The physiology of thyroid gland
ﺩ.ﺑﺎﻥ ﺟﺎﺑﺭ
Objectives :
■
Describe the structure of the thyroid gland and how it relates to its function.
■
Define the chemical nature of the thyroid hormones and how they are synthesized.
■
Describe the role of protein binding in the transport of thyroid hormones and peripheral metabolism.
■
Identify the role of the hypothalamus and pituitary in regulating thyroid function.
■
Define the effects of the thyroid hormones in homeostasis and development.
■
Understand the basis of conditions where thyroid function is abnormal and how they can be treated.
The thyroid gland
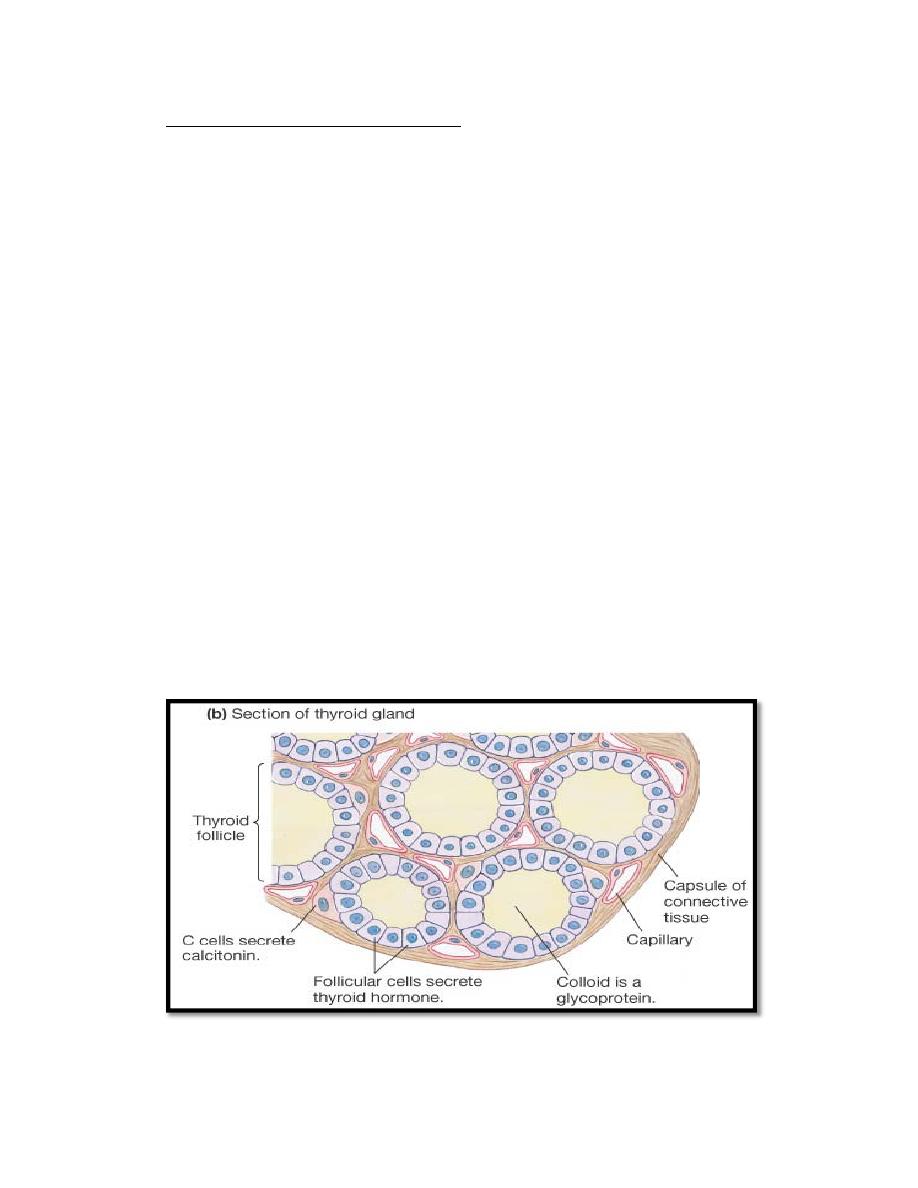
The thyroid gland, located immediately below the larynx on each side of
and anterior to the trachea. The thyroid gland is composed, of closed
follicles (figure 1) filled with a secretory substance called colloid and
lined with cuboidal epithelial cells ( called Follicular cells or Principle
cells) that secrete into the interior of the follicles. The major constituent
of colloid is the large glycoprotein thyroglobulin, which contains the
thyroid hormones (thyroxin (T4) and Triiodothyronine (T3). ) .In addition
to Follicular cells, the thyroid contain small number of parafollicular cells
(also called C‐cell), embedded inside the basal lamina surrounding the
follicle which secrete calcitonin. The thyroid gland has a blood flow
about five times the weight of the gland each minute.
Figure 1 Histology of thyroid gland

Synthesis and Secretion of the Thyroid Metabolic Hormones
About 93 % of the metabolically active hormones secreted by the
thyroid gland is T4, and 7 % T3 . However, almost all the T4 is eventually
converted to T3 in the tissues, so both are functionally important. The
functions of these two hormones are qualitatively the same, but they
differ in rapidity and intensity of action. T3 is about four times as potent
as T4, but it is present in the blood in much smaller quantities and
persists for a much shorter time than does T4. why??
Synthesis of thyroid hormones
The steps involved in synthesis of thyroid hormones(figure 2) are:
1.
Synthesis and secretion of thyroglobulin precursor.
The thyroid cells are typical protein secreting glandular cells. The
endoplasmic reticulum and Golgi apparatus synthesize and secrete into
the follicles a large glycoprotein molecule called thyroglobulin. Each
molecule of thyroglobulin contains about 70 tyrosine amino acids, and
they are the major substrates that combine with iodine to form the
thyroid hormones.
2.
Iodide Trapping
Iodides ingested orally are absorbed from the gastrointestinal tract into
the blood, most of the iodides are rapidly excreted by the kidneys, but
only about one fifth are selectively removed from the circulating blood
by the cells of the thyroid gland .
The basal membrane of the thyroid cell has the specific ability to pump
the iodide actively to the interior of the cell. This is achieved by the
action of a sodium‐iodide symporter. The energy for transporting iodide
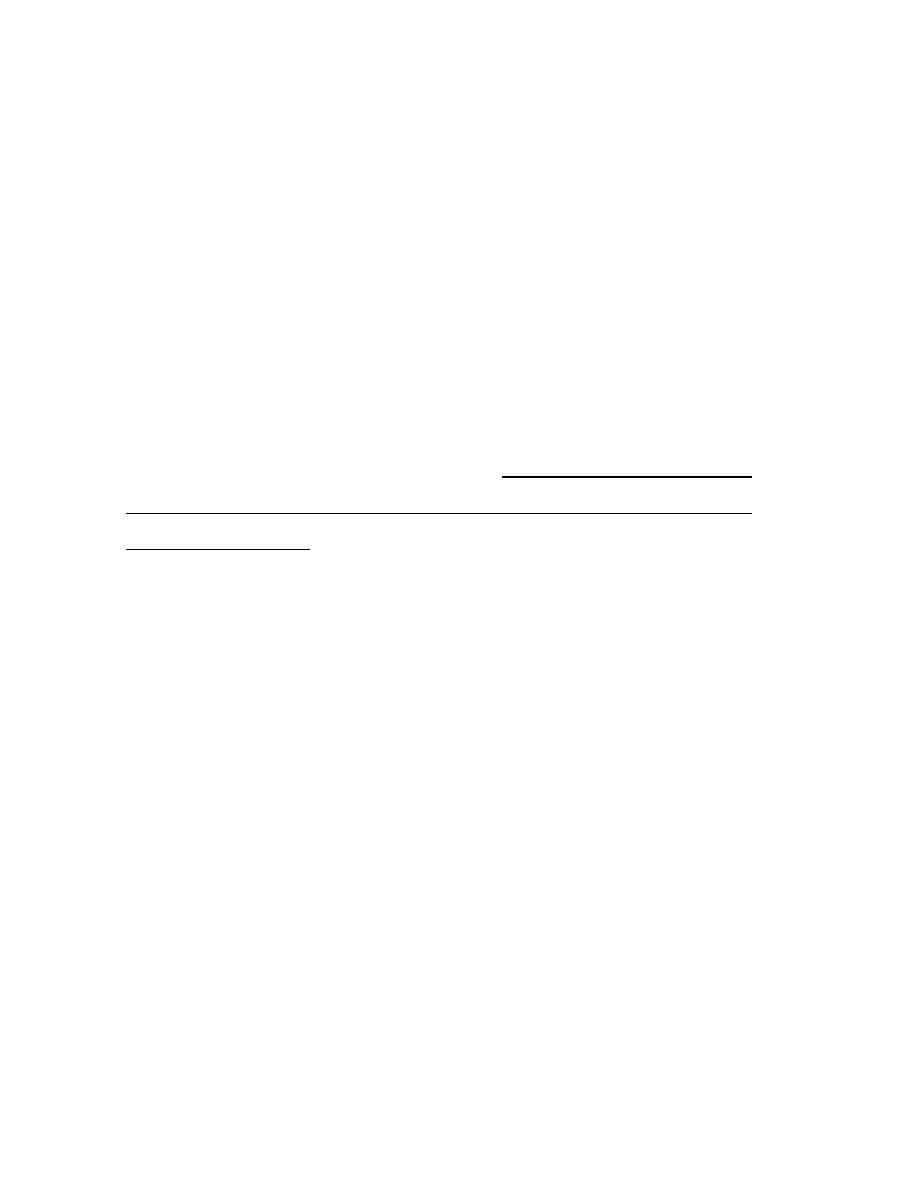
against a concentration gradient comes from …….?????
This process of concentrating the iodide in the cell is called iodide trapping.
Iodide is transported out of the thyroid cells across the apical membrane into
the follicle by a chloride‐iodide ion counter‐transporter molecule called
pendrin
.
3.
Oxidation of the Iodide Ion
The first essential step in the formation of the thyroid hormones is
conversion of the iodide ions to an oxidized form of iodine that is then
capable of combining directly with the amino acid tyrosine. This oxidation of
iodine is promoted by the enzyme peroxidase. When the peroxidase system is
blocked or hereditarily absent from the cells, the rate of formation of thyroid
hormones falls to zero.
4. Organification" of Thyroglobulin
The binding of iodine with the thyroglobulin molecule is called organification
of the thyroglobulin. Oxidized iodine will bind directly but slowly with the
amino acid tyrosine. Tyrosine is first iodized to monoiodotyrosine (MIT)and
then to diiodotyrosine(DIT).
5.
Coupling reaction
The iodotyrosine residues become coupled with one another. The major
hormonal product of the coupling reaction is T
4
, which is formed when two
molecules of DIT are joined together. Or one molecule of MIT couples with
one molecule of DIT to form T
3
. Small amounts of reverse T
3
(RT
3
) are formed
by coupling of DIT with MIT, but RT
3
does not appear to be of functional
significance in humans.

Storage of Thyroglobulin
The thyroid gland is able to store large amounts of hormone as thyroglobulin
molecule which contain up to 30 T4 molecules and a few T3 molecules Which
is sufficient to supply the body with its normal requirements of thyroid
hormones for 2 to 3 months.
Secretion of thyroid hormone
The thyroid cells sends out pseudopod extensions that close around small
portions of the colloid to form pinocytic .Then lysosomes in the cell cytoplasm
immediately fuse with these vesicles to form digestive vesicles. Multiple
proteases enzymes digest the thyroglobulin molecules and release T4 and T3
in free form. These then diffuse through the base of the thyroid cell into the
surrounding capillaries.
Some of the iodinated tyrosine in the thyroglobulin never become thyroid
hormones but remain MIT and DIT which not secreted into the blood.
Instead, their iodine is cleaved from them by a deiodinase enzyme that makes
all this iodine available again for recycling within the gland for forming
additional thyroid hormones.
About one half of the T4 is slowly deiodinated by 5'deiodinase enzyme to
form additional T3. Therefore, the hormone finally delivered to and used by
the tissues is mainly T3, a total of about 35 micrograms of T3 per day. At the
end , the remaining hormone are conjugated in the liver and released with
bile.
(Figure 2):The steps involved in synthesis of thyroid hormones
Transport of T4 and T3 to Tissues
On entering the blood, more than 99 % of the T4 and T3 combines
immediately with several of the plasma proteins, all of which are synthesized
by the liver. They combine mainly with thyroxin‐binding globulin and much
less with thyroxin‐binding prealbumin and albumin. Only free and albumin‐
bound thyroid hormone is biologically available to tissues.
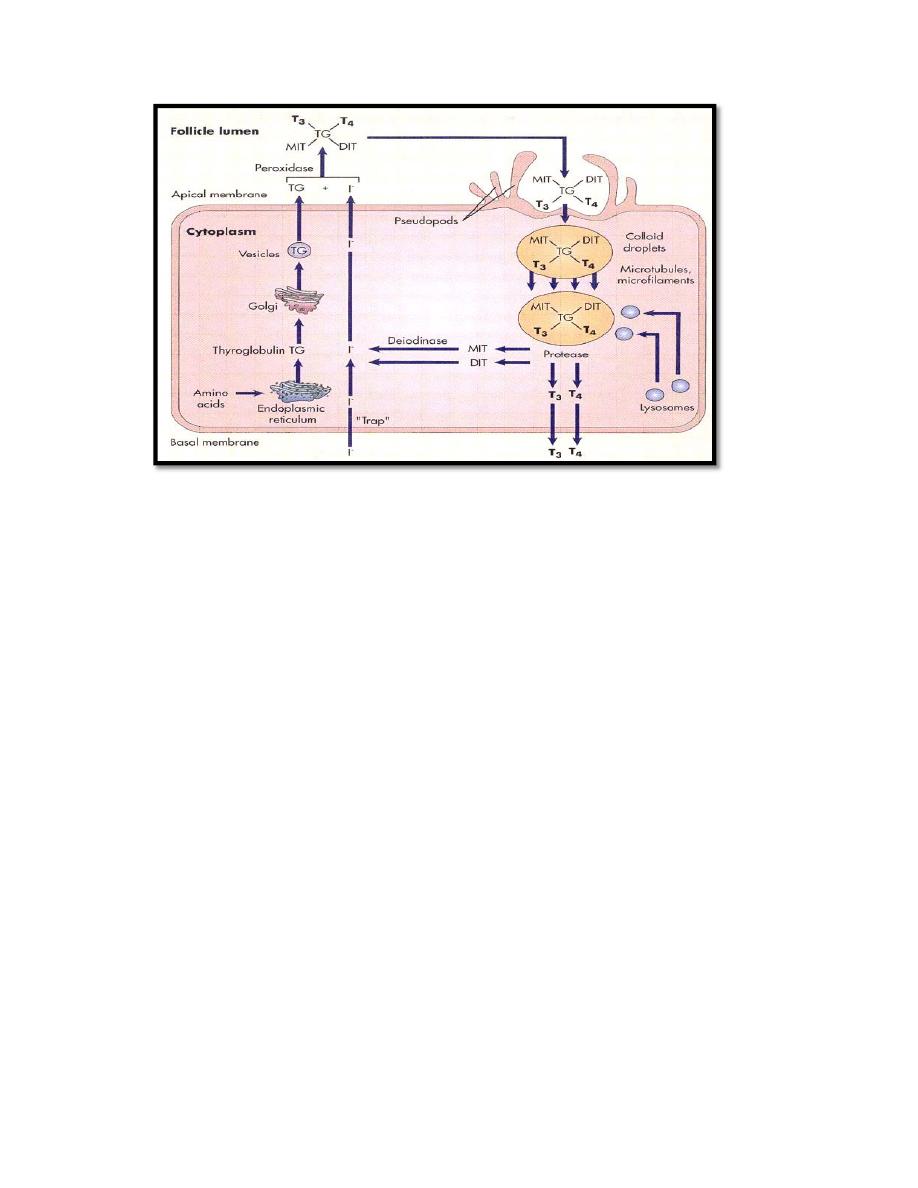
Mechanism of action
Receptors for thyroid hormones are nuclear type and its affinity is ten times
higher for T
3
than T
4
. Free thyroid hormone receptor (TR) without bound
hormone is bound to hormone response element of DNA (HRE) and
corepressor (CoR).After binding T
3
to receptor ‐ CoR is liberated and
coactivators (CoA) is bound and the transcription to mRNA begins(figure 3).
Thyroid hormones also appear to have nongenomic cellular effects that are
independent of their effects on gene transcription. Nongenomic actions of
thyroid hormone include the regulation of ion channels and oxidative
phosphorylation and appear to involve the activation of intracellular
secondary messengers such as cyclic AMP.
Figure 3: Mechanism of action of thyroid hormone
Regulation of thyroid hormone
The thyroid gland is part of the hypothalamic‐pituitary‐thyroid axis(figure 4).
Thyroid‐releasing hormone (TRH) from the hypothalamus stimulates
thyroid‐stimulating hormone (TSH) from the anterior pituitary gland, which
stimulates thyroid hormone release.
(TRH is also a potent stimulator of other
Hormone release from the pituitary?)
.
Thyroid‐stimulating hormone is a peptide hormone with one α‐chain and one
β‐chain.TSH acts through cyclic AMP mechanism.
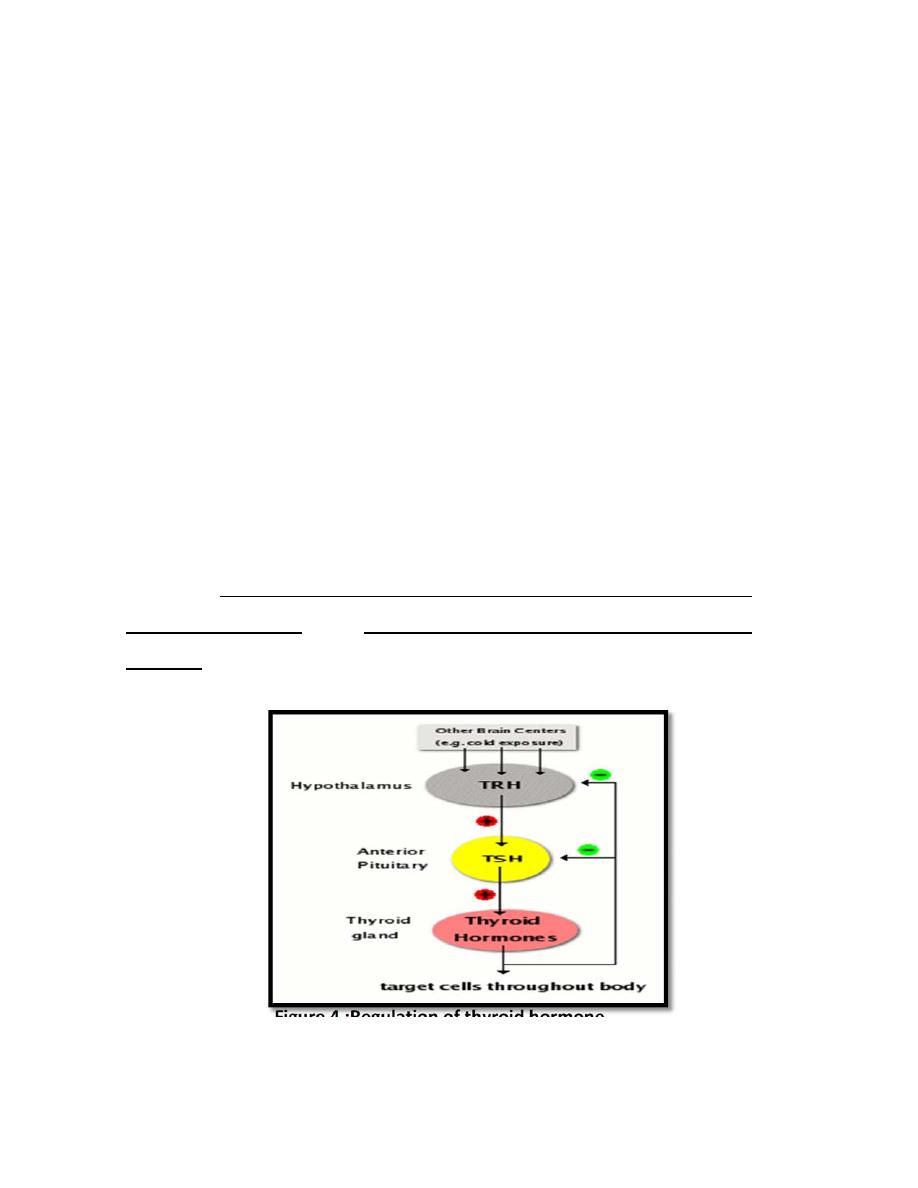
Binding of TSH to receptors on the membrane of thyroid epithelial cells
seems to:
stimulate all steps of thyroid hormone synthesis & release.
increase the size & vascularity of thyroid gland. Follicular cells
becomes columnar & active.
Prolonged stimulation of the gland by TSH‐‐‐‐‐‐>↑ size (hypertrophy) & number
(hyperplasia) of follicular cells ‐‐‐‐‐‐‐> enlargement of thyroid gland (goiter).
As blood concentrations of thyroid hormones increase, they inhibit both TSH
and TRH, leading to inhibit of thyroid epithelial cells. Later, when blood levels
of thyroid hormone have decayed, the negative feedback signal fades, and
the system wakes up again.
A number of other factors have been shown to influence thyroid hormone
secretion , Excess iodide intake, Stress, Somatostatin ,Glucocorticoids and
Dopamine inhibits it while exposure to a cold environment increase its
secretion
through their effect on TRH secretion from hypothalamus.
Figure 4 :Regulation of thyroid hormone
Physiological Actions of the Thyroid Hormones
The physiological functions of thyroid hormone are summarized in following
table:
Target
Effect
Mechanism
Heart
Increase heart rate
Increase number and affinity
of B‐adrenergic receptor
Increase strength of
contraction
Increase response to
catecholamine
Increase myosin filaments
Blood
vessels
Vasodilatation
Increase blood flow
Accumulation of metabolite
Muscle
Catabolic
Increase protein catabolism
Bone
Developmental and
metabolic
Promote normal growth and
development
Increase bone turnover
Blood
increase RBC and
blood volume
Increase erythropoietic activity
Brain
Developmental
Promote normal development
Respiratory
Increase the rate
and depth of
respiration
Increase oxygen consumption
and accumulation of
metabolites
Gut
Metabolic
Increase carbohydrate
absorption
Metabolism
Lipid
Increase lipolysis
carbohydrate
Increase all aspect of
metabolism
Protein
Increase protein synthesis
sexual
For normal sexual
function (fertility
and lipido)
Impressive
Other
Calorigenic
Increase oxygen consumption
by metabolic active tissue
Basal metabolic
rate
Increase 100 % in
hyperthyroidism
Normal Arterial Pressure ..why ?????
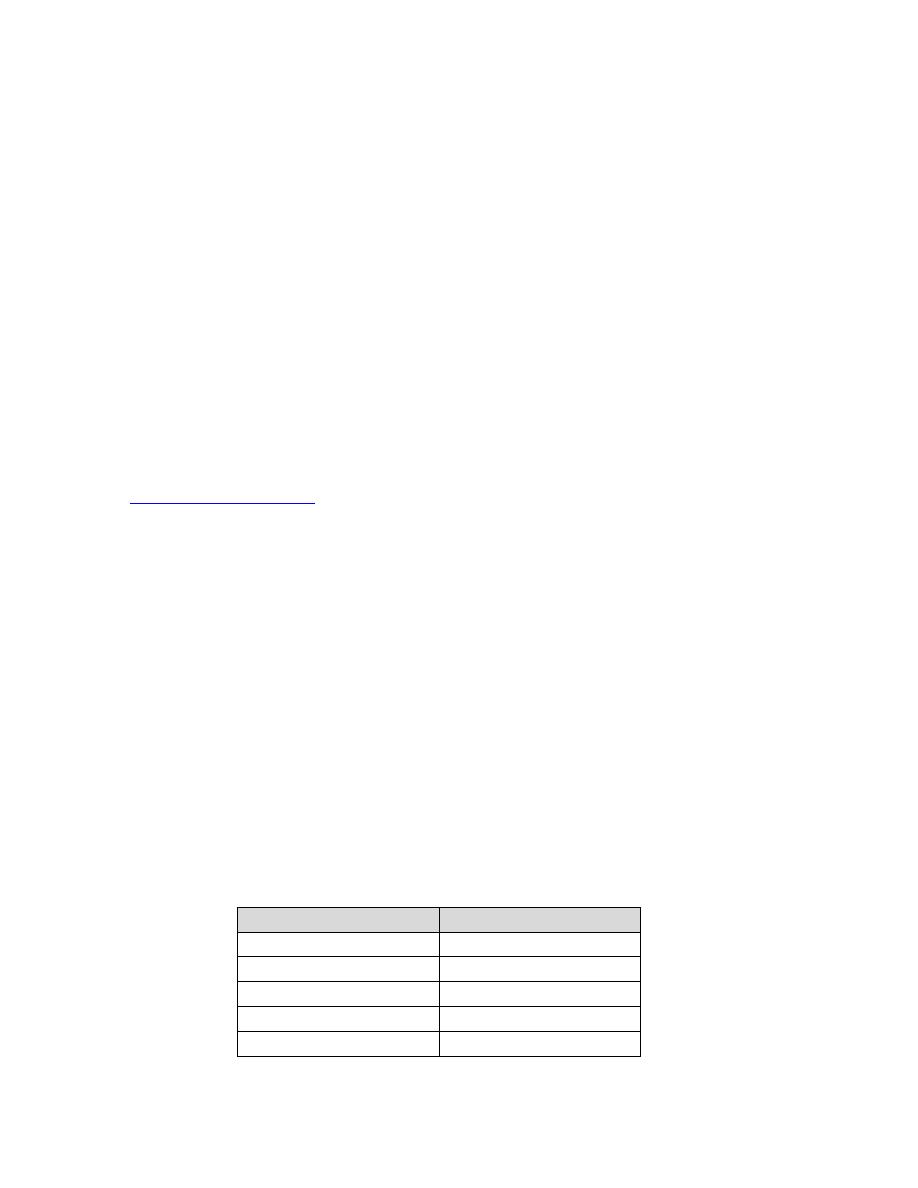
Thyroid function test (TFT)
Thyroid function test (TFT) include TSH , T3 and T4 but measurement of TSH
has become the principal test for the evaluation of thyroid function in most
circumstances.
A TSH value within the reference interval excludes the majority of cases of
primary overt thyroid disease. If TSH is abnormal, confirm the diagnosis with
free thyroxine (fT4).
So if TSH above the reference range , the condition is hypothyroidism
and if TSH below the reference range , the condition is hyperthyroidism.
"Normal" TSH levels
are considered to exclude hypothyroidism or
hyperthyroidism.
Measurements of free T4 and free T3 have replaced measurements of total
T4 and total T3 levels. Many conventional physicians do not test Total T4 or
Free T4. However, in some cases, along with elevated TSH, Total T4 or Free T4
levels that are below the reference range are considered evidence of
hypothyroidism. Along with low/suppressed levels of TSH, Total T4 or Free T4
levels that are above the reference range are considered evidence of
hyperthyroidism. Measurement of free T3 in patients with suspected
hyperthyroidism is rarely indicated. This is reserved for situations where
hyperthyroidism is suspected clinically and TSH is suppressed, but the fT4 is
not elevated. Measurement of fT3 is not indicated in hypothyroidism
Hormone
Reference Range
TSH
0.25 ‐ 5 µIU/mL
Total T4
60‐120nmol/l
Free T4
10.6 – 19.4 pmol/l
Total T3
0.95 ‐2.5 nmol/l
Free T3
4‐8.3 pmol/L
Thyroid Diseases
Disease is associated with both inadequate production and
overproduction of thyroid hormones.
Hypothyroidism: is the result from any condition that results in thyroid
hormone deficiency. Two well‐known examples include:
Iodine deficiency: Iodide is absolutely necessary for production of
thyroid hormones; without adequate iodine intake, thyroid hormones
cannot be synthesized. This problem was seen particularly in areas with
iodine‐deficient soils, and iodine deficiency has been eliminated by iodine
supplementation of salt.
Primary thyroid disease: Inflammatory diseases of the thyroid that
destroy parts of the gland are clearly an important cause of
hypothyroidism.
Common symptoms of hypothyroidism arising after early childhood
include lethargy, fatigue, cold‐intolerance,
Constipation Weight gain ,
weakness, hair loss and reproductive failure. If these signs are severe, the
clinical condition is called myxedema. In the case of iodide deficiency, the
thyroid becomes inordinantly large and is called a goiter.
The most severe form of hypothyroidism is seen in young children with
congenital thyroid deficiency. If that condition is not corrected by
supplemental therapy soon after birth, the child will suffer from
cretinism
, a form of irreversible growth and mental retardation.
Diagnosis of hypothyroidism by sign and symptom , TFT in addition to
imaging techniques.
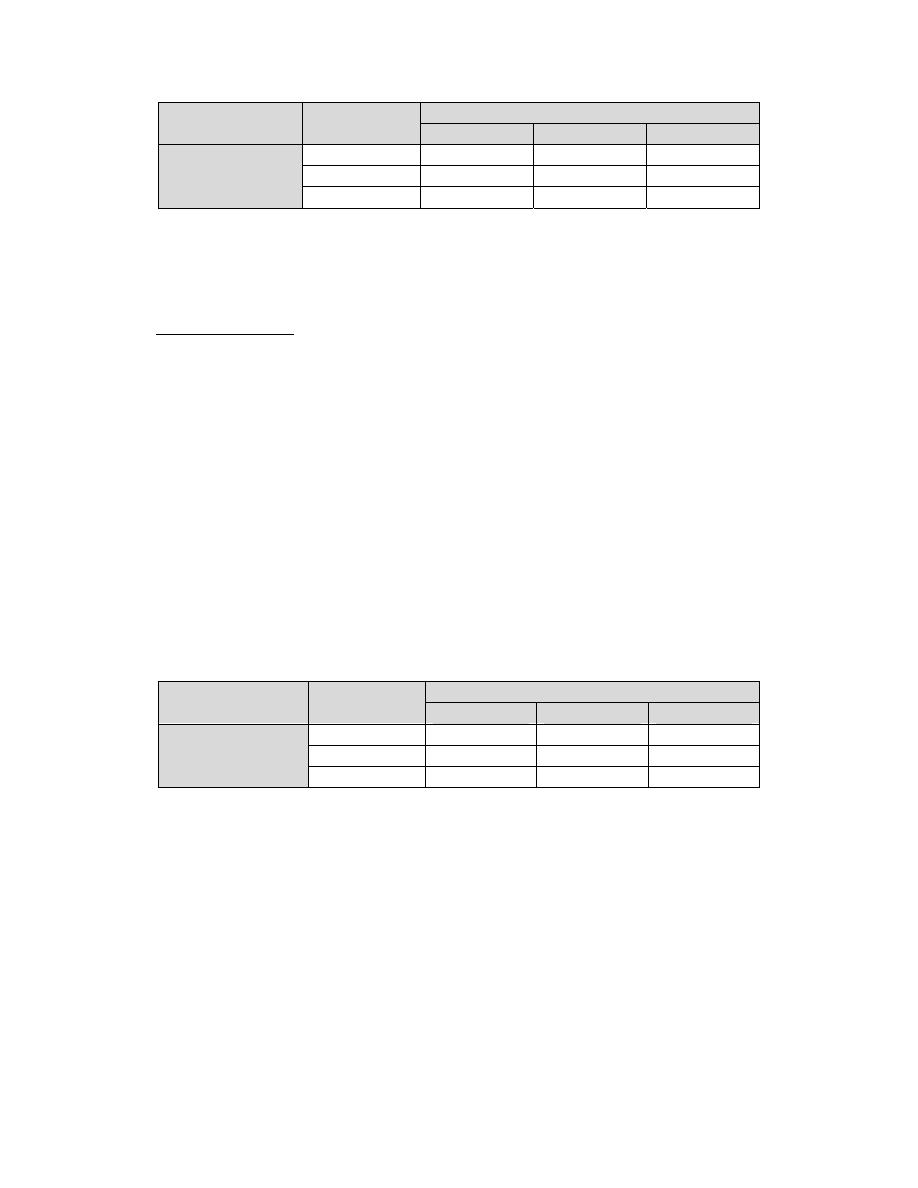
Disease
Types
TFT
TSH
T3
T4
Hypothyroidism
Primary
High
low
low
Secondary
low
low
low
Subclinical
High
Normal
Normal
Most cases of hypothyroidism are readily treated by oral administration
of synthetic thyroid hormone.
Hyperthyroidism: results from over secretion of thyroid hormones. It is
less common than hypothyroidism. The most common form of
hyperthyroidism is Graves disease, an immune disease in which
autoantibodies bind to and activate the thyroid‐stimulating hormone
receptor, leading to continual stimulation of thyroid hormone synthesis.
Common signs of hyperthyroidism are basically the opposite of those
seen in hypothyroidism, and include nervousness, tremor ,Weight loss
,insomnia, high heart rate, eye disease(exophtalmus) and anxiety.
Diagnosis of hyperthyroidism by sign and symptom , TFT , TSH receptor
antibody , in addition to imaging techniques.
Treatment For Hyperthyroidism
A. By using Antithyroid Substances
Antithyroid substances are the drugs which suppress the secretion of
thyroid hormones. Three well‐known antithyroid substances are:
Diseases
Types
TFT
TSH
T3
T4
Hyperthyroidism
Primary
low
High
High
Secondary
High
High
High
Subclinical
Low
Normal
Normal

1. Thiocyanate: prevents thyroid hormone synthesis by inhibiting the
iodide trapping (it can cause competitive inhibition of iodide transport into
the cell).
2. Propylthiouracil Decreases Thyroid Hormone Formation
Propylthiouracil (and other, similar compounds, such as methimazole and
carbimazole) prevents formation of thyroid hormone by blocking the
peroxidase enzyme and by blocking the coupling reaction. Propylthiouracil,
like thiocyanate, does not prevent formation of thyroglobulin. The absence of
T3 and T4 in the thyroglobulin can lead to tremendous feedback
inhancement of TSH secretion, thus promoting growth of the glandular tissue
and forming a goiter.
3.High Concentrations Iodides (
Decrease Thyroid Activity and Thyroid Size
High concentration iodide (100 times the normal plasma level), most
activities of the thyroid gland are decreased. The endocytosis of colloid is
paralyzed , so It has almost immediate shutdown of thyroid hormone
secretion into the blood. Because iodides in high concentrations decrease
all phases of thyroid activity, they slightly decrease the size of the thyroid
gland and especially decrease its blood supply, so it use before
thyroidectomy.
b. By Surgical Removal (thyroidectomy): In advanced cases of
perthyroidism, antithyroid substances is not effected So, thyroidectomy is
done.

