Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
*************************************************************
Endocrine System I:
The
endocrine system
produces various secretions called
hormones
[Gr.
hormaein, to set in motion] that release for delivery to the bloodstream for
transport to target cells and organs, serve as effectors to regulate the activities of
various cells, tissues, and organs in the body.
Its functions are essential in maintaining homeostasis and coordinating body
growth and development and are similar to that of the nervous system: Both
communicate information to peripheral cells and organs.
These two systems are functionally interrelated. But endocrine system produces
a slower and more prolonged response than the nervous system.
Both systems may act simultaneously on the same target cells and tissues.
The endocrine system including the discrete
endocrine Glands (pituitary
gland & hypothalamus, thyroid gl., adrenal gl. ,pineal gl. ,parathyroid gl.)
as well as
individual cells
within the gonads, liver, pancreas, kidney, and
gastrointestinal system.
Pituitary Gland(Hypophisis):
The
pituitary gland
and the
hypothalamus
, the portion of the brain to which the
pituitary gland is attached, are morphologically and functionally linked in the
endocrine and neuroendocrine control of other endocrine glands.
Gross Structure and Development
The pituitary gland is composed of glandular epithelial tissue and neural
(secretory) tissue.
The
pituitary gland
[Lat. Pituta , phlegm—reflecting its nasopharyngeal
origin] is a pea-sized, compound endocrine gland .
It is centrally located at the base of the brain, where it lies in a depression
of the sphenoid bone called the
sella turcica
.
A short stalk, the
infundibulum
, and a vascular network connect the
pituitary gland to the hypothalamus.
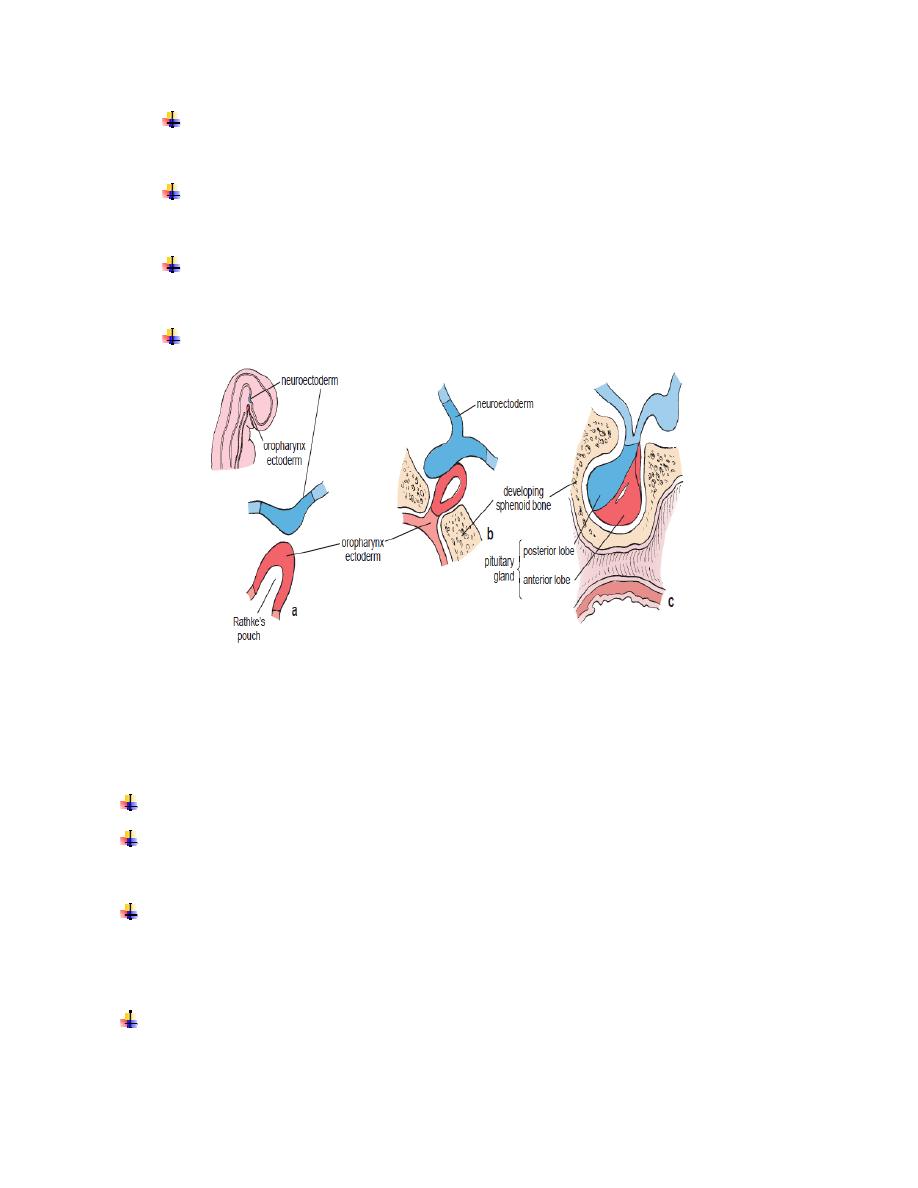
The pituitary gland has two functional components (Fig. 1,2):
Fig. (1) : development of pituitary gland
•
Anterior lobe (adenohypophysis)
, the glandular epithelial tissue.
•
Posterior lobe (neurohypophysis)
, the neural secretory tissue .
These two portions are of different embryologic origin.
The anterior lobe of the pituitary gland is derived from an evagination of the
ectoderm of the oropharynx
toward the brain
(Rathke’s pouch)
.
The posterior lobe of the pituitary gland is derived from a downgrowth (the
future infundibulum) of
neuroectoderm of the floor of the third ventricle
(the
diencephalon) of the developing brain (Fig. 1) .
The
anterior lobe of the pituitary gland
consists of three derivatives of
Rathke’s pouch:
Pars distalis
, which comprises the bulk of the anterior lobe of the
pituitary gland and arises from the thickened anterior wall of the pouch .
Pars intermedia
, a thin remnant of the posterior wall of the pouch that
abuts the pars distalis.
Pars tuberalis
, which develops from the thickened lateral walls of the
pouch and forms a collar or sheath around the infundibulum.
The
posterior lobe of the pituitary gland
consists of the following:
o
Pars nervosa
, which contains neurosecretory axons and their
endings.
o
Infundibulum
, which is continuous with the:
median eminence
and contains the neurosecretory axons forming the
hypothalamohypophyseal tracts .
Blood Supply & the Hypothalamo-Hypophyseal Portal System:
The blood supply derives from two groups of vessels coming off the internal
carotid artery .
The pituitary blood supply is derived from two sets of vessels:
•
Superior hypophyseal arteries
supply the pars tuberalis , median eminence, and
infundibulum.
•
Inferior hypophyseal arteries
primarily supply the pars nervosa. These vessels arise
solely from the internal carotid arteries.
An important functional observation is that most of the anterior lobe of the pituitary
gland has no direct arterial supply.
The hypothalamohypophyseal portal system provides the crucial link between the
hypothalamus and the pituitary gland.
The arteries that supply the pars tuberalis , median eminence, and infundibulum give
rise to fenestrated capillaries (the primary capillary plexus). These capillaries drain
into portal veins, called the
hypophyseal portal veins
, which run along the pars
tuberalis and give rise to a second fenestrated sinusoidal capillary network (the
secondary capillary plexus).
Nerve Supply
The nerves that enter the infundibulum and pars nervosa from the hypothalamic
nuclei are components of the posterior lobe of the pituitary gland .
The nerves that enter the anterior lobe of the pituitary gland are postsynaptic
fibers of the autonomic nervous system and have vasomotor function.
Structure and Function of the Pituitary Gland
Anterior Lobe of the Pituitary Gland (Adenohypophysis)
The anterior lobe of the pituitary gland regulates other endocrine glands .
Most of the
anterior lobe of the pituitary gland
has the typical organization of
endocrine tissue.
The cells are organized in clumps and cords separated by fenestrated sinusoidal
capillaries of relatively large diameter.
These cells respond to signals from the hypothalamus and synthesize and secrete
a number of pituitary hormones
.
Four hormones of the anterior lobe—
adrenocorticotropic hormone (ACTH),
thyroidstimulating (thyrotropic) hormone (TSH, thyrotropin), follicle-
stimulating hormone (FSH)
, and
luteinizing hormone (LH)
—are called
tropic hormones
because they regulate the activity of cells in other endocrine
glands throughout the body.
The two remaining hormones of the anterior lobe,
growth hormone (GH)
and
prolactin (PRL)
, are not considered tropic because they act directly on target
organs that are not endocrine.
Pars Distalis .
The cells within the
pars distalis
vary in size, shape, and staining properties.
The cells are arranged in cords and nests with interweaving capillaries.
Histologists identified three types of cells according to their staining reaction,
namely,
basophils (10%)
,
acidophils (40%)
, and
chromophobes (50%)
fig.(2)
.
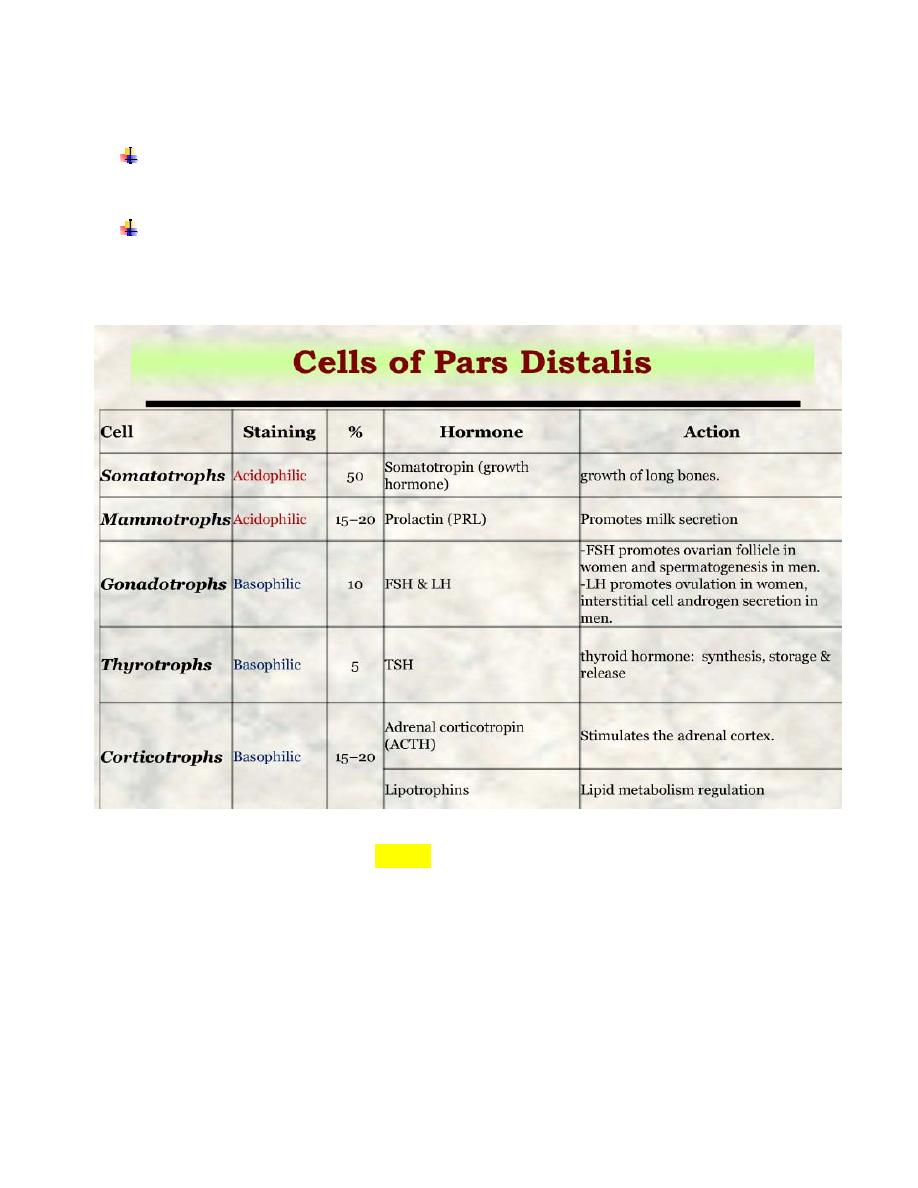
Five functional cell types are identified in the pars distalis on the basis of
immunocytochemical reactions (Table).
In addition to the five types of hormone-producing cells, anterior lobe of the
pituitary gland contains folliculostellate cells .
Folliculo-stellate cells
present in the anterior lobe of the pituitary gland are
characterized by a starlike appearance with their cytoplasmic processes encircling
hormone-producing cells. They have the ability to make cell clusters or small follicles,

and they do not produce hormones. It transmits signals from the pars tuberalis to pars
distalis. These signals may regulate hormone release throughout the anterior lobe of
the pituitary gland.
Pars Intermedia.
The
pars intermedia
surrounds a series of small cystic cavities that
represent the residual lumen of Rathke’s pouch
fig.(2)
. The parenchymal cells of the
pars intermedia surround colloid-filled follicles. The cells lining these follicles appear
to be derived either from folliculo-stellate cells or various hormone-secreting cells,
pars intermedia have vesicles larger than those found in the pars distalis.. The pars
intermedia contains
basophils
and
chromophobes
(Fig. 2). Frequently, the basophils
and cystic cavities extend into the pars nervosa.
fig.(2):Gross & microhistological sections of pituitary gland
Pars Tuberalis.
The
pars tuberalis
is an extension of the anterior lobe along the stalklike
infundibulum
fig.(2)
.
It is a highly vascular region containing veins of the hypothalamohypophyseal
system. The parenchymal cells are arranged in small clusters or cords in
association with the blood vessels.
Nests of squamous cells and small follicles lined with cuboidal cells are
scattered in this region. These cells often show immunoreactivity for ACTH,
FSH, and LH.
Posterior Lobe of the Pituitary Gland
(Neurohypophysis)
The posterior lobe of the pituitary gland is an extension of the central
nervous system (CNS) that stores and releases secretory products from the
hypothalamus , consists of the
pars nervosa
, the
infundibulum& median
eminance
that connects it to the hypothalamus
fig.(2).
The pars nervosa, contains the unmyelinated axons and their nerve endings of
approximately 100,000
neurosecretory neurons
whose cell bodies lie in the
supraoptic nuclei
and
paraventricular nuclei
of the hypothalamus.
The axons form the
hypothalamohypophyseal
tract and are unique in two
respects:
First, they do not terminate on other neurons or target cells but end in close proximity
to the fenestrated capillary network of the pars nervosa.
Second, they contain secretory vesicles in all parts of the cells, i.e., the cell body,
axon, and axon terminal.
The posterior lobe of the pituitary gland is not an endocrine gland. Rather, it
is a storage site for neurosecretions of the neurons of the supraoptic and
paraventricular nuclei of the hypothalamus.
The nonmyelinated axons convey neurosecretory products to the pars
nervosa.
Other neurons from the hypothalamic nuclei also release their secretory
products into the fenestrated capillary network of the infundibulum, the
first capillary bed of the hypothalamohypophyseal portal system .
There are neurosecretory vesicles in the nerve endings of the pars
nervosa, aggregate to form Herring bodies that contain either
oxytocin
or
antidiuretic hormone
(
ADH
; also called
vasopressin).
Oxytocin promotes contraction of smooth muscle of the uterus and
myoepithelial cells of the breast.
The pituicyte is the only cell specific to the posterior lobe of the
pituitary gland , Because of their many processes and relationships to the
blood, the pituicyte serves a supporting role similar to that of astrocytes in
the rest of the CNS.
Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
***********************************************************
Endocrine system part II
Hypothalamus:
The hypothalamus regulates pituitary gland activity.
The
hypothalamus
is located in the middle of the base of the brain, and it encapsulates
the ventral portion of the third ventricle.
It coordinates most endocrine functions of the body and serves as one of the major
controlling centers of the autonomic nervous system.
Some of the functions that it regulates include blood pressure, body temperature, fluid
and electrolyte balance, body weight, and appetite.
The hypothalamus produces numerous neurosecretory products. In addition to
oxytocin
and
ADH
, hypothalamic neurons secrete polypeptides that promote and inhibit the
secretion and release of hormones from the anterior lobe of the pituitary gland.
Pineal Gland:
The
pineal gland
(pineal body, epiphysis cerebri) is an endocrine or neuroendocrine
gland that regulates daily body rhythm.
It develops from neuroectoderm of the posterior portion of the roof of the diencephalon
and remains attached to the brain by a short stalk, it is located at the posterior wall of
the third ventricle near the center of the brain.
The pineal gland is a flattened, pine cone–shaped structure, hence its name.
The pineal gland contains two types of parenchymal cells:
Pinealocytes and interstitial (glial) cells.
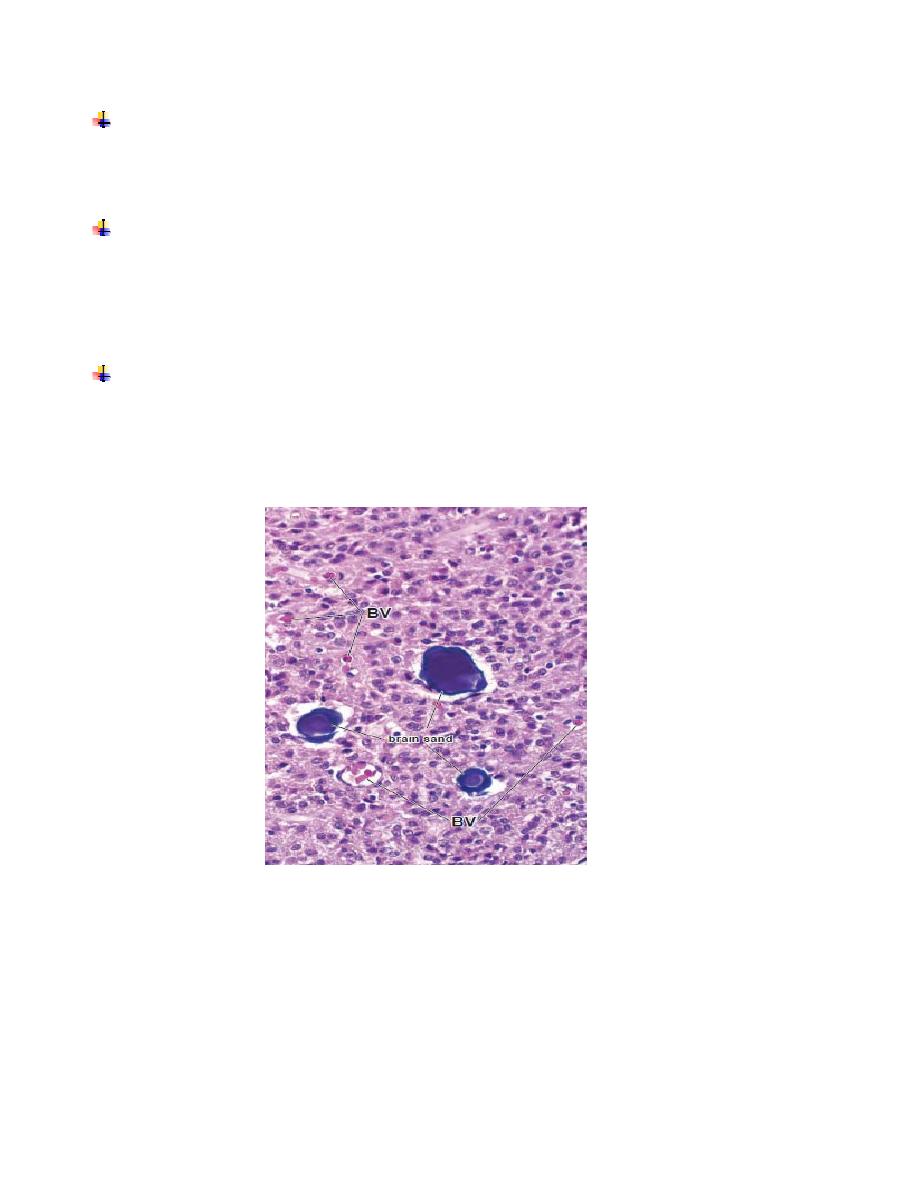
Pinealocytes
are the chief cells of the pineal gland. They are arranged in clumps or cords
within lobules formed by connective tissue septa that extend into the gland from the pia
mater that covers its surface.
The
interstitial (glial) cells
constitute about 5% of the cells in the gland. They have
staining and ultrastructural features that closely resemble those of astrocytes. In addition
to the two cell types, the human pineal gland is characterized by the presence of calcified
concretions, called
corpora arenacea
or
brain sand
(Fig. 1).
The human pineal gland relates light intensity and duration to endocrine
activity.The pineal gland is a photosensitive organ and an important timekeeper and
regulator of the day/night cycle (circadian rhythm).
Fig.(1)
•
Photomicrograph of human pineal gland. This higher-magnification photo micrograph
shows the characteristic concretions called brain sand or corpora arenacea.
Thyroid Gland:
The thyroid gland, located in the cervical region anterior to the larynx, consists of
two lobes united by an isthmus (fig.3).
It originates in early embryonic life from the foregut endoderm near the base of the
future tongue.
Its function is to synthesize the thyroid hormones: thynoxine (tetra-iodothyronin. or
T4)and tri-iodothyronine (T3), which are important for growth, for cell
differentiation, and for the control of the basal metabolic rate and oxygen
consumption in cells throughout the body.
Thyroid hormones affect protein, lipid, and carbohydrate metabolism .
The thyroid is composed of epithelial structures called thyroid follicles (fig.2)..
Each follicle consists of a simple epithelium and a central lumen filled with a
gelatinous substance called colloid .
Thyroid is the only endocrine gland in which a large quantity of secretory product is
stored . Moreover the accumulations is outside the cells, in the colloid of the follicles.
The thyroid gland is covered by a fibrous capsule from which septa extend into the
parenchyma , dividing it into lobules and carrying blood vessels, nerves, and
lymphatics.
Follicles are densely packed together, separated from one another only by sparse
reticular connective tissue (fig.2).
Follicular cells range in shape from squamous to low columnar and the follicles are
quite variable in diameter (fig.2).
The size and cellular features of thyroid follicles vary with their functional activity.
Active glands have more follicles of low columnar epithelium ; glands with mostly
squamous follicular cells are considered hypoactive.
Follicular epithelium contains two types of cells: follicular and parafollicular
cells.
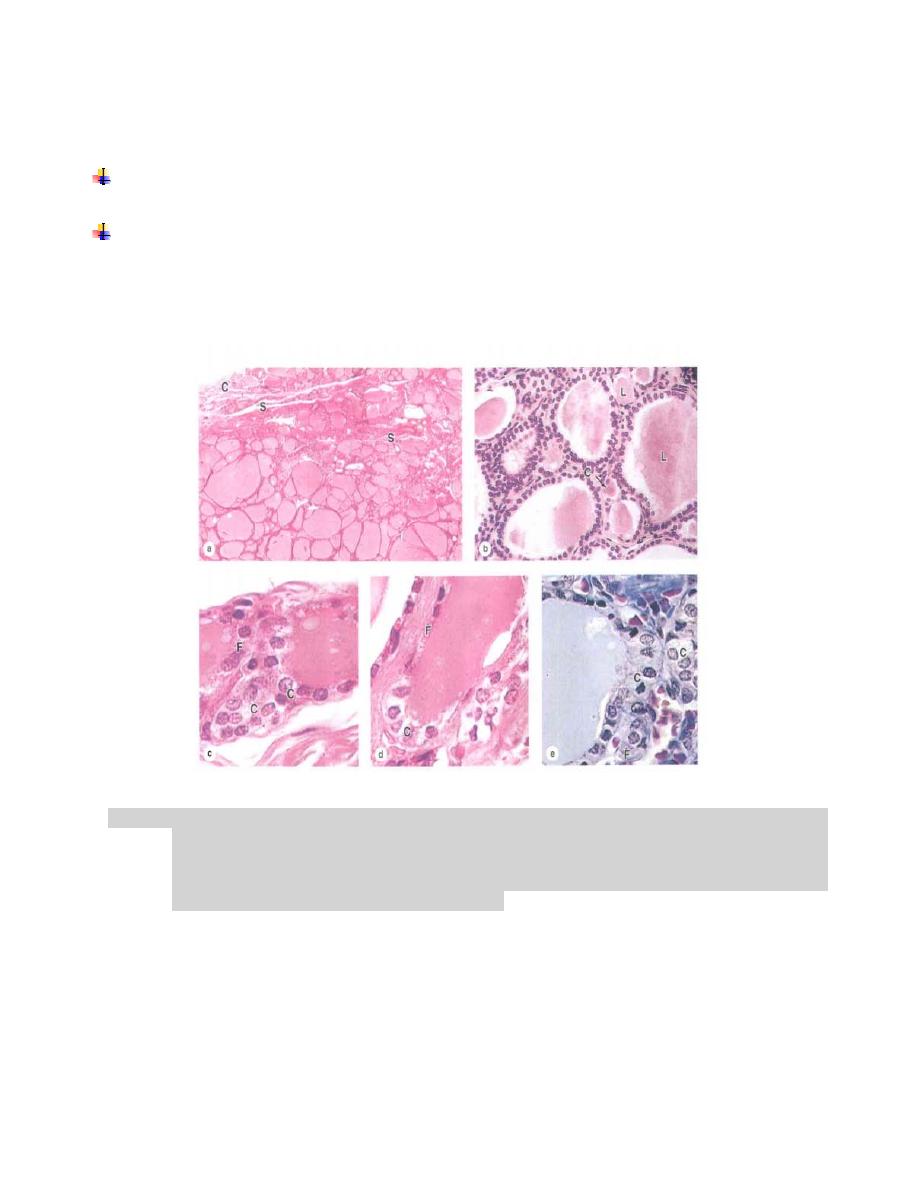
The parenchyma of the thyroid gland is composed of epithelium containing two types
of cells:
Follicular cells (principal cells)
are responsible for production of the thyroid
hormones T4 and T3, exhibit a slightly basophilic basal cytoplasm.
Parafollicular cells (C cells)
are located in the periphery of the follicular epithelium
and lie within the follicle basal lamina. These cells have no exposure to the follicle
lumen. They secrete
calcitonin
, pale staining and occur as solitary cells or small
clusters of cells.
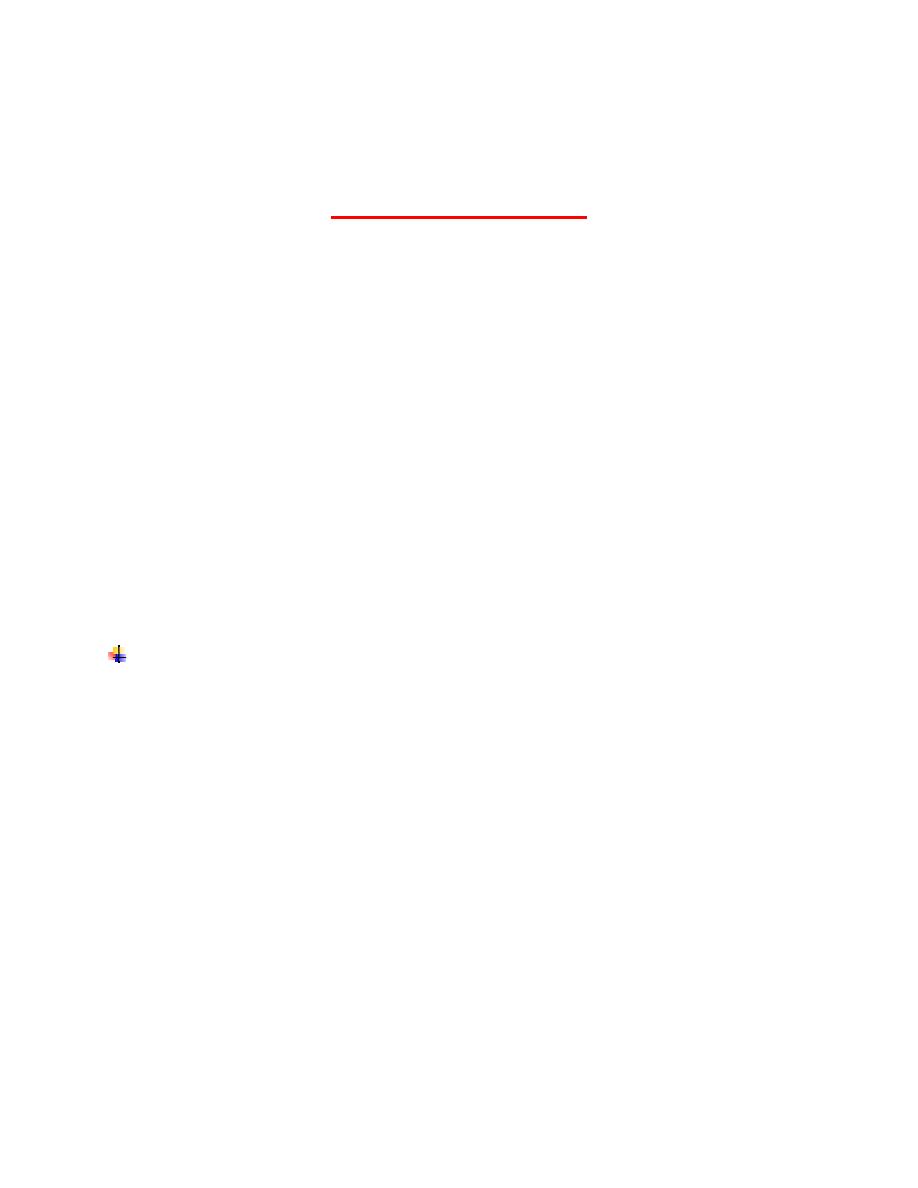
Figure (2). Thyroid gland .( a): A low-power micrograph of thyroid gland shows the thin capsule(C
), from which septa( S) with the larger blood vessels ,lymphatics and nerves enter the gland
. ( b):T he lumen( L) of each follicle is filled with colloid. (c,d,e) parafollicular cells (C)
which secrete calcitonin , may be part of the follicular epithelium or present in singly or in
groups outside of follicles follicular cells (F).
Parathyroid Glands:
The parathyroid glands are four small oval masses.
They are located on the back of the thyroid gland (fig.3), one at each end of the
upper and lower poles, usually embedded in the larger glandʾs capsule.
The parathyroid glands are derived from the pharyngeal pouches: the superior
glands from the fourth pouch and the inferior glands from the third pouch.
Each parathyroid gland is contained within a capsule which
sends septa into the gland, where they merge with reticular
fibers that support elongated cordlike clusters of secretory cells.
With increasing age many secretory cells are replaced with
adipocytes,
Two
types
of
cells
are
present
in
parathyroid
glands: chief (or principal) cells and oxyphil cells (fig.4).
The chief cells are small polygonal cells with round nuclei and
pale-staining
,slightly
acidophilic
cytoplasm
filled
with
irregularly shaped. These are secretory granules containing the
polypeptide parathyroid hormone (PTH).
Much smaller often clustered populations of oxyphil cells are sometime
present more commonly in older individuals (fig.4).
These are much larger than the principal cells and are
characterized
by
acidophilic
cytoplasm
filled
with
abnormally
shaped mitochondria Some oxyphilc ells show low levels of
PTH
synthesis
,suggesting
these
cells
are
transitional
derivatives from chief cells.
Parathyroid hormone targets osteoblasts.
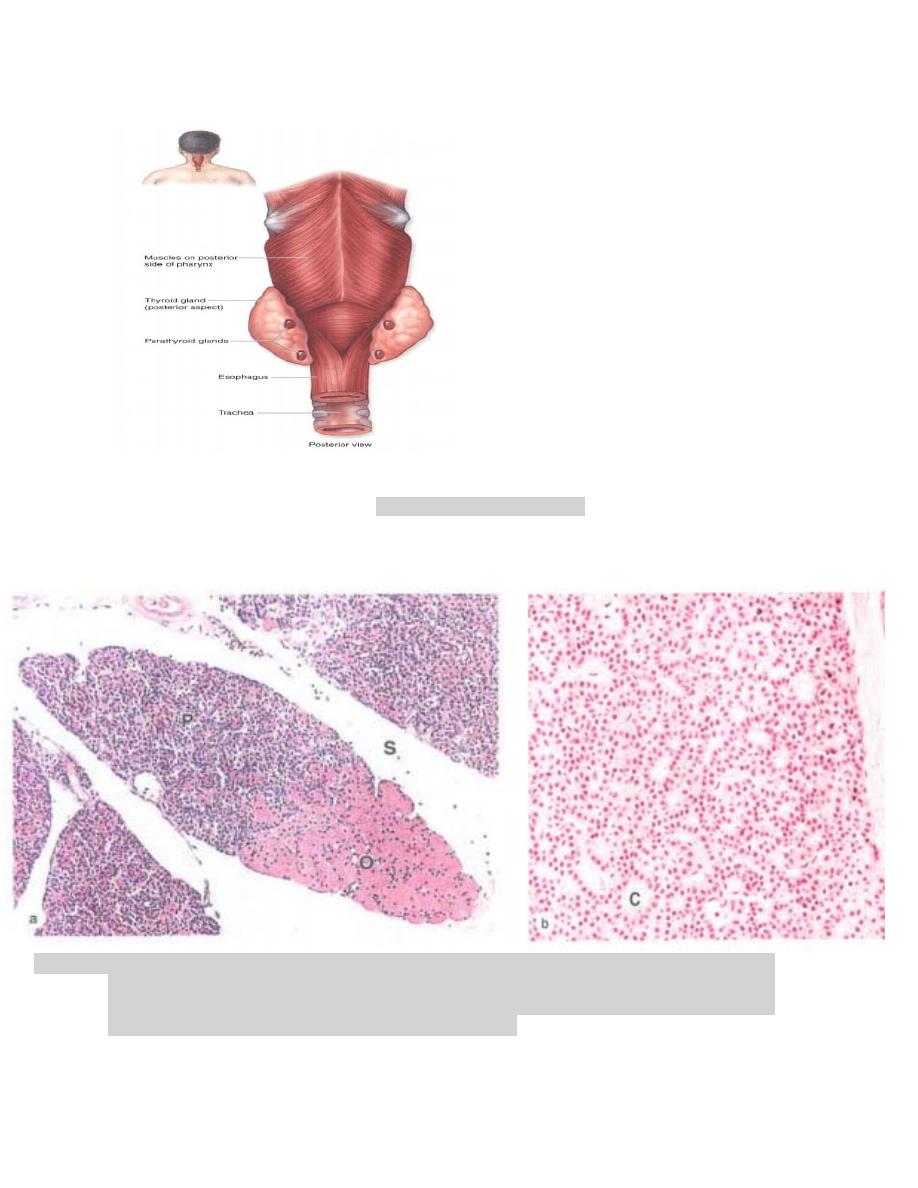
Figure (3). Parathyroid glands
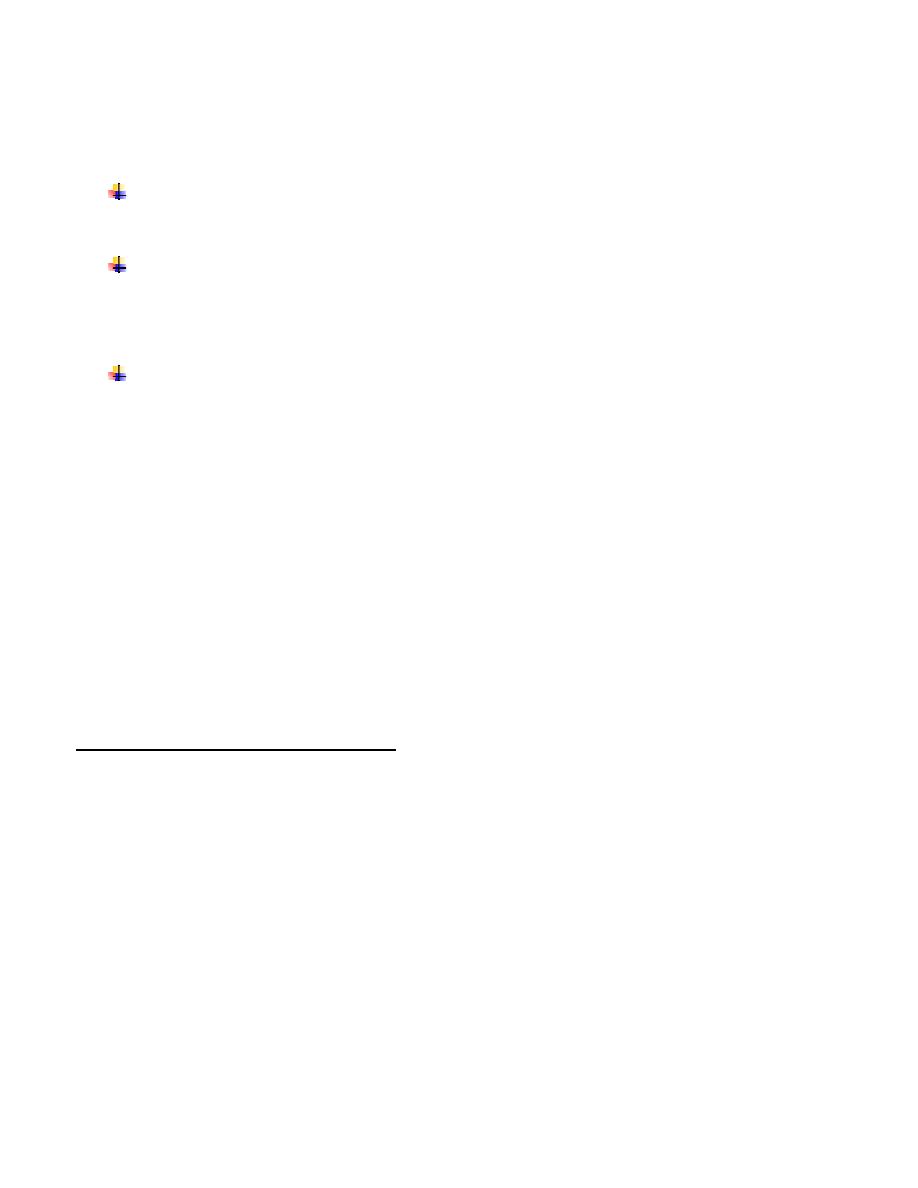
Figure (4). Parathyroid principal cells. (a): A small lobe of parathyroid gland surrounded by connective
tissue septa (s), shows mainly densely packed cords of small principal cells (P), also called
chief cells, oxyphil cells (O), ( b): The micrograph shows that principal cells are slightly
eosinophilic present in cords separated by capillaries( C)
Histology 2016-2017
Department of Anatomy &Histology:
Dr.Rajaa Ali
***********************************************************
Endocrine system part III
The
adrenal (suprarenal) glands
secrete both steroid hormones and
catecholamines.
They have a flattened triangular shape and are embedded in the perirenal fat at the
superior poles of the kidneys.
The adrenal glands are covered with a thick connective tissue capsule from which
trabeculae extend into the parenchyma , carrying blood vessels and nerves.
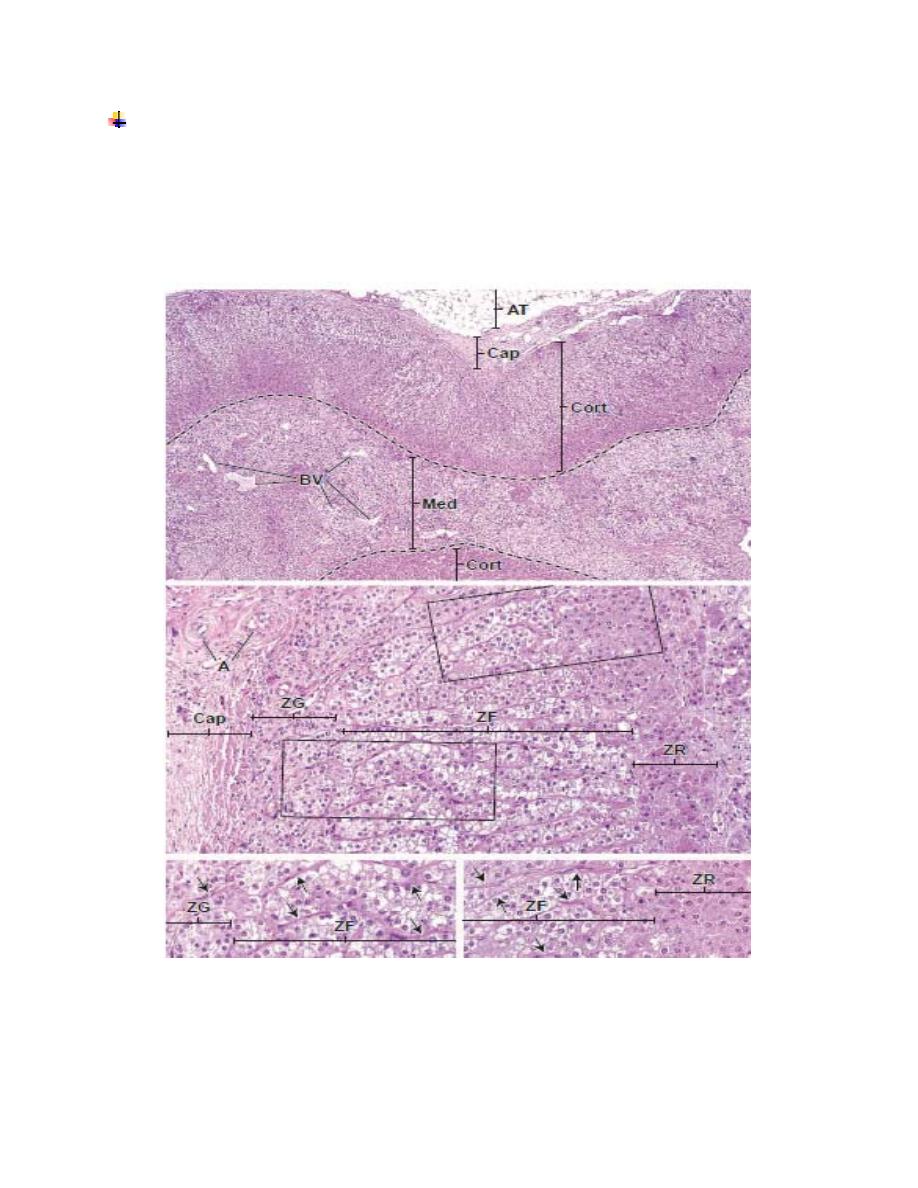
The secretory parenchymal tissue is organized into two distinct regions (Fig.1):
The
cortex
is the steroid-secreting portion. It lies beneath the capsule and
constitutes nearly 90% of the gland by weight.
The
medulla
is the catecholamine-secreting portion. It lies deep to the
cortex and forms the center of the gland.
Parenchymal cells of the cortex and medulla are of different embryologic origin.
Embryologically, the cortical cells originate from
mesodermal mesenchyme
,
whereas the medulla originates from
neural crest
cells that migrate into the
developing gland .
Although embryologically distinct, the two portions of the adrenal gland are
functionally related . The parenchymal cells of the adrenal cortex are controlled
in part by the anterior lobe of the pituitary gland and function in regulating
metabolism and maintaining normal electrolyte balance.
Blood Supply:
The
adrenal glands
are supplied with blood by the
superior, middle
, and
inferior suprarenal arteries
. These vessels branch before entering the capsule,
to produce many small arteries that penetrate the capsule. The vessels form a
system that consists of :
capsular capillaries
that supply the capsule.
fenestrated cortical sinusoidal capillaries
that supply the
cortex and then drain into the fenestrated modularly capillary
sinusoids.
medullary arterioles
that traverse the cortex, traveling within
the trabeculae , and bring arterial blood to the
medullary
capillary sinusoids
.
Lymphatic vessels
are present in the capsule and the connective tissue around the
larger blood vessels in the gland.
Cells of the Adrenal Medulla:
Chromaffin cells located in the adrenal medulla are innervated by
presynaptic sympathetic neurons.
The central portion of the adrenal gland, the
medulla
, is composed of a
parenchyma of large, pale-staining epithelioid cells called
chromaffin cells
(medullary cells)
, connective tissue, numerous sinusoidal blood capillaries, and
nerves.
The chromaffin cells are, in effect, modified neurons (Fig.1).
Numerous myelinated, presynaptic sympathetic nerve fibers pass directly to the
chromaffin cells of the medulla . When nerve impulses carried by the sympathetic
fibers reach the catecholamine-secreting chromaffin cells, they release their
secretory products.
Therefore, chromaffin cells are considered the equivalent of postsynaptic neurons.
However, they lack axonal processes.
Ganglion cells
are also present in the medulla. Their axons extend peripherally to
the parenchyma of the adrenal cortex to modulate its secretory activity and
innervate blood vessels.
Chromaffin cells of the adrenal medulla have a secretory function, the
catecholamines epinephrine and norepinephrine secreted by the chromaffin cells
are produced by different cell types:
One population of cells contains only large
dense core vesicles
.
These cells secrete norepinephrine.
The other population of cells
contains vesicles
that are smaller, more
homogeneous, and less dense. These cells secrete epinephrine.
Glucocorticoids secreted in the cortex induce the conversion of norepinephrine
to epinephrine in chromaffin cells. The catecholamines, in concert with the
glucocorticoids, prepare the body for the “fight-or-flight” response.
Zonation of the Adrenal Cortex:
The
adrenal cortex
is divided into three zones on the basis of the arrangement of
its cells (Fig.1):
•
Zona glomerulosa
, the narrow outer zone that constitutes up to 15% of the
cortical volume.
•
Zona fasciculata
, the thick middle zone that constitutes nearly 80% of the
cortical volume.
•
Zona reticularis
, the inner zone that constitutes only 5% to 7% of the cortical
volume but is thicker than the glomerulosa because of its more central location
Zona Glomerulosa:
The cells of the
zona glomerulosa
are arranged in closely packed ovoid clusters
and curved columns that are continuous with the cellular cords in the zona fasciculate ,
are relatively small and columnar or pyramidal. Their spherical nuclei appear closely
packed and stain densely.
The zona glomerulosa secretes aldosterone, which functions in the control of
blood pressure.
The cells of the zona glomerulosa secrete
mineralocorticoids
, compounds that
function in the regulation of sodium and potassium homeostasis and water balance. The
principal secretion,
aldosterone
, acts on the distal tubules of the nephron in the kidney,
the gastric mucosa, and the salivary and sweat glands to stimulate resorption of sodium
at these sites, as well as to stimulate excretion of potassium by the kidney.
Zona Fasciculata:
The cells of the
zona fasciculata
are large and polyhedral. They are arranged in
long straight cords, one or two cells thick, that are separated by sinusoidal capillaries.
The cells of the zona fasciculata have a lightly staining spherical nucleus. The principal
secretion of the zona fasciculata is glucocorticoids that regulate glucose and fatty acid
metabolism.
Zona Reticularis:
The zona reticularis produces glucocorticoids and androgens. The cells of the
zona reticularis
are noticeably smaller than those of the zona fasciculata, and
their nuclei are more deeply stained. They are arranged in anastomosing cords
separated by fenestrated capillaries. The cells have relatively few lipid droplets.
The cells in this zone are small because they have less cytoplasm than the cells in
the zona fasciculata; thus the nuclei appear more closely packed. They exhibit
features of steroid- secreting cells.
The principal secretions of the zona reticularis are weak androgens. The
principal secretion of the cells in the zona reticularis consists of weak
androgens
,
mostly
dehydroepiandrosterone (DHEA)
. The cells also secrete some
glucocorticoids, in much smaller amounts than those of the zona fasciculata.
Fig.(4): Adrenal gland A, arteries ; AT, adipose tissue ; BV, blood vessels ; Cap, capsule ; Cort,
cortex ; Med, medulla; ZF, zona fasciculate ; ZG, zona glomerulosa ; ZR, zona reticularis ;
arrows, connective tissue trabeculae ; dashed line, corticomedullary boundary.
