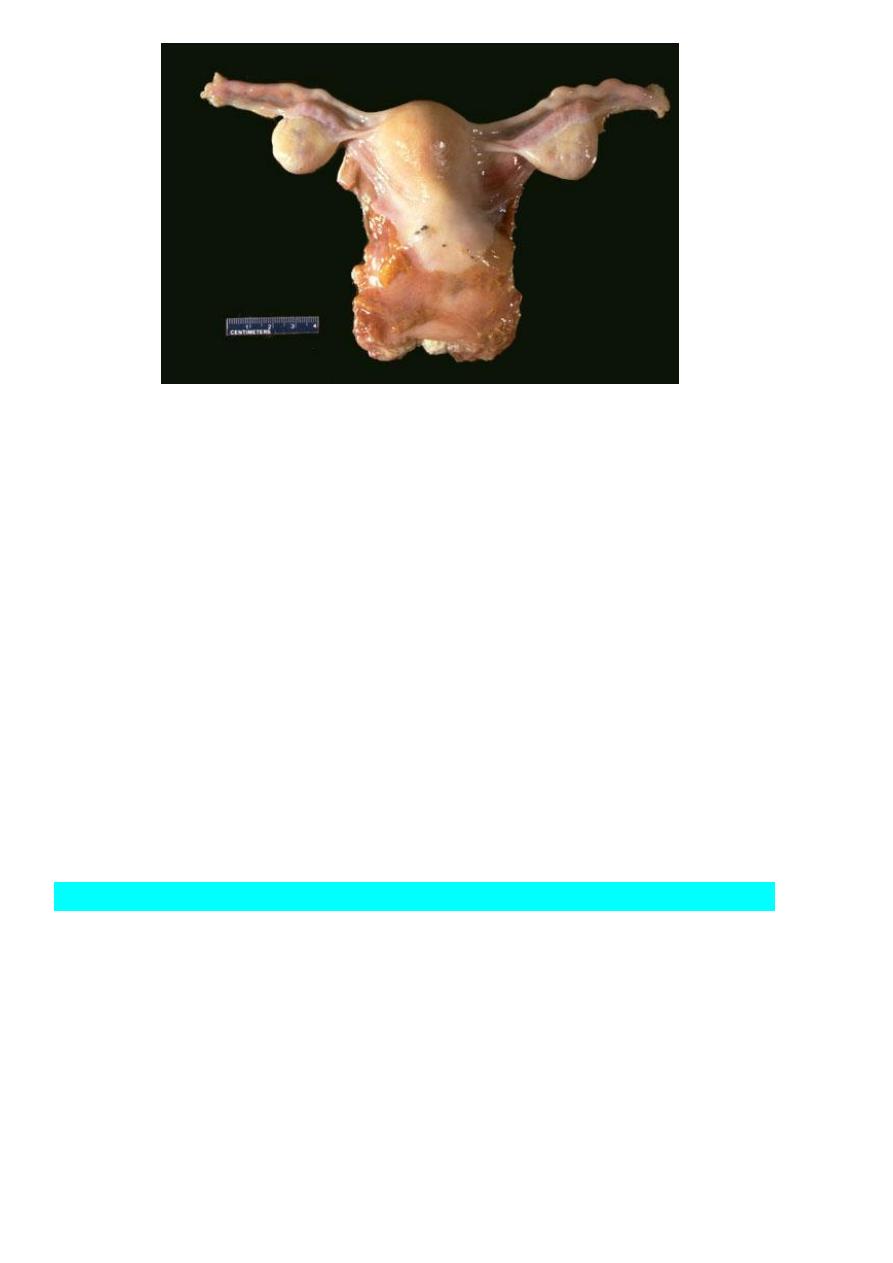
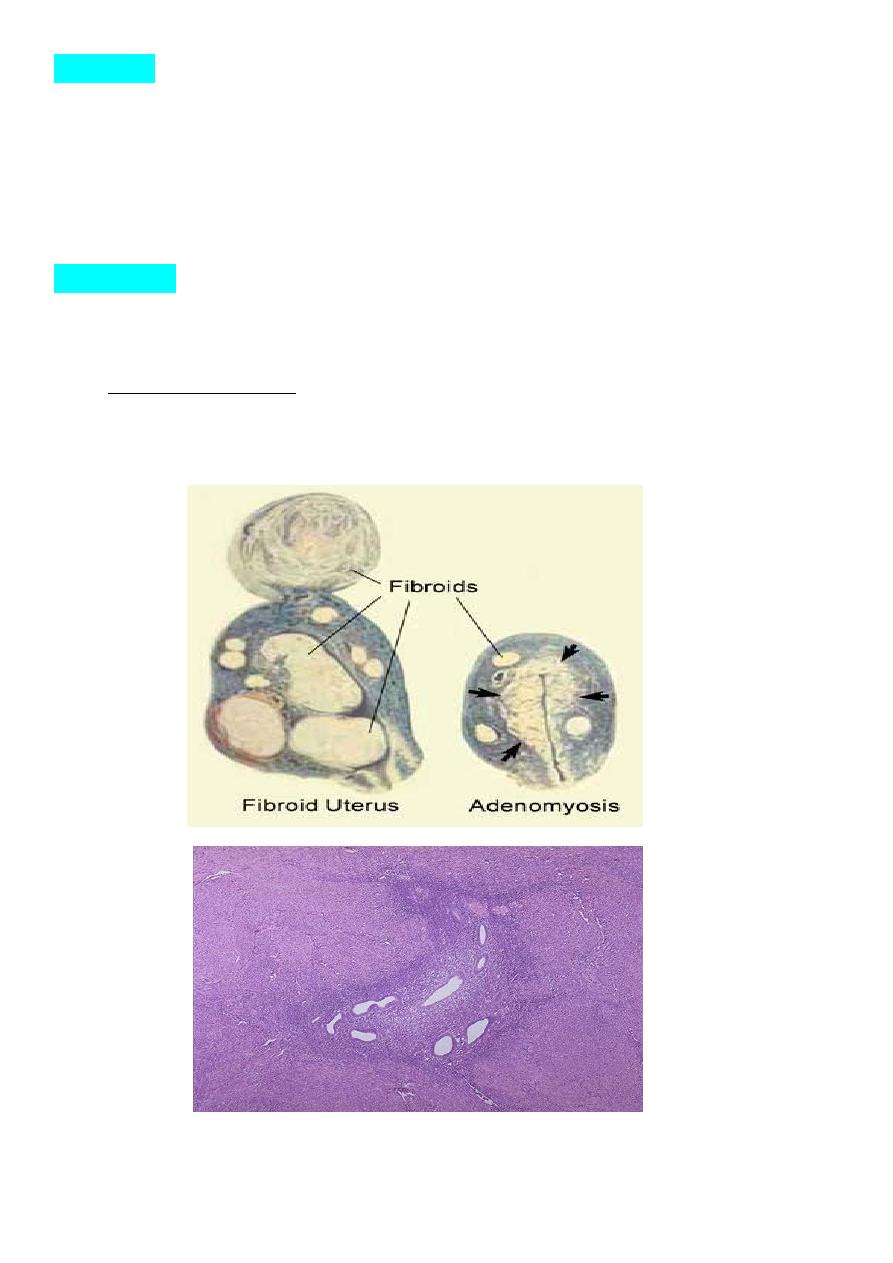
Pathology:
• Uterus uniformly enlarged (symmetrical enlargement).
• It causes localized thickening of part of uterine wall but this is not encapsulated and
can not be shelled out of the surrounding normal muscles (differ from uterine fibroid).
• Microscopically:glandular tissue and stroma in myometrium.
Adenomyosis occurs when endometrial glands and
stroma are found in the myometrium

8
The thickened and spongy appearing myometrial wall of this sectioned uterus is
typical of adenomyosis. There is also a small white leiomyoma at the lower left .
Clinical feature:
• Patients are usually multiparous and the age of 45 being the commonest age of
presentation and is very rare in nulliparous women.
• Many women are asymptomatic.
Symptomatic:
• The commonest presentation is that of menorrhagia associated with worsening
dysmenorrhoea (increasingly severe secondary dysmenorrhea). Patient may complain
from deep dysparunia especially pre-menstrually.
Pelvic Examination:
• bulky uterus , symmetrically enlarged.
• Some time tender if peri-menstrually examined.
Investigations:
*Ultrasound:
• transvaginal ultrasound which is primary modality as it shows Localized area in
endometrium.
*Magnetic resonance imaging (MRI):
• It is more accurate in diagnosing adenomyosis and can distinguish adenomyosis from
uterine fibroid.
*Histopathogy of hysterectomy specimen.

9
Treatment:
*Medical treatment:
• (non-steroidal anti-inflammatory drugs, combined oral contraceptives, high dose
progestrogens and the levonorgestrel-releasing intra-uterine system(LNG-IUS) are
helpful in relieve pain and excessive bleeding.
* surgical treatment
• Hysterectomy is the only method of curing the problem (without oopherectomy,
unless there are specific indications for removal of ovary).
• Endometrial ablation is relatively contraindicated since it will fail to remove deeply
infiltrating glands and is unlikely to be successful.
R
