Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
***********************************************************
Respiratory System I
Chapter Outline:
Overview of Respiratory System:
Nasal Cavity:
Vestibule of the Nasal Cavity.
Respiratory Region of the Nasal Cavity .
Olfactory Region of the Nasal Cavity .
Paranasal Sinuses
.
Pharynx.
Larynx.
Trachea .
Mucosa.
Submucosa.
Fibrocartiligenous coat.
Advantitia.
Bronchi.
Bronchioles.
Bronchiolar Structure .
Aleveoli.
.
Blood Supply
.
Lymphatic Vessels
.
Nerves
.
Pleura
Learning Objectives:
After studying this chapter, you should be
able to:
Locate and describe the organs of the respiratory system.
Describe the functions of the respiratory structures.
Overveiw of Respiratory System:
● T e structures which are responsible for the inhalation of air, exchange
of gases between the air and blood and exhalation of carbon dioxide
constitute the respiratory system.
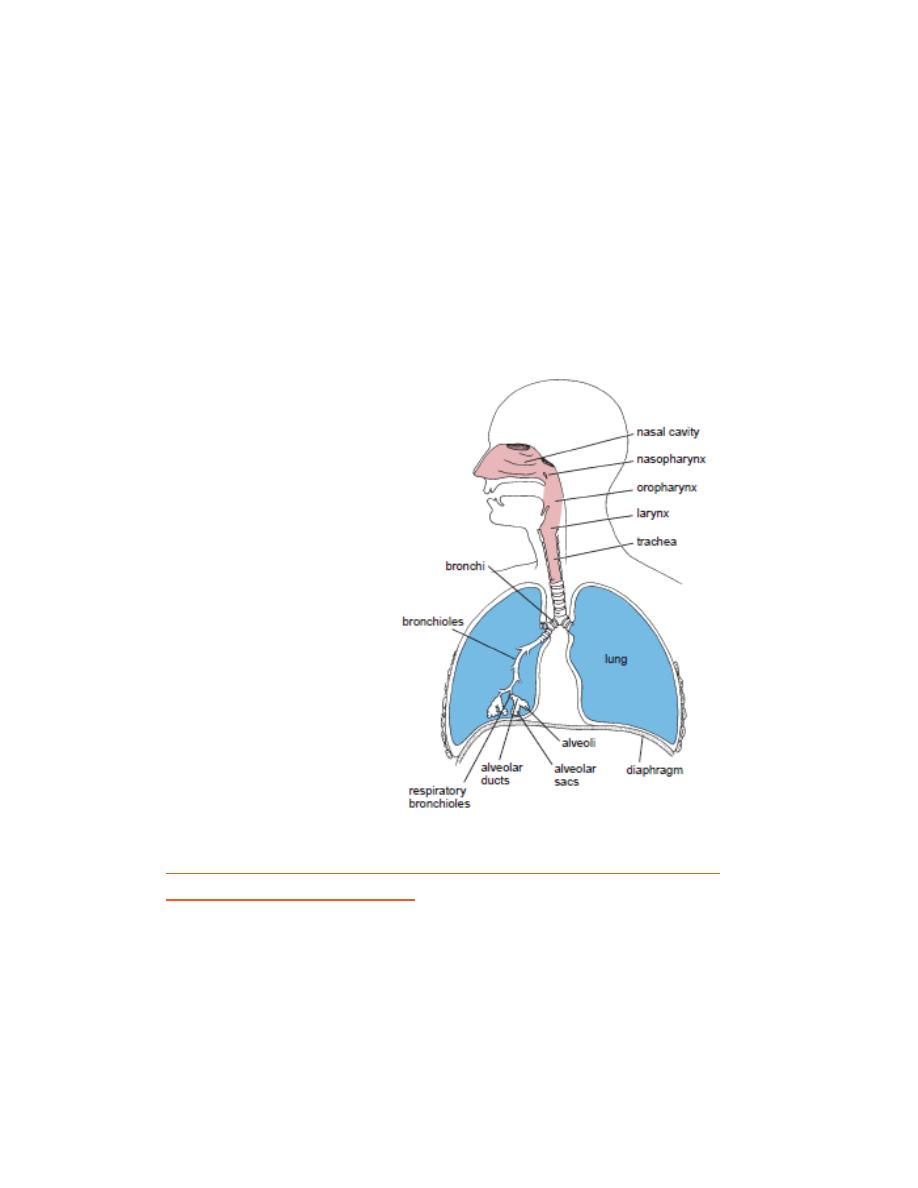
● Apart from respiration, this system is also responsible for olfaction and
sound production.
● T e respiratory system consists of two parts—a conducting part (which
carries air) and a respiratory part (where gas exchange takes place).
● T e conducting part consists of nasal cavity, paranasal sinuses,
nasopharynx, larynx, trachea, bronchi, bronchioles and terminal
bronchioles .
● T e respiratory part consists of respiratory bronchioles, alveolar ducts,
alveolar
sacs
and
alveoli.
GENERAL STRUCTURE OF THE CONDUCTING PORTION OF
THE RESPIRATORY TRACT
In general, the respiratory tract is made of four coats (Fig. ), namely:
1. Mucosa
It includes the epithelial lining and the underlying lamina propria. The
epithelium is usually pseudostratifi ed ciliated columnar epithelium with
goblet cells.

2. Submucosa
It is a layer of loose connective tissue containing mixed glands.
3. Cartilage layer
This layer is mostly formed by hyaline cartilage plus smooth muscle.
4. Adventitia
It is a layer of fi broelastic connective tissue merging with the surrounding
tissue.
STRUCTURAL CHANGES IN THE CONDUCTING PORTION OF
THE
RESPIRATORY
TRACT
(FROM
LARYNX
TO
BRONCHIOLE)
The epithelium gradually decreases in thickness (from
pseudostratified columnar ciliated to simple cuboidal ciliated).
Goblet cells in the epithelium gradually reduce in number and
completely disappear in the bronchiole.
Similarly, glands in the submucosa gradually decrease and
completely disappear distally (no glands in the bronchioles).
Elastic fibres gradually increase in amount.
The cartilage gradually reduces and disappear distally (no cartilage
in the bronchioles).
Smooth muscle fi bres relatively increase.
Nasal Cavity:
STRUCTURAL CHANGES IN THE CONDUCTING PORTION OF
THE RESPIRATORY TRACT (FROM LARYNX TO BRONCHIOLE)
The epithelium gradually decreases in thickness (from pseudostratifi
ed columnar ciliated to simple cuboidal ciliated).
Goblet cells in the epithelium gradually reduce in number and
completely disappear in the bronchiole.
Similarly, glands in the submucosa gradually decrease and
completely disappear distally (no glands in the bronchioles).
Elastic fi bres gradually increase in amount.
The cartilage gradually reduces and disappear distally (no cartilage
in the bronchioles).
Smooth muscle fi bres relatively increase.
Olfactory Region of the Nasal Cavity
The olfactory region is located on part of the dome of each nasal
cavity is lined with a specialized olfactory mucosa.In living tissue,
this mucosa is distinguished by its slight yellowish brown color
caused by pigment in the olfactory epithelium and the associated
olfactory glands.
The lamina propria of the olfactory mucosa is directly contiguous
with the periosteum of the underlying bone. The olfactory
epithelium contains very different cell types fig. Also, it lacks goblet
cells.
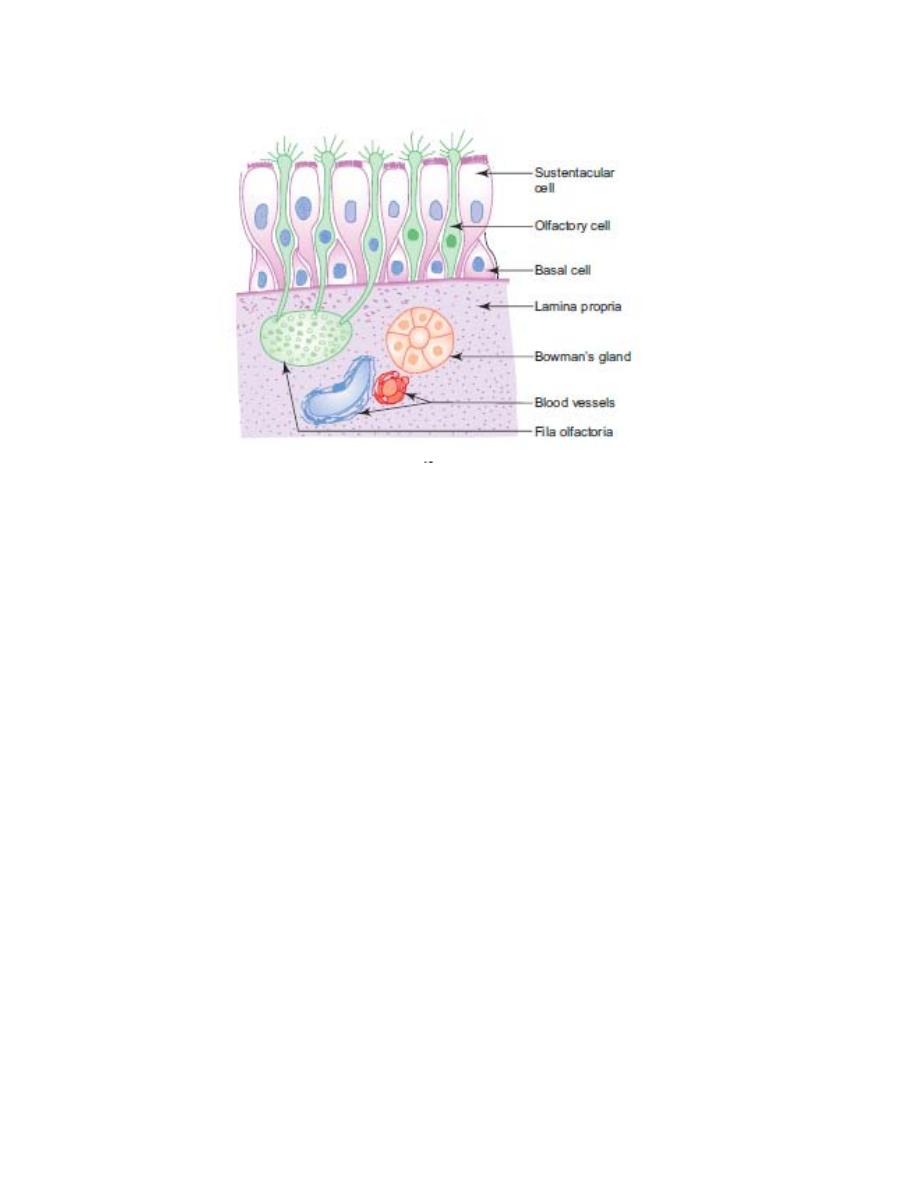
Fig.3 :olfactory mucosa
The olfactory epithelium is composed of the following cell types:
• Olfactory receptor cells are bipolar neurons that span the thickness of
the epithelium and enter the central nervous system.
• Supporting or sustentacular cells are columnar cells that are similar to
neuroglia cells and provide mechanical and metabolic support to the
olfactory receptor cells.
• Basal cells are stem cells from which new olfactory receptor cells and
supporting cells differentiate.
• Brush cells are the same cell type that occurs in the respiratory
epithelium.
Brush cells are columnar cells specialized for transduction of general
sensation.
The olfactory glands (Bowman’s glands), a characteristic feature
of the mucosa, are branched tubuloalveolar serous glands that
deliver their proteinaceous secretions via ducts onto the olfactory
surface.
The serous secretion of the olfactory glands serves as a trap and
solvent for odoriferous substances.
The identifying feature of the olfactory region of the nasal mucosa
in a histologic preparation is the presence of the olfactory nerves in
combination with olfactory glands in the lamina propria.
Respiratory region
It occupies the rest of the area of the nasal cavity. It is covered by
respiratory mucosa which is pink in colour and less thick
compared to olfactory mucosa.
The respiratory mucosa is firmly adherent to the underlying
periosteum or perichondrium.
Respiratory mucosa consists of respiratory epithelium
(pseudostratifi ed ciliated columnar epithelium with goblet cells.
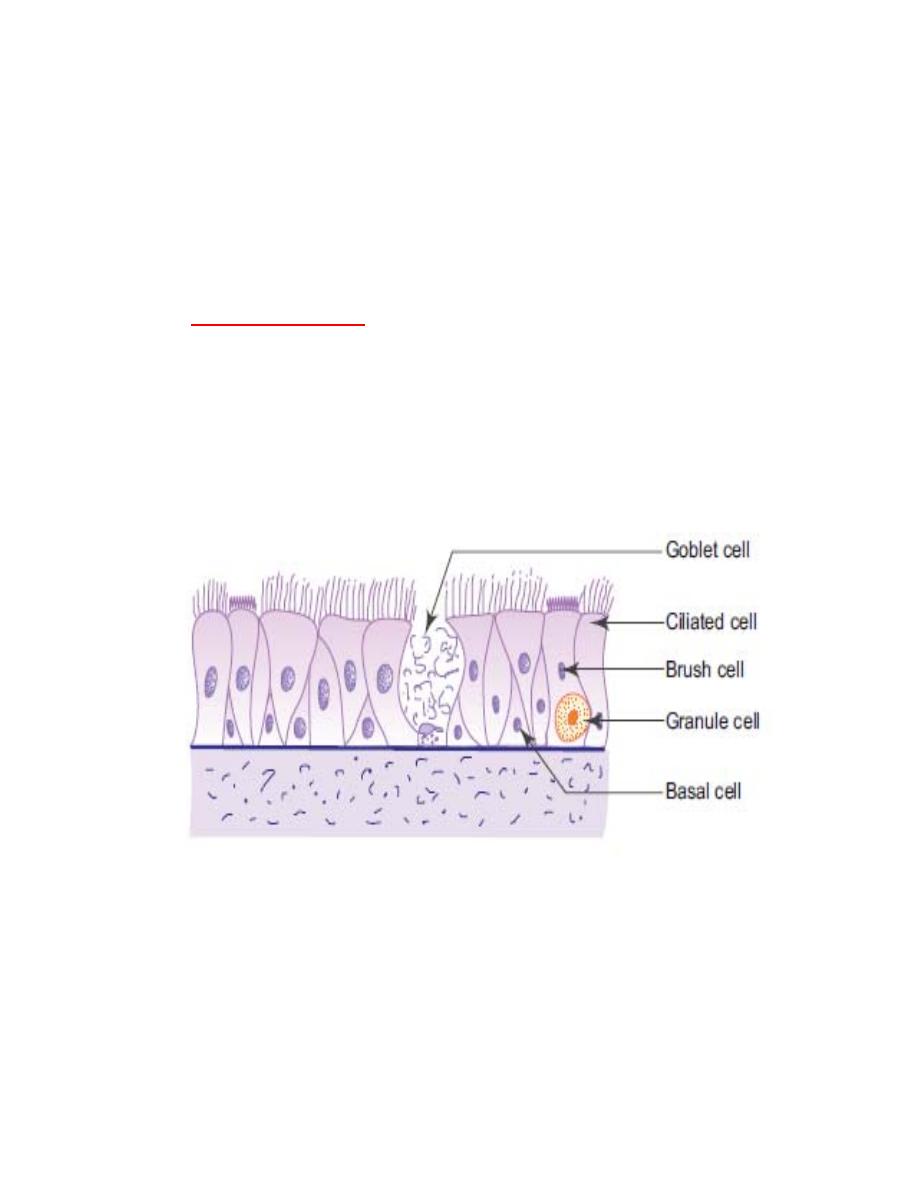
Fig.4:respiratory
mucosa
The respiratory epithelium is made of five cell types (Fig.4. These
are:
(a) Ciliated cells—columnar cells with cilia on their free surfaces, the most
abundant cell type, cilia beat towards the pharynx.
(b) Goblet cells—fl ask-shaped mucus secreting cells.

(c) Brush cells—columnar cells with microvilli on their free surfaces (may
have sensory function).
(d) Basal cells—small pyramidal cells, do not reach the surface, give rise
to other cell types.
(e) Granule cells—small round cells with many cytoplasmic granules
(form part of the APUD cell series).
The main function of the respiratory mucosa is conditioning of air, i.e.
the inspired air is:
o
cleaned by the sticky mucus of dust particles,
o
warmed by the vascular plexus in the lamina propria, and
o
moistened by the secretory fl uid provided by the glands.
Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
***********************************************************
Respiratory System II
PARANASAL SINUSES
● Paranasal sinuses are air-filled spaces in the bones around the nasal
cavity.
● There are our pairs o paranasal sinuses—frontal, sphenoidal , ethmoidal
and maxillary; they are present in the bones with the corresponding names.
● They open into the nasal cavity.
● They are lined by the respiratory mucosa.
PHARYNX
GENERAL FEATURES
Pharynx is a fibromuscular tube extending from the base of the skull
to the level of the sixth cervical vertebra where it becomes
continuous with the oesophagus.
It lies behind the nasal cavity (nasopharynx), oral cavity
(oropharynx) and larynx (laryngopharynx).
STRUCTURE
Pharynx is composed of the following four coats:
1. Mucosa
This comprises epithelium and lamina propria. The epithelium is
pseudostratifi ed ciliated columnar type in the nasopharynx and
stratified squamous type in the oropharynx and laryngopharynx.
Aggregation of lymphatic nodules in the lamina propria of the
posterior wall and around the opening of the auditory tube in the

nasopharynx results in the formation of pharyngeal and tubal
tonsils, respectively.
The palatine tonsil present in the lateral wall of the oropharynx and
the lingual tonsil in the pharyngeal part of tongue, are already dealt
with under lymphatic system.
2. Submucosa
It is formed by loose areolar connective tissue (pharyngobasilar fascia).
3. Muscle coat
This layer is formed by skeletal muscle arranged into inner
longitudinal and outer circular layers.
The circular layer is formed by the constrictors of pharynx.
4. Adventitia
It is formed by fibroelastic connective tissue (buccopharyngeal fascia).
LARYNX
● The larynx connects the oropharynx and the trachea. It is the component
of the conductive part of the respiratory system, and it is also responsible
or sound production.
● The interior of the larynx has two olds—vestibular and vocal olds—
projecting into the lumen (Fig.1).
● The vestibular old ( alse vocal cord) is lined by respiratory epithelium.
Underneath the epithelium, in the lamina propria, there are numerous
serous and mucous glands; the ducts o these glands open into the luminal
surface of the larynx.
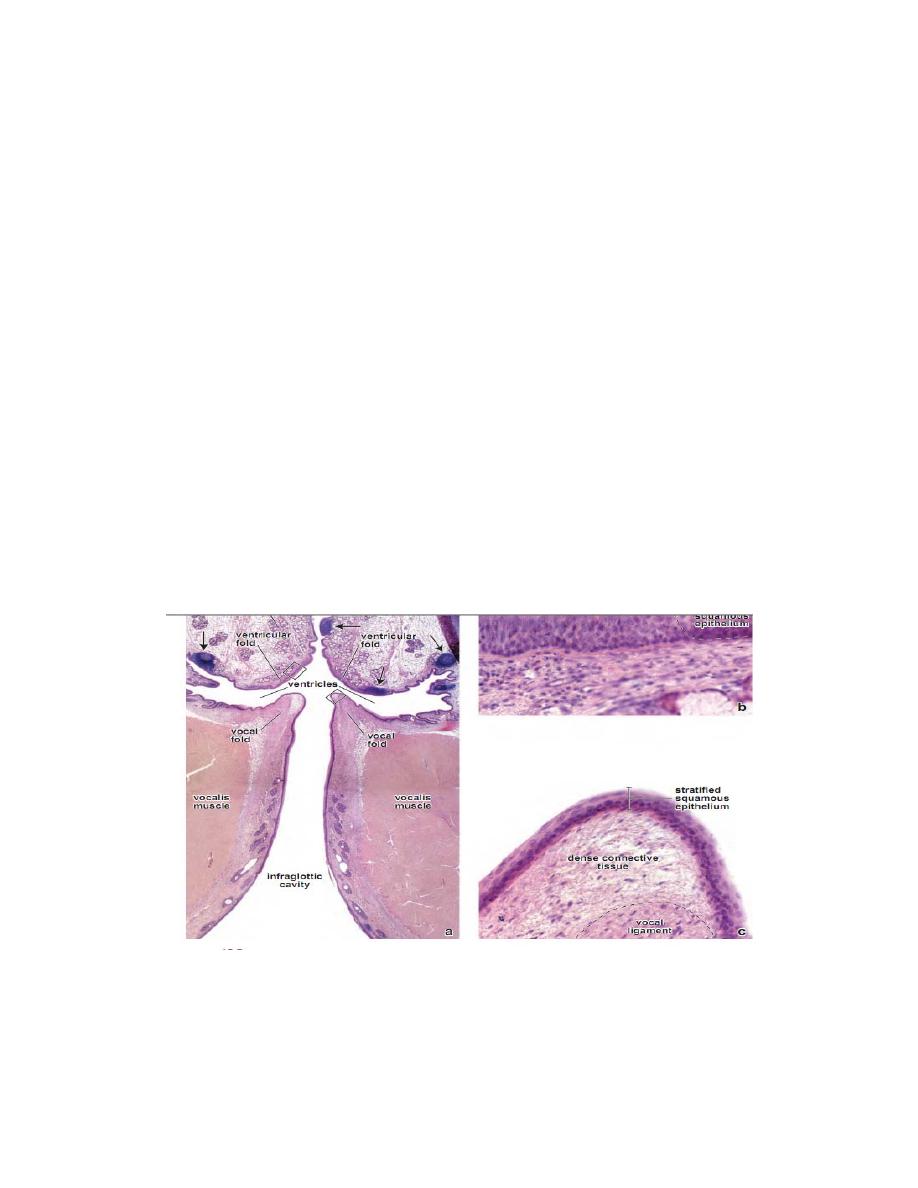
● The vocal old (true vocal cord) is lined by stratifed squamous non-
keratinised epithelium which provides protection from physical injury
during its movement.
The remaining parts of the interior of the larynx are lined by the
respiratory mucosa.
● Underneath the lamina propria , laryngeal cartilages are present.
• These are thyroid, cricoid, epiglottis, corniculate and cuneiform
cartilages; they are present in the wall o the larynx and form its
skeletal framework.
• The thyroid, cricoid and most of arytenoid consist of hyaline
cartilage .
• whereas the epiglottis, corniculate and cuneiform are elastic
cartilage.
Fig.1: histological section through the larynax
The cartilages are either hyaline or elastic in nature. These are:
Hyaline cartilages
Thyroid (unpaired)
Cricoid (unpaired)
Arytenoid (paired)
Elastic cartilages
Epiglottis (unpaired)
Cuneiform (paired)
Corniculate (paired)
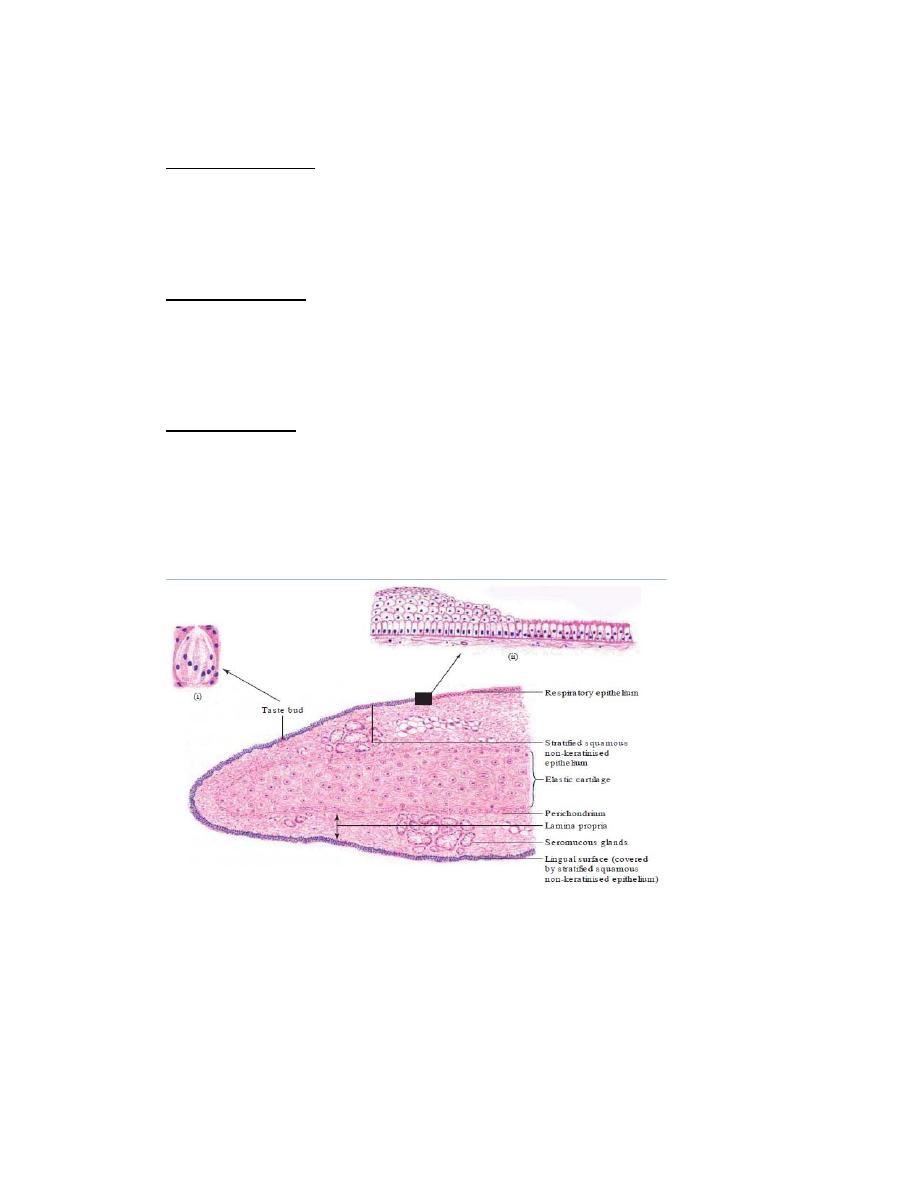
Epiglottis (Fig.)
● The epiglottis has upper and lower ends, anterior and posterior surfaces
and two lateral borders (fig.2 )
Fig. 2 : epiglottis
●The lingual surface (or anterior surface) and upper part of the laryngeal
surface (or posterior surface) are covered by stratified squamous non-
keratinised epithelium, and the rest of the laryngeal surface is covered by
respiratory epithelium.
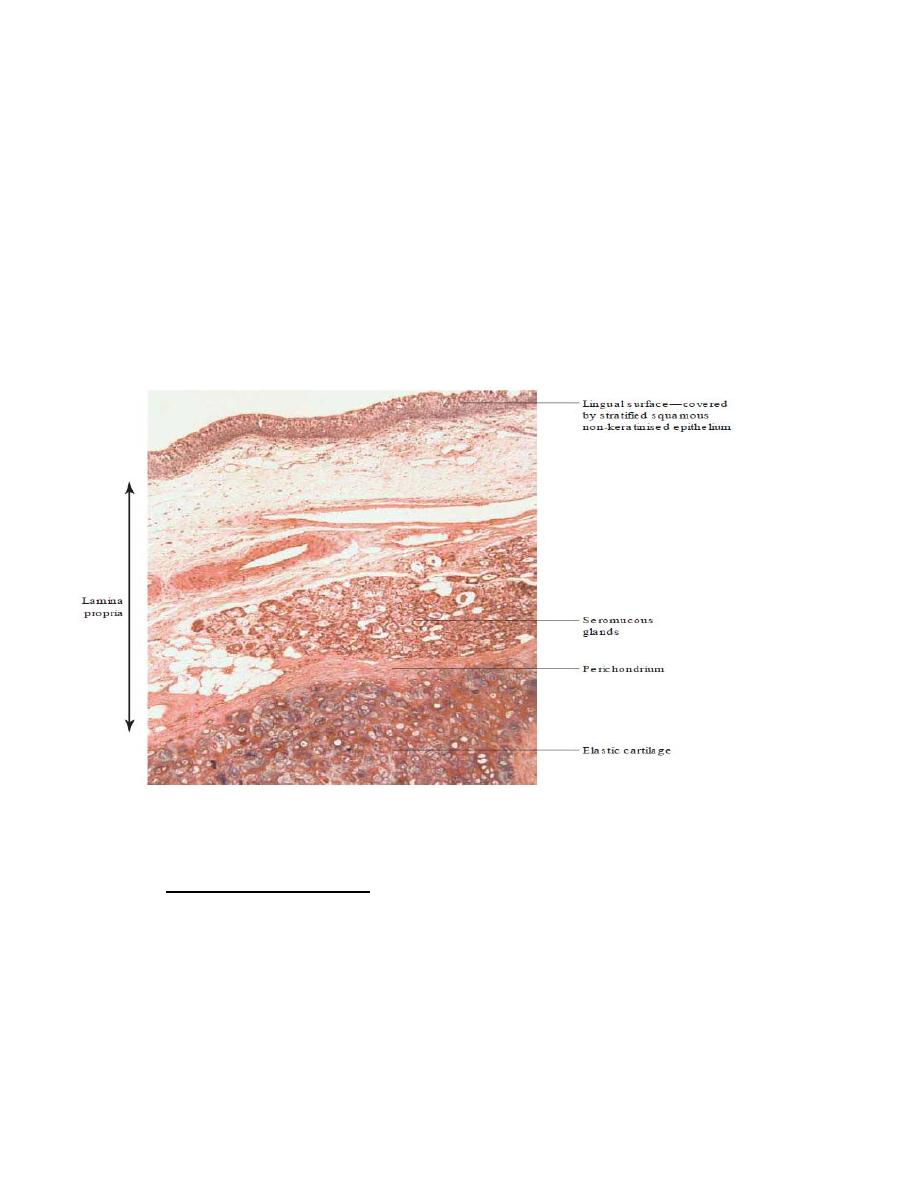
The upper part of the laryngeal surface, where the epithelium is
stratified squamous non-keratinised, shows the presence of some
taste buds.
● Lamina propria consists of connective tissue with numerous serous and
mucous glands (fig. 3 ).
● Elastic cartilage is present underneath the lamina propria and provides
the skeletal framework to the epiglottis.
Fig .3 : histological section through the epiglottis
TRACHEA (Fig. 4 ,5 ,6 )
● The luminal surface of the trachea is lined by respiratory epithelium.
● Lamina propria is present underneath the epithelium.
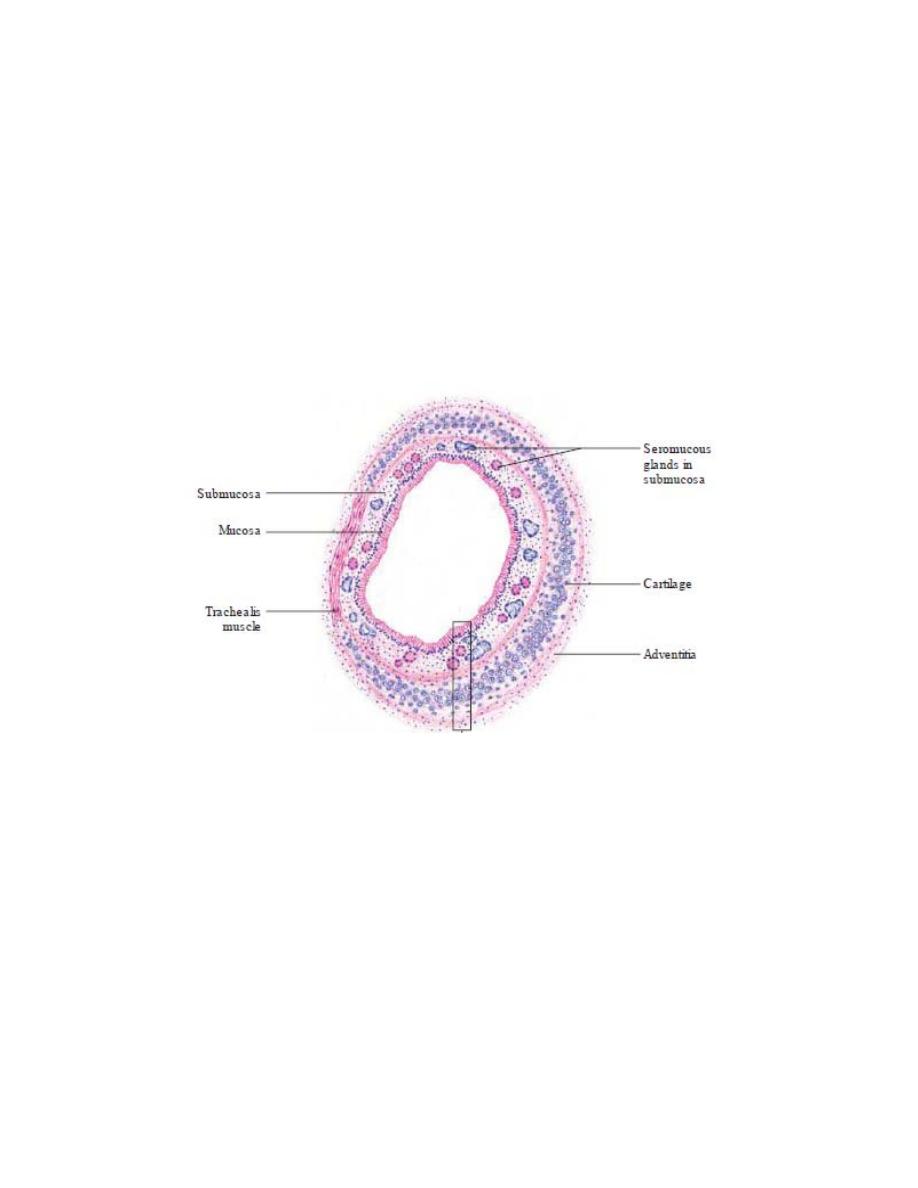
● underneath the lamina propria, there is the submucosa with serous and
mucous glands; the ducts of these glands open on the luminal surface of
the epithelium.
● Beneath the submucosa, there is ‘C’-shaped hyaline cartilage. The ends
of the ‘C’-shaped cartilage are on the posterior aspect of the trachea. The
two ends of these cartilages are joined by smooth muscle called trachealis
(Fig.4).
Fig. 4 : transfere section through the trachae
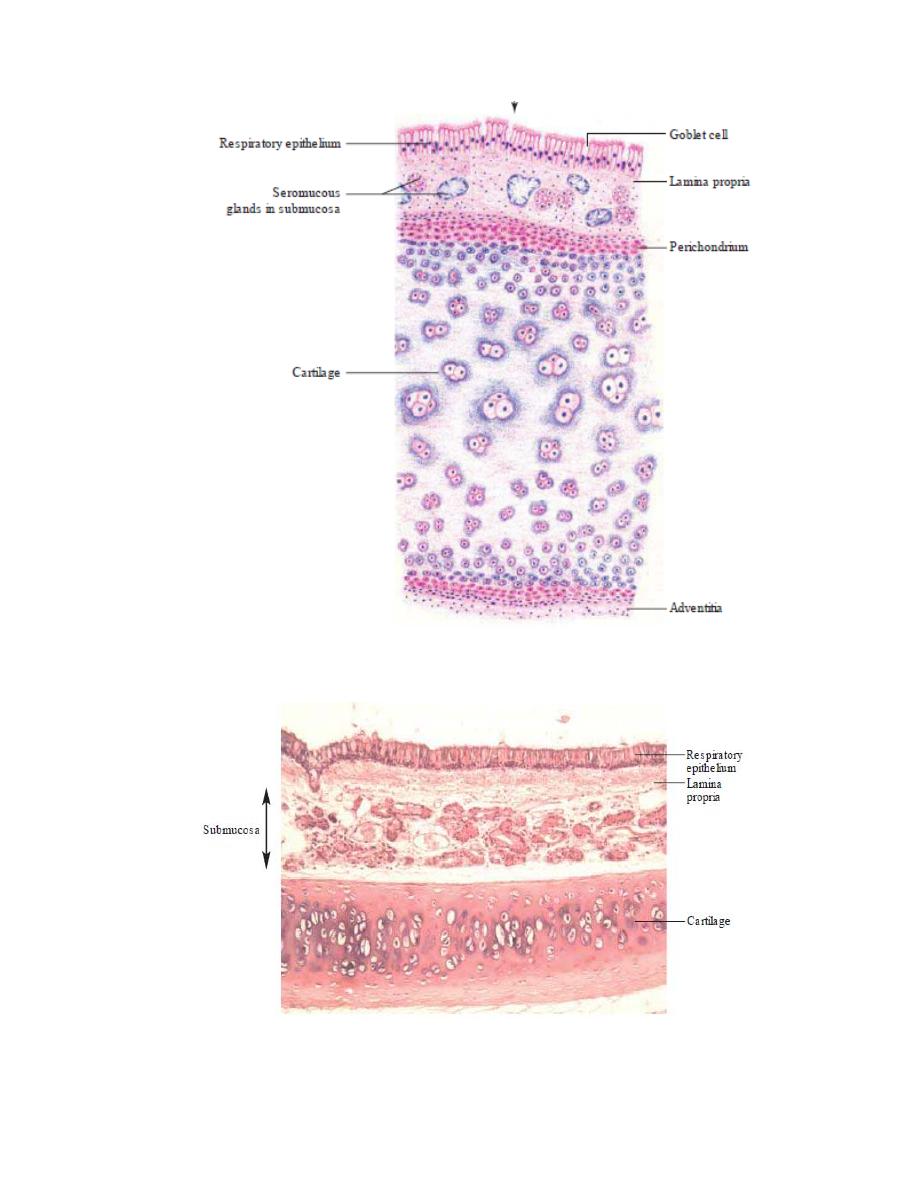
Fig. 5 : histological section through the trachae
Fig. 6 : histological section through the trachea

Trachea divides into principal bronchi in the thorax at the level
of T4
Each principal bronchus enters the lung at the hilum.
The structure of principal bronchus is similar to that of trachea.
Primary or Principal Bronchus .
The primary bronchus is similar to the trachea with a few differences
which are as follows:
● The cells o respiratory epithelium are shorter and have less number
of goblet cells.
● Between the lamina propria and the submucosa, there are bundles of
spirally arranged smooth muscle, completely encircling the bronchus.
● Glands in submucosa are less in number compared to those in the
submucosa of trachea.
● Cartilaginous rings completely encircle the bronchus.
Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
***********************************************************
Respiratory System III
Lung:
Lungs are the principal organs of respiration, situated in the thoracic
cavity one on either side of the mediastinum.
Each lung is conical in shape and is covered with visceral pleura.
It contains the terminal parts of the bronchial tree, namely,
intrapulmonary bronchus, bronchiole, respiratory bronchiole and
lung parenchyma (alveolar ducts and alveoli) along with blood
vessels.
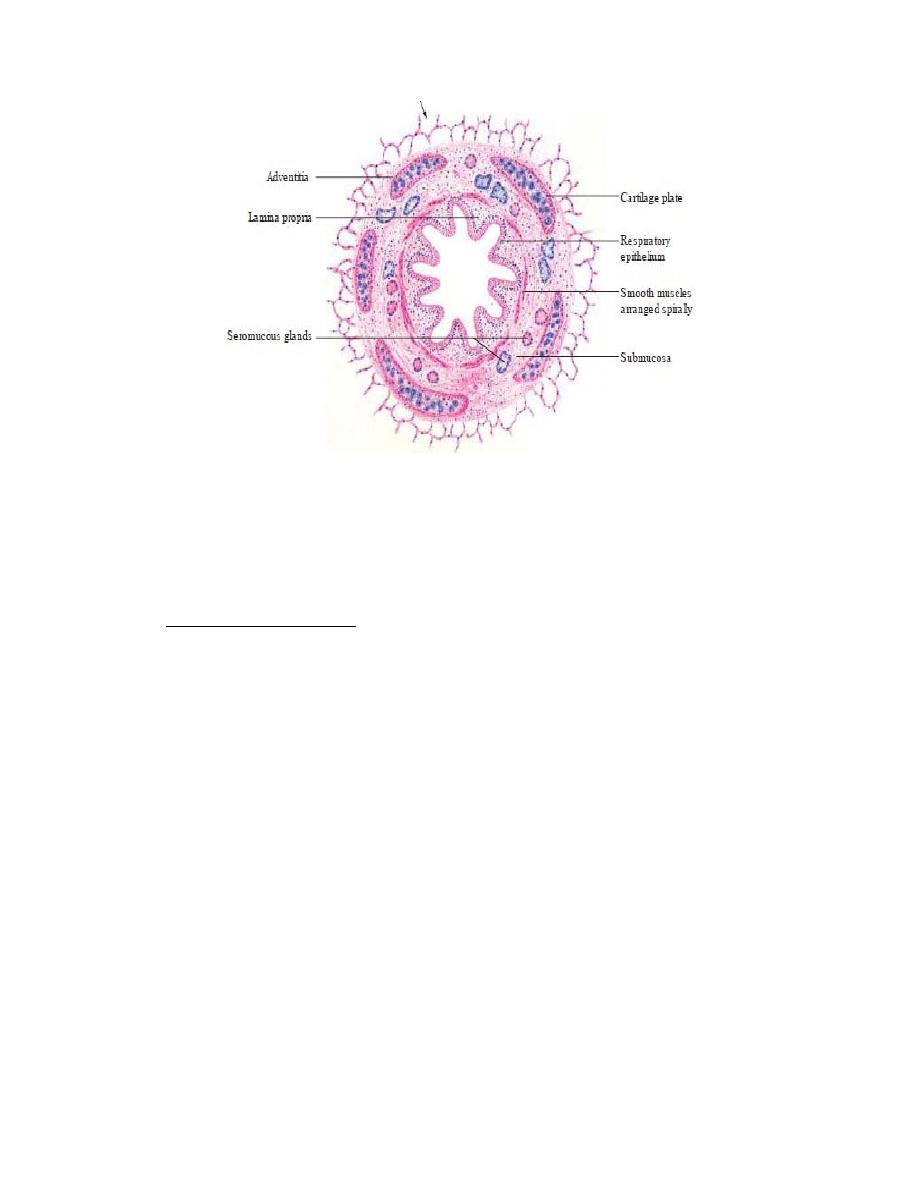
Intrapulmonary bronchus (secondary and tertiary bronchi)
In the lung each principal bronchus divides into secondary or lobar
bronchi which in turn divide into tertiary or segmental bronchi
Secondary and Tertiary Bronchi
They are similar to the primary bronchus except for the following:
● The number of goblet cells is further reduced in the epithelium.
● The number of glands in the submucosa is also reduced.
● The cartilage is present as irregular plates.
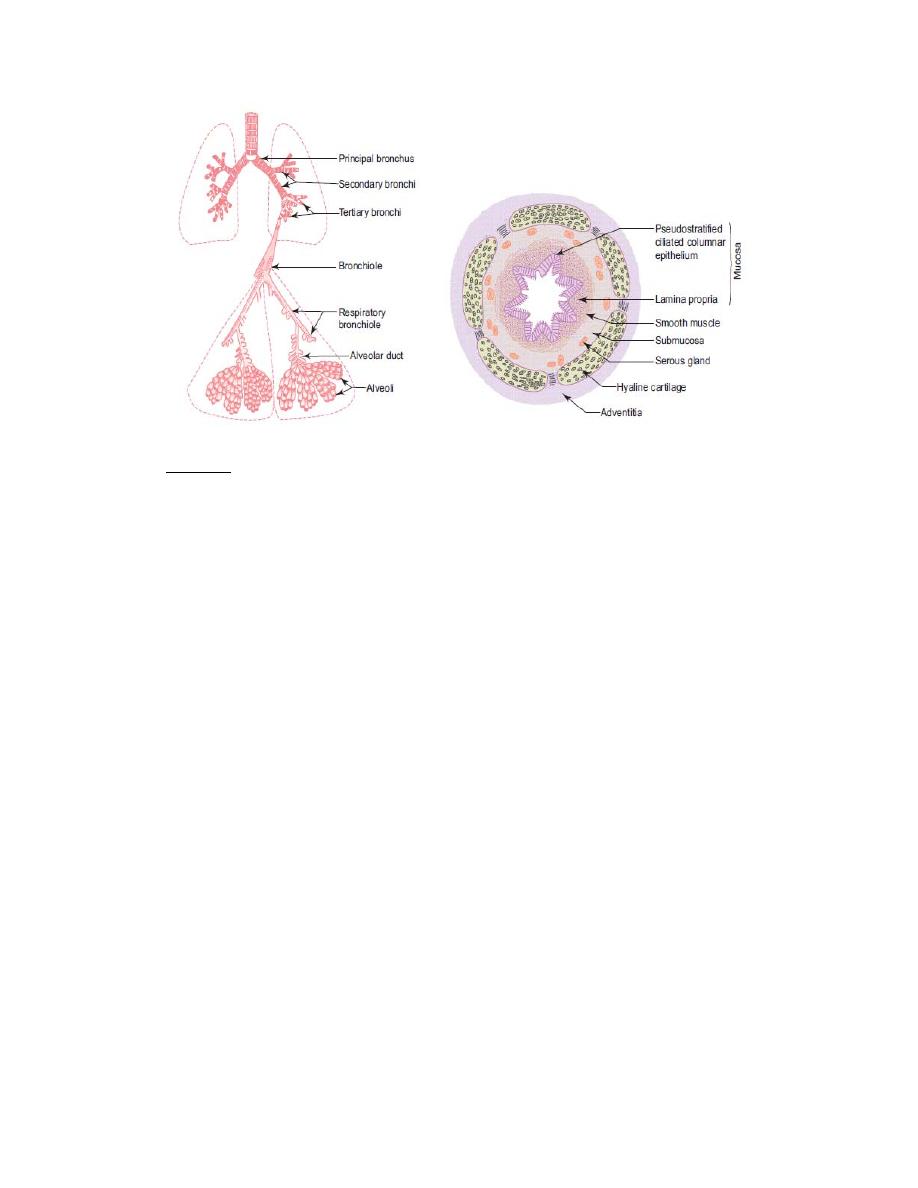
Mucosa
– It consists of epithelium and lamina propria.
– The epithelium is pseudostratified ciliated columnar variety with few
goblet cells.
– The lamina propria is rich in elastic fibres (longitudinally oriented).
– Mucosa is thrown into folds by the contraction of underlying smooth
muscle.
(b) Smooth muscle layer
– This layer consists of spirally running criss-cross bundles of smooth
muscle. Thus, in section the muscle layer appears to be discontinuous.
(c) Submucosa
– It contains few seromucous glands.
(d) Cartilage layer and adventitia
In contrast to C-shaped cartilage present in the trachea, the intrapulmonary
bronchus contains isolated plates of hyaline cartilage.

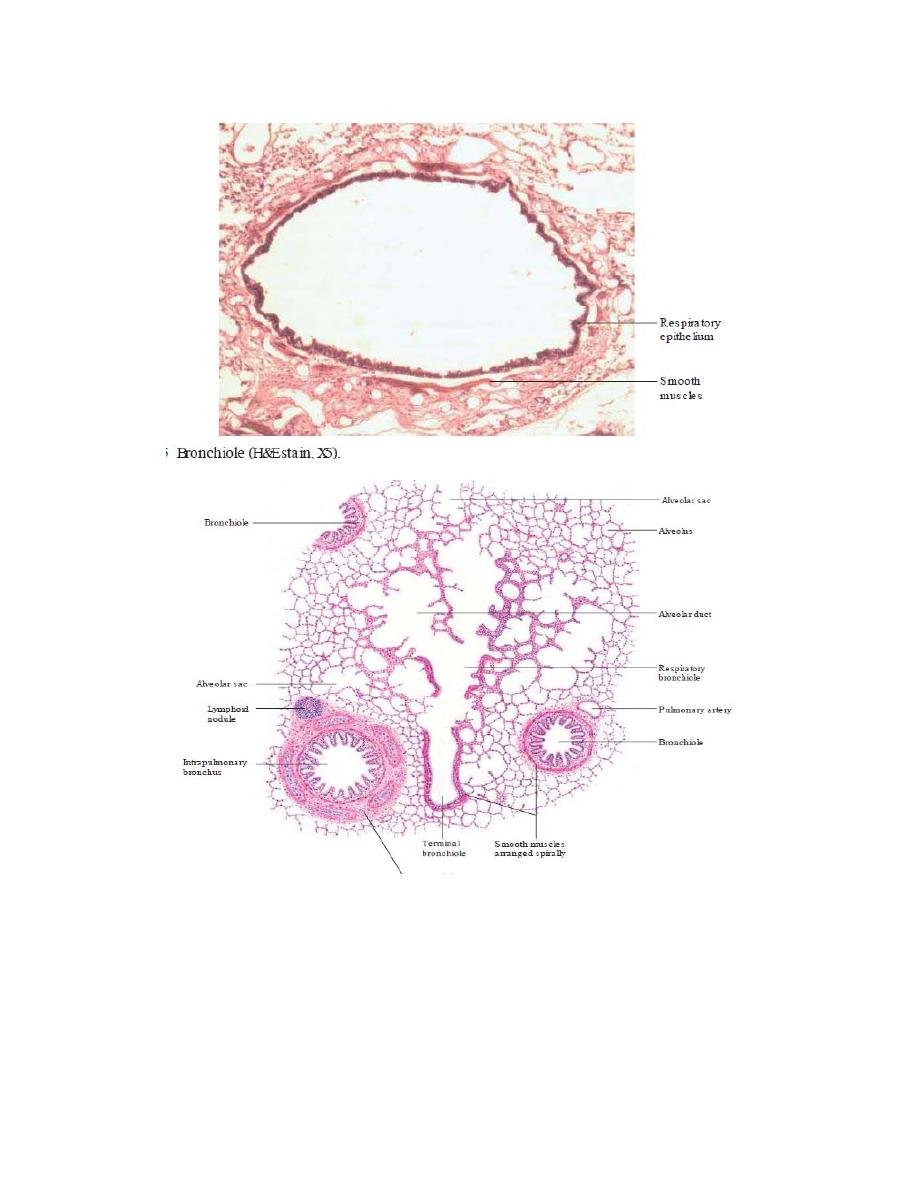
Bronchiole
Bronchioles are formed by repeated division of the tertiary bronchi.
Each bronchiole enters a pulmonary lobule, where it divides to form
5 to 7 terminal bronchioles.
The diameter of the terminal bronchiole is less than 1 mm.
Bronchioles are characterised by the presence of the following
features :
Simple columnar or cuboidal ciliated epithelial lining with no goblet
cells. Here goblet cells are replaced by Clara cells which secrete a
glycoprotein that protects the bronchiolar lining against oxidative
pollutants and inflammation.
– Thick smooth muscle layers (under the control of vagus and
sympathetic
nerves).
Stimulation
of
vagus
causes
bronchoconstriction. Stimulation of sympathetic nerve causes
bronchodilation.
– Many elastic fibres
– No glands
– No cartilage
In the epithelium of the terminal bronchiole, dome-shaped cells called
Clara cells
are also present ,
whose function is not known. They may
provide some protection against inhaled toxins and carcinogens.
Respiratory Bronchiole
● The respiratory bronchiole is lined by simple cuboidal epithelium; these
cells lack cilia.
● Goblet cells are absent.
● Epithelium is interrupted by alveoli, and at the opening of the alveoli the
epithelium changes to simple squamous epithelium.
● The smooth muscle forms a ring around the opening of the alveoli.
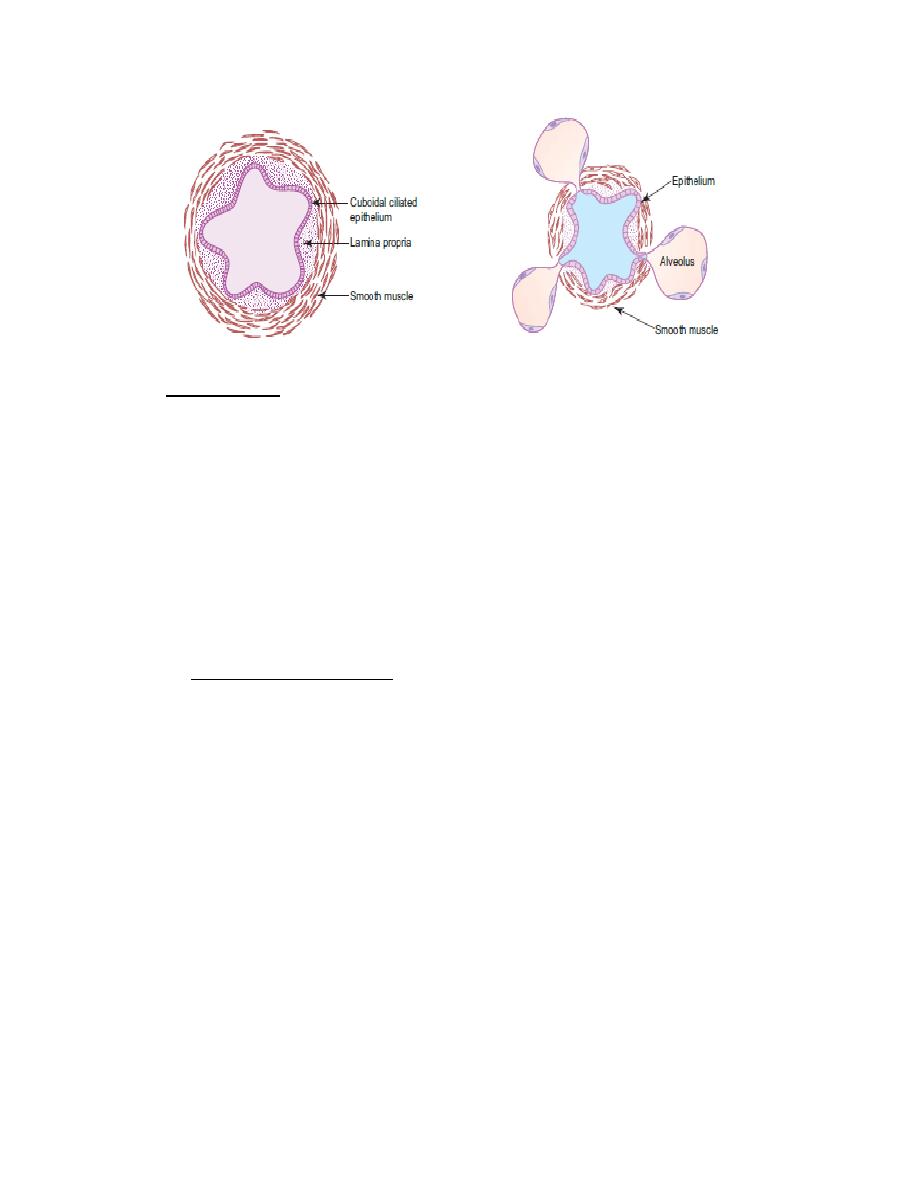
Alveolar Duct
● The wall of the alveolar duct consists of alveoli, lined by simple
squamous epithelium.
● Underneath the epithelium, smooth muscles form rings at the opening
of the alveolar sacs and alveoli ,which are seen as a small bulge, in the
wall in between two adjacent alveoli.
● Smooth muscles disappear in the terminal parts of alveolar ducts.
Alveolar Sac and Alveoli
● The alveolar duct opens into dead end sacs, the alveolar sacs, which
have openings of the alveoli.
● Alveoli increase the surface area for the gaseous exchange. Alveoli
are surrounded by a network of capillaries .The gaseous exchange
occurs between the air present in the alveoli and the blood in the
capillaries across their walls (see ‘Interalveolar Septum’).
● Alveoli are thin-walled outpouchings , lined by a single layer of cells;
these cells are of two types:
type I and type II cells, also called pneumocytes or alveolar cells.
Alveoli are separated by interalveolar septum which lies between thin
squamous epithelial linings of two neighbouring alveoli.

The interalveolar septum contains a network of capillaries
supported by reticular and elastic fibres , and occasionally
fibroblasts, mast cells and macrophages. The septum may contain
pores (alveolar pores of Kohn) which help in passage of air from one
alveolus to another, thus equalizing the pressure in the alveoli.
The elastic fibres enable the alveoli to expand during inspiration and
passively contract during expiration.
The reticular fibres support and prevent overdistension of the
alveoli.
Capillaries present in the interalveolar septum are lined by
continuous endothelium, the cytoplasm of which contains numerous
pinocytotic vesicles. The organelles are grouped around the nucleus
to make the rest of the area extremely thin allowing better exchange
of gases.
Alveolar macrophages (dust cells) are derived from monocytes and
are a part of mononuclear phagocytic system.
The cytoplasm of macrophages contain phagocytosed inhaled
carbon and dust particles which are passed on to them from
pneumocyte I through pinocytotic vesicles. The alveolar
macrophages sometimes migrate from septum to alveolar surface
(having come, cannot go back to septum) and are carried to the
pharynx through sputum and their characteristics is of diagnostic
importance.
The lining epithelium of the alveolus is made of two types of cells,
viz.,
(a) Type I pneumocytes/squamous epithelial cells
– Extremely thin squamous cells (25 nm thick).
– Cover 97% of alveolar surface.
– Contain abundant pinocytic vesicles which play a role in
absorption of surfactant and removal of particulate contaminants
from the surface.
– Form part of the blood-air barrier.
(b) Type II pneumocytes/great alveolar cells/septal cells
– Roughly cuboidal in shape, found in groups of 2 or 3 cells between
type I pneumocytes.
– Cover 3% of alveolar surface.
– Bear microvilli on their free surfaces.
– Contain foamy vacuolated cytoplasm due to presence of lamellated
bodies.
– These lamellated bodies contain a complex lipoprotein which on
release spreads over the alveolar surface forming pulmonary
surfactant that lowers the surface tension and prevents the alveoli
from collapsing during expiration. The surfactant also has
bactericidal properties. The surfactant layer is constantly being
renewed.
It is removed from the surface by type I pneumocytes and
macrophages.
Air–Blood Barrier
The oxygen molecule present in the alveolus diffuses across the
epithelial cells lining the alveolus, the used basement membrane of the
alveolus and capillary, the endothelial cells of the capillary and finally
into the red blood cell .
PULMONARY CIRCULATION
● Lungs have dual blood supply through bronchial and pulmonary
vessels.
● Bronchial vessels supply the conducting part of the lungs and
pulmonary vessels supply the respiratory part.
● The blood vessels accompany the airways; they are present in the
connective tissue that is present around the airways.
● At the level of the alveolar ducts, arterioles divide and form a
capillary network around alveoli. These capillary networks are present
in the interalveolar septum.
LYMPHATIC CIRCULATION
● Lymphatic vessels accompany the blood vessels.
● No lymphatic vessels are present in the alveolar sac and
interalveolar septa.
PLEURA
● Pleura is a serous sac which covers the lungs.
● It consists of visceral and parietal layers. Between the two layers is a
potential space known as pleural cavity which contains pleural fluid.
● The visceral layer lines the lungs and the parietal layer lines the
interior of the thoracic cavity.
● Histologically, pleura consists of mesothelium (simple squamous
epithelium) overlying a thin layer of vascular connective tissue.
Clinical Correlates
Emphysema
● It is characterised by abnormal permanent dilatation of airways distal to
the terminal bronchiole. Dilatations occur due to destruction of the walls
of the airways. Cigarette smoking and air pollution are the causative
actors.

Bronchiectasis
● It is characterised by permanent dilatation o the bronchi and
bronchioles due to damage to the muscles and elastic tissue.
Bronchial Asthma
● It occurs due to increased responsiveness o the airway to the allergen.
The diameter of the airway is reduced due to contraction of the smooth
muscles present in the airway.
Pulmonary Oedema
● It refers to accumulation of fluid within the lung parenchyma and air
spaces of the lungs. The fluid entering the alveoli of the lungs prevents
gaseous exchange. Pulmonary oedema is seen in left ventricular failure
(it can occur in several other conditions also) when the left ventricle ails
to empty completely. As a result backpressure develops in the left atrium,
pulmonary veins and capillaries. Due to increase in capillary hydrostatic
pressure, the fluid moves from the capillaries into the alveolar spaces.
