
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
1
Objectives
1. List and describe the layers of the GIT.
2. Outline the histological features of the three layers of submucosa of
submucosa .
3. Compare the local function and histological features of Meissner and
Auerbech plexuses.
4. Outline the different types of epithelium within oral cavity and link this
difference to functional adaptation.
5. Summarize the functional and histological structure of submucosal
gland.
6. Relate the functional to histological feature of muscularis externa alayer
esophagus in aprocess of swallowing.
7. Outline the structural and functional adaptats of the gastroesophageal
8. Outline the difference in histological features of outer layer of esophagus
along its caurse.
Digestive Tract: Introduction
The digestive system consists of the digestive tract; oral cavity, esophagus, stomach, small ,
large intestines, rectum, and anus and its associated glands; salivary glands, liver, gallbladder
and pancreas. Its function is to obtain the molecules necessary for the maintenance, growth, and
energy needs of the body from ingested food.
Large molecules such as proteins, fats, complex carbohydrates, and nucleic acids are broken
down into small molecules that are easily absorbed through the lining of the digestive tract,
mostly in the small intestine. Water, vitamins, and minerals are also absorbed from ingested food.
In addition, the inner layer of the digestive tract is a protective barrier between the content of the
tract's lumen and the internal milieu of the body.
The first step in the complex process known as digestion occurs in the mouth, where food is
moistened by saliva and ground by the teeth into smaller pieces; saliva also initiates the digestion
of carbohydrates. Digestion continues in the stomach and small intestine, where the food
transformed into its basic components (e.g, amino acids, monosaccharaides, free fatty acids,
monoglycerides) is absorbed. Water absorption occurs in the large intestine, causing the
undigested contents to become semisolid.
General Structure of the digestive
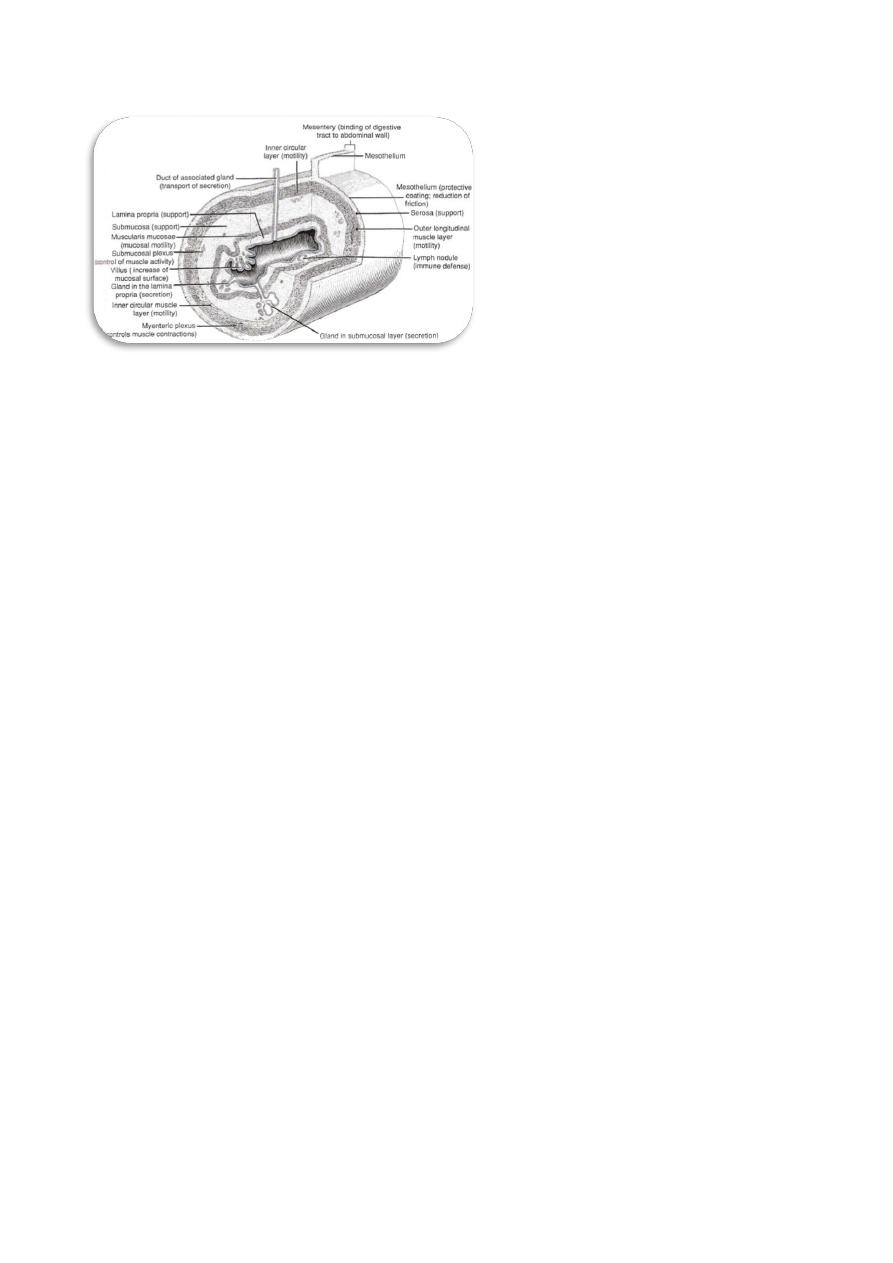
Based on its histological organization, the wall of the digestive tract can be divided into four
tunics (Fig.1).
1. Mucosa is the innermost layer of the digestive wall. It includes epithelium, lamina propria, and
muscularis mucosae.

anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
2
a. The epithelium consists of simple columnar epithelium lining most of the tract and
stratified squamous epithelium lining the two ends, the esophagus and anal canal.
b. The lamina propria is a loose connective tissue that contains abundant ground substance,
many fibers, and numerous connective tissue cells such as fibroblasts, macrophages, mast
cells, plasma cells, and leukocytes.Various types of glands are found in the lamina propria
depending on the region of the digestive tract.
c. The muscularis mucosae is a very thin layer of smooth muscle, which is the boundary
between the mucosa and the submucosa. It is usually arranged in an inner circular and
outer longitudinal layer. However, the muscularis mucosae varies in different regions, and
it is often diffi cult to distinguish between the muscle layers.
2. Submucosa is a thick layer of dense irregular connective tissue ,this layer contains blood
vessels, lymphatic vessel and submucosal (Meissner) plexuses, which contain nerve fibers and
neurons of the enteric nervous system. In some regions of the digestive tract, this layer is
characterized by mucous glands or lymphatic nodules.
3. Muscularis externa is composed of two or three oblique, circular, and longitudinal muscle
layers, which vary from region to region. Most of the muscularis externa consists of smooth
muscle fibers, but the upper and middle esophagi contain some skeletal muscle. The myenteric
(Auerbach) plexuses (nerve fibers and neurons of the enteric nervous system) are located
between the muscle layers. They innervate and control contraction of the muscularis externa.
4. Serosa and adventitia are coverings of the outermost wall of the digestive tract. Most parts of
the digestive tract are covered by serosa, a thin layer of loose connective tissue lined by
mesothelium. The mesothelium produces a lubricating fluid that reduces friction during
movement of the organs against each other ,
The serosa is the visceral layer of the peritoneum and covers the wall of the digestive
tract where it connects to the mesentery in the peritoneal cavity (intraperitoneal organs).
The adventitia is a layer of loose connective tissue without mesothelium that covers the
upper region of the esophagus, part of the duodenum, and the lower part of the digestive
tract, such as the rectum and anal canal. Adventitia covers regions of the digestive tract
where it is connected to other organs or to the body wall (e.g., retroperitoneal organs).
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
3
(Figure ,1): The structure of a portion of the digestive tract with various layers and
components and their function.
Oral Cavity
The oral cavity is lined with stratified squamous epithelium, which may be keratinized,
partially keratinized,or nonkeratinized depending on the location
masticatory mucosa is the keratinized cell layers resist damage from abrasion and are
best developed on the gingiva (gum) and hard palate. The lamina propria in these
regions rests directly on the periosteum of underlying bone.
lining mucosa is Nonkeratinized squamous epithelium predominates in the over the
soft palate, cheeks, the floor of the mouth, and the pharynx,the posterior region of
the oral cavity leading to the esophagus. Lining mucosa overlies a thick submucosa
containing many minor salivary glands, which secrete continuously to keep the mucosal
surface wet, and diffuse lymphoid tissue. Throughout the oral cavity, the epithelium
contains transient antigen-presenting cells and rich sensory innervation.
The lips
The central core of the lip contains the orbicularis oris (skeletal) muscle, which is
innervated by the facial nerve , and contributes to lip movement and facial expressions.
The Lips are divided into the three regions:
A.
external (skin) region It is covered by keratinized stratified squamous epithelium.
The sebaceous glands in the dermis are associated with hair follicles, and sweat
glands are present. The skin of the lip is like thin skin and can be divided into
epidermis and dermis.
B.
The vermilion zone of the lip is covered by parakeratinized stratified squamous
epithelium. Sebaceous glands (Fordyce granules or spots) may be found in the
connective tissue and are not associated with hair follicles. These glands have ducts
that release their oily product directly onto the surface of the lip. The vermilion zone
appears red because of many blood vessels near the surface of the thin and
translucent epithelium . This region can become thick and forms the sucking pad in
infants.
C.
Internal region (labial mucosa) of the lip is an example of lining mucosa, which
is covered by nonkeratinized stratified squamous epithelium and contains many
elastic fibers; it is very flexible and can be stretched. Its submucosa layer contains

anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
4
many minor salivary glands (mucous glands). The minor salivary glands in the lips
are often called labial glands.
The palate
It is divided into an anterior hard palate (possessing a bony shelf in its core) and
aposterior soft palate (possessing skeletal muscle in its core). The palate separates the nasal
cavity from the oral cavity. Therefore, the palate has a nasal aspect and an oral aspect. The
entire nasal aspect of the palate (with the exception of the uvula) is lined by
pseudostratified ciliated columnar epithelium (respiratory epithelium).
1. The hard palate is lined on its oral aspect by stratified squamous parakeratinized
to stratified squamous keratinized epithelium (masticatory mucosa). it contains
adipose tissue anteriorly and minor mucous salivary glands posteriorly in the oral
aspect of its connective tissue, the lamina propria in these regions rests directly on
the periosteum of underlying bone.
2. The soft palate is lined on its oral aspect by stratified squamous nonkeratinized
epithelium(lining mucosa). It contains minor mucous salivary glands in the oral
aspect of its connective tissue.
Tongue
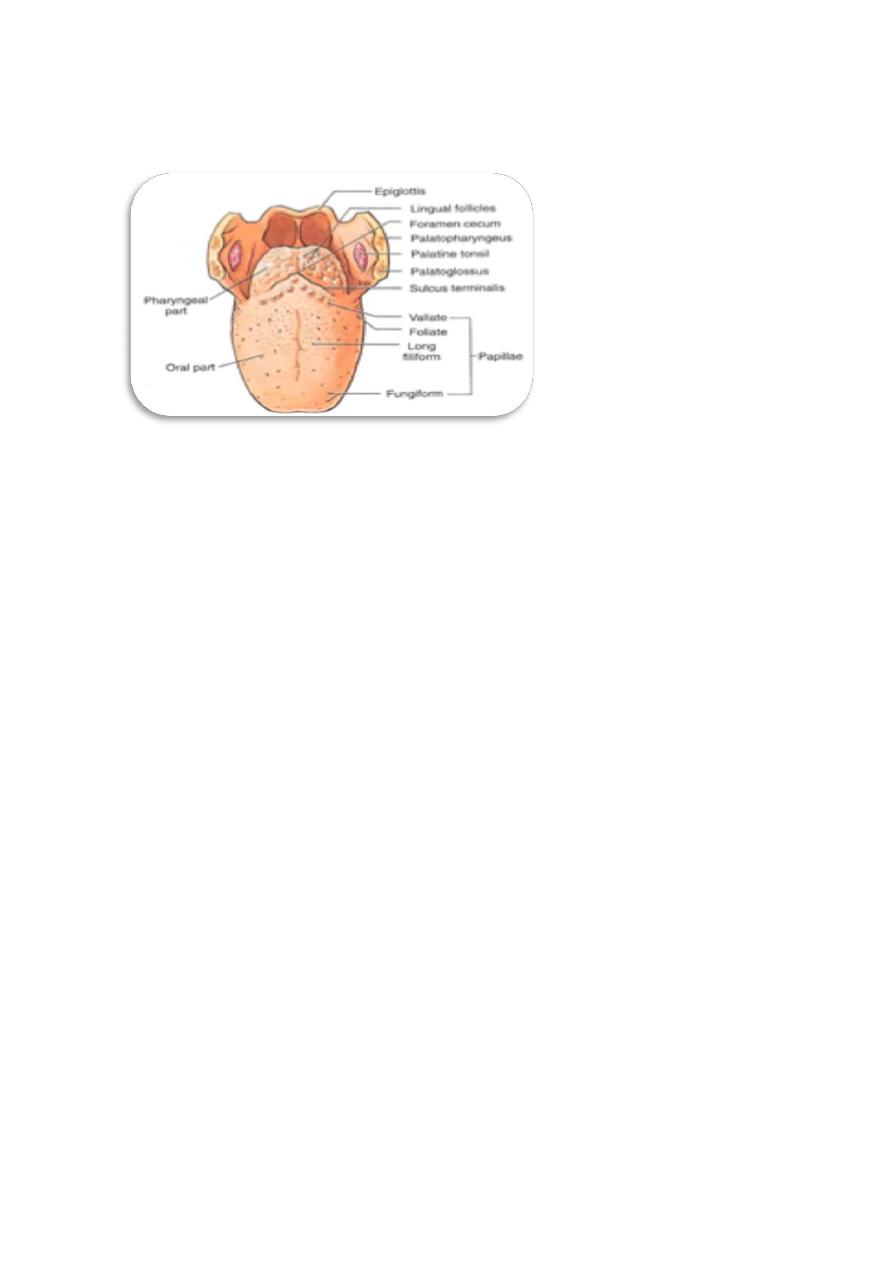
The tongue is divided into an anterior two-thirds(papillary area) and a posterior one-
third(tonsillar area) by the V-shaped sulcus terminalis, whose apex ends in the foramen
cecum(Fig,2). Its dorsal surface is covered by specialized mucosa stratified squamous
parakeratinized to keratinized epithelium, whereas its ventral surface is covered by
stratified squamous nonkeratinized epithelium. Both epithelial surfaces are underlain by a
lamina propria and submucosa of dense irregular collagenous connective tissue. The tongue
possesses a core of skeletal muscle, which forms the bulk of the tongue.
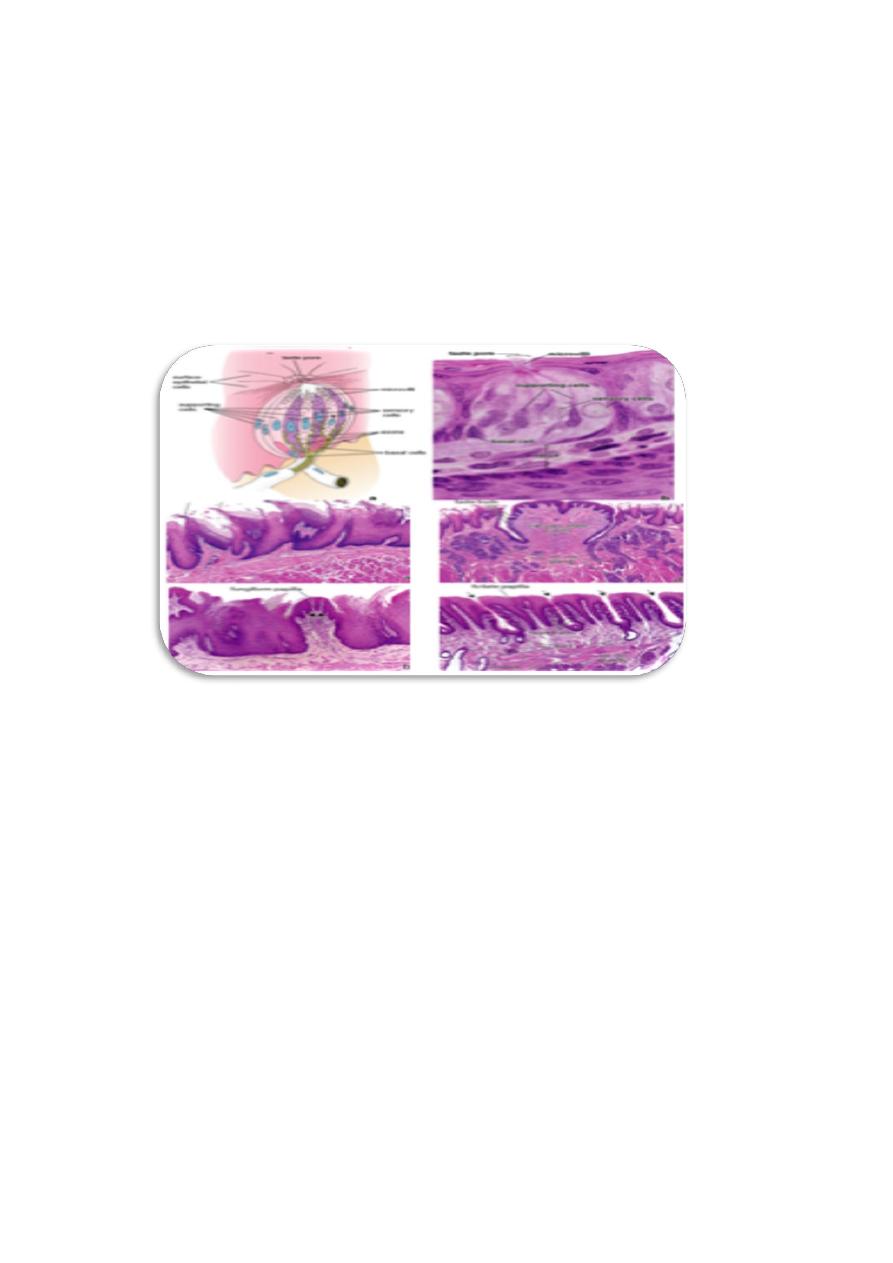
They are four types of lingual papilla(Fig,3).
1. Filiform papillae are the smallest and most numerous of the four types of papillae. They cover
almost the entire superior surface of the anterior two thirds of the tongue and are packed in rows
that parallel the sulcus terminalis. Each of the papillae appears cone shaped with some branching
processes. Connective tissue forms the central core of each papilla. Filiform papillae have no
taste buds and extend from the nonkeratinized stratified squamous epithelium. The surface of the
papilla is keratinized and is exposed to a great deal of abrasion .
2. Fungiform papillae are less numerous than the filiform papillae. They are mushroom shaped
and are scattered among the filiform papillae .Fungiform papillae are located at the tip and on the
two lateral edges of the tongue. They are more numerous near the tip of the tongue. Taste buds
are found on the apical surfaces of fungiform papillae.
3. Circumvallate papillae are large and round with a flat topped cylindrical structure. There are
about 10 to 14 papillae arranged in a row along the sulcus terminalis. Each papilla is surrounded
by a deep groove (moat), which forms a valley around the papilla. Taste buds are found in the
lateral walls of each papilla .
4. Foliate papillae are leaf like folds with flat tops and have deep clefts between the papillae.
They are located on the posterior lateral surface of the tongue. They are more prominent in some
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
5
animals (such as rabbits) than in humans. Foliate papillae contain taste buds in the lateral walls of
the papillae.
(Figure ,2): Surface of the tongue on the region close to its V-shaped boundary, between the
anterior and posterior portions. Note the lymphoid nodules (lingual tonsil), glands, and
papillae.
Taste buds
Taste buds are present on fungiform, foliate, and circumvallate papillae. In
histologic sections, taste buds appear as oval, pale-staining bodies that extend through the
thickness of the epithelium .A small opening onto the epithelial surface at the apex of the
taste bud is called the taste pore. Three principal cell types are found in taste buds:
•
Neuroepithelial (sensory) cells gustatory (taste) cells,
are the most numerous cells in the
taste bud. These elongated cells extend from the basal lamina of the epithelium to the taste
pore, through which the tapered apical surface of each cell extends microvilli. At their base
they form a synapse with the processes of afferent sensory neurons. The turnover time of
neuroepithelial cells is about 7-10 days.
•
Supporting cells are less numerous. They are also elongated cells that extend from the
basal lamina to the taste pore. Like neuroepithelial cells, they contain microvilli on their
apical surface and possess tight junctions, but they do not synapse with the nerve cells. The
turnover time of supporting cells is also about 10 days.
• Basal cells(stem cells) are small cells located in the basal portion of the taste bud, near the
basal lamina. They are the stem cells for the two other cell types, these cells have ability to
division and differentiation to another type of cells(Fig,3).
Function.
Taste buds detect at least five broad categories of tastants: sodium ions (salty);
hydrogen ions from acids (sour); sugars and related compounds (sweet); alkaloids and
certain toxins (bitter); and amino acids such as glutamate and aspartate (umami; Jap.
umami, savory). Salt and sour tastes are produced by ion channels and the other three
taste categories are mediated by G-protein–coupled receptors. Receptor binding produces
depolarization of the gustatory cells, stimulating the sensory nerve fibers that send
information to the brain for processing. Conscious perception of tastes in food requires
olfactory and other sensations in addition to taste bud activity.
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
6
In Glands of von Ebner are minor salivary glands that deliver their serous secretion
into the furrow surrounding each papilla, assisting the taste buds in perceiving stimuli. These
glands also deliver their saliva into the furrows of the foliate papillae.
The muscular core of the tongue is composed of bundles of skeletal muscle fibers
arranged in three planes with minor salivary glands interspersed among them.
Connective tissue between the small fascicles of muscle is penetrated by the lamina
propria, which makes the mucous membrane strongly adherent to the muscular core.
1. A lingual tonsil is located on the dorsal surface of the posterior one-third of the
tongue.
(Figure ,3): The lingual papilla(four types) and taste buds.
Summary of Structures of the Oral Mucosa
I. Lining mucosa (covering of inner surface of the lips and cheeks, soft palate, inferior
surface of the tongue, and floor of the mouth)
A. Epithelium: nonkeratinized stratified squamous epithelium
B. Lamina propria: connective tissue with many elastic fibers and few collagen fibers
C. Submucosa: connective tissue with minor salivary glands and their ducts
II. Masticatory mucosa (covering of gingiva and hard palate)
A.
Epithelium: keratinized stratified squamous epithelium
B.
B. Lamina propria: connective tissue with few elastic fibers and many dense
collagen fibers
C. No submucosa
III. Specialized mucosa (tongue)
A. Filiform papillae: no taste buds
B. Fungiform papillae: taste buds on apical surface of the papilla—sweet, sour, salty
C. Circumvallate papillae: taste buds in lateral wall of the papilla—bitter and contain
the serous gland in the base called Von Ebner gland.
D. Foliate papillae: taste buds in lateral wall of papilla
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
7
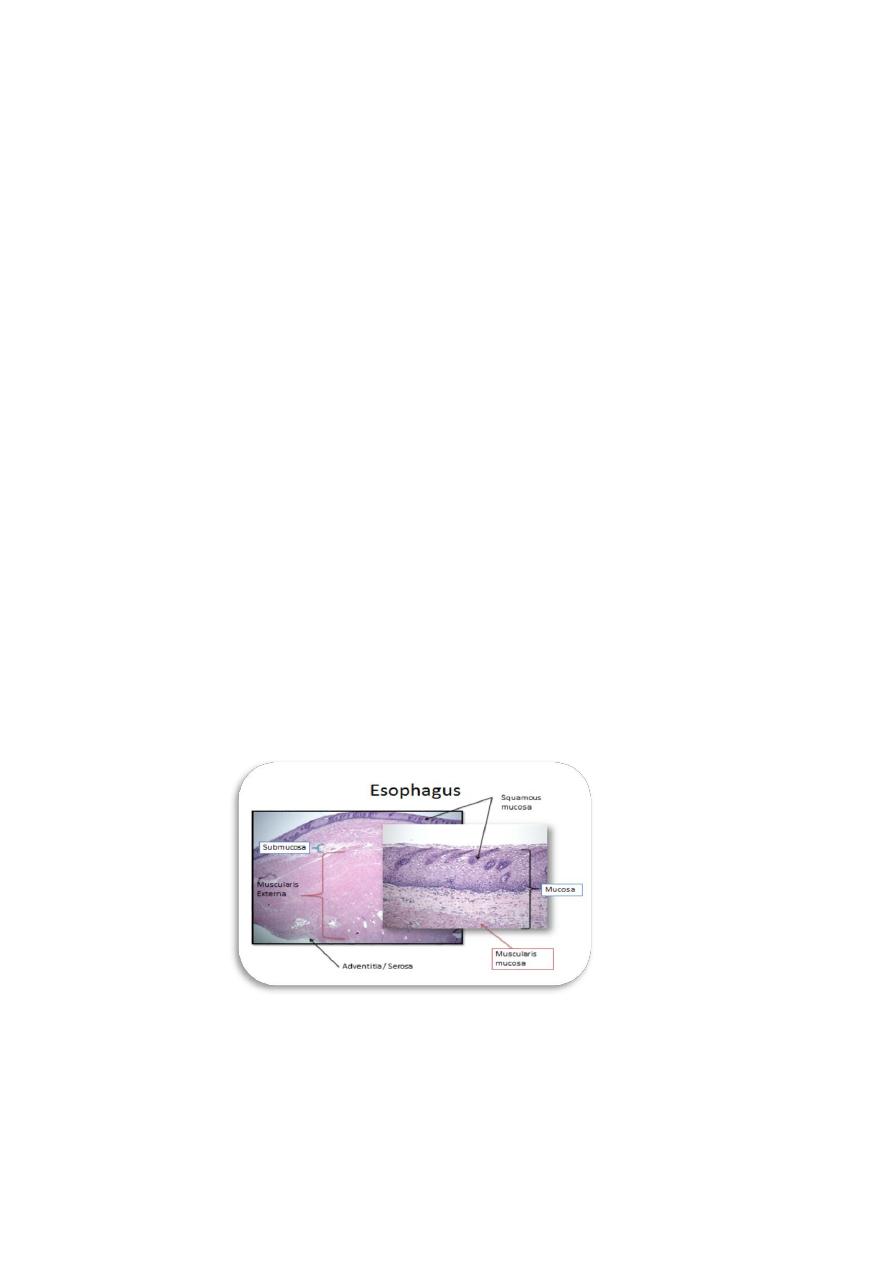
Esophagus
The esophagus is the upper part of the digestive tract, connecting the oral cavity to the
stomach. The major function of the esophagus is to provide passage for food from the mouth
to the stomach. The luminal surface of the esophagus is lined by nonkeratinized stratified
squamous epithelium. Mucous glands called esophageal glands are located in the
submucosa of the esophagus. The muscularis externa consists of two layers of muscle: inner
circular and outer longitudinal layers. Both skeletal and smooth muscle fibers are found in
the muscularis externa of the esophagus. The proportions of skeletal and smooth muscle
fibers are different in different regions of the esophagus. Swallowing begins with
voluntary muscle action but finishes with involuntary peristalsis
The esophagus can be divided into three regions:
The upper esophagus, middle esophagus, and lower esophagus(Fig,4).
1. The upper esophagus connects the oropharynx to the middle esophagus,this
segment contains numerous esophageal glands in the submucosa. these glands
secrete mucus to lubricate the esophageal wall so that food will pass through
easily, the upper esophagus contains only skeletal muscle fibers in the muscularis
externa. These are voluntary muscle fibers and are innervated by the
glossopharyngeal nerve (cranial nerve ).
2. The middle esophagus has mucosa similar to that of the upper esophagus, the
esophageal glands in the submucosa are less numerous than in the upper
esophagus ,the muscularis externa contains both skeletal and smooth muscles.
3. The lower esophagus connects the esophagus to the cardiac of the stomach,this
region contains large numbers of mucous glands in the lamina propria and
submucosa,these are called esophageal cardiac glands and produce mucous
secretions to protect the lower esophagus from being damaged by reflux of acidic
gastric juices from the stomach, the lower esophagus contains only smooth
muscle fibers in the muscularis externa, these are controlled by the enteric
branches of the vagus nerve.
(Figur,4):The four layers of esophageal wall include mucosa, submucosa,muscularis
externa and serosa /adventitia.

anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
Date:5-7/10/2016
8
