
1
Fifth stage
Gynaecology
Lec-
د
.
اسماء
26/12/2016
Pelvic Inflammatory Disease
(PID)
Pelvic inflammatory disease (PID) is the term used to describe upper genital tract
infection in women.
Infection may involve the endometrium , with or without involving the fallopian tubes
,ovaries ,myometrium , parametrium and pelvic peritoneal space.
Its usually affecting non pregnant in reproductive age group (10%) and occasionally
pregnant women.
studies demonstrate the importance of pathogenic lower genital tract pathogen in the
development of PID its usually associated with sexually transmitted condition,and the
condition is usually polymicrobial
The organisms most commonly implicated are Chlamydia trachomatis, Neisseria
gonorrhoeae, mycoplasmas and mixed anaerobes.
True incidence is unknown due to non-specificity or lack of symptoms.
In UK about 2% of young women give history of PID.
PID is increasing because of the increase in gonorrhoea and chlamydia infection.
Pathophysiology of PID
A common cause of PID is from a sexually transmitted infection (the bacteria are passed
on during sex). A bacterium called chlamydia is the most common cause. Gonorrhoea is
another quite common cause of PID . A mixture of chlamydia plus gonorrhoea
sometimes occurs. mycoplasma species also common , these are recognised cause of
non gonococcal urethritis in male and females, these are STI with inoculation occurring
during intercourse , the bacteria can be in the cervix for quite some times without
causing symptoms before traveling into the uterus. That is why some women develop
PID weeks or months after having sex with an infected person.
Both C.trachomatis and N.gonorrhoea have well defined molecular virulance factors that
mediate genital attachment and cell damage. PID develops in 15-30% of women of
women with inadequately treated gonococcal and chlamydial cervicitis.
The largely asymptomatic nature of chlamydial cervicitis in female and urethritis in men
makes routine screening and treatment for chlamydia necessary for the prevention of
PID.
The most common microbial isolates recovered from patients at laproscopy or at
drainage of pelvic abscesses are endogenous lower reproductive tract or gastrointestinal
microflora,including E coli,bacteroids,prevotella species,G.vaginalis and anaerobic

2
streptococci ; these common sexually transmitted and endogenous agents should be
covered during antibiotics treatment.
Some cases of PID are not due to a sexually transmitted infection. The vagina normally
contains various bacteria. These are normally harmless and are not passed on by sexual
contact. However, these bacteria sometimes causes PID. This is more of a risk after
having a baby, or after a procedure such as an insertion of an intrauterine device (IUD).
Risk factors
Age < 25 (sexually active with thin cervical mucos)
Recent change in sexual partner.
Multiple partners.
Low SES and smoking.
Previous STI.
Lack of condom.
Preexisting bacterial vaginosis increase risk suggesting some synergy between the
different infection.
In addition to sexual transmission, PID may follow:
Intrauterine device (IUD) insertion.
Termination of pregnancy.
Post partum states.
Upper genital tract instrumentation.
There is evidence that immune response is genetically determined and increased risk of
PID is observed in women with HLA subtype A31 while HLA DQA 0501 and DQB 0402
have lower rate of infertility following diagnosis of PID.
Certain strains of bacteria are more likely to cause PID than others.
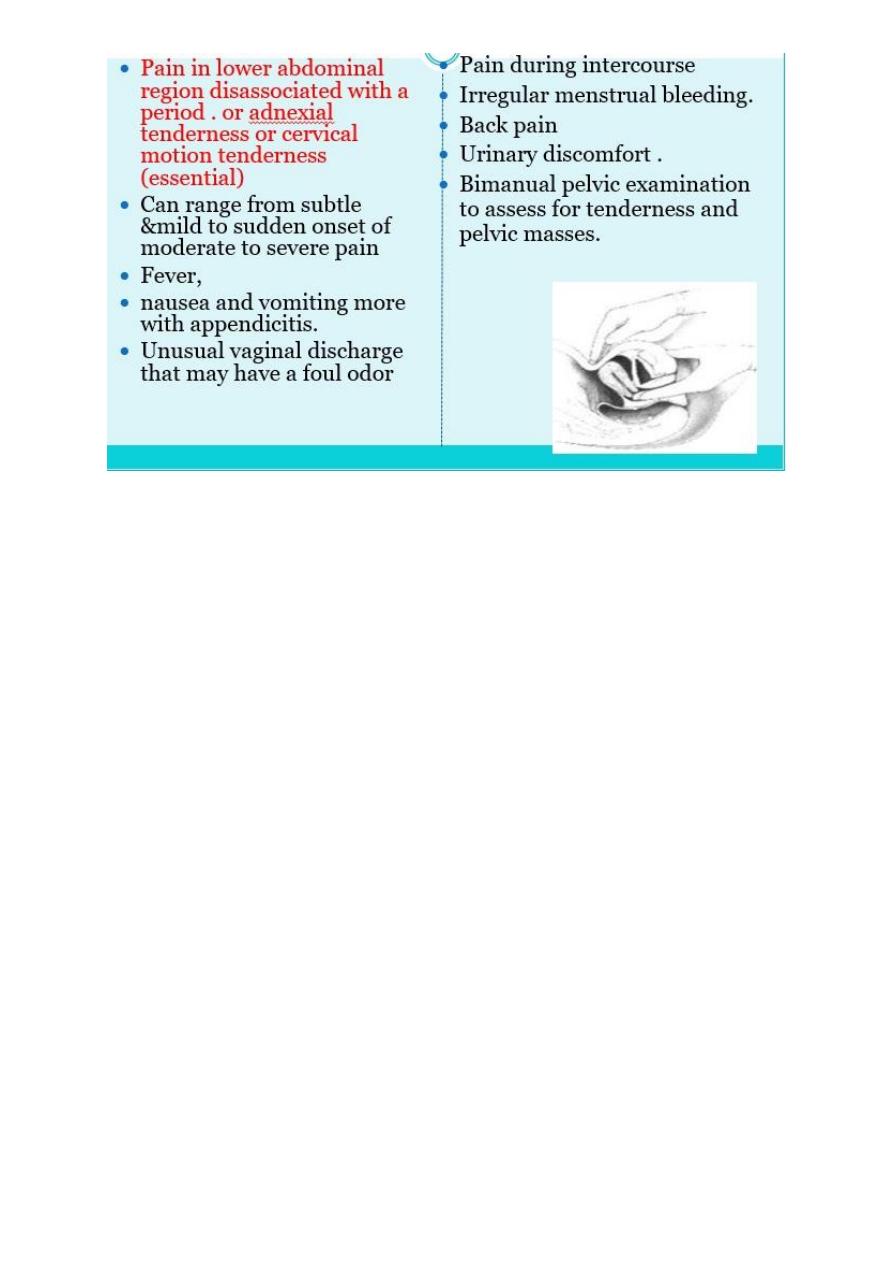
Symptoms and signs
Estimated up to 60% sub-clinical – that is may have no or minimal symptoms.
May present with lower abdominal pain, deep dyspareunia, discharge, chills and
fever. Less common is abnormal vaginal bleeding ,dysuria ,nausea and
vomiting….some women are asymptomatic.
On examination may have lower abdominal tenderness, cervical motion tenderness,
uterine and/or adnexal tenderness, mucopurulant cervicitis , fever is the least
common finding.
3
Complications
Tubo-ovarian abscess.
Chronic pelvic pain.,endometriosis and hysterectomy.(more)
Ectopic pregnancy (6x).
Premature delivery
tubal factor infertility(14x).
Perihepatitis (Fitz-Hugh Curtis syndrome) occurs rarely.
Diagnosis
Diagnosis is clinical, taking into account the history, clinical findings and
supplemental tests.
Diagnosis is often difficult because of variation in the presenting symptoms
No single laboratory test is diagnostic of PID and STI tests will often be negative.
A low threshold for diagnosis is appropriate in view of important sequel and
diagnostic uncertainty.
Result of PID
Can be life threatening.
Causes complications of conception, pregnancy, & fertility.
Inflammation of fallopian tubes.
Scarring of abdominal cavity tissue.
Scarring of fallopian tubes, causing blockage which can lead to ectopic pregnancy (tubal
conception).
Diagnosed women have 6-10 times increase of ectopic pregnancy.
Causes high pregnancy-related deaths among African American.
4
Initiate PID treatment for one of the following criteria: Pelvic pain: Uterine tenderness
OR adnexal tenderness OR cervical motion tenderness.
Additional supportive features :
Abnormal cervical or vaginal mucopurulent discharge.
Fever >38.3°C.
Elevated white blood cell (WBC) or CRP.
Presence of white blood cells on saline microscopy of vaginal fluid.
Confirmed infection with an STI or bacterial vaginosis.
Specific criteria for PID:
Endometrial biopsy with histological endometritis.
Transvaginal sonography and MRI indicating thickened fluid fulled tubes with or
without free pelvic fluid or tubo-ovarian abscess.
Laparoscopic abnormalities consistent with PID ; It’s invasive procedure only used if
the diagnosis is in doubt or if the patient not respond to treatment with in 24-72
hours when the diagnosis is clear and a sample for culture can be taken as the
accurate causative bacteria is different from that isolated from the endocervix.
Differential diagnoses
The main differential diagnosis to consider are:
Pregnancy complications, e.g. ectopic, spontaneous abortion.
Appendicitis.
Endometriosis.
irritable bowel syndrome.
complications of an ovarian cyst i.e. rupture, torsion.
functional pain (pain of unknown physical origin).
Diagnostic tests
All women with suspected PID should have a full evaluation for STIs including:
Endocervical swab/s for chlamydia and gonorrhoea testing.
A high vaginal swab for bacterial vaginosis and trichomoniasis.
Urine pregnancy test to exclude ectopic pregnancy.
Consider FBC (leukocytosis in pyogenic and sever infection) ,ESR and CRP.
Serology for STI; hepatitis B, syphilis and HIV and culture for trichomonas vaginalis is
recommended.
Pelvic ultrasound studies:enlarged swollen fallopian tubes as well as cul-de-sac fluid.
Laparoscopy is invasive ,and costly and effective empiric antimicrobial therapy is now
available these eliminate the need for laparoscopy use for diagnosis only used for
differentiation from other processes like appendicitis

5
Management
– Assess for PID severity (mild, moderate or severe).
– Treatment should cover for infection with gonorrhoea, chlamydia and anaerobes.
– Patients with severe infection, pregnancy or a suspected tubo-ovarian abscess require
gynaecology referral.
– Unwell patient require rest .
– Most patients are managed as out patient .
– Admittion to hospital is indicated if diagnosis is in doubt, if sever symptoms as acute
abdomen ,and if i.v. antibiotics are required.
Treatment regimens:
For Mild/moderate PID : Few regimens provide >90% efficacy.
Regimen 1 : Ofloxacin 400 mg BID plus metronidazole 500mg BID each orally for 14
days.
Regimen 2 : Ceftriaxone 500mg im stat PLUS Doxycycline 100mg twice daily orally for
14 days PLUS Metronidazole 400mg twice daily orally or for 14 days.
Note
o Advise to abstain from sex until abdominal pain has settled and to use condoms until
7 days after all sexual contacts have been treated.
o Metronidazole may be discontinued if not tolerated.
o The regimen may be used for mild penicillin allergy.
o Contraindications to administration of ceftriaxone are cephalosporin allergy or
previous severe penicillin allergy such as anaphylaxis.
For inpatient treatment:
Regimen1 :
Cefotetan 2 gm iv every 12 hours or
Cefoxitin 2 gm iv every 6 hours ,plus
Doxycycline 100 mg BID orally or iv for 14 days,
Add clindamycine or metronidazole for more anaerobic coverage.
Concerns about poor compliance :
Ceftriaxone 500mg im stat PLUS
Azithromycin 1g on day 1 and day 8.

6
Note:
o There is insufficient data on long term efficacy to recommend for first line use.
o The regimen may be used where there are concerns regarding ability to abstain from
alcohol during treatment.
For IUD users:
Evidence suggests PID treatment is not hindered by the presence of an IUD.
The decision as to whether or not an IUD should be left in situ should be made on a case
by case basis in consultation with the patient.
If the IUD is removed, recommend delaying this until approx 24 hours into antibiotic
therapy .
If there is inadequate clinical response at review, IUD removal should be considered.
“Management of sexual partners/contacts”
o A significant proportion of PID is caused by chlamydia. It is often passed on during sex.
o Men often have no symptoms with chlamydia, but can still pass on the infection.
o The test for chlamydia is not 100% reliable. Treatment makes sure that any possible
infection which may have been missed by the tests is cleared.
o If the sexual partner is infected and not treated, chlamydia may be passed back again
after you are treated.
o Perform a full sexual health check
o Do not wait for test results – treat empirically with azithromycin 1g stat.
o If gonococcal infection is suspected then add ceftriaxone 500mg im stat.
o Advise them to use condoms or abstain from sex for 7 days after initiation of treatment
until results of tests are available.
o If chlamydia or gonorrhoea positive – partner notification as above.
Follow-up
In mild PID, patients should be reviewed in 1 week and pelvic examination repeated
to confirm resolution of signs and review results.
In moderate PID, patients should be reviewed in 48-72 hours and if not improving
consider gynaecological referral.
Repeat a sexual health check 3 months after treatment.
About 1 in 5 women who have PID have a further episode. This is usually within two
years.
7
Reasons why this may occur include:
– If the sexual partner was not treated. You are then likely to get the infection
back again.
– If the patient did not take the antibiotics properly, or for long enough. The
infection may then not clear completely, and may flare up again later.
– If there is change in the sexual partner.
Some women are more prone to infection once their uterus or fallopian tubes have
been damaged by a previous episode of PID.
Outcome of PID
Difficulty becoming pregnant (infertility). PID can cause scarring or damage to the
fallopian tubes. This can occur whether or not the PID caused symptoms.
An increased risk of an ectopic pregnancy if you become pregnant. (This is a pregnancy
that develops in a fallopian tube and can cause serious problems.) Again, this is due to
damage to the fallopian tube by the infection. If you have had PID and become
pregnant, you have about a 1 in 10 chance that the pregnancy will be ectopic.
Chronic (persistent) pain develops in about 1 in 5 cases. This often includes pain during
sex.
The risk of developing some complications of pregnancy such as miscarriage, premature
birth, and stillbirth are increased in pregnant women with untreated PID.
Reiter's syndrome. This is an uncommon cause of arthritis and eye inflammation. It is an
uncommon complication of PID. It is thought to be due to the immune system 'over-
reacting’ to pelvic infection in some cases.
