
1
5th stage
Gynecology
Lec-3
Dr.asmaa
5/10/2016
Primary amenorrhoea
The student at the end of this lecture should be able to :
o
Define primary amenorrhoea.
o
Classify the causes of primary amenorrhoea.
o
Understand the changes of puberty.
o Exclude anatomical abnormality in patients with normal secondary sexual
characteristics.
Primary amenorrhoea
: is defined as absence of spontaneous menstruation by 16 years
of age in the presence of normal secondary sexual characteristics .
OR by 14 years of age when there is absence of secondary sexual characteristics (2
years of thelarche).
menstruation is not an event but part of the sexual development at the time of puberty ,it
occurs at any time between the10-18 years old .
NORMAL PUBERTY
:
Puberty is the time when one becomes functionally able to reproduce ,including both
physical and psychological development.
There is 5 changes (secondary sexual characteristics)these are the
:
1.breast growth.
2. pubic hair growth
3. axillary hair growth
4. growth spurt
5. onset of menstruation
later on ovulation become established
These changes occurs as a result of endocrine changes .
During childhood gonadotrophin levels are low both in term of pulse frequency and
amplitude ,then establishment of the mature hypothalamus and GNRH release leads to a
normal endocrine environment.
2
Oestradiol start to rise from the developing ovarian follicles, this oestrogen leads to
secondary sexual development of the breast and establishment of menstruation.
The secretion of androgen, (DHEA) and (DHEAS) begins from the age of 6 years prime
the development of pubic and axillary hair growth.
Clinical classification of primary amenorrhea:
A) Primary amenorrhea with sexual infantilism.
B) Primary amenorrhea with breast development and mullerian anomalies.
C) Ammenorrhea /oligomenorrhea with breast development and normal mullerian
system.
A)Primary ammenorrhea with sexual infantilism
Hypogonadotrophic causes (low FSH)(LH is low) (oestrogen low)
-Failure of GnRH secretion from the hypothalamus.
-Failure of FSH secretion from the anterior pituitary.
It may result from serious causes as CNS tumors ,kallman syndrome , prolactin secretin
tumor or general process of pituitary failure
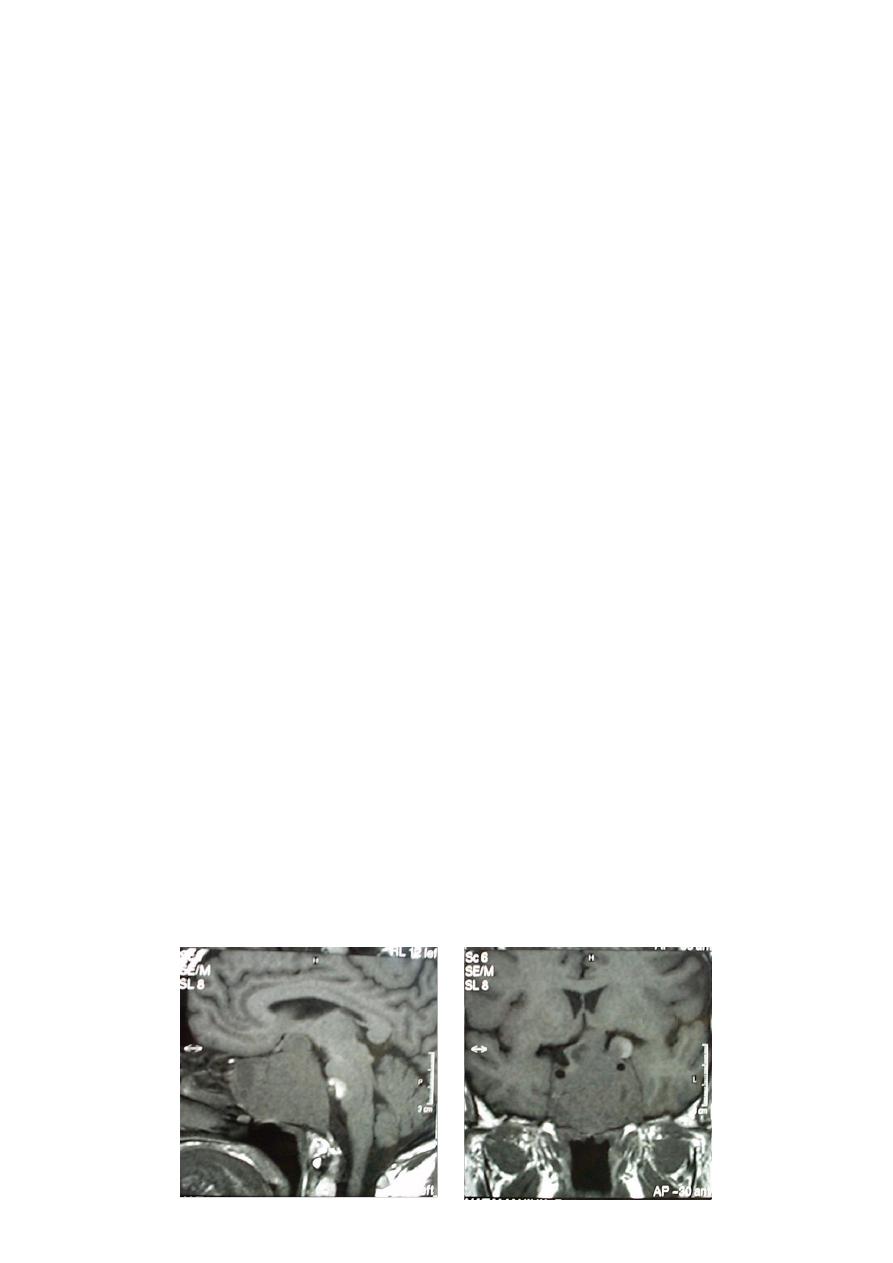
MRI,CT is adviced for diagnosisof tumor lesion and in addition of FSH measurement
we require TSH,GH,ACTH measurement.
Apparent hypogonadotrophic hypogonadism may actually represent constitutionally
delayed puberty due to undefined hereditary factors, there is commonly a history of late
puberty in family members.
Acquired causes of hypogonadotrophic hypogonadism
:
weight loss/ anorexia.
Exercise
stress
hyperprolactinaemia
17%of body weight is fat required for initiation of menarche, and 20% is required
to maintain menses.
The stress increase the level of circulating Endorphins can reduce the GnRH production
by the hypothalamus.
3
Hypergonadotrophic hypogonadisim
:causes (High FSH.LH) with low oestrogen
Result from congenital or acquired absence of ovarian follicles, causes includes:
Gonadal agenesis/ dysgenesis , including turner syndrome (45X0) and pure gonadal
dysgenesis(46XX,46XY),and mosaicism.
Most patient of this group will have no secondary sexual characteristics occasionally
patients with mosaicisim or turner syndrome will have sufficient ovarian follicular activity
and secrete oestrogen to cause breast development,menstruation,ovulation and rarely
even pregnancy .
In all patients Karyotype is required to exclude y chromosome as there is risk of
development of a gonadoblastoma: a benign germ cell tumor of the gonads , enentually
dysgerminoma a malignant germ cell tumor.
17-hydroxylase(p450c17) deficiency :
There is low sex steroid(oestrogen and androgen) there is hypertension and hypokalemia
due to mineralocorticoid excess. (excess aldosterone)
B)primary amenorrhoea with breast development and mullerian abnormality:
Patient in this group has 2 categories:
• Complete androgen insensitivity syndrome AIS.
• Mullerien dysgenesis or agenesis.
Differentiation between them is by measurement of serum testosterone level and by
determination of karyotype.
Androgen insensitivity syndrome:
There is defect in androgen receptor,their karyotype is 46XY and they demonstrate normal
level of testosterone although on the lower side of normal,they may also have mildly
elevated FSH and LH level because the testes are located in the abdominal wall cavity,with
greater temperature which is not allowing for normal male hormonal secretion. Breast
development is caused by small oestrogen produced by testes and by conversion of
androgen to oestrogen in the liver and else where.

4
The testes secrete normal amount of AMH so there is no uterus ,only a small vaginal
dimple.
Treatment:
gonadal resection to avoid neoplasia once puberty is complete.
Creation of neovagina.
Psychological counseling.
Mullerian dysgenesis or agenesis:
patient with primary amenorrhoea,breast development and 46XXkaryotype have level of
testosterone appropriate for females, amenorrhea occurs when the defect cause
obstruction of the vaginal canal like
1. Imperforate hymen
2. transverse vaginal septum
3. absent vagina and functioning uterus
4. absent vagina and non-functioning uterus
Heterosexual development:
• Congenital adrenal hyperplasia
• Androgen secreting tumors
• 5 alpha reductase deficiency
• True hermaphroite
• Absent mullerian inhibitor
Evaluation and management of primary amenorrhoea :
Most of condition are rare and constitutional delay is the most common diagnosis ,because
rest of diagnosis have serious implications diagnosis of constitutional delay should only
be made when all other syndrome have been excluded .
In
the female have normal secondary sexual characteristics ,
constitutional delay
no anatomical abnormality no endocrine abnormality only they have immature
pulsatile release of the GnRH. They will eventually menestruate spontaneously as the
maturation process proceeds.
5
If there is normal secondary sexual characteristics,check for anatomical
abnormality:
IF the uterus is present , then check for out flow tract Obstruction by:
examination
US
MRI or CT scanning
Treatment is by pelvic reconstruction surgery.
IF the uterus is absent check the karyotype:
If 46XX, Rokitansky syndrome is the most likely diagnosis.
If 46XY, Xy female is the likely diagnosis which require surgical removal of the gonads
as the malignant potential is 30% in these patients
IF the anatomy is normal check the gonadotrophin and prolactin:
1. If LH:FSH ratio is elevated
<
<
<
PCOS
2. If increase PRL <<< prolactinoma
Treatment is by bromocriptine or surgery
3. if increase gonadotrophin <<< resistant ovary syndrome further diagnosis is by
ovarian biopsy
4. if decrease gonadotrophin Indicate constitutional delay :reassurance, annual review
, may induce one cycle by COCP
About 25% of patients with primary amenorrhoea with presence of breast and Uterus,
have:
elevated prolactin serum level.
No galactorrhoea.
radiological abnormality indicate the presence of pituitary adenoma

6
If serum prolactin is normal, differential Diagnosis will include:
PCOS
hypothalamic-pituitary dysfunction(exercise,anorexia)
premature ovarian failure
Absence of secondary sexual characteristics:
Measure the gonadotrophin:
Low <<< hypogonadotrophic hypogonadism
High <<< karyotype should be performed:
46XX in patients with premature ovarian failure, the resistant ovary syndrome or
gonadal agenesis.
46XY in 46XY gonadal agenesis or testicular enzymatic failure.
In patient with hypogondotrophic hypo gonadism treatment directed to:
Manage avoidable underlying problems.
In isolated GNRH deficiency replacement therapy (oestrogen and progesterone) to
induce secondary sexual characteristics development.
These patients can be informed that they are infertile and ovulation can be induced
by various fertility regimes
