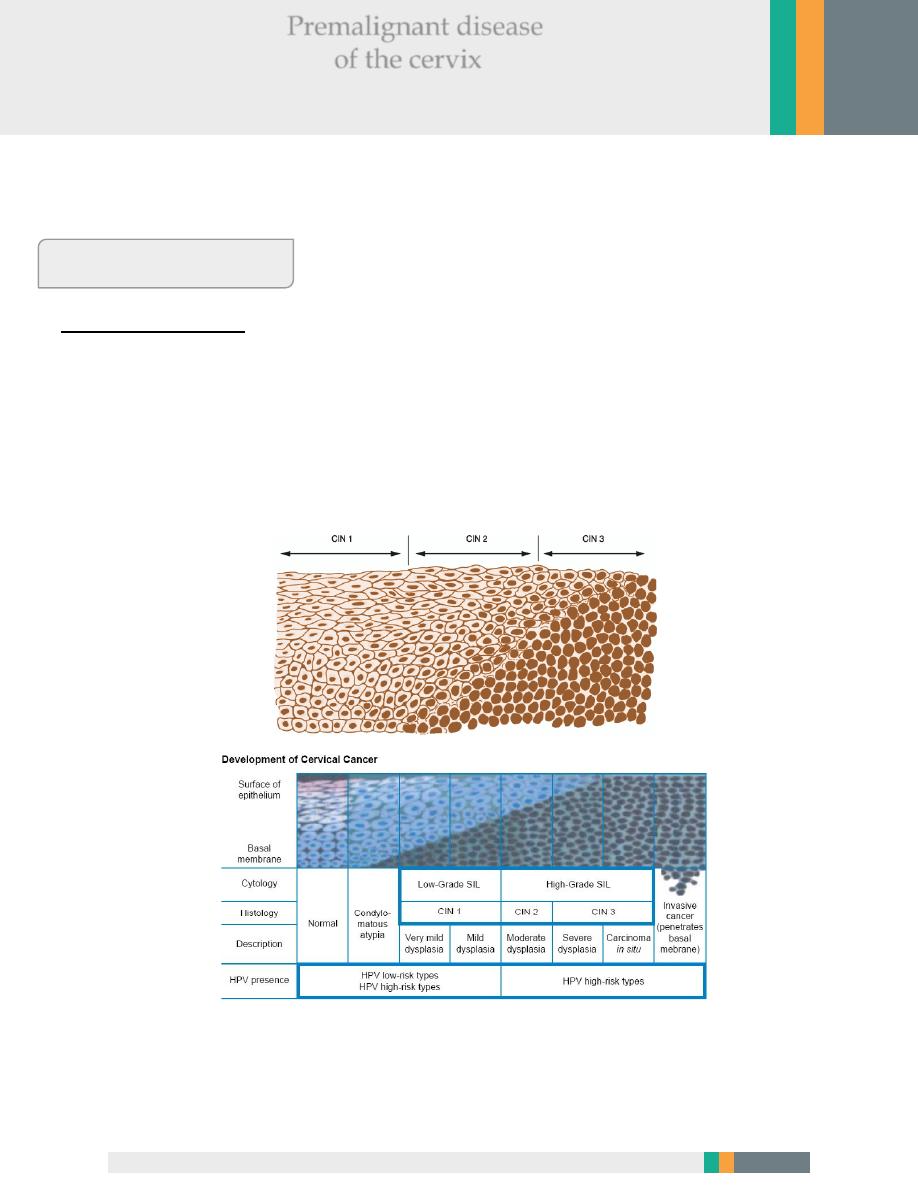
Classification of CIN
A. CIN classification
CIN 1 (mild dysplasia) involvement of the inner one-third of the epithelium.
CIN 2 (moderate dysplasia) involvement of inner one-half to two-third
CIN 3 (severe dysplasia/carcinoma in situ) full thickness involvement.
Diagram of cervical intraepithelial neoplasia compared with normal epithelium.
Gynecology Zakho hospital
Dr.Asmaa December 62, 2016
Cervical Intraepithelial Neoplasia
Premalignant disease
of the cervix
2
Or can be classified as:
*Low grade lesions (CIN1 and HPV-associated changes) in which there is a
significant chance of regression and low progressive potential.
*High grade lesions (CIN 2 and CIN 3) are likely to behave as cancer precursors.
A diagnosis of CIN is based primarily on the presence of nuclear a typia and loss of
normal squamous maturation (polarity).
Accurate grading of CIN lesions becomes important as we begin to understand
the rates of regression, persistence and progression of the low-grade (CIN 1) and
high-grade lesions (CIN 2 and 3), as their treatment and clinical follow-up are
quite different.
Cervical pre-cancer has along natural history.
36% of women with CIN3 would develop invasive cancer if left untreated.
More than 40% of women with minor cytological abnormalities will revert to
normal without treatment.
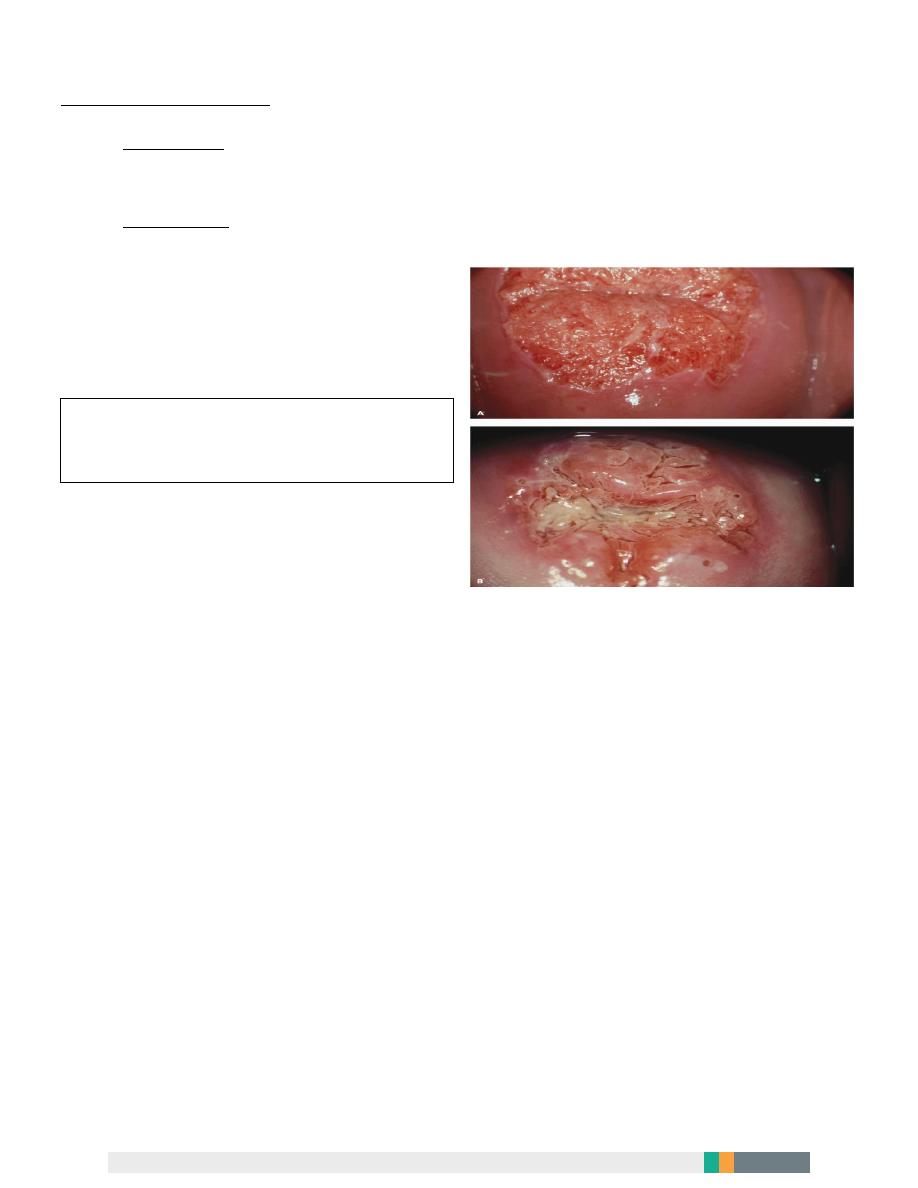
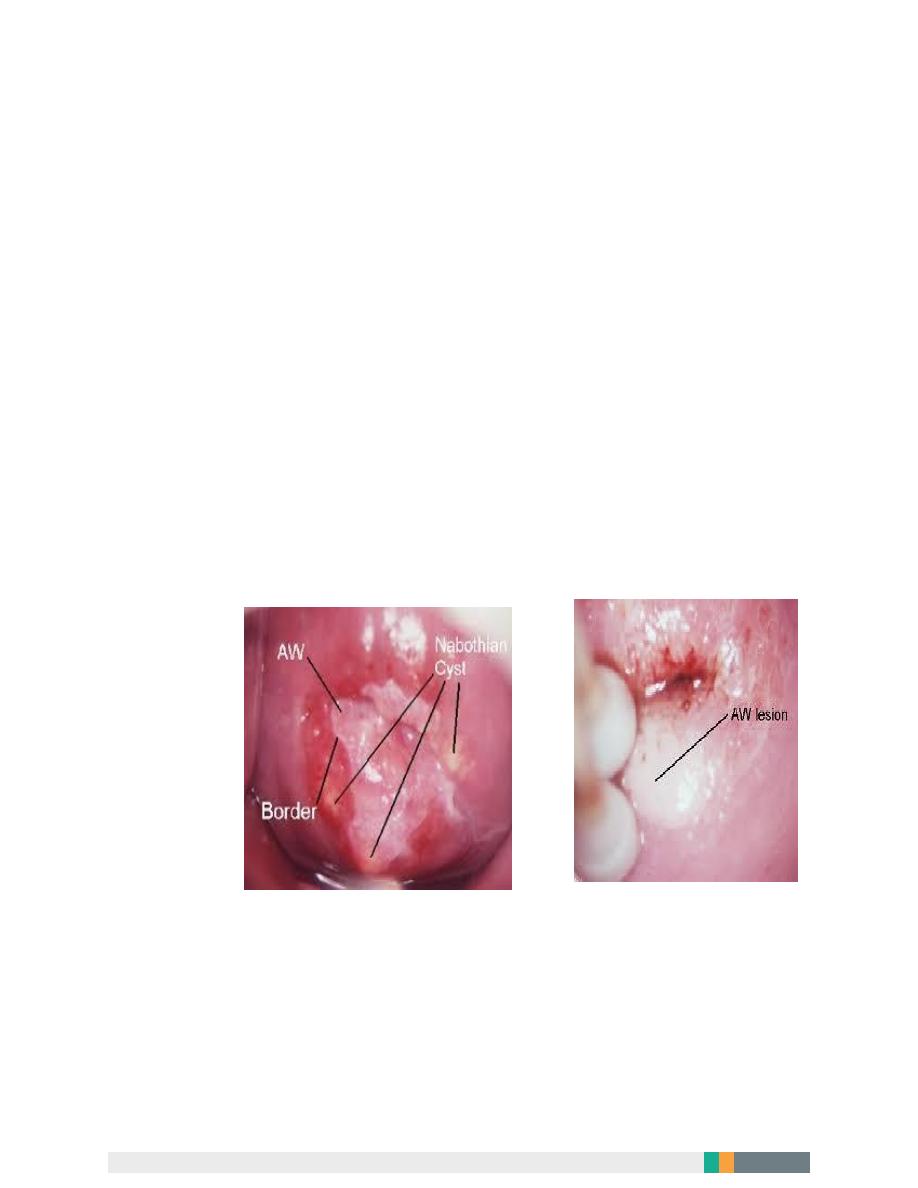
A: Active metaplasia in the transformation zone.
B: Maturing metaplasia in the transformation zone
3
Clinical presentation
The disease is a symptomatic.
The premalignant lesions cause no symptoms and are not recognizable with the
naked eye.
Results of the cervical smear test
The cytologist will classify the smear accordingly:
A. Normal results:
Mean that no atypical, dysplastic, or cancer cells were detected, and the cervix is
normal. It is seen in About 9 in 10 routine cervical screening tests.
(Note: a normal result means a very low chance of developing cancer of the
cervix - not a 100% guarantee that it will not occur.)
B. Abnormal result:
Some changes in the cells are found in about 1 in 10 tests. There is a range of
changes that may occur. In nearly all cases, these changes do not mean cancer.
Inflammatory –excessive leucocytes, candida or trichomonas.
C. Borderline.
(Cellular appearance that cannot be described as normal).
Mild dysplasia
Moderate dysplasia.
Severe dysplasia.
Possible invasive carcinoma. Rarely, a cancer of the cervix is diagnosed by a
cervical screening test.

4
Management of abnormal cervical smears
Inflammatory smears should be treated by antibiotics or antifungal agents
accordingly. And the smear repeated 3-6 months later.
Border line smear advice to Repeat smear in 6-12 months and refer for
colposcopy if abnormalities persist.
Ideally all women with abnormal cervical cytology (some mild ,moderate ,sever
dysplasia) should have colposcopic assessment to exclude an invasive process
and to identify the extent of abnormality.
Colposcope
5
Minor or borderline abnormal changes are quite common. These often clear away
on their own and most mild changes do not progress to anything serious.
However, any change needs to be monitored as some may progress to become
more serious in the future. A repeat test after 3-12 months is commonly advised,
depending on the type and degree of change. Often the changes will be resolved
when the test is repeated. If the changes don’t resolved or the changes are more
marked, then a referral to colposcopy is advised.
Any patient with a grossly abnormal cervix should have a punch biobsy
regardless of the results of Papanicolaou smear.
Inflammation
6
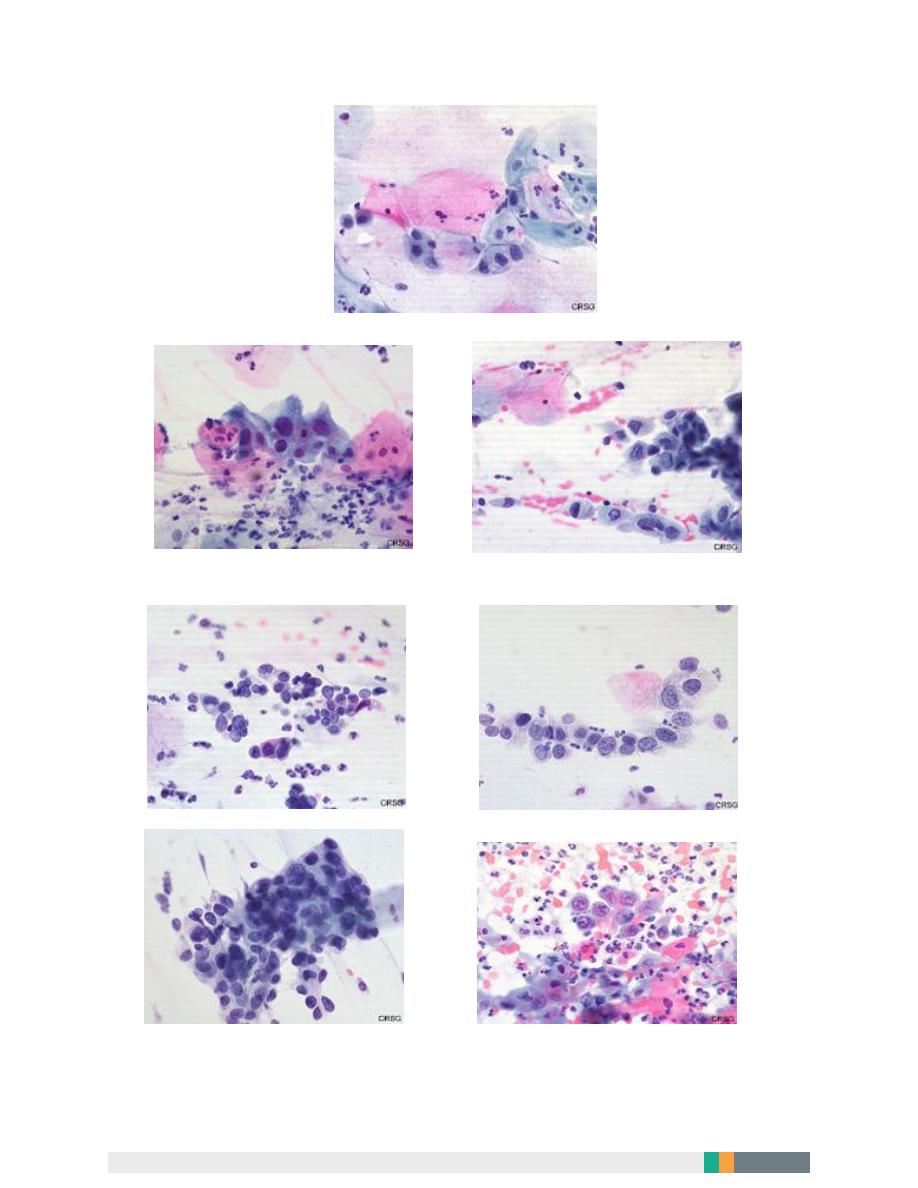
CIN1
CIN2
CIN3
CIN3 ca in situ Squamous cell carcinoma
7
CIN2
High Grade SIL
CIN1
Low grade SIL (L-SIL)
8
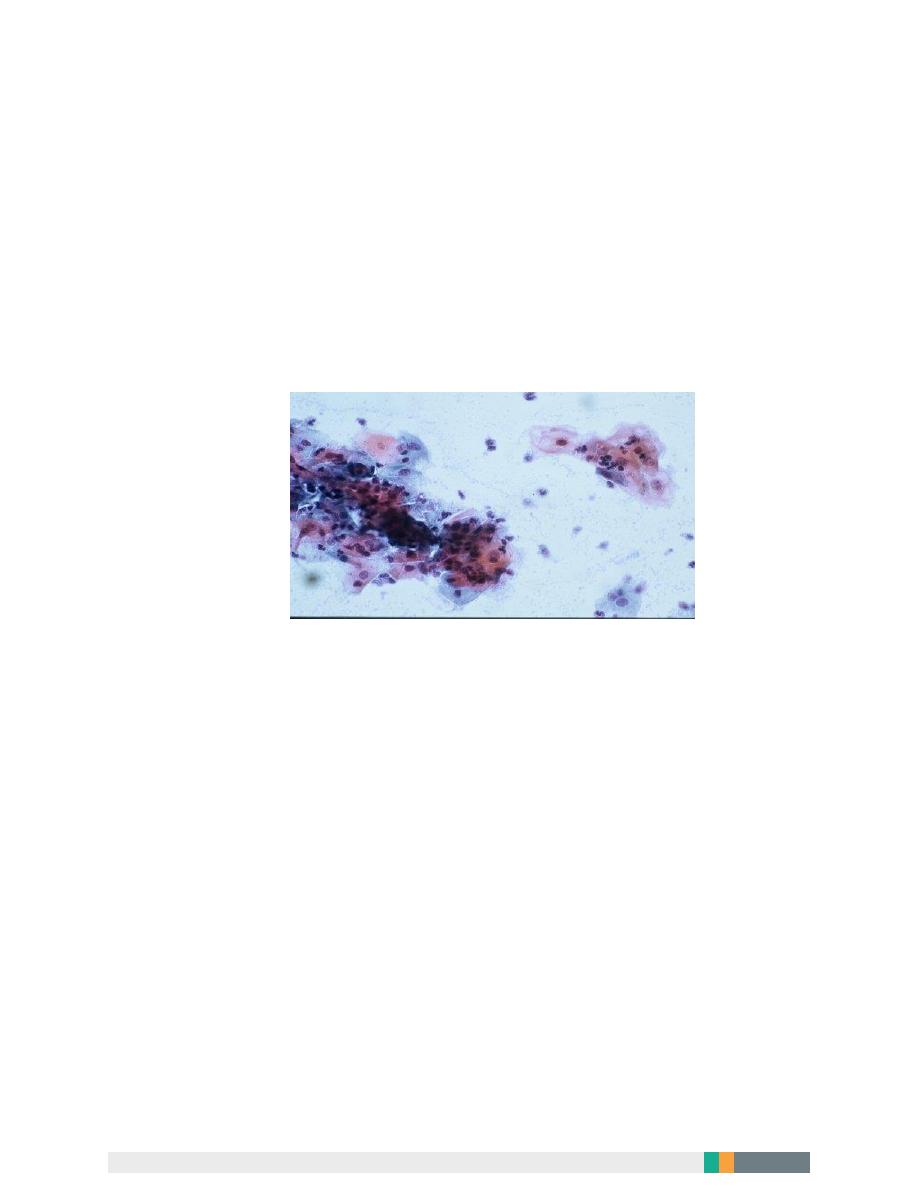
The cytologic features of normal squamous epithelial cells can be seen at the center top and bottom, with
orange to pale blue plate-like squamous cells that have small pyknotic nuclei. The dysplastic cells in the center
extending to upper right are smaller overall with darker, more irregular nuclei.
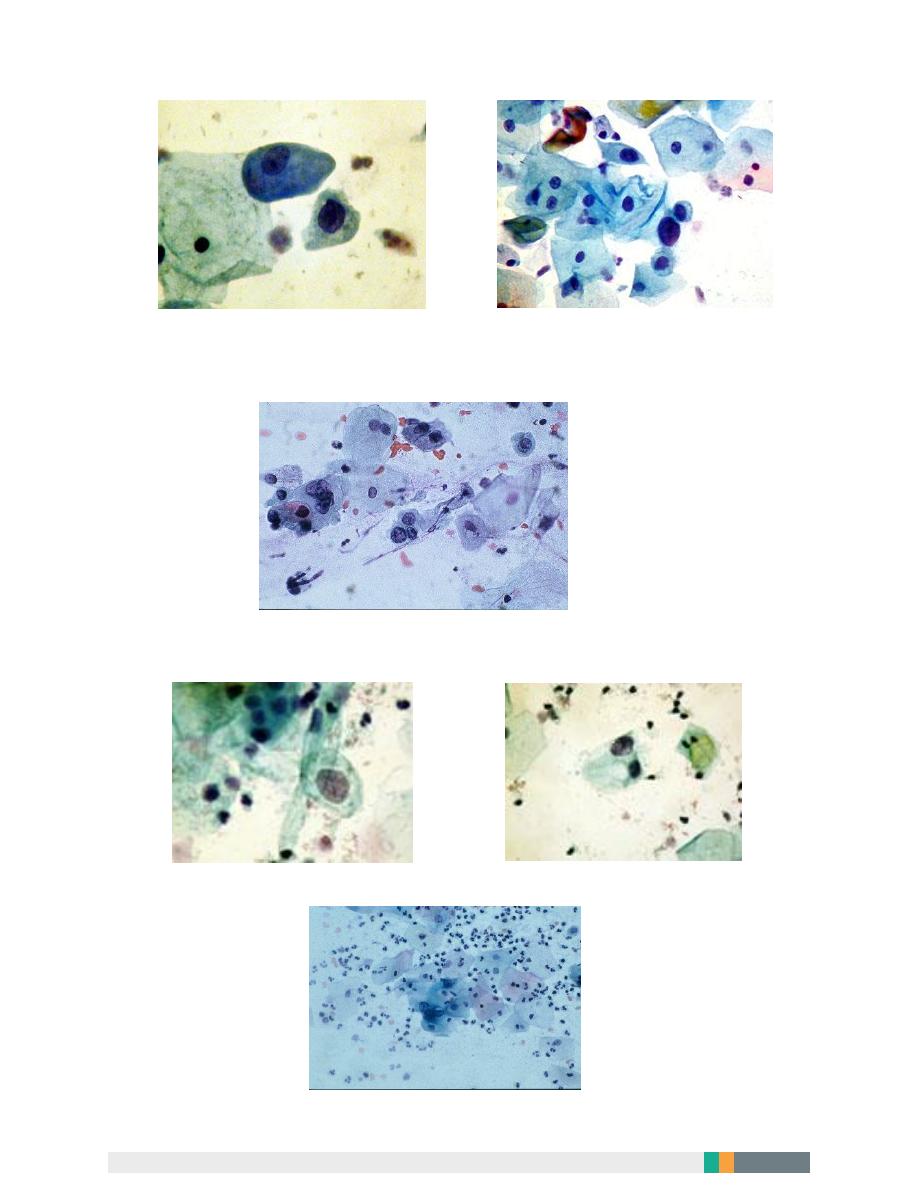
Gardnerella Vaginalis
Mixed bacterial flora
9
Candida
HERPS
10
Colposcopy:
It is a binocular operating microscope with magnification of 5-20 times. Indicated
for further investigation of smear abnormalities.
It has been used to examine the cervix in detail to:
a. Identify dysplastic abnormalities on the ectocervix.
b. Detect changes in the cellular pattern and vascularity of the covering
epithelium.
c. Allow the accurate localization of the abnormal epithelium.
d. Exclude an invasive process.
Colposcopic examination
We have two methods:
1. Saline method.
The cervix and vagina is moistened thoroughly with normal saline in order to view the
vascular pattern.
Gross lesion, vascular details and opacity of epithelium is noticed.
Green filter is used to evaluate the details of vascular epithelium when the blood
vessels appears dark.
Occasionally abnormal epithelium will stand out from The surrounding epithelium.
CIN has the potential to be an invasive malignancy but dose not have malignant
properties. High grade lesions (CIN2 and CIN3) should be treated, but there is some
debate about CIN1 they allow CIN 1 lesions to be treated or kept under close
surveillance.
11
2. Classical or extended method:
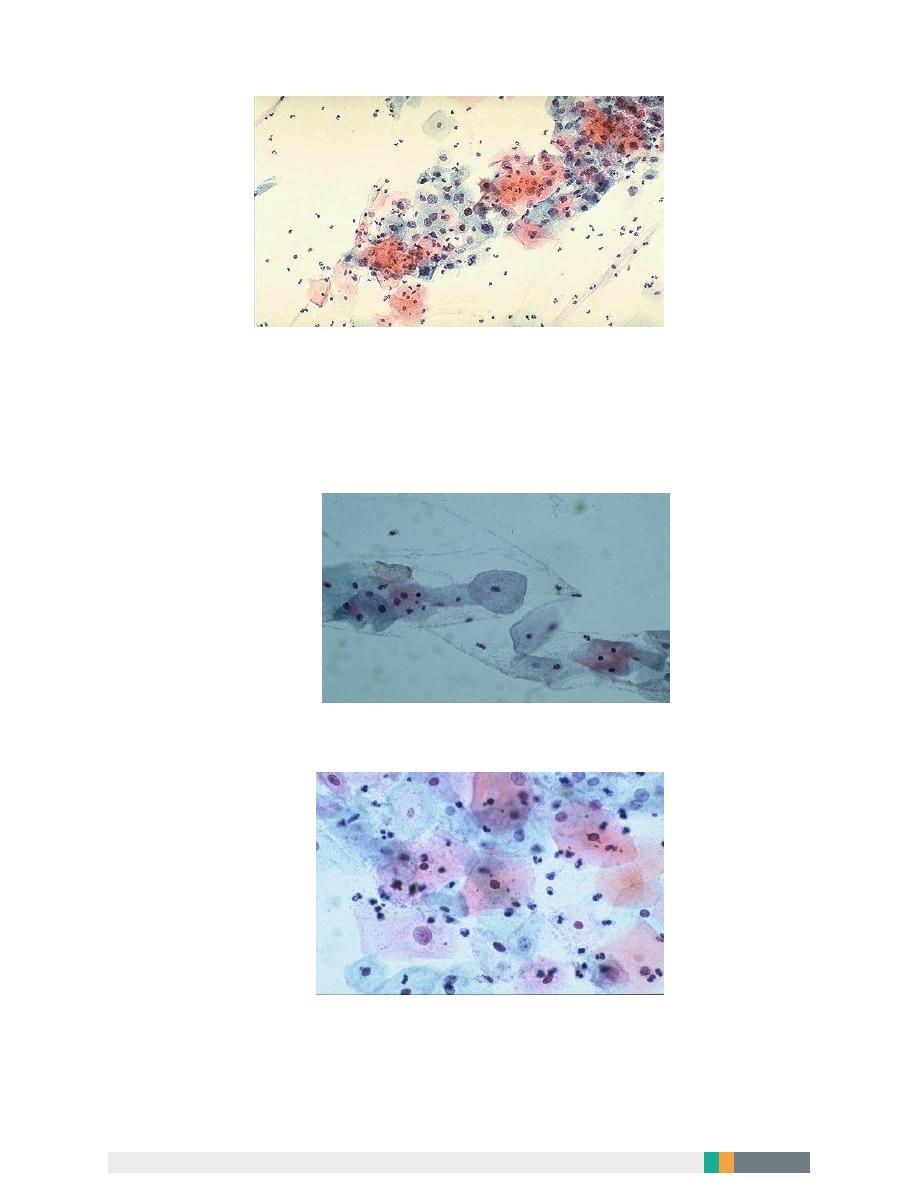
Acetic acid test :After removing the excess mucos , the cervix is liberally moist with a
large swab of loose cotton wool soaked in dilute acetic acid of 3-5%,by this all the
epithelia with high nucleo-cytoplasmic ratio will turn white. this action is transient and
disappear after 1-3 minutes, and it’s better to wait for at least a minute before
recording the acetowhite changes .
Satisfactory colposcopy :
The important part of colposcopy is to look for the entire sequaocoluminar junction
and one should be able to see the overlying columinar epithelium even if it’s inside the
cervical canal then to examine the vaginal fornices and walls.
Tissues with high nuclear activity and high nuclear-cytoplasmic ratio turn white after
application of acetic acid, the faster the aceto whiteness appears and the longer it
persist will reflect the degree of underlying abnormality and more likely to be high
grade intraepithelial lesion
Acetic acid test
Acetic acid test

12
Iodine test:
The cervix and vagina is liberally painted with iodine solution with 50% aqueous
solution because alcohol cause destruction of epithelium.brown staining will occur in
glycogen rich epithelium(sequamous epithelium).
Iodine negative areas occurs in :
Inflammation
Columnar epithelium.
Thin regenerating epithelium.
Immature metaplasia.
Atrophic epithelium
HSIL
13
Normal colposcopic finding
Original sequamous epithelium.
Pink smooth featureless on the cervix and vagina no Remnants of columnar epithelium
such as gland Opening Or nabothian cysts . it doesn’t turn white after acetic acid
applications and stain brown after application of lugol’s Iodine.Sometimes vascular
pattern as looped capillariesor as fine net work .
Treatment of CIN
The treatment for cervical dysplasia must be individualized for each woman,
taking into account:
1. The grade of the dysplasia (CIN1, CIN2, or CIN3).
2. The findings at colposcopy.
3. The woman's age.
4. Reproductive status.
5. And other factors.
Treatment for CIN include:
CIN has the potential to be an invasive malignancy but dose not have malignant
properties. high grade lesions (CIN2 and CIN3) should be treated, but there is
some debate about CIN1 as some allow CIN 1 lesions to be treated and others
advice to be kept under close surveillance
..

14
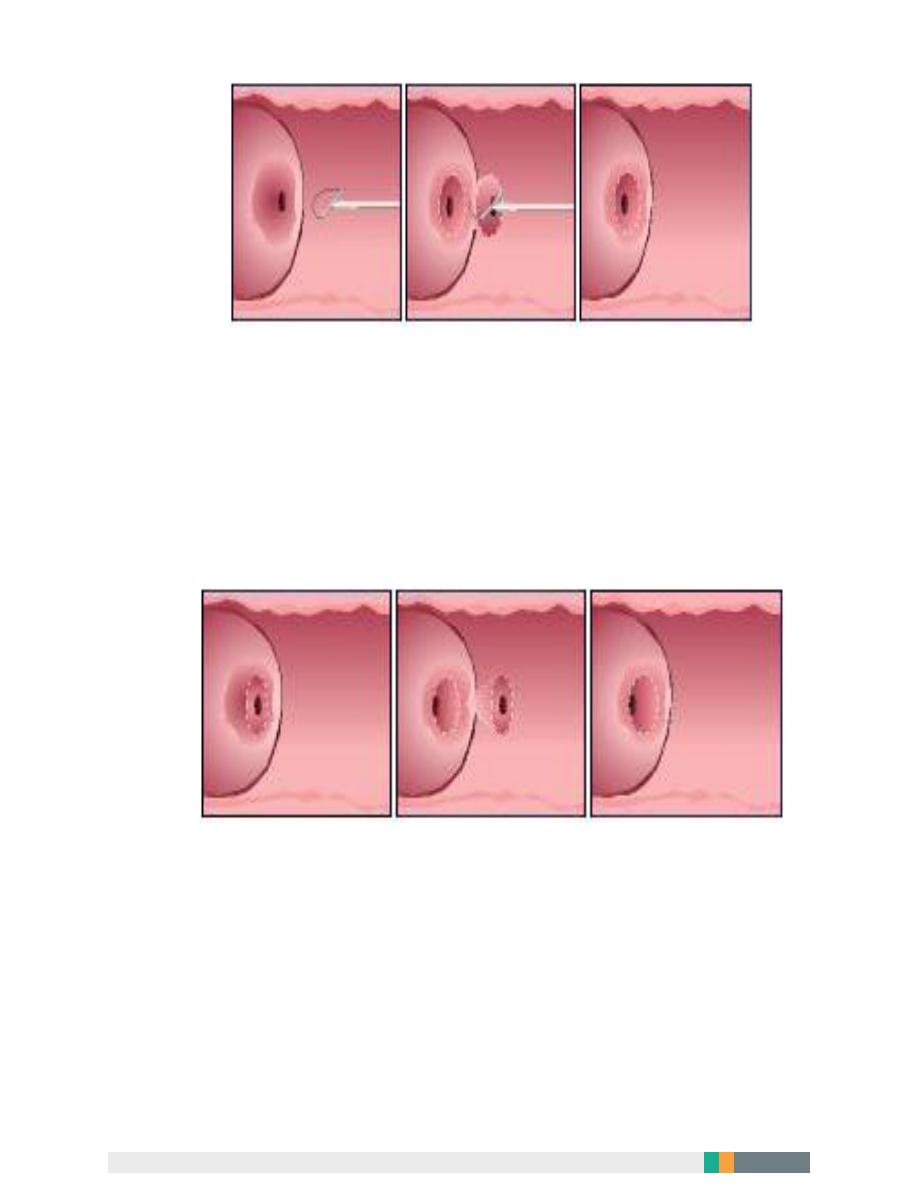
Treatment involves completely removing the abnormal epithelium.
This can be done by:
1
. Destroying the abnormal epithelium.( cryosurgery, laser vaporization)
2. Excisional techniques:(This allows better histopathological interpretation of the
excised specimen).
These techniques include:
local excision
Loop electrode excision procedure (LEEP).
Cone biopsy.
trachelectomy (excision of cervix).
hysterectomy.
The success of treatment is usually defined as negative cytology 6 months
following intervention.
Therapeutic vaccination aims to boost host's cell-mediated immunity but still
experimental.
Follow up:
Follow up of patient treated for CIN is controversial between colposcopy or
cytology. other tests such as a HPV DNA test may be advocated
15
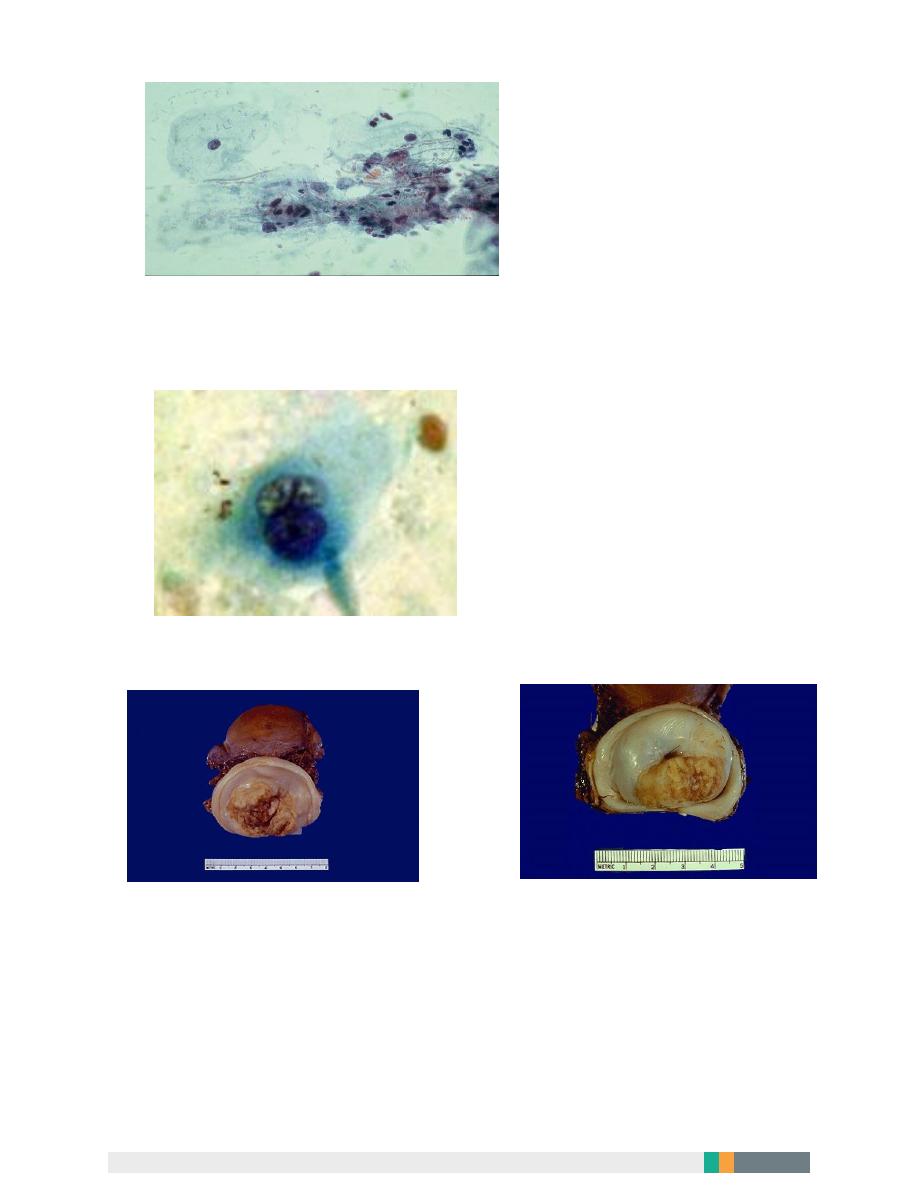
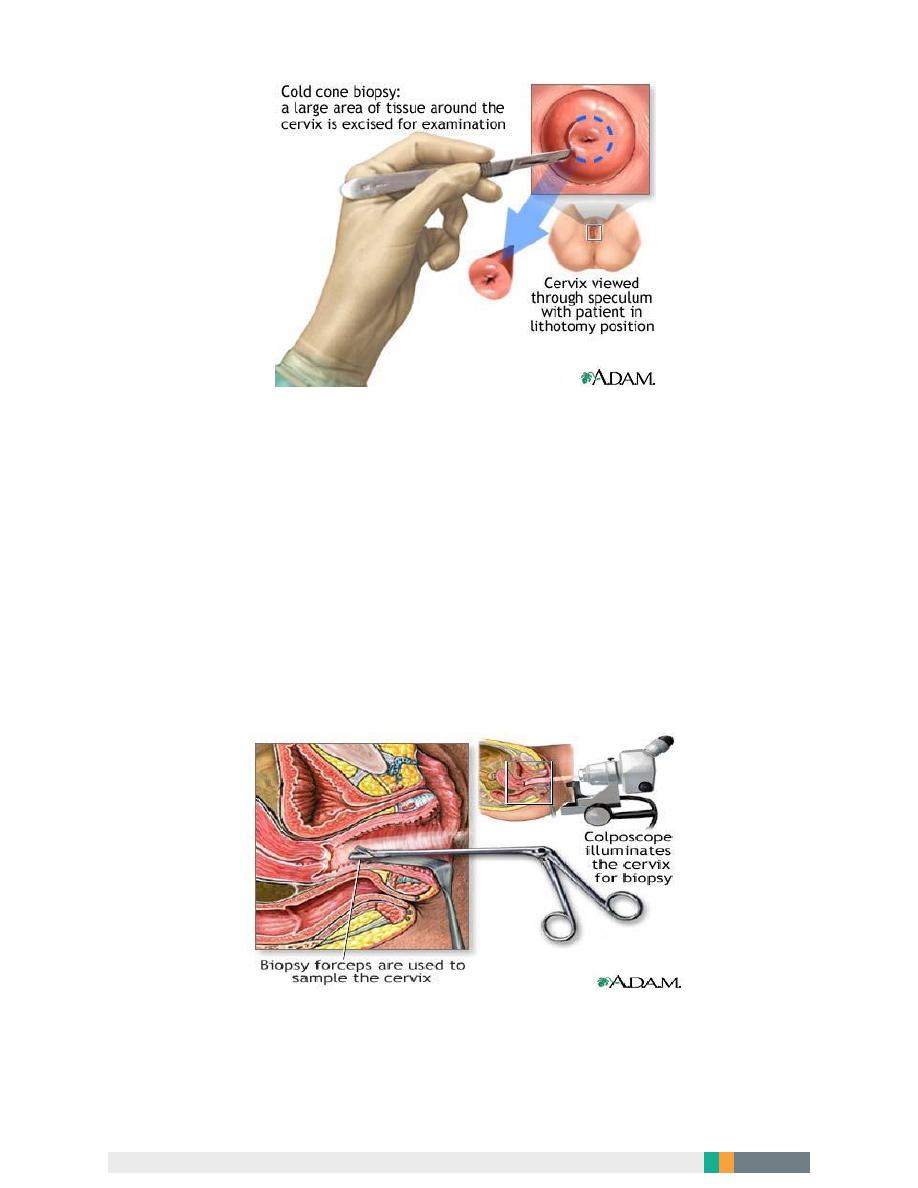
LEEP (loop electrosurgical excision procedure(. After freezing the area with local
anesthetic, an electrical wire loop is inserted into the vagina and all the abnormal
tissue is removed. This procedure is also done in the physician's office.
A cone biopsy refers to removal of a cone-shaped piece of tissue. The tissue
removed provides a more extensive sample for diagnosis than a simple biopsy. A
cone biopsy is usually done in the operating room.
16
The cold cone biopsy is a surgical procedure requiring general anesthesia and is
indicated by the presence of precancerous changes in the cervix .
What happens after treatment?
After treatment for dysplasia, patients are followed closely to make sure all the
dysplasia is gone, and that new dysplasia does not occur. Typically, patients are
followed with frequent Pap smears for two years after treatment, e.g. Pap smears
every 3 to 4 months for the first year, and then every 6 months for the second
year. If all the Pap smears come back negative, the patient is be cured, and is
then followed with yearly Pap smears.
A colposcopy-directed biopsy is a procedure in which the cervix is examined with a colposcope for abnormalities and a
tissue sample is taken .
A.LY
