1
Fifth stage
Gynaecology
Lec-
د.اسماء
26/12/2016
Premalignat disease of the cervix
Cervical cancer kills about 250000 women a year.
It’s the commonest cause of death from cancer in women .it’s the commonest after
breast cancer.
80% of cases are reported in developing countries.
In developed countries regular screening program has reduced the incidence of
cervical cancer.
Cervical cancer is a preventable disease because of:
1. There is usually a phase of premalignant intra-epitheilial neoplasia with long
natural history.
2. The cervix is a relatively accessible organ to examine.
3. simple test available for the diagnosis of the presence of pre-malignancy.
4. Treatment for pre-invasive disease is highly effective.
Premalignant disease of the cervix
1.cervical disease
2.Cervical intraepithelial neoplasia
(Cervical dysplasia)
Aetiology
Human papillomavirus (HPV) infection.
HPV Infection is a sexually transmitted infection spread by skin-to-skin contact during
intercourse (condoms do not protect from infections).
HPVs are a large family of over 100 different virus types with some (e.g. types 6, 11, 16,
18, 31, 33) having a preference for genital skin .
Where as types 6 and 11 cause genital warts cervical condylomata and low grade CIN,
types 16, 18, 31 and 33 have oncogenic, i.e. cancer-causing properties.
HPV infection is extremely common and in majority of cases will not lead to
development of cancer. Progression or regression depends on several factors that
interfere with the host's ability to clear the virus such as in.
2
Transplant patient.
HIV-Positive women.
Smoking. to be related to the immunosuppressive effects of nicotine derivatives
within the cervix which may act as a cofactor with HPV in triggering the development
of CIN.
Adolescent cervix is more susceptible to carcinogenic stimuli because of active
process of squamous metaplasia which occur within the transformation zone.
Squamous metaplasia is an physiological process but under the influence of HPV
,cellular alterations occurs that result into atypical transformation zone initiate CIN.
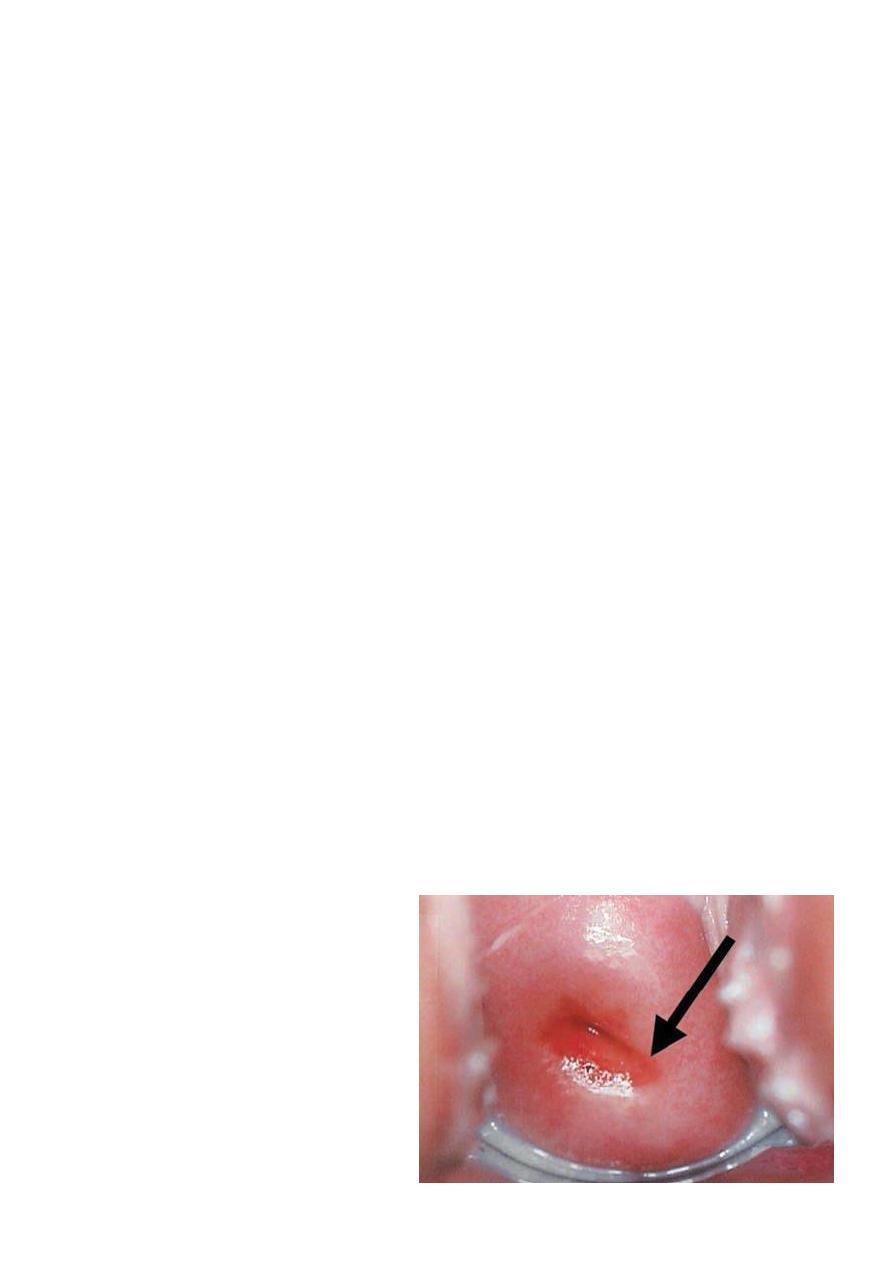
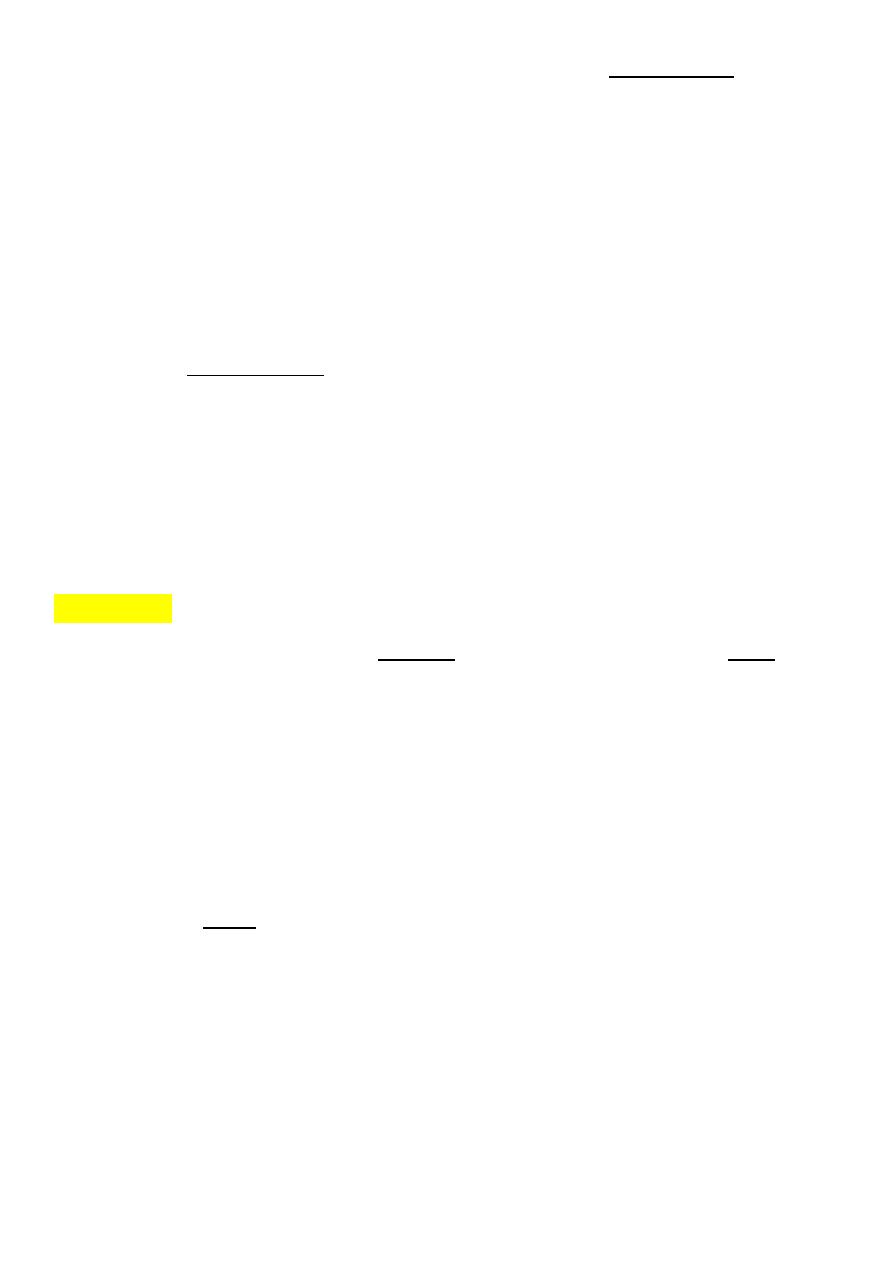
Normal cervix is lined by squamous epithelium in the vagina (ectocervix) and
columnar epithelium within the cervical canal (endocervix).
The meeting of the two types of epithelial is called the squamo-columnar junction
(SCJ) and this is usually at the ectocervix.
The position of the SCJ varies throughout the reproductive years. In children it lies at
the ectocervix, at puberty it extends outwards as the cervix enlarges and in adult life
it returns to the ectocervix through the process of metaplasia, which is a
physiological change from columnar epithelium to squamous epithelium.
The transformation zone is defined as the area where the original SCJ Was to the
current SCJ and it includes areas of metaplasia. Occasionally, When the mucous
columnar epithelium is covered by squamous epithelium
There is retention of mucus – this is called a nabothian follicle.
The transformation zone (TZ) is the site where premalignancy and malignancy
develop.
3
HPV infection can persist in certain individuals, and for reasons unknown (possibly
smoking) an oncogenic process can be triggered in the region of the TZ where
metaplasia occurs. Integration of the viral DNA into the basal cells of the cervical
epithelium in the TZ can lead to immortalization of the basal cells and rapid turnover
of the basal cells within the epithelium. This disordered immaturity within the
epithelium is called ‘cervical intraepithelial neoplasia’ and is truly an intraepithelial
condition (cancer is diagnosed when this process breaks the basement membrane).
CIN can be divided into
low-grade (CIN1) and high-grade disease (CIN 2 and 3).
Natural history of CIN
Regression and progression of CIN may occur.
Spontaneous regression of low-grade disease is not uncommon and is likely to occur
through the patient’s own cell-mediated immunity.
This is the argument for observational follow up in patients With low-grade abnormality.
High-grade disease is Less likely to regress spontaneously and requires treatment as there is
a risk of progression to cancer.
if high grade lesion is left untreated, around 20 % of patients may develop cancer of
the cervix.
Reasons for this remain unclear but may include reduced host immunity, oncogenic (cancer
causing) HPV types and smoking.
There is a convincing link between CIN and cancer of the cervix as nearly all microscopic
cancers of the cervix exist with CIN.
Screening for CIN
Cells exfoliated from the cervix can be Cytologically examined and act as a good screening
test
Screening for cervical intraepithelial neoplasia (CIN)
Medical screening method
Detect premalignant and malignant processes of cervix.
Prevent progression of abnormal cells to cancer.
This is NOT a diagnostic test!

4
Cervical cancer screening with cytology provides the opportunity for early effective
intervention and has reduced morbidity and mortality
Papanicolaou original use wooden spatula
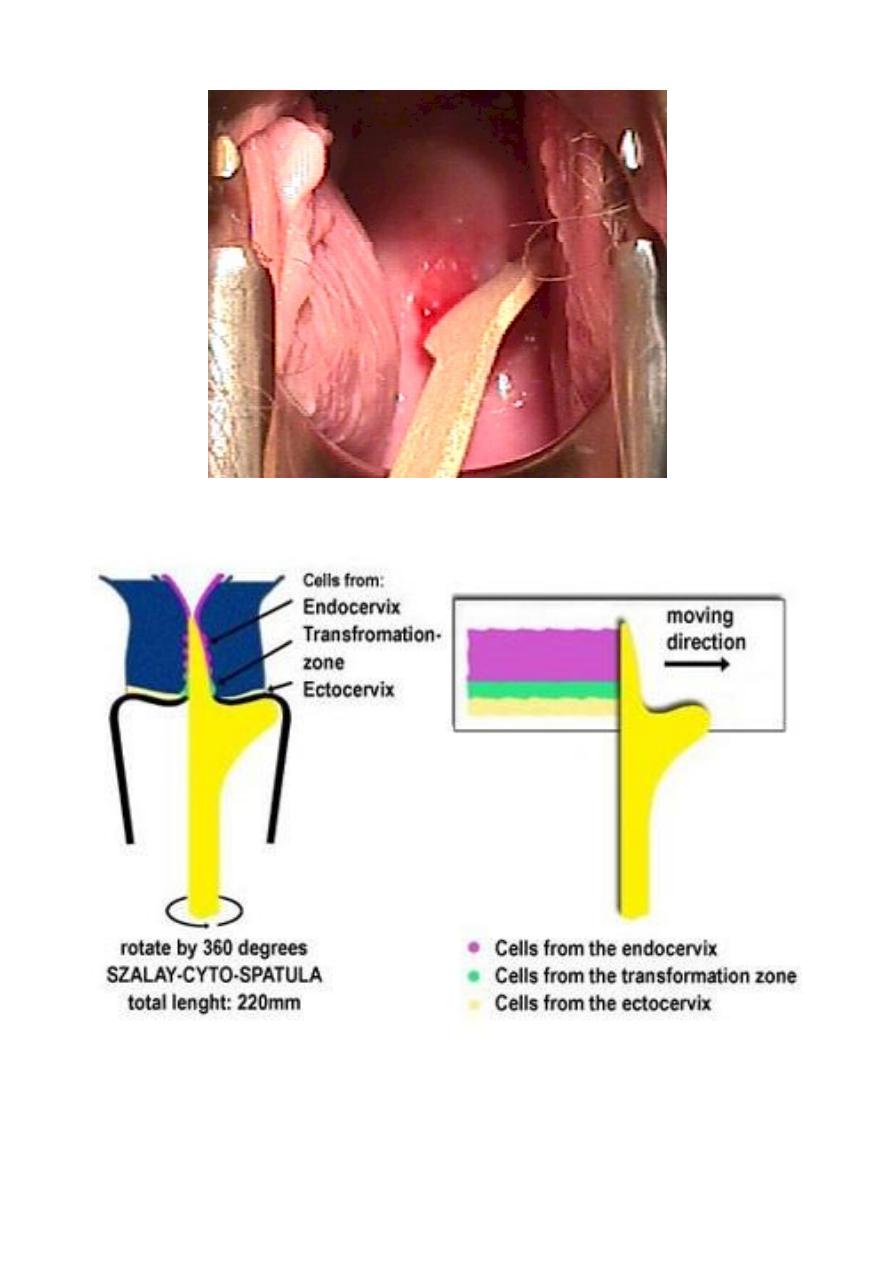
liquid-based cytology where a small brush is used to sample cells from the
transformation zone and the brush head placed in fixative.
Visual inspection with acetic acid (VIA)
Visual inspection with acetic acid and magnification (VIAM).
Colposcopy
Cervicography
Automated pap smears
Molecular (HPV/DNA) tests.
Co-testing using the combination of cytology plus HPV DNA testing is an appropriate
screening test for women older than 30 years (applied in some places).
An abnormal smear can show cells in different degrees of maturity (dyskaryosis). Like CIN,
cells can be classified as low grade (mild Dyskaryosis and borderline change) or high grade
(moderate and severe dyskaryosis)
There is some correlation between smear grade and the degrees of CIN on the
cervix, but it is not totally reliable Smears act as a means of referring patients to the
colposcopy clinic for further assessment.
The sensitivity of the cervical smear in picking up women with CIN is around 70 percent
;however, as there is slow progression for most women with CIN to cancer, if a lesion is
missed then this should be picked up on a subsequent smear.
5
Papanicolaou (Pap) smear test
Is a screening test for asymptomatic Women
to detect treatable pre-invasive squamous abnormalities of the Cervix
Small number of women will develop invasive Cancer
Not diagnostic-rather screening test to detect early changes on the cervix.
Exfoliative cervical cytology was a technique to collect the cells that had been shed
from the cervix.
It is a simple and painless test that may cause minor discomfort.
Cervical Smear aims to prevent cancer, not to detect cancer.
Cervical cancer screening should begin at age 21 years and not before age 21 because
it may lead to unnecessary and harmful evaluation and treatment in women at very
low risk of cancer.
Women who have been immunized against HPV-16 and HPV-18 should be screened
by the same regimen as nonimmunized women because it doesn’t prevent against all
high –risk HPV viral type.
frequency of cervical cytology screening
Annual cervical cytology screening is recommended for women aged 21–29 years.
Women aged 30 years and older who have had three consecutive cervical cytology
test results that are negative for intraepithelial lesions and malignancy may be
screened every 2-3 years.
6
women with any of the following risk factors may still require more frequent cervical
cytology screening:
• Women who are infected with human immunodeficiency virus (HIV)
• Women who are immunosuppressed (such as those who have renal transplants).
• Women who were exposed to diethylstilbestrol in utero.
• Women previously treated for CIN 2, CIN 3, or cancer (continue to have annual screening
for at least 20 years).
Pap Smear is not necessary in women in these categories:
1. Virgin patient.
2. Total Hysterectomy for benign disease.
3. Recent result of pap smear.
4. Age over 65 and over 10 benign Pap Smears.
Preparation
To prepare for the Pap test, for two days before the test ,women should avoid:
Vaginal Douching .
Using tampons.
sexual intercourse.
Using birth control foams, creams, or jellies or vaginal medications or creams.
the ideal time for a woman to have a Pap Smear is five days after her menstrual
period has ended.
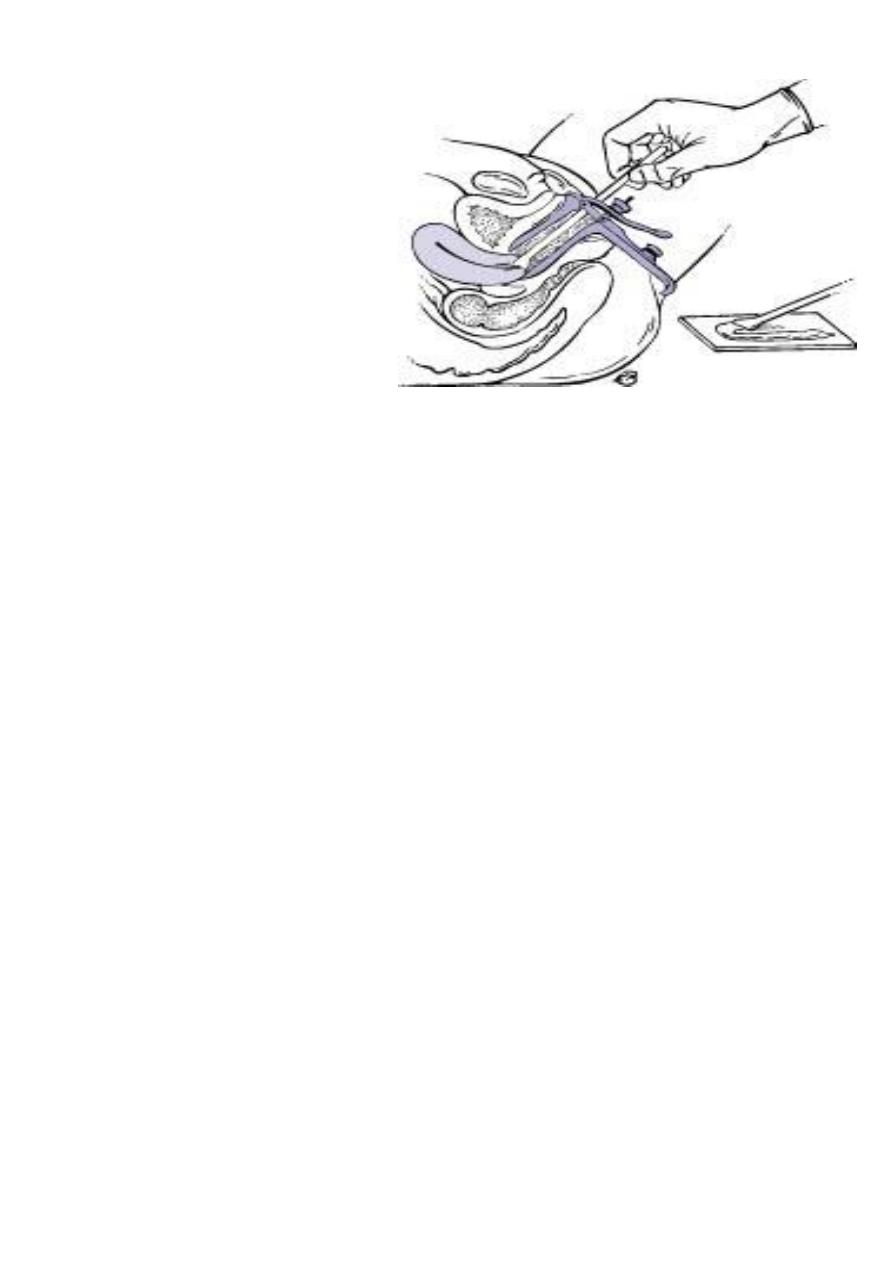
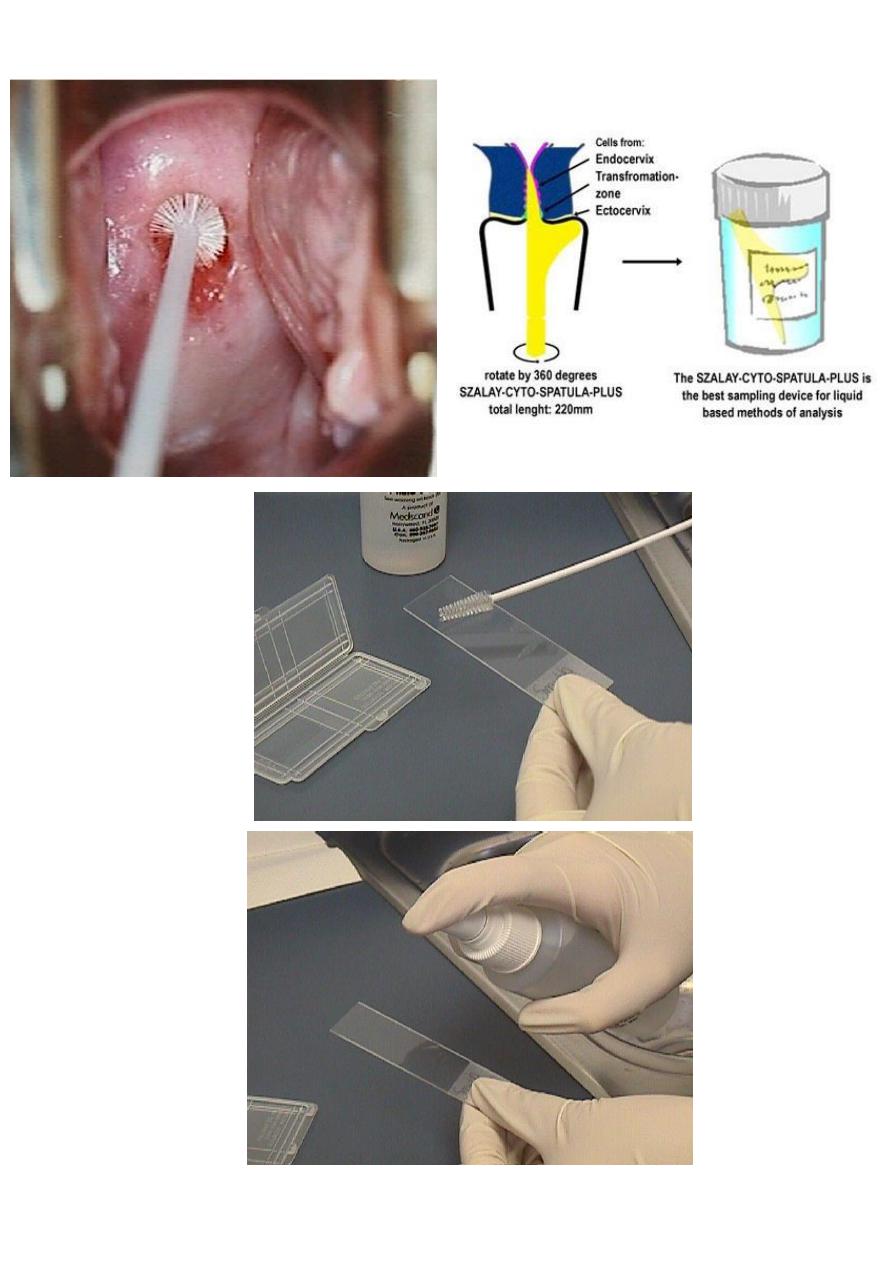
Exfoliated cells are collected from the transformation zone of the cervix by Use
spatula of different size or brush.
There are two methods of preparing and processing cervical smear slides.
These methods are:
1.
conventional cervical (Pap) smear test. collecting the cells smears on a microscope
slide and applies a fixative. The slide is sent to a laboratory for evaluation.
7

8
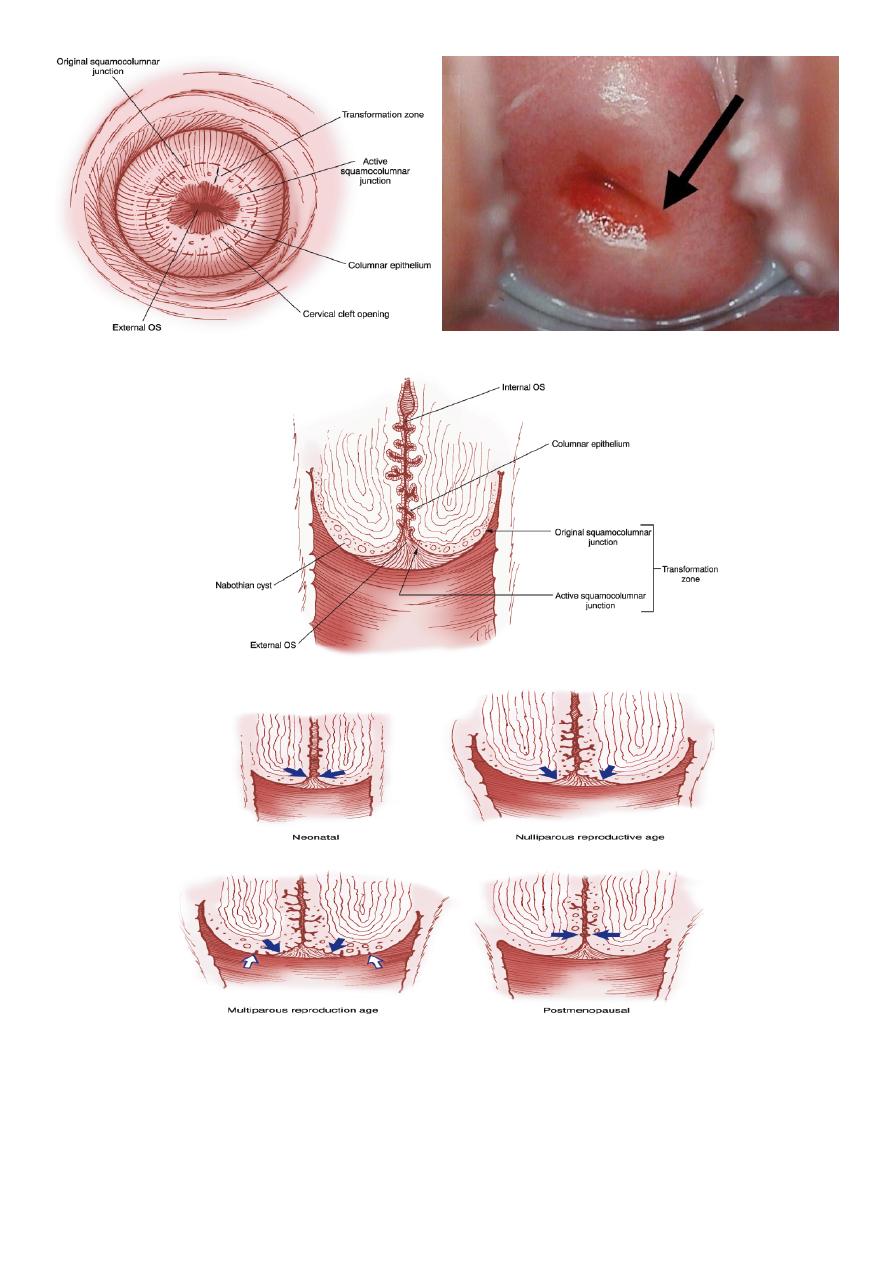
The Spatula with the optimal shape and size is chosen
Broom type sampler
The 'tongue' of the spatula is introduced into the canal, whilst its 'shoulder' is
positioned on the 3 o'clock position of the ectocervix at the beginning of the
procedure . With gentle pressure the spatula is rotated in a clockwise direction.
9
2.
liquid based cytology (LBC) test.
Cell transferred to a vial of liquid preservative that is processed in the laboratory to
produce a slide for interpretation by light microscopy.
10
